Abstract
Background
Elevation of the immature/total granulocyte (I/T-G) ratio has been reported after out-of-hospital cardiac arrest (OHCA). Our purpose here was to evaluate the prognostic significance of the I/T-G ratio and to investigate whether the I/T-G ratio improves neurological outcome prediction after OHCA.
Methods
This single-center prospective cohort study included consecutive immunocompetent patients admitted to our intensive care unit over a 3-year period (2012–2014) after successfully resuscitated OHCA. The I/T-G ratio was determined in blood samples collected at admission.
Results
We studied 204 patients (77 % male, median age, 58 [48–67] years), of whom 64 % had a suspected cardiac cause of OHCA, 62 % died in the unit, and 31.5 % survived with good cerebral function. Independent outcome predictors by multivariate analysis were age, first shockable rhythm, bystander-initiated resuscitation, and I/T-G ratio. Compared to the model computed without the I/T-G ratio, the model with the ratio performed significantly better [areas under the ROC curves (AUCs), 0.78 vs. 0.83, respectively; P = 0.04]. These items were used to develop the MyeloScore equation: ([0.47 × I/T-G ratio] + [0.023 × age in years]) − 1.26 if initial VF/VT − 1.1 if bystander-initiated CPR. The MyeloScore predicted neurological outcomes with similar accuracy to the previously reported OHCA score (0.83 and 0.85, respectively; P = 0.6). The ROC–AUC was 0.84, providing external validation of the MyeloScore.
Conclusions
The I/T-G ratio independently predicts neurological outcome after OHCA and, when added to other known risk factors, improves neurological outcome prediction. The clinical performance of the MyeloScore requires evaluation in a prospective study.
Similar content being viewed by others
Background
Out-of-hospital cardiac arrest (OHCA) is a major cause of death in Western countries with yearly estimates of 235,000–325,000 in the USA and 350,000–700,000 in Europe [1, 2]. Among patients who recover spontaneous circulation after an OHCA, very few survive with sufficient neurological function to ensure self-sufficiency [3]. Predicting the neurological outcome of patients who are comatose after an OHCA therefore has major ethical and socioeconomic implications [4] yet is an extraordinarily challenging task. Several clinical, laboratory, and electrophysiological risk factors have been identified [5]. Nevertheless, an accurate assessment of the neurological prognosis is usually possible only after several days in the intensive care unit (ICU). In most patients, the neurological prognosis cannot be assessed accurately until several days after admission to the intensive care unit (ICU).
The systemic inflammatory response syndrome (SIRS) initially described in patients with sepsis also develops after successfully resuscitated cardiac arrest. One feature of SIRS is elevation of the immature/total granulocyte (I/T-G) ratio, which is associated with mortality in both neonates and adults with sepsis [6, 7]. In a recent prospective observational study, we documented I/T-G elevation after OHCA and showed that this feature was associated with postcardiac arrest syndrome (PCAS) and ICU mortality [8].
The main objective of this single-center prospective cohort study was to evaluate the performance of I/T-G in predicting neurological outcomes after OHCA. The secondary objective was to develop a score for improving the early accurate prediction of neurological outcomes.
Methods
The study was approved by the our institutional review board (Comité de Protection des Personnes Nord-Ouest), which waived the requirement for written informed consent, as all study procedures were either components of standard care or involved minimal risk to the patients. Nevertheless, oral informed consent was obtained from each patient or next of kin.
Patients
We prospectively included consecutive adults (>18 years) admitted to the medical ICU of the University Hospital, in Caen, France, between June 2012 and November 2014, with successfully resuscitated OHCA. Patients were included if they presented a stable return to spontaneous circulation (ROSC). Some of these patients were also included in a previously published study (130/204 patients) [8]. We excluded pregnant women and patients with immunosuppression (hematological malignancies, solid-organ or bone marrow transplant recipients, leukocyte count <1 × 109/L, corticosteroids in a daily dosage >0.5 mg/kg of prednisone-equivalent, or other immunosuppressants), and patients with refractory cardiac arrest.
For external validation, we used patients with OHCA admitted to the Cochin University Hospital in Paris, France, between January 1, 2014, and December 31, 2015.
