Abstract
Background
Prognostic abilities of medical parameters, which are scoring systems, measurements and biomarkers, are important for stratifying critically ill patients. Indocyanine green plasma disappearance (ICG-PDR) is an established clinical tool for the assessment of liver perfusion and function. Copeptin, MR-proANP and pro-ADM are biomarkers whose prognostic value is still unclear. The goal of this prospective study was to evaluate ICG-PDR, copeptin, MR-proANP and pro-ADM to predict prolonged length of stay (pLOS) in the ICU.
Methods
This study was conducted as a prospective single center study including 110 consecutively admitted ICU patients. Primary endpoint was prolonged length of stay (pLOS) in the ICU, defined as more than three days of stay there.
Results
ROC analysis showed an AUC of 0.73 for ICG-PDR, 0.70 for SAPS II, 0.65 for MR-proANP, 0.64 for pro-ADM and 0.54 for copeptin for pLOS in the ICU.
Conclusions
The prediction of pLOS in the ICU might be better by means of ICG-PDR than with the new biomarkers copeptin, MR-proANP or pro-ADM. Nevertheless, there is more need for research to evaluate whether ICG-PDR is an overall prognostic marker for pLOS.
Trial registration
(ClinicalTrials.gov number, NCT01126554).
Similar content being viewed by others
Background
The prognostic abilities of medical parameters, which are scoring systems, measurements and biomarkers, are important for stratifying critically ill patients [[1]] to optimize resources and further investigation in this area is warranted.
The Simplified Acute Physiology Score (SAPS II) is a validated scoring system to predict mortality in critically ill patients [[2]]. Regardless of the underlying diagnosis, the combination of 17 variables allows reliable outcome prediction. SAPS II models have proved to be competitive to the SOFA (Sequential Organ Failure Assessment) based score models [[3]]. However, SAPS II scoring is less reliable for prediction of length of stay (LOS) in the ICU [[4],[5]].
Indocyanine green plasma disappearance rate (ICG-PDR) is closely correlated to hepatic function due to its hepatic metabolization. The non-invasive ICG measurement, based on pulse dye measurement using a finger-clip, has been shown to correlate well with the classical measurements [[6]] and is non-invasive and easy to use. ICG-PDR has proven to predict mortality in critically ill patients comparable to the SAPS II score [[7]], as well as to predict complications in liver cirrhosis patients [[8]] and posthepatectomy liver failure [[9]]. The capability of ICG-PDR to predict LOS in the ICU remains elusive.
Several new biomarkers are under investigation in the ICU for critically ill patients.
Copeptin, a peptide of 39 amino acids, is the C-terminal part of pro-arginine vasopressin also called C-terminal-pro-arginine vasopressin (CT-proAVP). It reveals several physiologic actions: arteriolar vasoconstriction (V1-receptor mediated), an anti-diuretic effect in the kidneys (V2-receptor mediated) [[10]] and is probably involved in the secretion of ACTH (V3-receptor mediated) [[11]]. It has been proven to predict mortality in patients with community acquired pneumonia [[12]], stroke [[13]], and traumatic brain injury [[14]].
Atrial natriuretic peptide (ANP) is a counter-regulatory hormone synthesized in the heart, being cleaved and released during hemodynamic stress or myocardial injury. High mid-region proANP levels (MR-proANP) are associated with high mortality in patients with acute myocardial infarction [[15]] and chronic obstructive pulmonary disease (COPD) exacerbation [[16]].
Proadrenomedullin (pro-ADM) is a 185 amino acid-long precursor of the vasodilator adrenomedullin (52 amino acids). It is released during severe infection, especially septic shock and is influenced by age, body mass index and glomerular filtration rate in healthy volunteers [[17]]. Like MR-proANP, it has been proven to predict mortality in patients with COPD exacerbation [[18]] and acute myocardial infarction [[19],[20]].
While these biomarkers have proven useful to predict mortality in different settings, to our knowledge no data are available concerning their predictive value of ICU pLOS. The goal of this study was to investigate the accuracy of ICG-PDR, SAPS II, copeptin, MR-proANP, pro-ADM and other established biomarkers for prediction of pLOS in the ICU.
