Abstract
The urokinase plasminogen activator receptor (uPAR) plays a multifaceted role in almost any process where migration of cells and tissue-remodeling is involved such as inflammation, but also in diseases as arthritis and cancer. Normally, uPAR is absent in healthy tissues. By its carefully orchestrated interaction with the protease urokinase plasminogen activator and its inhibitor (plasminogen activator inhibitor-1), uPAR localizes a cascade of proteolytic activities, enabling (patho)physiologic cell migration. Moreover, via the interaction with a broad range of cell membrane proteins, like vitronectin and various integrins, uPAR plays a significant, but not yet completely understood, role in differentiation and proliferation of cells, affecting also disease progression. The implications of these processes, either for diagnostics or therapeutics, have received much attention in oncology, but only limited beyond. Nonetheless, the role of uPAR in different diseases provides ample opportunity to exploit new applications for targeting. Especially in the fields of oncology, cardiology, rheumatology, neurology, and infectious diseases, uPAR-targeted molecular imaging could offer insights for new directions in diagnosis, surveillance, or treatment options.
Similar content being viewed by others
Background
Tissue remodeling is pivotal in embryonic development, tissue repair, and numerous pathologies. Temporary degradation of the extracellular matrix (ECM) is a delicate process requiring the careful coordination of proteases, receptors, and cell-signaling molecules where over-degradation can result in osteoarthritis, osteolysis, cardiomyopathy, and invasion/metastasis of tumor cells, and where over-production of the ECM often leads to fibrosis [1]. It seems conceivable that monitoring of the process of matrix remodeling offers possibilities for diagnosis, surveillance, and possibly even treatment of the associated diseases. For clinical applications, such as biomedical imaging or therapy, a cell-associated target protein with a central role within the ECM-remodeling process, but with limited expression in healthy tissue, would be helpful in identifying patient groups requiring more intensive monitoring or therapy. Furthermore, molecular imaging enables real-time imaging of pathophysiology, providing novel insights into disease processes that cannot be gathered with current techniques such as post-mortem tissue analysis or with animal models [2, 3].
Inherent to its nature, molecular imaging is fundamentally dependent on identifying appropriate targets that are informative about the underlying pathophysiology of the process studied [4]. As targeting different epitopes on the same protein may influence the ability to image specific processes, formal description of the epitope is crucial. Important to realize is that differing epitopes on the same protein can alter the results and consequently, describing the epitope of interest is just as crucial [5, 6]. Therefore, a key competence of targeted imaging is designing the best performing probe for the imaging modality of choice. The choices to be made are extensive and have already been covered in reviews elsewhere [7,8,9].
The urokinase plasminogen activator receptor (uPAR) holds a central position in ECM proteolysis, but, next to the proteolytic role, uPAR is also involved in cell-cell and cell-ECM interactions, regulating cell signaling and hereby controlling cell proliferation, differentiation, and migration [10]. uPAR is normally hardly found in healthy tissue, but it is present in virtually all human malignancies, associated with disease aggressiveness, allowing tumors to escape their original boundaries [11, 12]. As a result, the field of uPAR-based oncological imaging is progressing rapidly and, not surprisingly, various positron-emission tomography (PET)-based molecular imaging clinical trials are currently being conducted for diagnosing aggressive cancers and determining cancer aggressiveness (NCT02755675, NCT02945826, and NCT03307460) [13, 14].
The last two decades have revealed that uPAR is not only a central orchestrator in oncology but also in processes ranging from neurology to auto-immune diseases [15, 16]. Likewise, by unraveling the various (patho)physiological processes uPAR contributes to novel opportunities to diagnose, treat, or monitor diseases have been revealed. The current review aims to identify non-neoplastic diseases where uPAR is of pathophysiological relevance and elaborate on the molecular imaging opportunities this provides.
The urokinase plasminogen activator receptor: a central player in an extensive interactome
In 1985, uPAR was first identified on monocytes as the cell membrane receptor of the urokinase plasminogen activator (uPA) [17, 18]. In the following 35 years, uPAR has been identified, although often only expressed transiently, on, among others, fibroblasts, endothelial cells, epithelial cells, and neurons [11, 19]. Rather than being cell-specific, uPAR expression should be considered as process-specific with all cells being able to express uPAR, but only doing this at very specific events, such as the cell extravasation and migration observed during wound healing (Fig. 1a). Consequently, most cells at rest have no uPAR on their cell membrane [11]. A closer look at uPAR-expressing cells reveals that uPAR is implicated in multiple processes where the balance of this determines the end result (Fig. 1b).
The urokinase plasminogen activator receptor (uPAR). a While usually quiescent in normal tissue, uPAR expression is observed transiently and locally during specific cellular processes such as extravasation and migration by wound healing. b At a cellular level, uPAR interacts in a multitude of pathways where the balance of each dictates the end result. c uPAR itself is a three domain extracellular structure linked to the plasma membrane by a glycosylphosphatidylinositol (GPI) anchor. d Classically uPAR functions as receptor for urokinase plasminogen activator (uPA) which subsequently breaks down the extracellular matrix (ECM) via plasminogen activation. e Intracellular signaling occurs via other receptors including vitronectin and integrins and can be uPA dependent and independent. f Internalization and recycling of uPAR occurs after a uPAR/uPA/PAI-1/LRP-1 complex has formed, which results in the degradation of uPA and PAI-1 and the recycling of uPAR and LRP-1. g uPAR can be cleaved at the GPI-anchor and between D1 and D2 resulting in various isoforms of soluble uPAR which can be quantified in the blood. h After cleavage of D1, uPAR D2-D3 induces chemotaxis by interacting with formyl peptide receptor-like 1 (FPRL1)
To understand how uPAR can play such a diverse and central role, a careful examination of its structure needs to be made. uPAR is a 283 amino acid glycosylphosphatidylinositol (GPI)-anchored membrane protein consisting of three domains (D1-D3) linked by two flexible hinges (Fig. 1c) [20]. These three domains form a concave surface where uPA can bind [21]. Subsequently, uPAR mediates its other, non-proteolytic-related effects via protein interactions on the outer surface. D1 and the hinge region between D1 and D2 are vital for uPAR-vitronectin interactions, whereas various epitopes on D2-D3 interact with integrins, G protein-coupled receptors (GPCRs) and receptor tyrosine kinases like epidermal growth factor receptor, platelet-derived growth factor receptor, and insulin-like growth factor 1 receptor [22, 23]. With over 42 interacting proteins described, uPAR forms a central orchestrator of cell proliferation, differentiation, migration, and survival [10, 22].
Classically, the function of uPAR is fairly straightforward. Without intracellular or transmembrane domains, uPAR primarily functions as a receptor for (pro)uPA (Fig. 1d) [24]. uPA is a serine protease that catalyzes the activation of the ubiquitously present plasminogen into plasmin. Active plasmin degrades ECM proteins by itself or via activation of latent matrix metalloproteases (MMPs) [25]. Localization of both the inactive form, pro-uPA and active uPA to the cell surface, allows cells to focus extracellular matrix degradation toward the leading edge of the cell [26, 27]. However, this classic view of uPAR does not justify the many subtleties present in the uPAR interactome. For instance, the distinct central binding cavity of uPAR and the flexible hinges result in a conformational change after uPA binding that alters the vitronectin binding site, enhancing uPAR-vitronectin interaction on the outer surface of uPAR [23, 28,29,30]. Vice versa, vitronectin binding to uPAR influences the affinity for uPA [31]. Another subtlety of uPAR characteristics lies in the GPI anchoring to the cell, which influences distribution of uPAR toward lipid rafts and subsequently promotes specific protein-protein interactions [32,33,34]. Furthermore, GPI anchorage allows a rapid removal from the cell membrane, allowing a quick turnover and response time.
The intracellular signaling pathway initiated by uPAR, either enabled by uPA, with or without vitronectin, is still not entirely understood (Fig. 1e) [35,36,37,38,39]. On neutrophils and macrophages, CD11b/CD18 (MAC1, complement receptor 3 or αMβ2) colocalizes with uPAR and is essential for adhesion, migration, and phagocytosis [40,41,42,43,44,45,46,47]. In combination with the β1 integrin subunit, uPAR promotes differentiation, proliferation, adhesion, of epithelial and other cells and stimulates expression of uPA, uPAR, and MMPs, promoting extracellular proteolysis [38, 48,49,50,51,52,53,54]. Furthermore, β3-uPAR-mediated signaling enhances cell motility and invasion, while β6-uPAR interaction stimulates proliferation and cell differentiation [55,56,57,58].
Finally, recycling and cleavage of uPAR play an important role in cell functioning (Fig. 1f).
Plasminogen activator inhibitor-1 (PAI-1) and uPA are internalized for degradation via uPAR and lipoprotein receptor-related protein 1 interaction (LRP1) [59,60,61]. uPAR and LRP1 are recycled to the cell membrane ready for new interactions [62]. Cleavage of uPAR can occur at two sites: (I) within the GPI anchor by lipases, resulting in soluble uPAR (suPAR) and (II) between D1 and D2 resulting in cleaved uPAR (soluble D1 and soluble or membrane-bound D2-D3) (Fig. 1g) [63]. The exact function of full-length suPAR is unclear but suPAR might function as a scavenger protein for uPA, consequently competitively inhibiting cell surface proteolysis [64, 65]. Cleavage of D1 unveils an amino acid sequence (amino acids, 88-92) on D2-D3 that is unable to interact with integrins but interacts with GPCR formyl peptide receptor-like 1 (FPRL1), prompting migration (Fig. 1h) [66]. When cleaved, the same D2-D3 epitope induces chemotaxis in FPRL1-expressing cells [67, 68].
uPAR in cardiovascular disease: determining plaque instability in atherosclerosis
Although significant improvements have been made in the management of cardiovascular disease, it is still a leading cause of death worldwide [69]. The current state-of-art diagnostic techniques, such as angiography or perfusion imaging, can accurately identify stenosis location and luminal occlusion in order to guide revascularization, however, fail to determine risk of rupture [70, 71]. Identifying these patients is the next challenging frontier in cardiovascular disease research: more than 50% of patients who die suddenly have no evident clinical symptoms and autopsy studies indicate that the majority of myocardial infarctions are caused by non-flow limiting lesions [72,73,74]. Based on its mechanistic role, molecular imaging of uPAR expression status might be an alternative and more targeted tool to improve the recognition of atherosclerotic plaques and the risk of rupture.
Atherosclerosis is the formation of intimal plaques consisting of two interacting regions: a central core covered by a fibrous cap. Cholesterol filled monocyte-derived macrophage-foam cells form the core whereas the cap consists of vascular smooth muscle cells (VSMCs) that have been recruited from the media [75,76,77]. In both regions of the plaques, the urokinase plasminogen activation axis (uPA/uPAR/PAI-1 axis) has been shown pivotal for development and progression of the disease. Monocyte adherence and recruitment toward lesion sites are dependent on uPAR expression, and upon arrival in the lesion, uPA interaction with uPAR has been implicated in the differentiation of monocytes to macrophages, and cholesterol biosynthesis and subsequent lipid uptake (Fig. 2a, b) [78,79,80,81,82,83]. In response to vascular injury, VSMCs undergo a change from a physiological contractile phenotype to the pathological synthetic phenotype, allowing them to migrate, proliferate, and produce extracellular matrix, as found in the caps of atherosclerotic plaques. This process is stimulated by intimal macrophages-derived uPA binding to the uPAR present on VSMCs (Fig. 2c) [84,85,86,87,88,89,90,91,92,93]. Furthermore, uPAR expression upregulates the calcification of these lesions, although the consequences for plaque stability remain to be clarified [94, 95]. Overall, many in vitro mechanistic studies demonstrate the enhanced presence and pivotal role of uPAR in atherogenesis and negative (inward) remodeling [78, 92, 96]. These data are supported by various immunohistochemical studies on patients, which have clearly localized uPAR overexpression to atherosclerosis: while normal arterial tissue is negative for uPAR, intensely positive stained lymphocytes, macrophages, and intimal smooth muscle cells are found in atherosclerotic lesions and atheroma’s [93, 97,98,99,100,101]. Likewise, the overexpression of uPAR is confirmed in gene analysis with a 1.5 fold higher uPAR expression in endarterectomies [99]. The level of uPAR overexpression has been associated with disease severity and localized uPAR expression is indicative for areas at risk for rupture (Fig. 2d) [98, 99, 102].
uPAR in atherosclerosis. a Monocyte extravasation across the endothelium lesions is dependent on uPAR. b Upon interaction with uPA these monocytes differentiate into macrophages, eventually resulting in cholesterol filled monocyte-derived macrophages. c uPA released from macrophages interacts with uPAR on synthetic smooth muscle cells stimulating their migration. d Localized uPAR overexpression in an atherosclerotic plaque increases the risk of rupture. uPAR is represented by the red 3-domain structure as described in Fig. 1 on the cell membrane of uPAR expressing cells and uPA by the green structure in the extracellular matrix and bound to uPAR
As uPAR has been implicated in the pathophysiology of atherosclerosis, various studies have attempted to improve disease outcomes by targeting of uPAR to block its function. Viral and non-viral expression vectors, encoding constructs consisting of ATF (the amino-terminal fragment of urokinase with high affinity for uPAR) in combination with inhibitors of the plasminogen pathway like BPTI (bovine pancreas trypsin inhibitor) or of matrix metalloproteinases like TIMP1 (tissue inhibitor of matrix metalloproteinases 1), successfully inhibited neointimal formation, VSMC migration, and vein graft thickening in rodent models and human saphenous vein cultures [103,104,105,106]. Eventually, a construct consisting of all three of these proteins has been shown to lead to the strongest reduction in vein graft thickening in hypercholesterolemic mice [107]. While these preclinical studies show evident potential of uPAR as target for atherosclerosis targeting, the concept has not yet been progressed toward a clinical application neither for therapy nor for diagnostic monitoring via molecular targeted imaging.
uPAR in auto-immune disease: imaging disease activity in rheumatoid arthritis
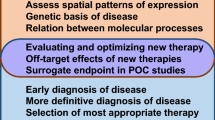
Rheumatoid arthritis (RA) is a chronic inflammatory disease with a lifetime risk of 3.6% for women and 1.7% for men [108]. Anatomical imaging techniques, such as conventional radiology, ultrasound, and magnetic resonance imaging, along with clinical criteria, are the standard to diagnose and monitor RA [109]. These modalities are able to identify RA as soon as 6-8 weeks after arthritis onset and sometimes even before the first clinical symptoms [110, 111]. Current research efforts lie in patient stratification according to disease severity and identifying responders to expensive novel biologicals [111]. Targeted molecular imaging might offer a solution for the current goals of identifying aggressive disease and treatment potential, providing a more reliable prognosis, evaluating/comparing new therapies, and providing new insights in the pathophysiology of RA [110, 112].