Care of patients with OHCA
All patients with a sustained return to spontaneous circulation (ROSC) after OHCA were admitted to our ICU for management according to our standard protocol, which included close monitoring, hemodynamic support, mechanical ventilation, and analgesia/sedation. Briefly, emergency coronary angiography was performed whenever a cardiac etiology could not be ruled out. Therapeutic hypothermia (TH) was used in all patients with initial ventricular fibrillation (VF) or ventricular tachycardia (VT) [9] and in those patients with initial pulseless electric activity (PEA) or asystole who had a suspected cardiac etiology or were expected by the physicians to have good outcomes. TH with a target temperature of 33–34 °C was induced then maintained for 12–24 h using an endovascular cooling catheter (Icy™ Catheter; Alsius, Irvine, CA, USA). During TH, the patients received adjusted midazolam and sufentanil dosages for sedation, combined with atracurium. Sedation was stopped at TH discontinuation in patients without shock or other complications or, in patients not managed with TH, at ICU admission. After TH, the target rewarming rate was 0.5 °C/h and the target temperature was 37 °C.
Neurological function was assessed by daily clinical neurological examinations and, between day 2 and day 4, by serum neuron-specific enolase (NSE) measurements, electroencephalography (EEG), and cortical somatosensory evoked potential (SSEP) recordings. Electrophysiological tests were performed without sedation and, in patients who received TH, after rewarming. In patients with bilateral absence of cortical SSEPs (N20) [10], further treatment was considered futile, and active care was withdrawn. In addition, in accordance with previous reports [5, 11, 12], for patients with at least three adverse prognostic factors after 72 h, withdrawal of active care was discussed at a staff meeting held 5 days after ICU admission. These adverse prognostic factors were absence of pupillary light reflexes or corneal reflexes, extensor posturing or no motor responses to painful stimulation, persistent myoclonus [13], serum NSE elevation [14], and a malignant EEG pattern [15].
Immature granulocyte counts
Each included patient had a blood sample drawn at ICU admission for blood cell counts and automated analysis of leukocyte differentials using the XE-2100 system (Sysmex, Kobe, Japan). The immature granulocyte population was composed of promyelocytes, myelocytes, and metamyelocytes, but not blasts. As described elsewhere [16], a lysing reagent was used to lyse the erythrocytes and to create ultramicroscopic pores in the leukocyte cell membranes that allowed the entry of a polymethine dye with high affinity for nucleic acids. The leukocytes were then analyzed based on nucleic-acid fluorescence and side scatter [17].
Data collection
The following data were collected prospectively for each patient, according to the Utstein style [18]: demographics, cause of OHCA, initial heart rhythm, time from collapse to basic life support (no-flow time) and from basic life support to ROSC (low-flow time), Simplified Acute Physiology Score II (SAPS II) [19] and Sequential Organ Failure Assessment (SOFA) score [20] on day 1, laboratory findings at ICU admission, ICU mortality, and cause of death. The OHCA score was calculated for each patient as follows [21]: [−13 if the initial recorded rhythm is VF or VT] + [6 × ln(no-flow time)] + [9 × ln(low-flow time)] − [1434/(serum creatinine)] + [10 × ln(arterial lactate)]. The CAHP score was calculated based on the previously published nomogram [22]. Postresuscitation shock was defined as a need for intravenous vasoactive therapy (epinephrine or norepinephrine) for more than 6 h after ROSC despite adequate fluid loading.
Neurological outcome assessment
The primary evaluation criterion was the cerebral performance category (CPC) at hospital discharge. For this study, we defined a good neurological outcome as CPC 1 or 2, that is, alive with good cerebral performance (CPC 1) or sufficient cerebral function for independent activities of daily living, with or without mild neurological or psychological deficits (CPC 2). CPC scores 3–5, that is, severe cerebral disability (CPC 3), coma or vegetative state (CPC 4), and death (CPC 5), were defined as a poor neurological outcome.
Statistical analysis
Quantitative variables were described as mean and standard deviation if normally distributed and as median [25th–75th percentiles] otherwise. Qualitative variables were described as n (%). To compare the two groups (good [CPC 1–2] and poor [CPC 3–5] neurological outcome at hospital discharge), we used Student’s t test for means, the Mann–Whitney U test for medians, and the Chi-square test (or Fisher’s exact test when the sample was small) for percentages.
We first performed a univariate analysis to identify patient characteristics at ICU admission that were associated with a good neurological outcome. These variables were then selected in a multivariate logistic regression via a stepwise procedure to build a multivariate model designed to identify factors independently and significantly associated with good neurological outcome. The odds ratios (ORs) and adjusted ORs (aORs) were computed with their 95 % confidence intervals (95 % CIs).