Methods
Study design
This prospective single center study was conducted at the surgical ICU (10 beds, 920 patients in the year 2010) at the University Hospital of Zurich from 1 August 2010 to 31 October 2010. During this period, all patients admitted to our ICU were eligible for inclusion regardless of underlying disease or reason for admission. Exclusion criteria were: age below 18 years, pregnancy, inclusion in another study, patients or relatives not able to understand the German language or known iodine allergy (a component of ICG). The aim was the comparison of the prognostic value of the ICG-liver test and SAPS II score on the one hand with new biomarkers (copeptin, pro-ADM and MR-proANP), and on the other hand to established biomarkers (bilirubin, aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (AP), International Normalized Ratio (INR), hemoglobin, white blood cell (WBC) count, activated partial thromboplastin time (aPTT), dDimer, cystatin C, C-reactive protein (CRP), procalcitonin (PCT), IL-6, the B-type natriuretic peptide (NT-proBNP) Primary endpoint was prolonged length of stay (pLOS) in the ICU, represented by more than three days. A power calculation was performed with the assumption of 5% mortality and 30% of pLOS in the patient population; therefore 110 patients with an estimated drop-out of 10% were prospectively included. Initially, mortality was considered as primary endpoint but the financial burden of such a large sample size (hundreds of patients) was unaffordable. Therefore, the study was performed with the endpoint pLOS.
The study was approved by the local ethical committee and informed consent was achieved by all patients or next of kin. The trial was registered as ClinicalTrials.gov number, NCT 01126554.
Study protocol
After achievement of informed consent, patients were included into the study. Baseline characteristics were collected. Reason for ICU admission was classified as visceral surgery, thoracic surgery, medical disease and others. Blood samples used for the analysis were drawn within two hours after admission. The ICG-liver testing was performed non-invasively within 60 minutes after ICU admission by pulse spectrophotometry (LiMON®, Pulsion Medical Systems AG, Munich, Germany). Following an intravenous bolus injection of ICG (0.25 mg/kg; ICG Pulsion Medical Systems AG, Munich, Germany), plasma ICG concentrations were determined by pulse spectrophotometry with a finger-clip sensor. Using two near-infrared wavelengths, the plasma disappearance rate of ICG (ICG-PDR) was calculated automatically by the time course of the blood ICG concentration. Normal values are defined as ICG-PDR ≥ 16%/minute. SAPS II score was calculated after 24 hours.
Laboratory analysis
Venous whole blood samples were collected in tubes containing either ethylenediaminetetraacetic acid (EDTA) or lithium heparin. Copeptin, MR-proANP and pro-ADM were determined in EDTA plasma by Time-Resolved Amplified Cryptate Emission (TRACE) technology on the KRYPTOR analyzer (BRAHMS, Henningsdorf, Germany).
Plasma levels of PCT and NT-proBNP were measured by electrochemiluminescence immunoassays on a COBAS 8000 modular analyzer (Roche Diagnostics, Rotkreuz, Switzerland). IL-6 levels were analyzed using a chemiluminescence enzyme immunoassay on an Immulite 2500 analyzer (Siemens Healthcare Diagnostics, Zurich, Switzerland) and cystatin C was measured by immuno-nephelometry on a Behring nephelometer system (Dade Behring, Dudingen, Switzerland).
Plasma concentrations of AST, ALT, AP, bilirubin and CRP, were measured on a COBAS 8000 modular analyzer (Roche Diagnostics, Rotkreuz, Switzerland).
Statistical analysis
All subjects were grouped into the two clusters: ICU stay ≤ three days and prolonged ICU stay (>three days). Univariate statistics of the biomarkers and tests applied in this study were done by Mann-Whitney U-test or Fishers exact test as appropriate. All P-values were considered two-sided and statistical significance was considered as P < 0.05. Biomarkers and tests showing statistical significance were further examined by receiver operating characteristics (ROC) analysis. Comparison of ROC analysis was done by comparison of area under the curve (AUC).
Accuracy of ICG, SAPS II, IL-6, dDimer, NT-proBNP, MR-proANP and pro-ADM were tested and the cut offs defined (significance and specificity based) by ROC analysis. Statistics were done with SPSS for Windows version 18.0 (SPSS, Chicago, IL, USA).
Results
Baseline characteristics
We screened 117 patients admitted to the ICU during the study period. Seven patients were not enrolled due to exclusion criteria. After a drop-out of four patients, because of two lost blood sample sets and two withdrawals of consent, the data of 106 patients were analyzed.
Forty-one of the patients were female (38.7%) and 65 male (61.3%). ICU mortality was 2.8% (n = 3), whereas hospital mortality was 6.6% (n = 7). The four diagnostic groups were: visceral surgery 53 patients (50.0%), thoracic surgery 27 patients (25.5%), medical group 7 patients (6.6%) and others 19 patients (17.9%). Thirty-eight patients were ventilated on admission to the ICU, whereas 28 could be extubated within the first 12 hours after admission. In the visceral surgery group, 20 underwent liver surgery (wedge resection, left or right hemihepatectomy). Eight patients had preexisting liver dysfunction (2 Child C and 6 Child B cirrhosis).