As RA progresses, the initially sparsely populated articular region becomes infiltrated with immune cells, neutrophils and monocytes/macrophages, fibroblast-like synoviocytes (FLS), and osteoclasts [113, 114]. The interaction of these cells directly with each other and via cytokines has many similarities with locally invasive malignancies, leading to chronic inflammation, and tissue invasion, remodeling, and destruction [113, 115]. In the RA microenvironment, FLS acquire the tumor-like characteristic of being able to escape growth limits, enhance migration and invasion, and to prompt angiogenesis [16]. The similarities between RA and cancer have led to the identification of commonly activated pathways with one being centered around uPAR.
RA manifestation in joints is defined by persistent synovial inflammation, where leukocytes from the innate and adaptive immune system infiltrate the synovial compartment and interact with present synoviocytes [116]. To support the influx, adhesion, and migration of cells into the synovial compartment, endothelial cells overexpress uPAR (Fig. 3a) [45, 117, 118]. However, uPAR expression is limited to endothelial cells. Neutrophils stimulate the inflammatory process through secretion of uPA and domain 2-3 of uPAR, whereby the latter probably functions as a chemoattractant for other formyl peptide receptor expressing leukocytes (Fig. 3b) [114, 118, 119]. The secreted uPA interacts in autocrine and paracrine fashion with uPAR on neutrophils, FLS, macrophages, and chondrocytes, enhancing the invasive and proliferative properties of these cells (Fig. 3c, d) [16, 115, 120,121,122,123,124,125,126,127,128,129,130,131]. The importance of uPAR has been confirmed by studies where knockdown of uPAR in FLS-inhibited proliferation, migration, and invasion in vitro [16]. Furthermore, compared to their wildtype littermates, PLAUR−/− mice show significant reduction of arthritis incidence and severity in a collagen-induced arthritis model [132]. However, an earlier study suggested that uPAR is not essential for RA development [133]. Induction of arthritis by intra-articular uPA injection is not dependent on the uPAR-binding fragment of uPA. Furthermore, the arthritis incidence is similar in PLAUR−/− mice and their genetic counterparts after uPA injection [133]. While this model results in joints with morphological features of arthritis, the question can be beckoned if intra-articular injection of uPA accurately reflects the etiology and progression of RA in humans.
uPAR in rheumatoid arthritis. a uPAR on neo-angiogenic endothelium support the influx of inflammatory cells. b Neutrophils secrete uPA and uPAR-D2/3 further escalating the inflammation. c The uPA interacts via autocrine and paracrine methods with neutrophils, fibroblast-like synoviocytes, macrophages and chondrocytes, activating invasive, and proliferative pathways in these cells. d uPAR on osteoclasts promotes bone destruction. uPAR is represented by the red 3-domain structure as described in Fig. 1 on the cell membrane of uPAR expressing cells and uPA by the green structure in the extracellular matrix and bound to uPAR
Besides influencing the inflammatory stage of RA, uPAR also attenuates the bone destruction occurring in late stage RA disease. Osteoclast differentiation, the subsequent bone destruction and bone mineral density (BMD), is significantly decreased in uPAR knockout mice and stimulated by uPAR overexpression [134]. With this knowledge in mind, loss of BMD has been successfully inhibited in a lipopolysaccharide-induced bone destruction mouse model using the uPAR targeting peptide (Ȧ6) [135].
The therapeutic possibilities by targeting uPAR in vivo have been investigated using uPAR antisense treatment and adenovirus-mediated gene transfer of the amino terminal fragment of uPA fused to human serum albumin. Both inhibit cartilage invasion while the latter also decreases both the incidence and severity of the disease [115, 136, 137]. However, blocking uPAR using the anti-uPAR monoclonal antibody mR1 in collagen-induced and delayed-type hypersensitivity arthritis models has no effect on RA progression [118]. This discrepancy can partly be explained by difference in methods (antisense vs. adenovirus vs. monoclonal antibody administration), targeting uPA vs. uPAR, and by the differences in models used.
While preclinical in vivo research is still inconclusive, several studies with clinically used agents have demonstrated that various treatment options for RA reach their effect by targeting the urokinase plasminogen activation pathway. Tenoxicam, a non-steroidal anti-inflammatory drug, has been shown to downregulate monocyte uPAR expression and hyaluronic acid treatment decreases the immunostaining for uPAR expression on FLS [122, 123]. Furthermore, the widely used corticosteroid deflazacort also modulates the urokinase pathway by inducing PAI-1 and inhibiting uPA and uPAR expression in RA FLS but not in healthy cells [138]. Physiologically, proliferation and invasion of RA FLS are inhibited by deflazacort. In addition, soluble uPAR levels correlate with response to biologicals such as the tumor necrosis factor (TNF)-inhibitor adalimumab [139].
All-in-all there is substantial evidence for the role of uPA/uPAR/PAI-1 axis in RA development and progression. Although future studies will need to confirm this, targeting uPAR for imaging purposes has the potential of providing relevant information on disease activity, prognosis, and treatment effect [140].
Central nervous system pathology: unraveling pathophysiology of degenerative disease
The nervous system, with the brain as its helm, is the most complex and pivotal system of the human body. Therefore, neurodegenerative disorders, such as Alzheimer’s disease (AD) and Creutzfeld-Jakob disease (CJD), auto-immune diseases, such as multiple sclerosis (MS), and infectious diseases, such as cerebral malaria (CM) and acquired immunodeficiency syndrome dementia complex (ADC), have disastrous consequences for patients. The emergence of molecular imaging has enabled more in-depth research into these pathologies as well as possibilities for diagnosis and monitoring of disease before clinical features occur [141,142,143,144].
While uPAR expression is very low, if not absent, in the adult brain, it plays a pivotal role in the developing brain (Fig. 4a) [15, 145]. In the early brain binding of uPA to uPAR stimulated neuritogenesis, neuronal migration, and differentiation via both proteolytic and nonproteolytic pathways resulting in axonal growth and branching of both the central and peripheral nerves [146,147,148,149,150]. The uPA/uPAR axis is of such importance that dysregulation has been implicated with epilepsy, schizophrenia, and autism. PLAUR, the gene encoding uPAR, and its promotor have been found to be upregulated in autistic patients [151, 152]. Furthermore, in rats, uPAR expression was increased in interneurons after spontaneous seizures [153]. On the other hand, uPAR−/− mice were more susceptible to seizures, increased anxiety, and altered social behavior; all characteristics of epilepsy, schizophrenia and autism [154, 155]. The discovery that uPAR functions as a receptor for SRPX2, an important regulator of synapse formation, and that both are co-located both spatially and temporally in the developing brain, further implicates uPAR’s role in the (patho)physiology of the nervous system. Although the actual function of SRPX2 remains to be elucidated, the Y72S mutation in SRPX2 leads to an almost sixfold increased affinity for uPAR, and clinically manifests in seizures, speech deficit, and mental retardation [156, 157].
uPAR in degenerative nervous system disorders. a uPAR expression is practically absent in the healthy human brain. In Alzheimer’s disease uPAR expression is found on (b) cortical neurons, (c) activated microglial cells after exposure to the amyloid plaques, and (d) in the vascular wall promoting uPA activation, subsequent extracellular matrix breakdown and corresponding spontaneous hemorrhages. In multiple sclerosis, uPAR (e) is expressed on inflammatory cells and activated microglial cells promoting local damage. f Furthermore, uPAR expression on dendritic cells influences subsequent T cell differentiation. uPAR is represented by the red 3-domain structure as described in Fig. 1 on the cell membrane of uPAR expressing cells and uPA by the green structure in the extracellular matrix and bound to uPAR
Various neurodegenerative diseases present with enhanced uPAR expression. AD is the leading cause of dementia and can be characterized pathologically as intracellular tangles and extracellular deposition of amyloid β creating senile plaques [158, 159]. uPAR expression has been found in both the cortical neurons and the vascular wall of AD patients (Fig. 4b) [19, 160,161,162]. Interestingly, the cerebellum, a region of the brain that is usually not affected by AD, is negative for uPAR in these patients [162]. Corresponding in vitro studies demonstrates that microglia upregulate uPAR mRNA and protein after exposure to aggregated amyloid β (Fig. 4c) [161, 162]. Furthermore, uPA and plasminogen activity is increased, which could lead to the vulnerability of the cerebral vessel wall due to extracellular matrix breakdown and corresponding spontaneous hemorrhages observed in AD (Fig. 4d) [161]. In CJD, another fatal degenerative disease with a mean survival of 7.3+/−0.2 months after clinical onset, significantly more neurons, primarily focused in cortical layer 3-5, express uPAR, where the expression has been associated with damaged neurons as seen by chromatin condensation, hypertrophic swelling, and degeneration [160, 163]. Microglial cells, but not astrocytes, also express uPAR [160].
MS is an autoimmune disease where an immune response is mounted against the central nervous system by autoreactive lymphocytes resulting in lesions that are characterized by inflammation, demyelination, and degeneration of neurons [164]. While autopsy material from healthy brains exhibits almost no uPAR expression, uPAR gene and protein expression are significantly elevated on MS microvessels, mononuclear cells, macrophages, pericytes, and smooth muscle cells [165,166,167,168,169]. Microglial cells cultured from an MS patient show an activated morphology in combination with high levels of uPAR, whereas control microglial cells from normal brain tissue express little to no uPAR mRNA and protein. After in vitro activation, these normal microglia present a spindle-shape morphology and express uPAR [170]. In an animal model of experimental autoimmune encephalomyelitis (EAE), elevated uPAR expression is detected in the inflammatory lesions by both immune and microglial cells (Fig. 4e) and increased uPA activity at the dorsal horn and central spinal cord [171, 172]. EAE in uPAR−/− mice is characterized by a delayed onset, chronicity, persisting inflammatory cuffs with increased levels of uPA and more extensive demyelination. The dysregulated adhesion and migration of inflammatory cells in uPAR−/− mice explains the delayed onset while the inability to recycle uPA via uPAR reflects the increased neuronal damage [173]. In a later study, uPAR−/− mice with EAE are shown to exhibit more severe disease with a twofold increase in microglial activation and increased infiltration of mononuclear cells but reduced immune response, rendering the mouse incapable of recovery [174]. The recently revealed crosstalk between the coagulation pathway (coagulation factor XII, FXII) and immunity in MS underlines the role of uPAR in this disease. uPAR on dendritic cells (Fig. 4f) is responsible for the immune modulatory function of FXII, tipping the balance of T cell differentiation toward the TH17 phenotype, as a signal receiver and relaying the message, via CD11b integrin, intracellularly (Fig. 4f) [175]. All-in-all, there is initial evidence that uPAR plays a fundamental role in MS, but whether uPAR expression is protective or destructive remains to be elucidated and, considering uPAR’s multifaceted aspects, could actually be both.
Various infectious diseases can have drastic neurological manifestations. ADC is one of the most severe consequences of human immunodeficiency virus 1 (HIV-1) infection [176]. The lesions showed membranous uPAR expression in immunohistochemical stainings that colocalized with HIV-1 p24 antigen in both macrophages, microglial, and multinucleated giant cells [177, 178]. Not coincidentally, soluble uPAR levels are a strong independent predictor for HIV-1 infection survival [179]. While combination antiretroviral therapy has successfully dropped the incidence of ADC from 20 to 5%, milder forms of HIV-associated neurocognitive disorder still occur with an incidence of 20-50% [176]. No study has evaluated uPAR in these cases. Plasmodium falciparum is another infectious agent that can lead to severe neurologic impairment with persistent neurocognitive deficits characterized as CM [180]. In post-mortem specimens of patients with CM uPAR expression, detected by immunohistochemical staining, of microglia, reactive astrocytes and endothelial cells is limited to areas with microvasculature containing parasitized erythrocytes, petechial bleedings and Dürck’s granulomas [181]. In the mouse model of CM, known as severe malaria (SM) as the syndrome in mice is not limited to the brain, uPAR deficiency has profound effect on thrombocytopenia. Platelet trapping, which is a reliable predictor of forthcoming death, does not occur in uPAR−/− mice [182]. The current theory holds that platelets form an adhesive surface in microvascular beds for parasitized erythrocytes in the cerebrum and consequently play a pivotal role in the development of CM [183].