Maximum-likelihood estimation was then performed to analyze all factors available on ICU admission and significantly associated with the neurological outcome in the multivariate model, and the results were used to develop a predictive score (the MyeloScore). The receiver operating characteristics (ROC) curve of this score was plotted and the area under the curve (AUC–ROC) computed (c-index) to assess performance in predicting the neurological outcome.
We used SAS version 15.0 (Chicago, IL, USA) for data analysis. All tests were two-sided, and P values <0.05 were considered statistically significant.
Results
Patient characteristics
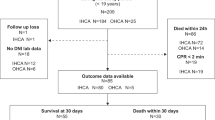
Of the 214 OHCA survivors admitted to our ICU during the 3-year study period, 6 died early after admission, 4 of them had cardiac arrest recurrence, and 2 of them presented a refractory postcardiac arrest shock (n = 2). All of them died at the admission to ICU, before blood samples were drawn. Four had immune deficiencies (immunosuppressants in 3 and hematological malignancy in 1). These patients were not included in the analysis. Thus, 204 patients were studied (Fig. 1). Their main characteristics are listed in Table 1.
The patients were predominantly male (n = 156, 77 %). A cardiac cause was identified in 130 (64 %) patients. Noncardiac causes were respiratory (n = 26), hanging (n = 18), neurological (n = 6), and miscellaneous (n = 24). Coronary angiography was performed in 131 (64 %) patients, and angioplasty in 62 (30 %). TH was induced in 85/91 (93 %) patients with VF/VT and 45/113 (40 %) patients with PEA/asystole. The ICU mortality rate was 62 % (126 patients).
Risk factors associated with a poor neurological outcome (CPC 3–5)
Of the 204 patients, 64 (31.5 %) were CPC 1 or 2 at hospital discharge. Table 2 reports the variables significantly associated with a good neurological outcome by univariate analysis. Those available at ICU admission were younger age, cardiac arrest in a public place, witnessed arrest, bystander-initiated CPR, and on-scene epinephrine therapy. Laboratory variables associated with a good neurological outcome were lower values for arterial lactate, creatinine, and I/T-G. The ROC–AUC for hospital neurological outcome prediction of I/T-G ratio was 0.75 [0.68–0.82].
Variables independently associated with a good neurological outcome by multivariable logistic regression were younger age, initial VF/VT, bystander-initiated cardiopulmonary resuscitation (CPR), and lower I/T-G ratio (Table 3).
Performance of the MyeloScore
MyeloScore development
The equation for computing the MyeloScore based on variables available at ICU admission and independently associated with the neurological outcome at hospital discharge was as follows:
As shown in Fig. 2a, the ROC–AUC of the multivariate model described above performed significantly better than the same model without I/T-G in predicting the neurological outcome at hospital discharge (ROC–AUC, 0.83 vs. 0.78; P = 0.04). Thus, adding I/T-G to established risk factors improved the ability to discriminate between patients with and without good neurological outcomes.
The MyeloScore performed similarly to the previously reported OHCA score in terms of predicting a good neurological outcome (CPC 1 or 2) at hospital discharge [21]. However, a significant difference was noted between the MyeloScore and the CAHP score (ROC–AUC, 0.83 vs. 0.77; P = 0.02) (Fig. 2b).
The optimal cutoff value determined using the Yuden index was 1.044, and the sensitivity and specificity of the MyeloScore were 62.8 and 92.2 %, respectively.
MyeloScore validation
During the 2-year study period, 253 patients with OHCA were admitted to the medical ICU of the Cochin University Hospital. The I/T-G ratio at admission was available for 216 of these patients, who served for a validation study (Table 4). The ROC curve was plotted to assess the ability of the MyeloScore to separate patients with and without good neurological outcomes. The ROC–AUC was 0.84 [0.79–0.89], indicating good performance.