Overall, 25 (23.6%) patients had a prolonged length of stay in the ICU. There was no statistical significant difference between the diagnostic groups in respect to pLOS or normal LOS. The median of LOS was 4.2 days in all patients.
Univariate data
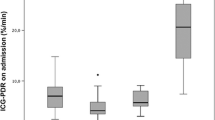
The univariate analysis of laboratory values between the short stay and prolonged stay groups in the ICU and baseline criteria are shown in Table 1. There was no statistical difference in baseline criteria between the diagnostic groups. There was a statistical significance between the two groups concerning ICG-PDR (P = 0.03), bilirubin (P = 0.003), AST (P = 0.02), ALT (P = 0.05), SAPS II (P = 0.01), IL-6 (P = 0.005), Ddimer (P = 0.02), aPTT (0.05), MR-proANP (P = 0.03) and pro-ADM (P = 0.03) while copeptin did not show a statistical significant difference (P = 0.67).
ROC analysis
The ROC analysis is shown in Table 2. ICG-PDR (AUC 0.73) and SAPS II (AUC 0.7) did perform better for prediction for prolonged length of stay in the ICU than the new biomarkers MR-proANP (AUC 0.65), pro-ADM (AUC 0.64) and copeptin (AUC 0.54). There was no statistical difference between ICG-PDR and SAPS II (P = 0.78).
Discussion
The main finding of this study is the value of ICG-PDR in prediction of pLOS in the ICU. The measurement is easy to perform and, in contrast to the SAPS II score, consists of only one value and not of seventeen values, which made its application time-saving and quick. As ICG-PDR reflects liver function, this finding confirms that impaired liver function is of crucial importance in the assessment and prognosis of critical care patients. Impaired liver function shows a wide spectrum of immunosuppressant effects, metabolic and pharmacological disturbances and coagulation disorders. Thus, ICG-PDR might be a representative surrogate for a summation of these effects with negative influence for intensive care patients. This suggestion is supported by the fact that in our study the patients with pLOS also had higher serum bilirubin, AST and ALT levels as well as a prolonged aPTT. There was no better discrimination of MR-proANP and pro-ADM between long- and short-term LOS in the ICU than ICG-PDR. A potential explanation might be that the heterogeneous population presented with impaired liver function at a grade of severity, but the MR-proANP and pro-ADM pathways were activated by different underlying pathologies and probably do not reflect the severity of disease. Nevertheless, there are patient populations in which those markers showed a good predictive accuracy in prediction of outcome [[18],[21],[22]], but still we lack data about ICU patients. A recent study by Guignant et al. reported an association between elevated pro-ADM levels and nosocomial infection in patients after septic shock, whereas copeptin and MR-proANP showed no correlation in this population [[23]].
Copeptin failed to discriminate LOS between long-term and short-term patients; therefore, its prognostic value seems to be weak in this area. One reason might be that the main trigger for copeptin release - as a part of the vasopressin pathway - is hypovolemia, which, in our study population of postsurgical and resuscitated medical ICU patients, was definitely not the case. In our institution, most of the unstable patients are monitored by the PiCCO-system (Pulsion, Munich, Germany), Swan-Ganz catheter or by means of echocardiography, which might have led to an adequate volemia at the point of admission.
One important study limitation is the heterogeneous and small patient population, which might explain some of the results. Nevertheless, our cohort was a representative ICU population of a university hospital center with patients of considerable pathological complexity and severity. Furthermore, we assessed only one data point of every marker per patient on admission. Whether a repetitive regimen of measurement at, for instance, day 3 or 5, would have shown different results, remains unclear. These findings might help - but only in combination with clinical signs and the experience of the ICU staff - to utilize and optimize the scarce ICU resources by early stratification, which might lead to earlier but safe discharge to intermediate care units.
Conclusion
The prediction of pLOS in the ICU might be better by means of ICG-PDR than with the new biomarkers copeptin, MR-proANP or pro-ADM. Nevertheless, there is a need for further research to evaluate whether ICG-PDR is an overall prognostic marker for pLOS.