While in most neurological disease processes, there is no clear indication whether uPAR expression is protective or destructive, the evidence currently accumulated suggests a critical role for uPAR in the pathophysiology of AD, MS, ADC, and MC. Grossly, aberrant uPAR expression is linked to an altered immune-phenotype, consequently altering the progressing of the disease. In addition to the post-mortem pathology and animal models, we are dependent on for research, an uPAR targeting tracer may enable in vivo imaging of the various pathophysiological processes going on in real-time and consequently enrich our understanding of these disease. This knowledge can potentially be used to dictate treatment and monitor disease based on uPAR signaling.
Inflammatory bowel disease: imaging macrophage polarization
Inflammatory bowel disease (IBD) is an umbrella term consisting of chronic relapsing inflammatory disorders of the intestinal tract. Ulcerative colitis (UC) characterizes itself as inflammation of the mucosal layer of the colon while Crohn’s disease (CD) displays transmural inflammation of any part of the gastrointestinal tract ranging from the mouth to the anus [184]. The current gold standard for diagnosis and surveillance of IBD is endoscopy and X-ray exams, but these techniques are limited by their invasiveness and patient tolerance. Molecular imaging might provide an opportunity for accurate non-invasive or endoscopic specification of IBD presence, transmural and extra-intestinal tissue involvement, and specific inflammatory profile [185,186,187,188]. While the etiology of IBD has not been fully elucidated yet, genetic, environmental, and immune factors have all been implicated.
The impaired immune response leads to extensive tissue remodeling and degradation in which the plasminogen activation cascade, including various MMPs and localized by uPAR, plays a major role [189,190,191,192]. Patients with active IBD have increased uPAR specific for macrophages at active lesions. Interestingly, uPAR D1-D3 is downregulated while uPAR D2-D3 is increased. In two different IBD mice models, uPAR expression has shown specific for CX3CR1+ macrophages and mirrored disease onset [193]. This subset of macrophages has an anti-inflammatory phenotype [194]. Therefore, knocking out uPAR exaggerates disease by amplifying the release of pro-inflammatory cytokines and altering polarization of macrophages. Low expression of uPAR D1-D3 and high expression of uPAR D2-3 by IBD patients can consequently lead to increased inflammation and disrupted bacterial removal (Fig. 5a, b) [193]. The therapeutic potential that targeting macrophages, and in extension uPAR, brings has not been unnoticed [195]. A cyclic peptide based of amino acids 88-92 of uPAR, [SRSRY], competed with uPAR for binding to FPRL1 but exerted an opposite effect: inhibiting migration as opposed to promoting it [196]. In vivo, [SRSRY], altered macrophage polarization and migration in colitis mice models and as such attenuated disease severity [197]. By competing with the migration sensitive epitope that becomes available after uPAR cleavage, [SRSRY], diminishes the destructive potential of uPAR D2-D3. While the research is still in its infancy, there is potential to determine macrophage polarization and disease progression by molecular imaging of uPAR. Determining the right epitope to direct the uPAR targeting moiety to, will be crucial for correct implementation and interpretation of uPAR-targeted molecular imaging in IBD as well as for other applications (Table 1). If addressed well, uPAR imaging has the potential to non-invasively diagnose IBD by identifying aberrant macrophage polarization and subsequently be used to monitor disease activity.
uPAR in inflammatory bowel disease. a Macrophage uPAR D1-D3 expression plays a significant role in the bacterial removal while (b) in inflammatory bowel disease macrophage differentiation is altered with as consequence an increase in uPAR D2-D3 expression and inadequate microbial maintenance. uPAR is represented by the red 3-domain structure as described in Fig. 1 on the cell membrane of uPAR expressing cells
uPAR imaging
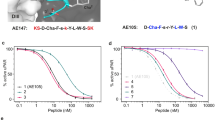
uPAR has been targeted for molecular imaging according by various approaches, each with its own advantages and disadvantages (Table 1, Fig. 6a). The first peptides targeting uPAR were ligand-based, utilizing the growth-factor domain of urokinase [215]. Targeting this natural interaction between uPA and uPAR with ATF or ATF-like constructs has been employed for magnetic-resonance imaging, near-infrared imaging, photo-acoustic imaging, and nuclear-imaging [198,199,200,201,202,203,204]. With a molecular weight of 18.5 kilodalton, ATF is cleared rapidly by the kidneys resulting in quick imaging times (30 min to 2 h) but also minimizing the time available to get sufficient contrast [216]. Conjugating ATF to nanoparticles (NPs) enhances blood circulation times resulting in optimal imaging times around 24-48 h after injection in vivo [198, 199, 202, 204]. Another advantage of ATF-NPs is their internalization, potentially increasing contrast [199, 200, 204]. Nonetheless, whether conjugated to a NP or not, uPAR targeting efficiency with ATF is dependent on the absence of endogenous urokinase on the majority of uPAR copies present and markedly reduced in models with high uPA expression [5, 201].
Targeting uPAR for molecular imaging. a Representation of binding domains of the uPAR imaging agents currently under development, their classification and suitable imaging modality. b Positive primary lesion with uPAR PET in human prostate cancer after injection of 64Cu-DOTA-AE105. Images adapted from Skovgaard et al. [218] and used under the terms of the Creative Commons CC BY license. c NIR optical imaging of orthotopic colon cancer with hybrid ATN-658
An alternative uses a 9-mer peptide which has led to the first uPAR PET clinical trials. This peptide, AE105, is the refined version of a 15-mer peptide identified by a phage display with uPAR-transfected cell lines and binds uPAR at the uPA-binding site in a species specific manner, like ATF [217, 218]. While AE105 has also been conjugated with (radio)-labels for single-photon emission computed tomography (SPECT) and near-infrared fluorescence (NIRF) in preclinical oncology studies, this section will focus on positron-emission tomography as AE105 PET is further along the clinical pipeline [205,206,207,208,209,210, 219, 220]. Initially, AE105 has been conjugated with the metal chelator DOTA and subsequently labeled with 64Cu. 64Cu-DOTA-AE105 specifically targets uPAR positive lesions in preclinical studies with signal corresponding to uPAR expression levels and epitope availability, but also resulted in high non-specific liver-uptake [221, 222]. Alternative 64Cu, 68Ga, and 18F tracer-chelator combinations decrease non-specific uptake but at the cost of lower tumor specific signal [223]. Phase I clinical trials with 64Cu-DOTA-AE105 have shown no adverse events or detectable pharmacological effects related to the tracer. Furthermore, all primary tumors (bladder, breast, and prostate) and the majority of metastasis are identifiable between 1 and 24 h after administration (Fig. 6b). In this study, two liver metastasis have not been visualized due to high background signal [13]. In addition, the feasibility of measuring mean 64Cu-DOTA-AE105 uptake in the arterial beds of these patients in order to non-invasively identify atherogenic lesions has been retrospectively evaluated [224]. While activated macrophages have higher uPAR expression, clear imaging capability of atherosclerosis has yet to be demonstrated with this tracer. The possibility to scan at early time points and the independence of 68Ga on an on-site cyclotron prompted to phase I trials of 68Ga-NOTA-AE105 [13, 14, 223]. 68Ga-Nota-AE105 resulted in decreased liver signal and specifically identified both primary tumors and one metastasis missed in the standard work up [14]. While initial clinical trial results are promising, allowing for rapid identification of cancerous lesions, endogenous uPA expression could present the biggest limiting factor of AE105 molecular imaging, especially in diseases where the expression of uPA is likely to be increased and paramount for outcomes [5, 225].
Another approach utilizes monoclonal antibodies to target uPAR. Both antibodies 2G10 and 3C6 are identified from a human fragment of the antigen binding (Fab) phage display library to have high affinities for uPAR. Consequently, these are expressed as recombinant IgG’s using the trastuzumab Fc domain [226]. 2G10 competes with uPA for uPAR binding while 3C6 prevents β1 integrin association with uPAR [211]. In human xenograft breast cancer models, 2G10 shows higher tumor uptake with NIRF and SPECT/CT than 3C6, probably due to higher epitope availability for 2G10 [212, 226]. Another thoroughly and extensively studied anti-uPAR antibody is ATN658. ATN658 was raised against a soluble D2-D3 uPAR fragment and recognizes domain 3 of uPAR, close to the C-terminus at amino acids 268-275 [47, 227]. ATN658 enables and anti-tumor effect by impairing α5β1 integrin adhesion to the ECM and is not effected by uPA or vitronectin interaction with uPAR [47, 228, 229]. In colorectal and oral xenograft cancer models NIRF and SPECT hybrid-labeled ATN658, accurately localized lesions as small as 1-2 mm in size in a range from 24 to 72 h post-injection (Fig. 6c) [213, 214]. ATN658 has been humanized and is awaiting clinical translation for NIRF-imaging [229].
A thorough assessment of the uPAR targeting agents reveals crucial differences in modalities, biodistributions, imaging windows, epitopes targeted, and production methods. Therefore, a one-size-fits-all solution to target all types of diseases where uPAR is involved is probably not feasible, like for most, if not all, molecular targets [5]. For instance, peptides may find their utility in more acute situations such as atherosclerosis imaging. Antibodies seem more ideal for abdominal imaging where the high non-specific background of kidneys can be a hindrance or in more elective settings where a large imaging window is desired. Not only will selecting an optimal agent be challenging, also designing and selecting preclinical animal models that take the species specificity of the imaging agents into account, since most tracers designed for clinical applications have high affinities for human uPAR but no or reduced affinities for mouse uPAR [201, 218, 226, 227].
Conclusions
uPAR is a central unit in regulating ECM proteolysis, migration, differentiation, and proliferation and hereby implicated in a range of inflammatory-related diseases, often holding pivotal roles and tipping the balance toward disease aggravation. Even though uPAR is almost completely absent in normal tissue, it will likely not be an appropriate target for the diagnosis of diseases, due to the common pathophysiological role. However, when it comes to visualization of diagnosed disease lesions, whether it be plaques that are about to rupture or aggravation of RA or IBD, uPAR plays a central pathophysiological role prompting its usefulness as a molecular imaging target. Furthermore, molecular imaging of uPAR can unravel the complex pathophysiological processes occurring, increasing our understanding of the disease, and consequently allowing the development of novel therapies, ultimately improving patient outcomes.
Availability of data and materials
Not applicable.
Abbreviations
- AD:
-
Alzheimer’s disease
- ADC:
-
Acquired immunodeficiency syndrome dementia complex
- ATF:
-
Amino-terminal fragment of urokinase
- BMD:
-
Bone mineral density
- BPTI:
-
Bovine pancreas trypsin inhibitor
- CD:
-
Crohn’s disease
- CJD:
-
Creutzfeld-Jakob disease
- CM:
-
Cerebral malaria
- D:
-
Domain: D1, D2, D3, D1-3, D1-2, D2-3
- ECM:
-
Extracellular matrix
- FLS:
-
Fibroblast-like synoviocytes
- FPRL1:
-
Formyl peptide receptor-like 1
- GPI:
-
Glycosylphosphatidylinositol
- GPCR:
-
G protein-coupled receptors
- HIV-1:
-
Human immunodeficiency virus 1
- IBD:
-
Inflammatory bowel disease
- LRP1:
-
Lipoprotein receptor-related protein 1
- MMP:
-
Matrix metalloprotease
- MS:
-
Multiple sclerosis
- NIRF:
-
Near-infrared fluorescence
- NP:
-
Nanoparticle
- PAI-1:
-
Plasminogen activator inhibitor type 1
- PET:
-
Positron emission tomography
- RA:
-
Rheumatoid arthritis
- SM:
-
Severe malaria
- SPECT:
-
Single-photon emission computed tomography
- TIMP1:
-
Tissue inhibitor of matrix metalloproteinases 1
- TNF:
-
Tumor necrosis factor
- UC:
-
Ulcerative colitis
- uPA:
-
Urokinase plasminogen activator
- uPAR:
-
Urokinase plasminogen activator receptor
- VSMC:
-
Vascular smooth muscle cell
References
Bonnans C, Chou J, Werb Z. Remodelling the extracellular matrix in development and disease. Nat Rev Mol Cell Biol. 2014;15:786–801. https://doi.org/10.1038/nrm3904.
Hamburg MA, Collins FS. The path to personalized medicine. N Engl J Med. 2010;363:301–4. https://doi.org/10.1056/NEJMp1006304.
Jung KH, Lee KH. Molecular imaging in the era of personalized medicine. J Pathol Trans Med. 2015;49:5–12. https://doi.org/10.4132/jptm.2014.10.24.
Herschman HR. Molecular imaging: looking at problems, seeing solutions. Science (New York, NY). 2003;302:605–8. https://doi.org/10.1126/science.1090585.