Discussion
The identification of biomarkers that predict the neurological outcome of successfully resuscitated OHCA is an area of active investigation. A few such biomarkers have been shown to perform well and are now used routinely, although they are helpful only several days after ROSC. We have reported that a high I/T-G ratio at ICU admission predicted ICU mortality after OHCA [8], and another group has confirmed this finding [23]. Here, in a large prospective cohort of patients after OHCA, we demonstrated that a higher I/T-G ratio at ICU admission independently predicted severe disability or death (CPC 3–5). Moreover, the admission I/T-G ratio provided prognostic information over and above that given by three previously established risk factors, namely age, VF/VT as the initial recorded rhythm, and bystander-initiated CPR. The MyeloScore based on all four factors performed well in discriminating between patients who would and would not survive with good neurological function. All the factors used in the MyeloScore are available at ICU admission.
I/T-G elevation, or granulocyte left shift, indicates an increase in circulating immature granulocytes and occurs in various acute conditions such as acute hematological malignancies, bleeding, and sepsis. An increase in circulating counts of immature granulocytes is a criterion for SIRS [24]. In survivors of cardiac arrest, ischemia–reperfusion induces a systemic inflammatory process akin to SIRS [25]. This early inflammatory response is often accompanied with a combination of circulatory dysfunction and anoxic brain injury known as postcardiac arrest syndrome (PCAS) [3]. Immature neutrophils enter the circulation early in the course of PCAS. The release by the bone marrow of immature granulocytes into the circulation may involve a variety of mechanisms such as bone marrow ischemia [26], neutrophil paralysis [27], and endotoxemia [28]. The finding of I/T-G elevation at ICU admission after OHCA argues against a role for infection. Furthermore, in our previous study [8], I/T-G was not significantly associated with mean arterial pressure at admission, fluid loading during resuscitation, or body temperature at admission. Thus, I/T-G elevation after OHCA seems to reflect noninfectious systemic inflammation.
Most current blood analyzers provide the count of immature granulocytes or a similar parameter routinely, without additional cost. We chose a widely used automated blood analyzer (XE 2100) to evaluate blood cell counts and I/T-G. Studies have established that automated counting is better than manual morphology-based counting for evaluating numbers of immature granulocytes in peripheral blood [29]. Another group used the ADVIA 2120 analyzer (Siemens, Forchheim, Germany) to determine another marker for granulocyte immaturity, known as the delta neutrophil index, which was high in OHCA survivors [23]. This index was also high in patients with sepsis [6]. Thus, an increase in circulating immature granulocytes may hold prognostic value regardless of the parameter used to assess it.
The early prediction of clinical outcomes after OHCA is singularly difficult. Most of the available prognostic tools can be used only several days after ICU admission. Furthermore, the use of TH delays the evaluation of neurological function [30], increasing the need for prognostic tools that perform well early after cardiac arrest. The OHCA score is based solely on variables available at ICU admission and predicts severe neurological disability or death (CPC 3–5) [21]. It was developed and validated in several cohorts of patients in Paris, France, and then further validated in a prospective cohort study conducted in the USA [31]. The OHCA score variables are initial shockable rhythm, creatinine, arterial lactate, and durations of no-flow and low-flow intervals. These variables chiefly reflect the circumstances before and during OHCA. They are also the main determinants of PCAS severity and are independent from the quality of post-OHCA care in the ICU [32]. In our population, the OHCA score had an AUC–ROC of 0.85, indicating good performance in predicting the short-term neurological outcome.
The MyeloScore performed similarly to the OHCA score in discriminating between patients who were CPC 1–2 or CPC 3–5 at hospital discharge. Importantly, adding the I/T-G ratio to age, initial rhythm, and bystander-initiated CPR significantly improved neurological outcome prediction. Three MyeloScore items are routinely recorded by on-scene healthcare providers, and the remaining item, the I/T-G ratio, is obtained at ICU admission. The durations of the no-flow and low-flow intervals are intentionally not included in the MyeloScore, but the effects of these two variables are probably reflected by the I/T-G ratio and bystander-initiated CPR. Furthermore, data on no-flow and low-flow durations are often inaccurate, and when the arrest is unwitnessed, the no-flow interval is unknown and the OHCA cannot be computed. To minimize the impact of inaccuracies in no-flow and low-flow data, logarithmic transformations of these two variables are used, making computation of the OHCA score more complex. In addition, two other OHCA items, serum creatinine and lactate levels, can be affected not only by OHCA-related ischemia–reperfusion, but also by preexisting disease such as renal failure or cirrhosis. In our cohort, the CAHP score performed less well than the MyeloScore and OHCA score in predicting outcomes. The CAHP score was developed and validated in large cohorts but may suffer from inaccuracies related to the use of a nomogram as opposed to an equation for its computation.