Abbreviations
- ACTH:
-
adrenocorticotropic hormone
- ALT:
-
alanine transaminase
- ANP:
-
atrial natriuretic peptide
- AP:
-
alkaline phosphatase
- aPTT:
-
activated partial thromboplastin time
- AST:
-
aspartate transaminase
- AUC:
-
area under the curve
- COPD:
-
chronic obstructive pulmonary disease
- CRP:
-
C-reactive protein
- CT-proAVP:
-
C-terminal-pro-arginine vasopressin
- EDTA:
-
ethylenediaminetetraacetic acid
- ICG-PDR:
-
indocyanine green plasma disappearance rate
- IL:
-
interleukin
- INR:
-
International Normalized Ratio
- LOS:
-
length of stay
- MR-proANP:
-
pro-atrial natriuretic peptide
- NT-proBNP:
-
B-type natriuretic peptide
- PCT:
-
procalcitonin
- pLOS:
-
prolonged length of stay
- pro-ADM:
-
proadrenomedullin
- ROC:
-
receiver operating characteristics
- SAPS II:
-
Simplified Acute Physiology Score
- SOFA:
-
Sequential Organ Failure Assessment
- TRACE:
-
Time-Resolved Amplified Cryptate Emission
- WBC:
-
white blood count
References
Stevens V, Lodise TP, Tsuji B, Stringham M, Butterfield J, Dodds Ashley E, Brown K, Forrest A, Brown J: The utility of acute physiology and chronic health evaluation II scores for prediction of mortality among intensive care unit (ICU) and non-ICU patients with methicillin-resistant Staphylococcus aureus bacteremia. Infect Control Hosp Epidemiol 2012,33(6):558–564. 10.1086/665731
Le Gall JR, Lemeshow S, Saulnier F: A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 1993,270(24):2957–2963. 10.1001/jama.1993.03510240069035
Minne L, Abu-Hanna A, de Jonge E: Evaluation of SOFA-based models for predicting mortality in the ICU: a systematic review. Crit Care 2008,12(6):R161. 10.1186/cc7160
Vasilevskis EE, Kuzniewicz MW, Cason BA, Lane RK, Dean ML, Clay T, Rennie DJ, Vittinghoff E, Dudley RA: Mortality probability model III and simplified acute physiology score II: assessing their value in predicting length of stay and comparison to APACHE IV. Chest 2009,136(1):89–101. 10.1378/chest.08-2591
Sakr Y, Marques J, Mortsch S, Gonsalves MD, Hekmat K, Kabisch B, Kohl M, Reinhart K: Is the SAPS II score valid in surgical intensive care unit patients? J Eval Clin Pract 2012,18(2):231–237. 10.1111/j.1365-2753.2010.01559.x
Faybik P, Krenn CG, Baker A, Lahner D, Berlakovich G, Steltzer H, Hetz H: Comparison of invasive and noninvasive measurement of plasma disappearance rate of indocyanine green in patients undergoing liver transplantation: a prospective investigator-blinded study. Liver Transpl 2004,10(8):1060–1064. 10.1002/lt.20205
Sakka SG, Reinhart K, Meier-Hellmann A: Prognostic value of the indocyanine green plasma disappearance rate in critically ill patients. Chest 2002,122(5):1715–1720. 10.1378/chest.122.5.1715
Forestier J, Dumortier J, Guillaud O, Ecochard M, Roman S, Boillot O, Lutringer D, Scoazec JY, Subtil F, Mion F: Noninvasive diagnosis and prognosis of liver cirrhosis: a comparison of biological scores, elastometry, and metabolic liver function tests. Eur J Gastroenterol Hepatol 2010,22(5):532–540. 10.1097/MEG.0b013e3283343f58
de Liguori CN, O’Reilly DA, Dajani K, Ghaneh P, Poston GJ, Wu AV: Perioperative use of the LiMON method of indocyanine green elimination measurement for the prediction and early detection of post-hepatectomy liver failure. Eur J Surg Oncol 2009,35(9):957–962. 10.1016/j.ejso.2009.02.003
Nickel CH, Bingisser R, Morgenthaler NG: The role of copeptin as a diagnostic and prognostic biomarker for risk stratification in the emergency department. BMC Med 2012, 10: 7. 10.1186/1741-7015-10-7
Thibonnier M, Preston JA, Dulin N, Wilkins PL, Berti-Mattera LN, Mattera R: The human V3 pituitary vasopressin receptor: ligand binding profile and density-dependent signaling pathways. Endocrinology 1997,138(10):4109–4122.