Baart VM, Boonstra MC, Sier CFM. uPAR directed-imaging of head-and-neck cancer. Oncotarget. 2017;8:20519–20. https://doi.org/10.18632/oncotarget.16240.
Ahn SB, Chan C, Dent OF, Mohamedali A, Kwun SY, Clarke C, et al. Epithelial and stromal cell urokinase plasminogen activator receptor expression differentially correlates with survival in rectal cancer stages B and C patients. PLoS One. 2015;10:e0117786. https://doi.org/10.1371/journal.pone.0117786.
Willmann JK, van Bruggen N, Dinkelborg LM, Gambhir SS. Molecular imaging in drug development. Nat Rev Drug Discov. 2008;7:591–607. https://doi.org/10.1038/nrd2290.
Chen K, Chen X. Design and development of molecular imaging probes. Curr Top Med Chem. 2010;10:1227–36. https://doi.org/10.2174/156802610791384225.
Boonstra MC, de Geus SW, Prevoo HA, Hawinkels LJ, van de Velde CJ, Kuppen PJ, et al. Selecting targets for tumor imaging: an overview of cancer-associated membrane proteins. Biomarkers in cancer. 2016;8:119–33. https://doi.org/10.4137/bic.S38542.
Smith HW, Marshall CJ. Regulation of cell signalling by uPAR. Nat Rev Mol Cell Biol. 2010;11:23–36. https://doi.org/10.1038/nrm2821.
Boonstra MC, Verspaget HW, Ganesh S, Kubben FJ, Vahrmeijer AL, van de Velde CJ, et al. Clinical applications of the urokinase receptor (uPAR) for cancer patients. Curr Pharm Des. 2011;17:1890–910. https://doi.org/10.2174/138161211796718233.
Mahmood N, Mihalcioiu C, Rabbani SA. Multifaceted role of the urokinase-type plasminogen activator (uPA) and its receptor (uPAR): diagnostic, prognostic, and therapeutic applications. Front Oncol. 2018;8:24. https://doi.org/10.3389/fonc.2018.00024.
Persson M, Skovgaard D, Brandt-Larsen M, Christensen C, Madsen J, Nielsen CH, et al. First-in-human uPAR PET: imaging of cancer aggressiveness. Theranostics. 2015;5:1303–16. https://doi.org/10.7150/thno.12956.
Skovgaard D, Persson M, Brandt-Larsen M, Christensen C, Madsen J, Klausen TL, et al. Safety, dosimetry, and tumor detection ability of (68)Ga-NOTA-AE105: first-in-human study of a novel radioligand for uPAR PET imaging. J Nucl Med. 2017;58:379–86. https://doi.org/10.2967/jnumed.116.178970.
Bruneau N, Szepetowski P. The role of the urokinase receptor in epilepsy, in disorders of language, cognition, communication and behavior, and in the central nervous system. Curr Pharm Des. 2011;17:1914–23. https://doi.org/10.2174/138161211796718198.
Liu Y, Pan YF, Xue YQ, Fang LK, Guo XH, Guo X, et al. uPAR promotes tumor-like biologic behaviors of fibroblast-like synoviocytes through PI3K/Akt signaling pathway in patients with rheumatoid arthritis. Cell Mol Immunol. 2018;15:171–81. https://doi.org/10.1038/cmi.2016.60.
Stoppelli MP, Corti A, Soffientini A, Cassani G, Blasi F, Assoian RK. Differentiation-enhanced binding of the amino-terminal fragment of human urokinase plasminogen activator to a specific receptor on U937 monocytes. Proc Natl Acad Sci U S A. 1985;82:4939–43. https://doi.org/10.1073/pnas.82.15.4939.
Vassalli JD, Baccino D, Belin D. A cellular binding site for the Mr 55,000 form of the human plasminogen activator, urokinase. J Cell Biol. 1985;100:86–92. https://doi.org/10.1083/jcb.100.1.86.
Asahina M, Yoshiyama Y, Hattori T. Expression of matrix metalloproteinase-9 and urinary-type plasminogen activator in Alzheimer’s disease brain. Clin Neuropathol. 2001;20:60–3.
Ploug M, Ellis V. Structure-function relationships in the receptor for urokinase-type plasminogen activator. Comparison to other members of the Ly-6 family and snake venom alpha-neurotoxins. FEBS Lett. 1994;349:163–8. https://doi.org/10.1016/0014-5793(94)00674-1.
Huai Q, Mazar AP, Kuo A, Parry GC, Shaw DE, Callahan J, et al. Science (New York, NY). 2006;311:656–9. https://doi.org/10.1126/science.1121143.
Eden G, Archinti M, Furlan F, Murphy R, Degryse B. The urokinase receptor interactome. Curr Pharm Des. 2011;17:1874–89. https://doi.org/10.2174/138161211796718215.
Huai Q, Zhou A, Lin L, Mazar AP, Parry GC, Callahan J, et al. Crystal structures of two human vitronectin, urokinase and urokinase receptor complexes. Nat Struct Mol Biol. 2008;15:422–3. https://doi.org/10.1038/nsmb.1404.
Ploug M, Ronne E, Behrendt N, Jensen AL, Blasi F, Dano K. Cellular receptor for urokinase plasminogen activator. Carboxyl-terminal processing and membrane anchoring by glycosyl-phosphatidylinositol. J Biol Chem. 1991;266:1926–33.
Mondino A, Blasi F. uPA and uPAR in fibrinolysis, immunity and pathology. Trends Immunol. 2004;25:450–5. https://doi.org/10.1016/j.it.2004.06.004.
Ellis V, Behrendt N, Dano K. Plasminogen activation by receptor-bound urokinase. A kinetic study with both cell-associated and isolated receptor. J Biol Chem. 1991;266:12752–8.
Vassalli JD, Wohlwend A, Belin D. Urokinase-catalyzed plasminogen activation at the monocyte/macrophage cell surface: a localized and regulated proteolytic system. Curr Top Microbiol Immunol. 1992;181:65–86. https://doi.org/10.1007/978-3-642-77377-8_3.
Wei Y, Waltz DA, Rao N, Drummond RJ, Rosenberg S, Chapman HA. Identification of the urokinase receptor as an adhesion receptor for vitronectin. J Biol Chem. 1994;269:32380–8.
Barinka C, Parry G, Callahan J, Shaw DE, Kuo A, Bdeir K, et al. Structural basis of interaction between urokinase-type plasminogen activator and its receptor. J Mol Biol. 2006;363:482–95. https://doi.org/10.1016/j.jmb.2006.08.063.
Gardsvoll H, Jacobsen B, Kriegbaum MC, Behrendt N, Engelholm L, Ostergaard S, et al. Conformational regulation of urokinase receptor function: impact of receptor occupancy and epitope-mapped monoclonal antibodies on lamellipodia induction. J Biol Chem. 2011;286:33544–56. https://doi.org/10.1074/jbc.M111.220087.
Zhao B, Gandhi S, Yuan C, Luo Z, Li R, Gardsvoll H, et al. Stabilizing a flexible interdomain hinge region harboring the SMB binding site drives uPAR into its closed conformation. J Mol Biol. 2015;427:1389–403. https://doi.org/10.1016/j.jmb.2015.01.022.
Cunningham O, Andolfo A, Santovito ML, Iuzzolino L, Blasi F, Sidenius N. Dimerization controls the lipid raft partitioning of uPAR/CD87 and regulates its biological functions. EMBO J. 2003;22:5994–6003. https://doi.org/10.1093/emboj/cdg588.
Caiolfa VR, Zamai M, Malengo G, Andolfo A, Madsen CD, Sutin J, et al. Monomer dimer dynamics and distribution of GPI-anchored uPAR are determined by cell surface protein assemblies. J Cell Biol. 2007;179:1067–82. https://doi.org/10.1083/jcb.200702151.
Gaus K, Le Lay S, Balasubramanian N, Schwartz MA. Integrin-mediated adhesion regulates membrane order. J Cell Biol. 2006;174:725–34. https://doi.org/10.1083/jcb.200603034.
Madsen CD, Ferraris GM, Andolfo A, Cunningham O, Sidenius N. uPAR-induced cell adhesion and migration: vitronectin provides the key. J Cell Biol. 2007;177:927–39. https://doi.org/10.1083/jcb.200612058.
Degryse B, Resnati M, Czekay RP, Loskutoff DJ, Blasi F. Domain 2 of the urokinase receptor contains an integrin-interacting epitope with intrinsic signaling activity: generation of a new integrin inhibitor. J Biol Chem. 2005;280:24792–803. https://doi.org/10.1074/jbc.M413954200.
Chaurasia P, Aguirre-Ghiso JA, Liang OD, Gardsvoll H, Ploug M, Ossowski L. A region in urokinase plasminogen receptor domain III controlling a functional association with alpha5beta1 integrin and tumor growth. J Biol Chem. 2006;281:14852–63. https://doi.org/10.1074/jbc.M512311200.
Tang CH, Hill ML, Brumwell AN, Chapman HA, Wei Y. Signaling through urokinase and urokinase receptor in lung cancer cells requires interactions with beta1 integrins. J Cell Sci. 2008;121:3747–56. https://doi.org/10.1242/jcs.029769.
Grove LM, Southern BD, Jin TH, White KE, Paruchuri S, Harel E, et al. Urokinase-type plasminogen activator receptor (uPAR) ligation induces a raft-localized integrin signaling switch that mediates the hypermotile phenotype of fibrotic fibroblasts. J Biol Chem. 2014;289:12791–804. https://doi.org/10.1074/jbc.M113.498576.
May AE, Kanse SM, Lund LR, Gisler RH, Imhof BA, Preissner KT. Urokinase receptor (CD87) regulates leukocyte recruitment via beta 2 integrins in vivo. J Exp Med. 1998;188:1029–37. https://doi.org/10.1084/jem.188.6.1029.
Simon DI, Rao NK, Xu H, Wei Y, Majdic O, Ronne E, et al. Mac-1 (CD11b/CD18) and the urokinase receptor (CD87) form a functional unit on monocytic cells. Blood. 1996;88:3185–94.
Sitrin RG, Todd RF 3rd, Albrecht E, Gyetko MR. The urokinase receptor (CD87) facilitates CD11b/CD18-mediated adhesion of human monocytes. J Clin Invest. 1996;97:1942–51. https://doi.org/10.1172/jci118626.
Ross GD. Role of the lectin domain of mac-1/CR3 (CD11b/CD18) in regulating intercellular adhesion. Immunol Res. 2002;25:219–27. https://doi.org/10.1385/ir:25:3:219.
Simon DI, Wei Y, Zhang L, Rao NK, Xu H, Chen Z, et al. Identification of a urokinase receptor-integrin interaction site. Promiscuous regulator of integrin function. J Biol Chem. 2000;275:10228–34. https://doi.org/10.1074/jbc.275.14.10228.
Pliyev BK, Antonova OA, Menshikov M. Participation of the urokinase-type plasminogen activator receptor (uPAR) in neutrophil transendothelial migration. Mol Immunol. 2011;48:1168–77. https://doi.org/10.1016/j.molimm.2011.02.011.
Pliyev BK, Arefieva TI, Menshikov MY. Urokinase receptor (uPAR) regulates complement receptor 3 (CR3)-mediated neutrophil phagocytosis. Biochem Biophys Res Commun. 2010;397:277–82. https://doi.org/10.1016/j.bbrc.2010.05.100.
Xu X, Cai Y, Wei Y, Donate F, Juarez J, Parry G, et al. Identification of a new epitope in uPAR as a target for the cancer therapeutic monoclonal antibody ATN-658, a structural homolog of the uPAR binding integrin CD11b (alphaM). PLoS One. 2014;9:e85349. https://doi.org/10.1371/journal.pone.0085349.
Aguirre-Ghiso JA, Liu D, Mignatti A, Kovalski K, Ossowski L. Urokinase receptor and fibronectin regulate the ERK(MAPK) to p38(MAPK) activity ratios that determine carcinoma cell proliferation or dormancy in vivo. Mol Biol Cell. 2001;12:863–79. https://doi.org/10.1091/mbc.12.4.863.
Aguirre Ghiso JA, Kovalski K, Ossowski L. Tumor dormancy induced by downregulation of urokinase receptor in human carcinoma involves integrin and MAPK signaling. J Cell Biol. 1999;147:89–104. https://doi.org/10.1083/jcb.147.1.89.
Ghosh S, Johnson JJ, Sen R, Mukhopadhyay S, Liu Y, Zhang F, et al. Functional relevance of urinary-type plasminogen activator receptor-alpha3beta1 integrin association in proteinase regulatory pathways. J Biol Chem. 2006;281:13021–9. https://doi.org/10.1074/jbc.M508526200.
Wei Y, Tang CH, Kim Y, Robillard L, Zhang F, Kugler MC, et al. Urokinase receptors are required for alpha 5 beta 1 integrin-mediated signaling in tumor cells. J Biol Chem. 2007;282:3929–39. https://doi.org/10.1074/jbc.M607989200.
Wei Y, Czekay RP, Robillard L, Kugler MC, Zhang F, Kim KK, et al. Regulation of alpha5beta1 integrin conformation and function by urokinase receptor binding. J Cell Biol. 2005;168:501–11. https://doi.org/10.1083/jcb.200404112.