Although scores can contribute to predict neurological outcomes, they provide probabilities and, therefore, cannot serve to make treatment decisions for the individual patient. Instead, neuroprognostication after OHCA should rely on a range of clinical, biological, and neurophysiological tests [33]. A poor score value considered alone cannot justify treatment limitation decisions. It can, however, be added to the many other available predictors, to help adjust the management strategy and anticipate the patient’s needs.
One limitation of our study is the single-center design, which may affect the general applicability of our findings. Furthermore, we did not assess the immune properties of the immature granulocytes. Our study merely indicates an association between a higher proportion of circulating immature granulocytes and a poorer outcome of OHCA. Whether immature granulocytes are involved in the pathogenesis of PCAS remains to be investigated. In sepsis, immature granulocytes seem to perform nearly as well as mature neutrophils in mediating innate immune functions [34]. Moreover, as in the OHCA score studies, the primary outcome in our study was the short-term CPC, at hospital discharge. Long-term CPC was not assessed. Nevertheless, in recent work, CPC at hospital discharge reflected long-term survival and seemed to hold promise for program evaluation and resuscitation research [35]. Last, we did not assess the I/T-G ratio at specific time points after admission. However, when developing the study protocol, we looked at I/T-G ratio values obtained routinely on the day after ICU admission (data not shown). At this time point, often more than 12 h after ROSC, the I/T-G ratio was consistently low (between 0.2 and 0.5 %), even in patients with poor outcomes. Thus, the I/T-G ratio determined later than in our study may not have predictive value.
Conclusion
After OHCA, the I/T-G ratio at ICU admission is independently associated with the neurological outcome at hospital discharge. We used this ratio and three other readily available items to develop the MyeloScore, which performed well in predicting neurological outcomes. The wide availability of I/T-G determination in hospital laboratories may facilitate the use of this marker. Whether the MyeloScore can help in risk stratification and, therefore, in making treatment decisions deserves to be investigated.
Abbreviations
- AUC:
-
area under the curve
- CPC:
-
cerebral performance category
- CPR:
-
cardiopulmonary resuscitation
- EEG:
-
electroencephalography
- ICU:
-
intensive care unit
- I/T-G ratio:
-
immature/total granulocyte ratio
- NSE:
-
neuron-specific enolase
- OHCA:
-
out-of-hospital cardiac arrest
- PCAS:
-
postcardiac arrest syndrom
- PEA:
-
pulseless electric activity
- ROC:
-
receiver operating characteristic
- ROSC:
-
return on spontaneous circulation
- SIRS:
-
systemic inflammatory response syndrom
- SSEP:
-
somatosensory evoked potential
- TH:
-
therapeutic hypothermia
- VF/VT:
-
ventricular fibrillation/ventricular tachycardia
References
Sans S, Kesteloot H, Kromhout D. The burden of cardiovascular diseases mortality in Europe. Task Force of the European Society of Cardiology on Cardiovascular Mortality and Morbidity Statistics in Europe. Eur Heart J. 1997;18(12):1231–48.
Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, Rea T, Lowe R, Brown T, Dreyer J, Davis D, Idris A, Stiell I. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300(12):1423–31.
Mongardon N, Dumas F, Ricome S, Grimaldi D, Hissem T, Pène F, Cariou A. Postcardiac arrest syndrome: from immediate resuscitation to long-term outcome. Ann Intensive Care. 2011;1(1):45.
Lippert FK, Raffay V, Georgiou M, Steen PA, Bossaert L. European Resuscitation Council Guidelines for Resuscitation 2010 Section 10. The ethics of resuscitation and end-of-life decisions. Resuscitation. 2010;81(10):1445–51.
Kudenchuk PJ, Sandroni C, Drinhaus HR, Böttiger BW, Cariou A, Sunde K, Dworschak M, Taccone FS, Deye N, Friberg H, Laureys S, Ledoux D, Oddo M, Legriel S, Hantson P, Diehl JL, Laterre PF. Breakthrough in cardiac arrest: reports from the 4th Paris International Conference. Ann Intensive Care. 2015;5(1):22.
Seok Y, Choi JR, Kim J, Kim YK, Lee J, Song J, Kim SJ, Lee KA. Delta neutrophil index: a promising diagnostic and prognostic marker for sepsis. Shock. 2012;37(3):242–6.
