Abstract
Background
Immunotherapy represents a new therapeutic approach in non-small cell lung carcinoma (NSCLC) with the potential for prolonged benefits. Because of the systemic nature and heterogeneity of tumoral diseases, as well as the immune restoration process induced by immunotherapy, the assessment of therapeutic efficacy is challenging, and the role of FDG PET is not well established. We evaluated the potential of FDG PET to monitor NSCLC patients treated with a checkpoint inhibitor.
Results
This was a retrospective analysis of 28 NSCLC patients treated with nivolumab, a programmed cell death 1 (PD-1) blocker. All patients underwent a PET scan before treatment (SCAN-1) and another scan 2 months later (SCAN-2). Disease progression was assessed by immune PET Response Criteria in Solid Tumors (iPERCIST), which was adapted from PERCIST; and the immune Response Evaluation Criteria in Solid Tumors (iRECIST). iPERCIST is a dual-time-point evaluation of “unconfirmed progressive metabolic disease” (UPMD) status at SCAN-2. UPMD at SCAN-2 was re-evaluated after 4 weeks with SCAN-3 to confirm PMD. Patients with complete/partial metabolic response (CMR or PMR) or stable metabolic disease (SMD) at SCAN-2 or -3 were considered responders. Patients with UPMD confirmed at SCAN-3 were considered non-responders. The Kaplan-Meier method was used to estimate survival. At SCAN-2, we found 9/28 cases of PMR, 4/28 cases of SMD, 2/28 cases of CMR, and 13/28 cases of UPMD. Four of the 13 UPMD patients were classified as responders at SCAN-3 (PMR n = 1, SMD n = 3). The remaining nine UPMD patients were classified as non-responders due to clinical degradation, and treatment was stopped. The median follow-up was 16.7 months [3.6–32.2]. Responders continued treatment for a mean of 10.7 months [3.8–26.3]. Overall survival was longer for responders than that for non-responders (19.9 vs. 3.6 months, log rank p = 0.0003). The 1-year survival rates were 94% for responders and 11% for non-responders. A comparison with iRECIST showed reclassification in 39% (11/28) of patients with relevant additional prognostic information.
Conclusions
iPERCIST dual-time-point evaluation might be a powerful tool for evaluating anti-PD-1-based immunotherapy, with the ability to identify patients who can benefit most from treatment. The prognostic value of iPERCIST criteria should be confirmed in large prospective multicentric studies.
Similar content being viewed by others
Background
Lung cancer is one of the most common malignant tumors and represents the leading cause of death by cancer in Europe and in the USA [1, 2]. Non-small cell lung carcinoma (NSCLC) accounts for 85% of lung cancers [3], and close to 70% of patients present with locally advanced or metastatic disease at the time of diagnosis. Recently, immunotherapy has become a standard treatment after chemotherapy in NSCLC, whether locally advanced or metastatic, offering the potential for prolonged response and survival time [4]. Two phase III studies have demonstrated higher overall response and survival rates in patients with NSCLC treated with nivolumab versus docetaxel [5, 6].
Positron emission tomography/computed tomography (PET) with fluorodeoxyglucose (FDG) is widely used to assess the response to chemotherapy. However, the mechanisms of action of checkpoint inhibitors differ from those of chemotherapies. In some cases, the initial response to nivolumab may be an increase in the size and metabolism of tumor lesions due to lymphocyte infiltration, leading to false interpretations [7]. Several response patterns have been described with computed tomography (CT), but data with FDG PET monitoring are scarce. Because of the new mechanisms of action of therapies and the heterogeneity of malignant disease, methods of assessing response are complex, and the role of PET is not well established.
Recently, several attempts to establish adapted imaging criteria as follow-up to immunotherapy treatment have been proposed, notably the immune Response Evaluation Criteria in Solid Tumors (iRECIST) [8]. Regarding metabolic imaging, PET Response Criteria in Solid Tumors (PERCIST) have been proposed for solid tumor monitoring but have not been validated with new immunotherapies. Consequently, the authors proposed other response criteria using a single-time-point PET analysis for immunotherapy response assessment, especially in melanoma patients. Cho et al. studied patients with advanced melanoma under immunotherapy using an early PET evaluation method combined with a CT scan (3–4 weeks) to predict the best overall response at 4 months [9]. The conclusion of the work was that the combination of functional and anatomical imaging parameters obtained early after the start of treatment appears predictive for eventual response at 4 months. Anwar et al. proposed using an absolute number of 4 newly emerged FDG-avid lesions on post-therapy PET scans in melanoma patients under ipilimumab to provide reliable information for treatment response [10, 11]. However, as well-written in the paper from Pinker et al., a new response category, including an indeterminate response, based on a dual-time-point evaluation could be relevant during the metabolic evaluation of immunotherapy, as already shown with iRECIST [12]. This indeterminate response or “unconfirmed” status recognizes that delayed responses or immune-mediated flares can both occur in the first months of immunotherapy treatment [12]. This additional category provides the clinician flexibility to continue treatment in good general status patients and to perform a subsequent evaluation to confirm or deny a truly progressive disease [12].
Based on this assumption, we chose to introduce and evaluate metabolic criteria based on a dual-time-point evaluation, as proposed with iRECIST. We designed a retrospective study to evaluate the prognostic value of FDG PET using modified PERCIST criteria adapted from iRECIST, which we called Immune PET Response Criteria in Solid Tumors (iPERCIST), in monitoring patients with NSCLC treated with an anti-programmed death-1 checkpoint inhibitor.