Ferraris GM, Schulte C, Buttiglione V, De Lorenzi V, Piontini A, Galluzzi M, et al. The interaction between uPAR and vitronectin triggers ligand-independent adhesion signalling by integrins. EMBO J. 2014;33:2458–72. https://doi.org/10.15252/embj.201387611.
Margheri F, Luciani C, Taddei ML, Giannoni E, Laurenzana A, Biagioni A, et al. The receptor for urokinase-plasminogen activator (uPAR) controls plasticity of cancer cell movement in mesenchymal and amoeboid migration style. Oncotarget. 2014;5:1538–53. https://doi.org/10.18632/oncotarget.1754.
Smith HW, Marra P, Marshall CJ. uPAR promotes formation of the p130Cas-Crk complex to activate Rac through DOCK180. J Cell Biol. 2008;182:777–90. https://doi.org/10.1083/jcb.200712050.
Adachi Y, Lakka SS, Chandrasekar N, Yanamandra N, Gondi CS, Mohanam S, et al. Down-regulation of integrin alpha(v)beta(3) expression and integrin-mediated signaling in glioma cells by adenovirus-mediated transfer of antisense urokinase-type plasminogen activator receptor (uPAR) and sense p16 genes. J Biol Chem. 2001;276:47171–7. https://doi.org/10.1074/jbc.M104334200.
Xiong JP, Mahalingham B, Alonso JL, Borrelli LA, Rui X, Anand S, et al. Crystal structure of the complete integrin alphaVbeta3 ectodomain plus an alpha/beta transmembrane fragment. J Cell Biol. 2009;186:589–600. https://doi.org/10.1083/jcb.200905085.
Ahn SB, Mohamedali A, Anand S, Cheruku HR, Birch D, Sowmya G, et al. Characterization of the interaction between heterodimeric alphavbeta6 integrin and urokinase plasminogen activator receptor (uPAR) using functional proteomics. J Proteome Res. 2014;13:5956–64. https://doi.org/10.1021/pr500849x.
Conese M, Nykjaer A, Petersen CM, Cremona O, Pardi R, Andreasen PA, et al. Alpha-2 macroglobulin receptor/Ldl receptor-related protein(Lrp)-dependent internalization of the urokinase receptor. J Cell Biol. 1995;131:1609–22. https://doi.org/10.1083/jcb.131.6.1609.
Czekay RP, Kuemmel TA, Orlando RA, Farquhar MG. Direct binding of occupied urokinase receptor (uPAR) to LDL receptor-related protein is required for endocytosis of uPAR and regulation of cell surface urokinase activity. Mol Biol Cell. 2001;12:1467–79. https://doi.org/10.1091/mbc.12.5.1467.
Degryse B, Sier CF, Resnati M, Conese M, Blasi F. PAI-1 inhibits urokinase-induced chemotaxis by internalizing the urokinase receptor. FEBS Lett. 2001;505:249–54. https://doi.org/10.1016/s0014-5793(01)02797-1.
Nykjaer A, Conese M, Christensen EI, Olson D, Cremona O, Gliemann J, et al. Recycling of the urokinase receptor upon internalization of the uPA: serpin complexes. EMBO J. 1997;16:2610–20. https://doi.org/10.1093/emboj/16.10.2610.
Sidenius N, Sier CF, Blasi F. Shedding and cleavage of the urokinase receptor (uPAR): identification and characterisation of uPAR fragments in vitro and in vivo. FEBS Lett. 2000;475:52–6. https://doi.org/10.1016/s0014-5793(00)01624-0.
Wilhelm O, Weidle U, Hohl S, Rettenberger P, Schmitt M, Graeff H. Recombinant soluble urokinase receptor as a scavenger for urokinase-type plasminogen activator (uPA). Inhibition of proliferation and invasion of human ovarian cancer cells. FEBS Lett. 1994;337:131–4. https://doi.org/10.1016/0014-5793(94)80259-9.
Thuno M, Macho B, Eugen-Olsen J. suPAR: the molecular crystal ball. Dis Markers. 2009;27:157–72. https://doi.org/10.3233/dma-2009-0657.
Montuori N, Carriero MV, Salzano S, Rossi G, Ragno P. The cleavage of the urokinase receptor regulates its multiple functions. J Biol Chem. 2002;277:46932–9. https://doi.org/10.1074/jbc.M207494200.
Resnati M, Pallavicini I, Wang JM, Oppenheim J, Serhan CN, Romano M, et al. The fibrinolytic receptor for urokinase activates the G protein-coupled chemotactic receptor FPRL1/LXA4R. Proc Natl Acad Sci U S A. 2002;99:1359–64. https://doi.org/10.1073/pnas.022652999.
de Paulis A, Montuori N, Prevete N, Fiorentino I, Rossi FW, Visconte V, et al. Urokinase induces basophil chemotaxis through a urokinase receptor epitope that is an endogenous ligand for formyl peptide receptor-like 1 and -like 2. J Immun (Baltimore, Md: 1950). 2004;173:5739–48. https://doi.org/10.4049/jimmunol.173.9.5739.
Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139:e56–e528. https://doi.org/10.1161/cir.0000000000000659.
Tavakoli S, Vashist A, Sadeghi MM. Molecular imaging of plaque vulnerability. J Nucl Cardiol. 2014;21:1112–28quiz 29. https://doi.org/10.1007/s12350-014-9959-4.
Anwaier G, Chen C, Cao Y, Qi R. A review of molecular imaging of atherosclerosis and the potential application of dendrimer in imaging of plaque. Int J Nanomedicine. 2017;12:7681–93. https://doi.org/10.2147/ijn.s142385.
Virmani R, Burke AP, Farb A, Kolodgie FD. Pathology of the vulnerable plaque. J Am Coll Cardiol. 2006;47:C13–8. https://doi.org/10.1016/j.jacc.2005.10.065.
Tarkin JM, Dweck MR, Evans NR, Takx RA, Brown AJ, Tawakol A, et al. Imaging atherosclerosis. Circ Res. 2016;118:750–69. https://doi.org/10.1161/circresaha.115.306247.
Bala G, Broisat A, Lahoutte T, Hernot S. Translating molecular imaging of the vulnerable plaque-a vulnerable project? Mol Imaging and Biology. 2018;20:337–9. https://doi.org/10.1007/s11307-017-1147-x.
Rafieian-Kopaei M, Setorki M, Doudi M, Baradaran A, Nasri H. Atherosclerosis: process, indicators, risk factors and new hopes. Int J Prev Med. 2014;5:927–46.
Weber C, Noels H. Atherosclerosis: current pathogenesis and therapeutic options. Nat Med. 2011;17:1410–22. https://doi.org/10.1038/nm.2538.
Fuhrman B. The urokinase system in the pathogenesis of atherosclerosis. Atherosclerosis. 2012;222:8–14. https://doi.org/10.1016/j.atherosclerosis.2011.10.044.
Larmann J, Jurk K, Janssen H, Muller M, Herzog C, Lorenz A, et al. Hepatic overexpression of soluble urokinase receptor (uPAR) suppresses diet-induced atherosclerosis in low-density lipoprotein receptor-deficient (LDLR-/-) mice. PLoS One. 2015;10:e0131854. https://doi.org/10.1371/journal.pone.0131854.
May AE, Schmidt R, Kanse SM, Chavakis T, Stephens RW, Schomig A, et al. Urokinase receptor surface expression regulates monocyte adhesion in acute myocardial infarction. Blood. 2002;100:3611–7. https://doi.org/10.1182/blood-2002-03-0778.
Gu JM, Johns A, Morser J, Dole WP, Greaves DR, Deng GG. Urokinase plasminogen activator receptor promotes macrophage infiltration into the vascular wall of ApoE deficient mice. J Cell Physiol. 2005;204:73–82. https://doi.org/10.1002/jcp.20262.
Fuhrman B, Nitzan O, Karry R, Volkova N, Dumler I, Aviram M. Urokinase plasminogen activator (uPA) stimulates cholesterol biosynthesis in macrophages through activation of SREBP-1 in a PI3-kinase and MEK-dependent manner. Atherosclerosis. 2007;195:e108–16. https://doi.org/10.1016/j.atherosclerosis.2007.06.025.
Ohwaki K, Bujo H, Jiang M, Yamazaki H, Schneider WJ, Saito Y. A secreted soluble form of LR11, specifically expressed in intimal smooth muscle cells, accelerates formation of lipid-laden macrophages. Arterioscler Thromb Vasc Biol. 2007;27:1050–6. https://doi.org/10.1161/atvbaha.106.137091.
Yu H, Maurer F, Medcalf RL. Plasminogen activator inhibitor type 2: a regulator of monocyte proliferation and differentiation. Blood. 2002;99:2810–8. https://doi.org/10.1182/blood.v99.8.2810.
Mukhina S, Stepanova V, Traktouev D, Poliakov A, Beabealashvilly R, Gursky Y, et al. The chemotactic action of urokinase on smooth muscle cells is dependent on its kringle domain. Characterization of interactions and contribution to chemotaxis. J Biol Chem. 2000;275:16450–8. https://doi.org/10.1074/jbc.M909080199.
Stepanova V, Jerke U, Sagach V, Lindschau C, Dietz R, Haller H, et al. Urokinase-dependent human vascular smooth muscle cell adhesion requires selective vitronectin phosphorylation by ectoprotein kinase CK2. J Biol Chem. 2002;277:10265–72. https://doi.org/10.1074/jbc.M109057200.
Kunigal S, Kusch A, Tkachuk N, Tkachuk S, Jerke U, Haller H, et al. Monocyte-expressed urokinase inhibits vascular smooth muscle cell growth by activating Stat1. Blood. 2003;102:4377–83. https://doi.org/10.1182/blood-2002-12-3872.
Kusch A, Tkachuk S, Lutter S, Haller H, Dietz R, Lipp M, et al. Monocyte-expressed urokinase regulates human vascular smooth muscle cell migration in a coculture model. Biol Chem. 2002;383:217–21. https://doi.org/10.1515/bc.2002.022.
Kiyan Y, Tkachuk S, Hilfiker-Kleiner D, Haller H, Fuhrman B, Dumler I. oxLDL induces inflammatory responses in vascular smooth muscle cells via urokinase receptor association with CD36 and TLR4. J Mol Cell Cardiol. 2014;66:72–82. https://doi.org/10.1016/j.yjmcc.2013.11.005.
Kiyan Y, Limbourg A, Kiyan R, Tkachuk S, Limbourg FP, Ovsianikov A, et al. Urokinase receptor associates with myocardin to control vascular smooth muscle cells phenotype in vascular disease. Arterioscler Thromb Vasc Biol. 2012;32:110–22. https://doi.org/10.1161/atvbaha.111.234369.
Vallabhaneni KC, Tkachuk S, Kiyan Y, Shushakova N, Haller H, Dumler I, et al. Urokinase receptor mediates mobilization, migration, and differentiation of mesenchymal stem cells. Cardiovasc Res. 2011;90:113–21. https://doi.org/10.1093/cvr/cvq362.
Kiyan J, Smith G, Haller H, Dumler I. Urokinase-receptor-mediated phenotypic changes in vascular smooth muscle cells require the involvement of membrane rafts. Biochem J. 2009;423:343–51. https://doi.org/10.1042/bj20090447.
Kiyan J, Kusch A, Tkachuk S, Kramer J, Haller H, Dietz R, et al. Rosuvastatin regulates vascular smooth muscle cell phenotypic modulation in vascular remodeling: role for the urokinase receptor. Atherosclerosis. 2007;195:254–61. https://doi.org/10.1016/j.atherosclerosis.2006.12.030.
Noda-Heiny H, Daugherty A, Sobel BE. Augmented urokinase receptor expression in atheroma. Arterioscler Thromb Vasc Biol. 1995;15:37–43.
Kalbasi Anaraki P, Patecki M, Tkachuk S, Kiyan Y, Haller H, Dumler I. Urokinase receptor mediates osteoclastogenesis via M-CSF release from osteoblasts and the c-Fms/PI3K/Akt/NF-kappaB pathway in osteoclasts. J Bone Min Res. 2015;30:379–88. https://doi.org/10.1002/jbmr.2350.
Kalbasi Anaraki P, Patecki M, Larmann J, Tkachuk S, Jurk K, Haller H, et al. Urokinase receptor mediates osteogenic differentiation of mesenchymal stem cells and vascular calcification via the complement C5a receptor. Stem Cells Dev. 2014;23:352–62. https://doi.org/10.1089/scd.2013.0318.
Farris SD, Hu JH, Krishnan R, Emery I, Chu T, Du L, et al. Mechanisms of urokinase plasminogen activator (uPA)-mediated atherosclerosis: role of the uPA receptor and S100A8/A9 proteins. J Biol Chem. 2011;286:22665–77. https://doi.org/10.1074/jbc.M110.202135.
Salame MY, Samani NJ. Masood I, deBono DP. Expression of the plasminogen activator system in the human vascular wall. Atherosclerosis. 2000;152:19–28. https://doi.org/10.1016/s0021-9150(99)00441-4.
Svensson PA, Olson FJ, Hagg DA, Ryndel M, Wiklund O, Karlstrom L, et al. Urokinase-type plasminogen activator receptor is associated with macrophages and plaque rupture in symptomatic carotid atherosclerosis. Int J Mol Med. 2008;22:459–64.