Murphy K, Weiner J. Use of leukocyte counts in evaluation of early-onset neonatal sepsis. Pediatr Infect Dis J. 2012;31(1):16–9.
Sauneuf B, Bouffard C, Cornet E, Daubin C, Desmeulles I, Masson R, Seguin A, Valette X, Terzi N, Parienti JJ, du Cheyron D. Immature/total granulocyte ratio: a promising tool to assess the severity and the outcome of post-cardiac arrest syndrome. Resuscitation. 2014;85(8):1115–9.
Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, Smith K. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346(8):557–63.
Zandbergen EG, Hijdra A, Koelman JH, Hart AA, Vos PE, Verbeek MM, de Haan RJ, PROPAC Study Group. Prediction of poor outcome within the first 3 days of postanoxic coma. Neurology. 2006;66(7):62–8.
Daubin C, Guillotin D, Etard O, Gaillard C, du Cheyron D, Ramakers M, Bouchet B, Parienti JJ, Charbonneau P. A clinical and EEG scoring system that predicts early cortical response (N20) to somatosensory evoked potentials and outcome after cardiac arrest. BMC Cardiovasc Disord. 2008;8:35.
Wijdicks EF, Hijdra A, Young GB, Bassetti CL, Wiebe S. Practice parameter: prediction of outcome in comatose survivors after cardiopulmonary resuscitation (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2006;67(2):203–10.
Thomke F, Marx JJ, Sauer O, Hundsberger T, Hägele S, Wiechelt J, Weilemann SL. Observations on comatose survivors of cardiopulmonary resuscitation with generalized myoclonus. BMC Neurol. 2005;5:14.
Daubin C, Quentin C, Allouche S, Etard O, Gaillard C, Seguin A, Valette X, Parienti JJ, Prevost F, Ramakers M, Terzi N, Charbonneau P, du Cheyron D. Serum neuron-specific enolase as predictor of outcome in comatose cardiac-arrest survivors: a prospective cohort study. BMC Cardiovasc Disord. 2011;11:48.
Synek VM. Value of a revised EEG coma scale for prognosis after cerebral anoxia and diffuse head injury. Clin Electroencephalogr. 1990;21(1):25–30.
Ruzicka K, Veitl M, Thalhammer-Scherrer R, Schwarzinger I. The new hematology analyzer Sysmex XE-2100: performance evaluation of a novel white blood cell differential technology. Arch Pathol Lab Med. 2001;125(3):391–6.
Fujimoto H, Sakata T, Hamaguchi Y, Shiga S, Tohyama K, Ichiyama S, Wang FS, Houwen B. Flow cytometric method for enumeration and classification of reactive immature granulocyte populations. Cytometry. 2000;42(6):371–8.
Peberdy MA, Cretikos M, Abella BS, Devita M, Goldhill D, Kloeck W, Kronick SL, Morrison LJ, Nadkarni VM, Nichol G, Nolan JP, Parr M, Tibballs J, van der Jagt EW, Young L. Recommended guidelines for monitoring, reporting, and conducting research on medical emergency team, outreach, and rapid response systems: an Utstein-style scientific statement: a scientific statement from the International Liaison Committee on Resuscitation (American Heart Association, Australian Resuscitation Council, European Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, and the New Zealand Resuscitation Council); the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiopulmonary, Perioperative, and Critical Care; and the Interdisciplinary Working Group on Quality of Care and Outcomes Research. Circulation. 2007;116(21):2481–500.
Le Gall JR, Lemeshow S, Saulnier F. A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270(24):2957–63.
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, Reinhart CK, Suter PM, Thijs LG. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707–10.
Adrie C, Cariou A, Mourvillier B, Laurent I, Dabbane H, Hantala F, Rhaoui A, Thuong M, Monchi M. Predicting survival with good neurological recovery at hospital admission after successful resuscitation of out-of-hospital cardiac arrest: the OHCA score. Eur Heart J. 2006;27(23):2840–5.
Maupain C, Bougouin F, Lamhaut L, Deye N, Diehl JL, Geri G, Perier MC, Beganton F, Marijon E, Jouven X, Cariou A, Dumas F. The CAHP (Cardiac Arrest Hospital Prognosis) score: a tool for risk stratification after out-of-hospital cardiac arrest. Eur Heart J. 2015. doi:10.1093/eurheartj/ehv556.