Kruger S, Ewig S, Kunde J, Hanschmann A, Marre R, Suttorp N, Welte T: C-terminal provasopressin (copeptin) in patients with community-acquired pneumonia - influence of antibiotic pre-treatment: results from the German competence network CAPNETZ. J Antimicrob Chemother 2009,64(1):159–162. 10.1093/jac/dkp148
Katan M, Fluri F, Morgenthaler NG, Schuetz P, Zweifel C, Bingisser R, Muller K, Meckel S, Gass A, Kappos L, Steck AJ, Engelter ST, Müller B, Christ-Crain M: Copeptin: a novel, independent prognostic marker in patients with ischemic stroke. Ann Neurol 2009,66(6):799–808. 10.1002/ana.21783
Dong XQ, Huang M, Yang SB, Yu WH, Zhang ZY: Copeptin is associated with mortality in patients with traumatic brain injury. J Trauma 2011,71(5):1194–1198. 10.1097/TA.0b013e31821283f2
Meune C, Twerenbold R, Drexler B, Balmelli C, Wolf C, Haaf P, Reichlin T, Irfan A, Reiter M, Zellweger C, Meissner J, Stelzig C, Freese M, Capodarve I, Mueller C: Midregional pro-A-type natriuretic peptide for diagnosis and prognosis in patients with suspected acute myocardial infarction. Am J Cardiol 2012,109(8):1117–1123. 10.1016/j.amjcard.2011.11.047
Bernasconi M, Tamm M, Bingisser R, Miedinger D, Leuppi J, Muller B, Christ-Crain M, Stolz D: Midregional proatrial natriuretic peptide predicts survival in exacerbations of COPD. Chest 2011,140(1):91–99. 10.1378/chest.10-1353
Bhandari SS, Davies JE, Struck J, Ng LL: Influence of confounding factors on plasma mid-regional pro-adrenomedullin and mid-regional pro-A-type natriuretic peptide concentrations in healthy individuals. Biomarkers 2011,16(3):281–287. 10.3109/1354750X.2011.553750
Stolz D, Christ-Crain M, Morgenthaler NG, Miedinger D, Leuppi J, Muller C, Bingisser R, Struck J, Muller B, Tamm M: Plasma pro-adrenomedullin but not plasma pro-endothelin predicts survival in exacerbations of COPD. Chest 2008,134(2):263–272. 10.1378/chest.08-0047
Meune C, Balmelli C, Twerenbold R, Reiter M, Reichlin T, Ziller R, Drexler B, Stelzig C, Freese M, Wolf C, Haaf P, Osswald S, Mueller C: Utility of 14 novel biomarkers in patients with acute chest pain and undetectable levels of conventional cardiac troponin. Int J Cardiol 2012, ᅟ: ᅟ. doi:10.1016/j.ijcard.2012.03.117
Klip IT, Voors AA, Anker SD, Hillege HL, Struck J, Squire I, van Veldhuisen DJ, Dickstein K: Prognostic value of mid-regional pro-adrenomedullin in patients with heart failure after an acute myocardial infarction. Heart 2011,97(11):892–898. 10.1136/hrt.2010.210948
Miller WL, Hartman KA, Burritt MF, Grill DE, Rodeheffer RJ, Burnett JC Jr, Jaffe AS: Serial biomarker measurements in ambulatory patients with chronic heart failure: the importance of change over time. Circulation 2007,116(3):249–257. 10.1161/CIRCULATIONAHA.107.694562
Shah RV, Truong QA, Gaggin HK, Pfannkuche J, Hartmann O, Januzzi JL Jr: Mid-regional pro-atrial natriuretic peptide and pro-adrenomedullin testing for the diagnostic and prognostic evaluation of patients with acute dyspnoea. Eur Heart J 2012, ᅟ: ᅟ.
Guignant C, Voirin N, Venet F, Lepape A, Monneret G: Persistent high level of circulating midregional-proadrenomedullin and increased risk of nosocomial infections after septic shock. J Trauma Acute Care Surg 2012,72(1):293–296.
Acknowledgements
This study was supported by BRAHMS only with laboratory kits and material. There was absolutely no involvement of BRAHMS in designing, conducting, analyzing samples/data or publication of the study at any time.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
Each author have participated sufficiently in the work to take public responsibility for appropriate portions of the content: MF, BZ and RG collected the majority of the data and drafted parts of the manuscript. KS, AV performed laboratory tests and drafted parts of the manuscript. PAS performed statistical analysis and drafted parts of the manuscript. SK redrafted the article and did most of the revisions. AV and MB led the project, collected parts of the data, performed additional statistical analysis and drafted parts of the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zoller, B., Spanaus, K., Gerster, R. et al. ICG-liver test versus new biomarkers as prognostic markers for prolonged length of stay in critically ill patients - a prospective study of accuracy for prediction of length of stay in the ICU. Ann. Intensive Care 4, 19 (2014). https://doi.org/10.1186/s13613-014-0019-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-014-0019-7