Chen W, Jin WQ, Chen LF, Williams T, Zhu WL, Fang Q. Urokinase receptor surface expression regulates monocyte migration and is associated with accelerated atherosclerosis. Int J Cardiol. 2012;161:103–10. https://doi.org/10.1016/j.ijcard.2011.12.094.
Raghunath PN, Tomaszewski JE, Brady ST, Caron RJ, Okada SS, Barnathan ES. Plasminogen activator system in human coronary atherosclerosis. Arterioscler Thromb Vasc Biol. 1995;15:1432–43.
Okada SS, Golden MA, Raghunath PN, Tomaszewski JE, David ML, Kuo A, et al. Native atherosclerosis and vein graft arterialization: association with increased urokinase receptor expression in vitro and in vivo. Thromb Haemost. 1998;80:140–7.
Steins MB, Padro T, Schwaenen C, Ruiz S, Mesters RM, Berdel WE, et al. Overexpression of urokinase receptor and cell surface urokinase-type plasminogen activator in the human vessel wall with different types of atherosclerotic lesions. Blood Coagul Fibrinolysis. 2004;15:383–91.
Quax PH, Lamfers ML, Lardenoye JH, Grimbergen JM, de Vries MR, Slomp J, et al. Adenoviral expression of a urokinase receptor-targeted protease inhibitor inhibits neointima formation in murine and human blood vessels. Circulation. 2001;103:562–9. https://doi.org/10.1161/01.cir.103.4.562.
Lamfers ML, Grimbergen JM, Aalders MC, Havenga MJ, de Vries MR, Huisman LG, et al. Gene transfer of the urokinase-type plasminogen activator receptor-targeted matrix metalloproteinase inhibitor TIMP-1.ATF suppresses neointima formation more efficiently than tissue inhibitor of metalloproteinase-1. Circ Res. 2002;91:945–52. https://doi.org/10.1161/01.res.0000041418.51906.57.
Eefting D, de Vries MR, Grimbergen JM, Karper JC, van Bockel JH, Quax PH. In vivo suppression of vein graft disease by nonviral, electroporation-mediated, gene transfer of tissue inhibitor of metalloproteinase-1 linked to the amino terminal fragment of urokinase (TIMP-1.ATF), a cell-surface directed matrix metalloproteinase inhibitor. J Vasc Surg. 2010;51:429–37. https://doi.org/10.1016/j.jvs.2009.09.026.
Lamfers ML, Lardenoye JH, de Vries MR, Aalders MC, Engelse MA, Grimbergen JM, et al. In vivo suppression of restenosis in balloon-injured rat carotid artery by adenovirus-mediated gene transfer of the cell surface-directed plasmin inhibitor ATF.BPTI. Gene Ther. 2001;8:534–41. https://doi.org/10.1038/sj.gt.3301437.
Eefting D, Seghers L, Grimbergen JM, de Vries MR, de Boer HC, Lardenoye JW, et al. A novel urokinase receptor-targeted inhibitor for plasmin and matrix metalloproteinases suppresses vein graft disease. Cardiovasc Res. 2010;88:367–75. https://doi.org/10.1093/cvr/cvq203.
Crowson CS, Matteson EL, Myasoedova E, Michet CJ, Ernste FC, Warrington KJ, et al. The lifetime risk of adult-onset rheumatoid arthritis and other inflammatory autoimmune rheumatic diseases. Arthritis Rheum. 2011;63:633–9. https://doi.org/10.1002/art.30155.
Colebatch AN, Edwards CJ, Ostergaard M, van der Heijde D, Balint PV, D’Agostino MA, et al. EULAR recommendations for the use of imaging of the joints in the clinical management of rheumatoid arthritis. Ann Rheum Dis. 2013;72:804–14. https://doi.org/10.1136/annrheumdis-2012-203158.
Wunder A, Straub RH, Gay S, Funk J, Muller-Ladner U. Molecular imaging: novel tools in visualizing rheumatoid arthritis. Rheumatology (Oxford). 2005;44:1341–9. https://doi.org/10.1093/rheumatology/keh709.
Put S, Westhovens R, Lahoutte T, Matthys P. Molecular imaging of rheumatoid arthritis: emerging markers, tools, and techniques. Arthritis Res Ther. 2014;16:208. https://doi.org/10.1186/ar4542.
Malviya G, Conti F, Chianelli M, Scopinaro F, Dierckx RA, Signore A. Molecular imaging of rheumatoid arthritis by radiolabelled monoclonal antibodies: new imaging strategies to guide molecular therapies. Eur J Nucl Med Mol Imaging. 2010;37:386–98. https://doi.org/10.1007/s00259-009-1272-0.
McInnes IB, Schett G. Pathogenetic insights from the treatment of rheumatoid arthritis. Lancet. 2017;389:2328–37. https://doi.org/10.1016/s0140-6736(17)31472-1.
Dinesh P, Rasool M. uPA/uPAR signaling in rheumatoid arthritis: shedding light on its mechanism of action. Pharmacol Res. 2018;134:31–9. https://doi.org/10.1016/j.phrs.2018.05.016.
Serrati S, Margheri F, Chilla A, Neumann E, Muller-Ladner U, Benucci M, et al. Reduction of in vitro invasion and in vivo cartilage degradation in a SCID mouse model by loss of function of the fibrinolytic system of rheumatoid arthritis synovial fibroblasts. Arthritis Rheum. 2011;63:2584–94. https://doi.org/10.1002/art.30439.
Guo Q, Wang Y, Xu D, Nossent J, Pavlos NJ, Xu J. Rheumatoid arthritis: pathological mechanisms and modern pharmacologic therapies. Bone research. 2018;6:15. https://doi.org/10.1038/s41413-018-0016-9.
Szekanecz Z, Haines GK, Koch AE. Differential expression of the urokinase receptor (CD87) in arthritic and normal synovial tissues. J Clin Pathol. 1997;50:314–9. https://doi.org/10.1136/jcp.50.4.314.
Almholt K, Hebsgaard JB, Nansen A, Andersson C, Pass J, Rono B, et al. Antibody-mediated neutralization of uPA proteolytic function reduces disease progression in mouse arthritis models. J Immunol. 2018;200:957–65. https://doi.org/10.4049/jimmunol.1701317.
Pliyev BK, Menshikov MY. Release of the soluble urokinase-type plasminogen activator receptor (suPAR) by activated neutrophils in rheumatoid arthritis. Inflammation. 2010;33:1–9. https://doi.org/10.1007/s10753-009-9152-0.
Fibbi G, Pucci M, Serni U, Cerinic MM, Del Rosso M. Antisense targeting of the urokinase receptor blocks urokinase-dependent proliferation, chemoinvasion, and chemotaxis of human synovial cells and chondrocytes in vitro. Proc Assoc Am Physicians. 1998;110:340–50.
Baran M, Mollers LN, Andersson S, Jonsson IM, Ekwall AK, Bjersing J, et al. Survivin is an essential mediator of arthritis interacting with urokinase signalling. J Cell Mol Med. 2009;13:3797–808. https://doi.org/10.1111/j.1582-4934.2009.00721.x.
Kirchheimer JC. Modulation of receptor bound urokinase-type plasminogen activator on human monocytes by non-steroidal antiinflammatory drugs. Scand J Rheumatol. 1993;22:53–7.
Nonaka T, Kikuchi H, Ikeda T, Okamoto Y, Hamanishi C, Tanaka S. Hyaluronic acid inhibits the expression of u-PA, PAI-1, and u-PAR in human synovial fibroblasts of osteoarthritis and rheumatoid arthritis. J Rheumatol. 2000;27:997–1004.
Nonaka T, Kikuchi H, Sohen S, Fukuda K, Hamanishi C, Tanaka S. Comparison of the inhibitory effects of two types (90 kDa and 190 kDa) of hyaluronic acid on the expression of fibrinolytic factors in human synovial fibroblasts. Mod Rheumatol. 2002;12:160–6. https://doi.org/10.3109/s101650200027.
Guiducci S, Del Rosso A, Cinelli M, Margheri F, D’Alessio S, Fibbi G, et al. Rheumatoid synovial fibroblasts constitutively express the fibrinolytic pattern of invasive tumor-like cells. Clin Exp Rheumatol. 2005;23:364–72.
Del Rosso M, Fibbi G, Magnelli L, Pucci M, Dini G, Grappone C, et al. Modulation of urokinase receptors on human synovial cells and osteoarthritic chondrocytes by diacetylrhein. Int J Tissue React. 1990;12:91–100.
Kirchheimer JC, Remold HG, Wanivenhaus A, Binder BR. Increased proteolytic activity on the surface of monocytes from patients with rheumatoid arthritis. Arthritis Rheum. 1991;34:1430–3.
Belcher C, Fawthrop F, Bunning R, Doherty M. Plasminogen activators and their inhibitors in synovial fluids from normal, osteoarthritis, and rheumatoid arthritis knees. Ann Rheum Dis. 1996;55:230–6. https://doi.org/10.1136/ard.55.4.230.
Ronday HK, Smits HH, Van Muijen GN, Pruszczynski MS, Dolhain RJ, Van Langelaan EJ, et al. Difference in expression of the plasminogen activation system in synovial tissue of patients with rheumatoid arthritis and osteoarthritis. Br J Rheumatol. 1996;35:416–23.
Busso N, Peclat V, So A, Sappino AP. Plasminogen activation in synovial tissues: differences between normal, osteoarthritis, and rheumatoid arthritis joints. Ann Rheum Dis. 1997;56:550–7. https://doi.org/10.1136/ard.56.9.550.
Cerinic MM, Generini S, Partsch G, Pignone A, Dini G, Konttinen YT, et al. Synoviocytes from osteoarthritis and rheumatoid arthritis produce plasminogen activators and plasminogen activator inhibitor-1 and display u-PA receptors on their surface. Life Sci. 1998;63:441–53. https://doi.org/10.1016/s0024-3205(98)00293-8.
Thornton S, Raghu H, Cruz C, Frederick MD, Palumbo JS, Mullins ES, et al. Urokinase plasminogen activator and receptor promote collagen-induced arthritis through expression in hematopoietic cells. Blood advances. 2017;1:545–56. https://doi.org/10.1182/bloodadvances.2016004002.
Jin T, Tarkowski A, Carmeliet P, Bokarewa M. Urokinase, a constitutive component of the inflamed synovial fluid, induces arthritis. Arthritis Res Ther. 2003;5:R9–r17.
Kanno Y, Ishisaki A, Miyashita M, Matsuo O. The blocking of uPAR suppresses lipopolysaccharide-induced inflammatory osteoclastogenesis and the resultant bone loss through attenuation of integrin beta3/Akt pathway. Immunity, inflammation and disease. 2016;4:338–49. https://doi.org/10.1002/iid3.116.
Kanno Y, Maruyama C, Matsuda A, Ishisaki A. uPA-derived peptide, A6 is involved in the suppression of lipopolysaccaride-promoted inflammatory osteoclastogenesis and the resultant bone loss. Immunity, inflammation and disease. 2017;5:289–99. https://doi.org/10.1002/iid3.169.
Apparailly F, Bouquet C, Millet V, Noel D, Jacquet C, Opolon P, et al. Adenovirus-mediated gene transfer of urokinase plasminogen inhibitor inhibits angiogenesis in experimental arthritis. Gene Ther. 2002;9:192–200. https://doi.org/10.1038/sj.gt.3301628.
van der Laan WH, Pap T, Ronday HK, Grimbergen JM, Huisman LG, TeKoppele JM, et al. Cartilage degradation and invasion by rheumatoid synovial fibroblasts is inhibited by gene transfer of a cell surface-targeted plasmin inhibitor. Arthritis Rheum. 2000;43:1710–8. https://doi.org/10.1002/1529-0131(200008)43:8<1710::AID-ANR6>3.0.CO;2-Y.
Del Rosso A, Cinelli M, Guiducci S, Pignone A, Fibbi G, Margheri F, et al. Deflazacort modulates the fibrinolytic pattern and reduces uPA-dependent chemioinvasion and proliferation in rheumatoid arthritis synoviocytes. Rheumatology (Oxford). 2005;44:1255–62. https://doi.org/10.1093/rheumatology/kei006.
Koga T, Okada A, Kawashiri S, Kita J, Suzuki T, Nakashima Y, et al. Soluble urokinase plasminogen activator receptor as a useful biomarker to predict the response to adalimumab in patients with rheumatoid arthritis in a Japanese population. Clin Exp Rheumatol. 2011;29:811–5.
Buckley BJ, Ali U, Kelso MJ, Ranson M. The urokinase plasminogen activation system in rheumatoid arthritis: pathophysiological roles and prospective therapeutic targets. Curr Drug Targets. 2019;20:970–81. https://doi.org/10.2174/1389450120666181204164140.
Kim E, Howes OD, Kapur S. Molecular imaging as a guide for the treatment of central nervous system disorders. Dialogues Clin Neurosci. 2013;15:315–28.
Lu FM, Yuan Z. PET/SPECT molecular imaging in clinical neuroscience: recent advances in the investigation of CNS diseases. Quant Imaging Med Surg. 2015;5:433–47. https://doi.org/10.3978/j.issn.2223-4292.2015.03.16.