Yune HY, Chung SP, Park YS, Chung HS, Lee HS, Lee JW, Park JW, You JS, Park I, Lee HS. Delta neutrophil index as a promising prognostic marker in out of hospital cardiac arrest. PLoS One. 2015;10(3):e0120677. doi:10.1371/journal.pone.0120677.
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G, International Sepsis Definitions Conference. 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Intensive Care Med. 2003;29(4):530–8.
Adrie C, Adib-Conquy M, Laurent I, Monchi M, Vinsonneau C, Fitting C, Fraisse F, Dinh-Xuan AT, Carli P, Spaulding C, Dhainaut JF, Cavaillon JM. Successful cardiopulmonary resuscitation after cardiac arrest as a “sepsis-like” syndrome. Circulation. 2002;106(5):562–8.
Shah AP, Youngquist ST, McClung CD, Tzvetkova E, Hanif MA, Rosborough JP, Niemann JT. Markers of progenitor cell recruitment and differentiation rise early during ischemia and continue during resuscitation in a porcine acute ischemia model. J Interferon Cytokine Res. 2011;31(6):509–13.
Adrie C, Laurent I, Monchi M, Cariou A, Dhainaut JF, Spaulding C. Postresuscitation disease after cardiac arrest: a sepsis-like syndrome? Curr Opin Crit Care. 2004;10(3):208–12.
Pillay J, Ramakers BP, Kamp VM, Loi AL, Lam SW, Hietbrink F, Leenen LP, Tool AT, Pickkers P, Koenderman L. Functional heterogeneity and differential priming of circulating neutrophils in human experimental endotoxemia. J Leukoc Biol. 2010;88(1):211–20.
Fernandes B, Hamaguchi Y. Automated enumeration of immature granulocytes. Am J Clin Pathol. 2007;128(3):454–63.
Perman SM, Kirkpatrick JN, Reitsma AM, Gaieski DF, Lau B, Smith TM, Leary M, Fuchs BD, Levine JM, Abella BS, Becker LB, Merchant RM. Timing of neuroprognostication in postcardiac arrest therapeutic hypothermia*. Crit Care Med. 2012;40(3):719–24.
Hunziker S, Bivens MJ, Cocchi MN, Miller J, Salciccioli J, Howell MD, Donnino MW. International validation of the out-of-hospital cardiac arrest score in the United States. Crit Care Med. 2011;39(7):1670–4.
Donnino MW, Miller JC, Bivens M, Cocchi MN, Salciccioli JD, Farris S, Gautam S, Cutlip D, Howell M. A pilot study examining the severity and outcome of the post-cardiac arrest syndrome: a comparative analysis of two geographically distinct hospitals. Circulation. 2012;126(12):1478–83.
Sandroni C, Cariou A, Cavallaro F, Cronberg T, Friberg H, Hoedemaekers C, Horn J, Nolan JP, Rossetti AO, Soar J. Prognostication in comatose survivors of cardiac arrest: an advisory statement from the European Resuscitation Council and the European Society of Intensive Care Medicine. Resuscitation. 2014;85(12):1779–89.
Drifte G, Dunn-Siegrist I, Tissieres P, Pugin J. Innate immune functions of immature neutrophils in patients with sepsis and severe systemic inflammatory response syndrome. Crit Care Med. 2013;41(3):820–32.
Phelps R, Dumas F, Maynard C, Silver J, Rea T. Cerebral performance category and long-term prognosis following out-of-hospital cardiac arrest. Crit Care Med. 2013;41(5):1252–7.
Authors’ contributions
BS, CB, EC, and NT designed the study, analyzed and interpreted the data and wrote the manuscript. JJP performed statistical analysis and had an important contribution to the interpretation of the data. CD, JB, AS, XV, and DDC participated in the design of the study and the interpretation of the data. NC collected the data needed for external validation of the MyeloScore. All authors read and approved the final manuscript.
Acknowledgements
This work was supported by institutional and departmental funds (Caen Teaching Hospital and Intensive Care Unit, respectively).
Competing interests
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Sauneuf, B., Bouffard, C., Cornet, E. et al. Immature/total granulocyte ratio improves early prediction of neurological outcome after out-of-hospital cardiac arrest: the MyeloScore study. Ann. Intensive Care 6, 65 (2016). https://doi.org/10.1186/s13613-016-0170-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-016-0170-4