Hargreaves RJ, Hoppin J, Sevigny J, Patel S, Chiao P, Klimas M, et al. Optimizing central nervous system drug development using molecular imaging. Clin Pharmacol Ther. 2015;98:47–60. https://doi.org/10.1002/cpt.132.
Bohnen NI, Kanel P, Muller M. Molecular imaging of the cholinergic system in Parkinson’s disease. Int Rev Neurobiol. 2018;141:211–50. https://doi.org/10.1016/bs.irn.2018.07.027.
Merino P, Diaz A, Jeanneret V, Wu F, Torre E, Cheng L, et al. Urokinase-type plasminogen activator (uPA) binding to the uPA receptor (uPAR) promotes axonal regeneration in the central nervous system. J Biol Chem. 2017;292:2741–53. https://doi.org/10.1074/jbc.M116.761650.
Lino N, Fiore L, Rapacioli M, Teruel L, Flores V, Scicolone G, et al. uPA-uPAR molecular complex is involved in cell signaling during neuronal migration and neuritogenesis. Developmental Dynamics. 2014;243:676–89. https://doi.org/10.1002/dvdy.24114.
Farias-Eisner R, Vician L, Silver A, Reddy S, Rabbani SA, Herschman HR. The urokinase plasminogen activator receptor (UPAR) is preferentially induced by nerve growth factor in PC12 pheochromocytoma cells and is required for NGF-driven differentiation. J Neurosci. 2000;20:230–9.
Semina E, Rubina K, Sysoeva V, Rysenkova K, Klimovich P, Plekhanova O, et al. Urokinase and urokinase receptor participate in regulation of neuronal migration, axon growth and branching. Eur J Cell Biol. 2016;95:295–310. https://doi.org/10.1016/j.ejcb.2016.05.003.
Del Bigio MR, Hosain S, Altumbabic M. Localization of urokinase-type plasminogen activator, its receptor, and inhibitors in mouse forebrain during postnatal development. Int J Dev Neurosci. 1999;17:387–99.
Hayden SM, Seeds NW. Modulated expression of plasminogen activator system components in cultured cells from dissociated mouse dorsal root ganglia. J Neurosci. 1996;16:2307–17.
Campbell DB, D’Oronzio R, Garbett K, Ebert PJ, Mirnics K, Levitt P, et al. Disruption of cerebral cortex MET signaling in autism spectrum disorder. Ann Neurol. 2007;62:243–50. https://doi.org/10.1002/ana.21180.
Campbell DB, Li C, Sutcliffe JS, Persico AM, Levitt P. Genetic evidence implicating multiple genes in the MET receptor tyrosine kinase pathway in autism spectrum disorder. Autism Research. 2008;1:159–68. https://doi.org/10.1002/aur.27.
Lahtinen L, Huusko N, Myohanen H, Lehtivarjo AK, Pellinen R, Turunen MP, et al. Expression of urokinase-type plasminogen activator receptor is increased during epileptogenesis in the rat hippocampus. Neuroscience. 2009;163:316–28. https://doi.org/10.1016/j.neuroscience.2009.06.019.
Powell EM, Campbell DB, Stanwood GD, Davis C, Noebels JL, Levitt P. Genetic disruption of cortical interneuron development causes region- and GABA cell type-specific deficits, epilepsy, and behavioral dysfunction. J Neurosci. 2003;23:622–31.
Levitt P. Disruption of interneuron development. Epilepsia. 2005;46(Suppl 7):22–8. https://doi.org/10.1111/j.1528-1167.2005.00305.x.
Roll P, Rudolf G, Pereira S, Royer B, Scheffer IE, Massacrier A, et al. SRPX2 mutations in disorders of language cortex and cognition. Hum Mol Genet. 2006;15:1195–207. https://doi.org/10.1093/hmg/ddl035.
Royer-Zemmour B, Ponsole-Lenfant M, Gara H, Roll P, Leveque C, Massacrier A, et al. Epileptic and developmental disorders of the speech cortex: ligand/receptor interaction of wild-type and mutant SRPX2 with the plasminogen activator receptor uPAR. Hum Mol Genet. 2008;17:3617–30. https://doi.org/10.1093/hmg/ddn256.
Anand R, Gill KD, Mahdi AA. Therapeutics of Alzheimer’s disease: past, present and future. Neuropharmacology. 2014;76 Pt A:27-50. doi:10.1016/j.neuropharm.2013.07.004.
Kumar A, Singh A. Ekavali. A review on Alzheimer’s disease pathophysiology and its management: an update. Pharmacol Rep. 2015;67:195–203. https://doi.org/10.1016/j.pharep.2014.09.004.
Deininger MH, Trautmann K, Magdolen V, Luther T, Schluesener HJ, Meyermann R. Cortical neurons of Creutzfeldt-Jakob disease patients express the urokinase-type plasminogen activator receptor. Neurosci Lett. 2002;324:80–2. https://doi.org/10.1016/s0304-3940(02)00168-4.
Davis J, Wagner MR, Zhang W, Xu F, Van Nostrand WE. Amyloid beta-protein stimulates the expression of urokinase-type plasminogen activator (uPA) and its receptor (uPAR) in human cerebrovascular smooth muscle cells. J Biol Chem. 2003;278:19054–61. https://doi.org/10.1074/jbc.M301398200.
Walker DG, Lue LF, Beach TG. Increased expression of the urokinase plasminogen-activator receptor in amyloid beta peptide-treated human brain microglia and in AD brains. Brain Res. 2002;926:69–79. https://doi.org/10.1016/s0006-8993(01)03298-x.
Pocchiari M, Puopolo M, Croes EA, Budka H, Gelpi E, Collins S, et al. Predictors of survival in sporadic Creutzfeldt-Jakob disease and other human transmissible spongiform encephalopathies. Brain : a journal of neurology. 2004;127:2348–59. https://doi.org/10.1093/brain/awh249.
Dendrou CA, Fugger L, Friese MA. Immunopathology of multiple sclerosis. Nat Rev Immunol. 2015;15:545–58. https://doi.org/10.1038/nri3871.
Washington R, Burton J, Todd RF 3rd, Newman W, Dragovic L, Dore-Duffy P. Expression of immunologically relevant endothelial cell activation antigens on isolated central nervous system microvessels from patients with multiple sclerosis. Ann Neurol. 1994;35:89–97. https://doi.org/10.1002/ana.410350114.
Dore-Duffy P, Washington R, Dragovic L. Expression of endothelial cell activation antigens in microvessels from patients with multiple sclerosis. Adv Exp Med Biol. 1993;331:243–8. https://doi.org/10.1007/978-1-4615-2920-0_38.
Gveric D, Hanemaaijer R, Newcombe J, van Lent NA, Sier CF, Cuzner ML. Plasminogen activators in multiple sclerosis lesions: implications for the inflammatory response and axonal damage. Brain. 2001;124:1978–88. https://doi.org/10.1093/brain/124.10.1978.
Archinti M, Britto M, Eden G, Furlan F, Murphy R, Degryse B. The urokinase receptor in the central nervous system. CNS Neurol Disord Drug Targets. 2011;10:271–94.
Cox MB, Bowden NA, Scott RJ, Lechner-Scott J. Altered expression of the plasminogen activation pathway in peripheral blood mononuclear cells in multiple sclerosis: possible pathomechanism of matrix metalloproteinase activation. Multiple sclerosis (Houndmills, Basingstoke, England). 2013;19:1268–74. https://doi.org/10.1177/1352458513475493.
Washington RA, Becher B, Balabanov R, Antel J, Dore-Duffy P. Expression of the activation marker urokinase plasminogen-activator receptor in cultured human central nervous system microglia. J Neurosci Res. 1996;45:392–9. https://doi.org/10.1002/(sici)1097-4547(19960815)45:4<392::Aid-jnr8>3.0.Co;2-4.
Teesalu T, Hinkkanen AE, Vaheri A. Coordinated induction of extracellular proteolysis systems during experimental autoimmune encephalomyelitis in mice. Am J Pathol. 2001;159:2227–37. https://doi.org/10.1016/s0002-9440(10)63073-8.
Cunningham O, Campion S, Perry VH, Murray C, Sidenius N, Docagne F, et al. Microglia and the urokinase plasminogen activator receptor/uPA system in innate brain inflammation. Glia. 2009;57:1802–14. https://doi.org/10.1002/glia.20892.
East E, Baker D, Pryce G, Lijnen HR, Cuzner ML, Gveric D. A role for the plasminogen activator system in inflammation and neurodegeneration in the central nervous system during experimental allergic encephalomyelitis. Am J Pathol. 2005;167:545–54. https://doi.org/10.1016/s0002-9440(10)62996-3.
Gur-Wahnon D, Mizrachi T, Maaravi-Pinto FY, Lourbopoulos A, Grigoriadis N, Higazi AA, et al. The plasminogen activator system: involvement in central nervous system inflammation and a potential site for therapeutic intervention. J Neuroinflammation. 2013;10:124. https://doi.org/10.1186/1742-2094-10-124.
Gobel K, Pankratz S, Asaridou CM, Herrmann AM, Bittner S, Merker M, et al. Blood coagulation factor XII drives adaptive immunity during neuroinflammation via CD87-mediated modulation of dendritic cells. Nat Commun. 2016;7:11626. https://doi.org/10.1038/ncomms11626.
Brew BJ, Chan P. Update on HIV dementia and HIV-associated neurocognitive disorders. Current neurology and neuroscience reports. 2014;14:468. https://doi.org/10.1007/s11910-014-0468-2.
Cinque P, Nebuloni M, Santovito ML, Price RW, Gisslen M, Hagberg L, et al. The urokinase receptor is overexpressed in the AIDS dementia complex and other neurological manifestations. Ann Neurol. 2004;55:687–94. https://doi.org/10.1002/ana.20076.
Sidenius N, Nebuloni M, Sala S, Zerbi P, Price RW, Gisslen M, et al. Expression of the urokinase plasminogen activator and its receptor in HIV-1-associated central nervous system disease. J Neuroimmunol. 2004;157:133–9. https://doi.org/10.1016/j.jneuroim.2004.08.038.
Sidenius N, Sier CF, Ullum H, Pedersen BK, Lepri AC, Blasi F, et al. Serum level of soluble urokinase-type plasminogen activator receptor is a strong and independent predictor of survival in human immunodeficiency virus infection. Blood. 2000;96:4091–5.
Idro R, Jenkins NE, Newton CR. Pathogenesis, clinical features, and neurological outcome of cerebral malaria. The Lancet Neurology. 2005;4:827–40. https://doi.org/10.1016/s1474-4422(05)70247-7.
Fauser S, Deininger MH, Kremsner PG, Magdolen V, Luther T, Meyermann R, et al. Lesion associated expression of urokinase-type plasminogen activator receptor (uPAR, CD87) in human cerebral malaria. J Neuroimmunol. 2000;111:234–40. https://doi.org/10.1016/s0165-5728(00)00368-4.
Piguet PF, Da Laperrousaz C, Vesin C, Tacchini-Cottier F, Senaldi G, Grau GE. Delayed mortality and attenuated thrombocytopenia associated with severe malaria in urokinase- and urokinase receptor-deficient mice. Infect Immun. 2000;68:3822–9. https://doi.org/10.1128/iai.68.7.3822-3829.2000.
Wassmer SC, Combes V, Grau GE. Pathophysiology of cerebral malaria: role of host cells in the modulation of cytoadhesion. Ann N Y Acad Sci. 2003;992:30–8. https://doi.org/10.1111/j.1749-6632.2003.tb03135.x.
Khor B, Gardet A, Xavier RJ. Genetics and pathogenesis of inflammatory bowel disease. Nature. 2011;474:307–17. https://doi.org/10.1038/nature10209.
Caobelli F, Evangelista L, Quartuccio N, Familiari D, Altini C, Castello A, et al. Role of molecular imaging in the management of patients affected by inflammatory bowel disease: state-of-the-art. World journal of radiology. 2016;8:829–45. https://doi.org/10.4329/wjr.v8.i10.829.
Catalano O, Maccioni F, Lauri C, Auletta S, Dierckx R, Signore A. Hybrid imaging in Crohn’s disease: from SPECT/CT to PET/MR and new image interpretation criteria. Q J Nucl Med Mol Imaging. 2018;62:40–55. https://doi.org/10.23736/s1824-4785.17.03053-9.
Meijer MJ, Mieremet-Ooms MA, Sier CF, van Hogezand RA, Lamers CB, Hommes DW, et al. Matrix metalloproteinases and their tissue inhibitors as prognostic indicators for diagnostic and surgical recurrence in Crohn’s disease. Inflamm Bowel Dis. 2009;15:84–92. https://doi.org/10.1002/ibd.20581.
Birch GP, Campbell T, Bradley M, Dhaliwal K. Optical molecular imaging of inflammatory cells in interventional medicine-an emerging strategy. Frontiers in oncology. 2019;9:882. https://doi.org/10.3389/fonc.2019.00882.
de Bruin PA, Crama-Bohbouth G, Verspaget HW, Verheijen JH, Dooijewaard G, Weterman IT, et al. Plasminogen activators in the intestine of patients with inflammatory bowel disease. Thromb Haemost. 1988;60:262–6.
de Jong E, Porte RJ, Knot EA, Verheijen JH, Dees J. Disturbed fibrinolysis in patients with inflammatory bowel disease. A study in blood plasma, colon mucosa, and faeces. Gut. 1989;30:188–94. https://doi.org/10.1136/gut.30.2.188.
Ravi A, Garg P, Sitaraman SV. Matrix metalloproteinases in inflammatory bowel disease: boon or a bane? Inflamm Bowel Dis. 2007;13:97–107. https://doi.org/10.1002/ibd.20011.
Laerum OD, Illemann M, Skarstein A, Helgeland L, Ovrebo K, Dano K, et al. Crohn’s disease but not chronic ulcerative colitis induces the expression of PAI-1 in enteric neurons. Am J Gastroenterol. 2008;103:2350–8. https://doi.org/10.1111/j.1572-0241.2008.01930.x.
Genua M, D’Alessio S, Cibella J, Gandelli A, Sala E, Correale C, et al. The urokinase plasminogen activator receptor (uPAR) controls macrophage phagocytosis in intestinal inflammation. Gut. 2015;64:589–600. https://doi.org/10.1136/gutjnl-2013-305933.
Weber B, Saurer L, Schenk M, Dickgreber N, Mueller C. CX3CR1 defines functionally distinct intestinal mononuclear phagocyte subsets which maintain their respective functions during homeostatic and inflammatory conditions. Eur J Immunol. 2011;41:773–9. https://doi.org/10.1002/eji.201040965.
Na YR, Stakenborg M, Seok SH, Matteoli G. Macrophages in intestinal inflammation and resolution: a potential therapeutic target in IBD. Nat Rev Gastroenterol Hepatol. 2019;16:531–43. https://doi.org/10.1038/s41575-019-0172-4.
Yousif AM, Minopoli M, Bifulco K, Ingangi V, Di Carluccio G, Merlino F, et al. Cyclization of the urokinase receptor-derived ser-arg-ser-arg-tyr peptide generates a potent inhibitor of trans-endothelial migration of monocytes. PLoS One. 2015;10:e0126172. https://doi.org/10.1371/journal.pone.0126172.
Genua M, Ingangi V, Fonteyne P, Piontini A, Yousif AM, Merlino F, et al. Treatment with a urokinase receptor-derived cyclized peptide improves experimental colitis by preventing monocyte recruitment and macrophage polarization. Inflamm Bowel Dis. 2016;22:2390–401. https://doi.org/10.1097/mib.0000000000000896.
Yang L, Peng XH, Wang YA, Wang X, Cao Z, Ni C, et al. Receptor-targeted nanoparticles for in vivo imaging of breast cancer. Clinical cancer research. 2009;15:4722–32. https://doi.org/10.1158/1078-0432.Ccr-08-3289.
Yang L, Mao H, Cao Z, Wang YA, Peng X, Wang X, et al. Molecular imaging of pancreatic cancer in an animal model using targeted multifunctional nanoparticles. Gastroenterology. 2009;136:1514–25.e2. https://doi.org/10.1053/j.gastro.2009.01.006.
Abdalla MO, Karna P, Sajja HK, Mao H, Yates C, Turner T, et al. Enhanced noscapine delivery using uPAR-targeted optical-MR imaging trackable nanoparticles for prostate cancer therapy. Journal of controlled release. 2011;149:314–22. https://doi.org/10.1016/j.jconrel.2010.10.030.
Liu D, Overbey D, Watkinson L, Giblin MF. Synthesis and characterization of an (111)in-labeled peptide for the in vivo localization of human cancers expressing the urokinase-type plasminogen activator receptor (uPAR). Bioconjug Chem. 2009;20:888–94. https://doi.org/10.1021/bc800433y.
Xi L, Zhou G, Gao N, Yang L, Gonzalo DA, Hughes SJ, et al. Photoacoustic and fluorescence image-guided surgery using a multifunctional targeted nanoprobe. Ann Surg Oncol. 2014;21:1602–9. https://doi.org/10.1245/s10434-014-3541-9.
Lee GY, Qian WP, Wang L, Wang YA, Staley CA, Satpathy M, et al. Theranostic nanoparticles with controlled release of gemcitabine for targeted therapy and MRI of pancreatic cancer. ACS Nano. 2013;7:2078–89. https://doi.org/10.1021/nn3043463.
Yang L, Sajja HK, Cao Z, Qian W, Bender L, Marcus AI, et al. uPAR-targeted optical imaging contrasts as theranostic agents for tumor margin detection. Theranostics. 2013;4:106–18. https://doi.org/10.7150/thno.7409.
Zhang X, Tian YE, Sun F, Feng H, Yang C, Gong X, et al. Imaging of human pancreatic cancer xenografts by single-photon emission computed tomography with (99 m)Tc-Hynic-PEG-AE105. Oncol Lett. 2015;10:2253–8. https://doi.org/10.3892/ol.2015.3504.
Persson M, Nedergaard MK, Brandt-Larsen M, Skovgaard D, Jørgensen JT, Michaelsen SR, et al. Urokinase-type plasminogen activator receptor as a potential PET biomarker in glioblastoma. Journal of Nuclear Medicine. 2016;57:272–8. https://doi.org/10.2967/jnumed.115.161703.
Juhl K, Christensen A, Persson M, Ploug M, Kjaer A. Peptide-based optical uPAR imaging for surgery: in vivo testing of ICG-Glu-Glu-AE105. PLoS One. 2016;11:e0147428. https://doi.org/10.1371/journal.pone.0147428.
Christensen A, Juhl K, Persson M, Charabi BW, Mortensen J, Kiss K, et al. uPAR-targeted optical near-infrared (NIR) fluorescence imaging and PET for image-guided surgery in head and neck cancer: proof-of-concept in orthotopic xenograft model. Oncotarget. 2017;8:15407–19. https://doi.org/10.18632/oncotarget.14282.
Juhl K, Christensen A, Rubek N, Karnov KKS, von Buchwald C, Kjaer A, et al. Oncotarget. 2019;10:6308–16. https://doi.org/10.18632/oncotarget.27220.
Kurbegovic S, Juhl K, Chen H, Qu C, Ding B, Leth JM, et al. Molecular targeted NIR-II probe for image-guided brain tumor surgery. Bioconjug Chem. 2018;29:3833–40. https://doi.org/10.1021/acs.bioconjchem.8b00669.
LeBeau AM, Duriseti S, Murphy ST, Pepin F, Hann B, Gray JW, et al. Targeting uPAR with antagonistic recombinant human antibodies in aggressive breast cancer. Cancer Res. 2013;73:2070–81. https://doi.org/10.1158/0008-5472.Can-12-3526.
LeBeau AM, Sevillano N, King ML, Duriseti S, Murphy ST, Craik CS, et al. Imaging the urokinase plasminongen activator receptor in preclinical breast cancer models of acquired drug resistance. Theranostics. 2014;4:267–79. https://doi.org/10.7150/thno.7323.
Boonstra MC, Van Driel P, Keereweer S, Prevoo H, Stammes MA, Baart VM, et al. Preclinical uPAR-targeted multimodal imaging of locoregional oral cancer. Oral Oncol. 2017;66:1–8. https://doi.org/10.1016/j.oraloncology.2016.12.026.
Boonstra MC, van Driel PB, van Willigen DM, Stammes MA, Prevoo HA, Tummers QR, et al. uPAR-targeted multimodal tracer for pre- and intraoperative imaging in cancer surgery. Oncotarget. 2015;6:14260-14273. doi:10.18632/oncotarget.3680.
Appella E, Blasi F. The growth factor module of urokinase is the binding sequence for its receptor. Ann N Y Acad Sci. 1987;511:192–5. https://doi.org/10.1111/j.1749-6632.1987.tb36247.x.
Lwin TM, Hoffman RM, Bouvet M. The development of fluorescence guided surgery for pancreatic cancer: from bench to clinic. Expert Rev Anticancer Ther. 2018;18:651–62. https://doi.org/10.1080/14737140.2018.1477593.
Goodson RJ, Doyle MV, Kaufman SE, Rosenberg S. High-affinity urokinase receptor antagonists identified with bacteriophage peptide display. Proc Natl Acad Sci U S A. 1994;91:7129–33. https://doi.org/10.1073/pnas.91.15.7129.
Ploug M, Østergaard S, Gårdsvoll H, Kovalski K, Holst-Hansen C, Holm A, et al. Peptide-derived antagonists of the urokinase receptor. affinity maturation by combinatorial chemistry, identification of functional epitopes, and inhibitory effect on cancer cell intravasation. Biochemistry. 2001;40:12157–68. https://doi.org/10.1021/bi010662g..
Persson M, El Ali HH, Binderup T, Pfeifer A, Madsen J, Rasmussen P, et al. Dosimetry of 64Cu-DOTA-AE105, a PET tracer for uPAR imaging. Nucl Med Biol. 2014;41:290–5. https://doi.org/10.1016/j.nucmedbio.2013.12.007.
Persson M, Hosseini M, Madsen J, Jørgensen TJ, Jensen KJ, Kjaer A, et al. Improved PET imaging of uPAR expression using new (64)cu-labeled cross-bridged peptide ligands: comparative in vitro and in vivo studies. Theranostics. 2013;3:618–32. https://doi.org/10.7150/thno.6810.
Li ZB, Niu G, Wang H, He L, Yang L, Ploug M, et al. Imaging of urokinase-type plasminogen activator receptor expression using a 64Cu-labeled linear peptide antagonist by microPET. Clinical Cancer Research. 2008;14:4758–66. https://doi.org/10.1158/1078-0432.Ccr-07-4434.
Persson M, Madsen J, Østergaard S, Jensen MM, Jørgensen JT, Juhl K, et al. Quantitative PET of human urokinase-type plasminogen activator receptor with 64Cu-DOTA-AE105: implications for visualizing cancer invasion. J Nuclear Medicine. 2012;53:138–45. https://doi.org/10.2967/jnumed.110.083386.
Skovgaard D, Persson M, Kjaer A. Imaging of prostate cancer using urokinase-type plasminogen activator receptor PET. PET Clin. 2017;12:243–55. https://doi.org/10.1016/j.cpet.2016.12.005.
Pedersen SF, Petersen LR, Skovgaard DC, Persson M, Johannesen HH, Brandt-Larsen M, et al. Feasibility of 64Cu-DOTA-AE105 for arterial wall in vivo PET of the urokinase-plasminogen-activator-receptor (uPAR). J Nucl Med. 2016;57:1632.
Schmitt M, Mengele K, Napieralski R, Magdolen V, Reuning U, Gkazepis A, et al. Clinical utility of level-of-evidence-1 disease forecast cancer biomarkers uPA and its inhibitor PAI-1. Expert Rev Mol Diagn. 2010;10:1051–67. https://doi.org/10.1586/erm.10.71.
Duriseti S, Goetz DH, Hostetter DR, LeBeau AM, Wei Y, Craik CS. Antagonistic anti-urokinase plasminogen activator receptor (uPAR) antibodies significantly inhibit uPAR-mediated cellular signaling and migration. J Biol Chem. 2010;285:26878–88. https://doi.org/10.1074/jbc.M109.077677.
Bauer TW, Liu W, Fan F, Camp ER, Yang A, Somcio RJ, et al. Targeting of urokinase plasminogen activator receptor in human pancreatic carcinoma cells inhibits c-met- and insulin-like growth factor-I receptor-mediated migration and invasion and orthotopic tumor growth in mice. Cancer Res. 2005;65:7775–81. https://doi.org/10.1158/0008-5472.Can-05-0946.
Rabbani SA, Ateeq B, Arakelian A, Valentino ML, Shaw DE, Dauffenbach LM, et al. An anti-urokinase plasminogen activator receptor antibody (ATN-658) blocks prostate cancer invasion, migration, growth, and experimental skeletal metastasis in vitro and in vivo. Neoplasia. 2010;12:778–88. https://doi.org/10.1593/neo.10296.
Mahmood N, Arakelian A, Khan HA, Tanvir I, Mazar AP, Rabbani SA. uPAR antibody (huATN-658) and Zometa reduce breast cancer growth and skeletal lesions. Bone Res. 2020;8:18. https://doi.org/10.1038/s41413-020-0094-3.
Code availability
Not applicable.
Funding
CS was in part funded by the European Commission under two Marie Skłodowska-Curie Action awards: H2020-MSCA-RISE-2019 (Project number: 872860 - PRISAR2) and H2020-MSCA-ITN-2019 (Project number: 857894 - CAST).
Author information
Authors and Affiliations
Contributions
VB designed the manuscript, performed the literature search and data analysis, and drafted the first version. RH made the figures and critically revised the manuscript. LFdGO, PQ, PK, and AV critically revised the manuscript. CS designed and critically revised the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This review does not contain any studies with human participants or animals performed by any of the authors.
Consent for publication
Not applicable.
Competing interests
Authors VB, RH, LFdGO, PQ, PK, AV, and CS declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Baart, V.M., Houvast, R.D., de Geus-Oei, L.F. et al. Molecular imaging of the urokinase plasminogen activator receptor: opportunities beyond cancer. EJNMMI Res 10, 87 (2020). https://doi.org/10.1186/s13550-020-00673-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13550-020-00673-7