Methods
Patients
Between April 2015 and January 2017, all consecutive patients referred for PET imaging with a diagnosis of NSCLC and who were treated with anti-programmed death-1 checkpoint inhibitor, nivolumab, were retrospectively selected from our database. Patients needed to have undergone a PET scan before the start of the treatment (SCAN-1) and to have at least a second evaluation PET scan 2 months after treatment (SCAN-2).
Nivolumab was prescribed according to current recommendations and the clinicians’ judgment. Treatment continuation was decided according to the clinical status and the evaluation of the imaging findings. To receive nivolumab, all patients had to have an Eastern Cooperative Oncology Group performance status < 2.
Imaging protocol
Baseline PET imaging was performed within 1 month before the start of immunotherapy. Follow-up PET imaging was performed in all patients at approximately 8 weeks (equivalent to 4 cycles of treatment) after the first dose of nivolumab (SCAN-2). When warranted, a second follow-up FDG-PET was performed 4 weeks later (equivalent to 2 cycles of treatment) to confirm disease progression (SCAN-3).
PET/CT images were acquired 60 min after intravenous injection of FDG at a dose of 3 MBq/kg. The serum glucose level was < 1.4 g/L at the time of injection in all patients. All PET images were acquired with a Gemini TF PET/CT scanner (Philips Medical Systems, the Netherlands). The Gemini TF is a time-of-flight-capable, fully 3D PET scanner with a 16-slice Brilliance CT scanner. CT images were obtained without injection of contrast medium and with the following settings: 120 kV, 100 mA, 16 × 1.5 mm collimation, 0.69 pitch, 3 mm slice thickness, and 1.5 mm increments. PET images were reconstructed by using a BLOB-OS-TF list-mode iterative algorithm with 2 iterations and 33 subsets. A single-scatter simulation model was used for scatter correction. Attenuation correction was based on the CT data. No post-reconstruction smoothing filter was used. The reconstructed spatial resolution was 5 mm in the center of the field of view. The image voxel size was 4 × 4 × 4 mm for PET images and 1.17 × 1.17 × 1.5 mm for CT images. Peak standardized uptake values normalized by lean body mass (SULpeak) was calculated in a 1-cm-diameter region of interest placed on the highest uptake site of the tumor. Mean liver SUL was measured in a 3-cm-diameter spherical ROI as recommended in PERCIST [13].
Metabolic response assessment
Images were centrally and jointly reviewed by two experienced nuclear physicians who had no knowledge of the patients’ medical history or symptoms (LG and MS). We introduced the concept of an iPERCIST classification, adapted from PERCIST and iRECIST [8, 13]. The objective was to obtain a reliable tool for assessing the response to immunotherapy, taking into account the possible avid-FDG lymphocytic tumoral infiltration under treatment. As recommended in PERCIST, baseline and follow-up scans were reviewed, and the lesion with the highest FDG uptake on each of these two scans was identified [14]. Complete metabolic response (CMR), partial metabolic response (PMR), and stable metabolic disease (SMD) were defined according to PERCIST [14]. CMR was defined as the visual absence of pathological FDG uptake in all baseline lesions identified on the baseline PET scan. PMR was defined as a decrease of at least 30% in the SULpeak of the target lesion, which is associated with an absence of progression of the non-target lesions. SMD was defined as an absence of response or progression.
Progressive metabolic disease (PMD) was defined as an increase of at least 30% in the SULpeak of the target lesion or as an unequivocal progression of the non-target lesions, regardless of the response in the target lesion. However, regarding PMD, we accounted for unconfirmed and confirmed progressive disease, from iRECIST [8], and established their corollaries with metabolic assessments. We defined two new categories replacing the PMD category: unconfirmed progressive metabolic disease (UPMD) and confirmed progressive metabolic disease (CPMD). UPMD was a PMD at SCAN-2, and CPMD was an UPMD confirmed 4 weeks later at SCAN-3. In iPERCIST, SCAN-3 is compared to SCAN-2, and patients were classified as CMR, PMR, SMD, or CPMD according to PERCIST recommendations. The continuation of treatment after the first evaluation by SCAN-2 was according to the physician’s judgment, which integrated metabolic response and the deterioration of clinical status, as described in iRECIST [8].
Finally, we classified patients as responders or non-responders. Patients with CMR, PMR, SMD, or UPMD followed by PMR or SMD were classified as responders. Patients with UMPD associated with clinical deterioration or UPMD followed by CPMD were classified as non-responders. These criteria are presented in Table 1.
In addition, we classified patients according to iRECIST criteria based on the CT (without contrast) part of the PET/CT scan [8] (see Table 1).
Statistical analysis
Overall survival (OS) was defined as the time from the start of immunotherapy to death from any cause. The 1-year survival rate in responders and non-responders was recorded. We compared OS and the 1-year survival rate between responders and non-responders. The Kaplan-Meier method was used to estimate survival probability, with the level of significance estimated by the log-rank test. The difference between the continuous data for the two groups was determined by the Mann-Whitney test. Statistical analyses were performed using R Core Team (2014) software. The results were considered statistically significant when p < 0.05.
Results
Patient characteristics
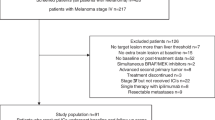
A total of 28 patients (18 men; median age 63 years [range 42–79 years]) were retrospectively included (Fig. 1). Patient demographics are shown in Table 2. Briefly, 23 patients (82%) had a smoking history, adenocarcinomas were the most common histological tumor type, 23 tumors (82%) were initially metastatic, 5 patients (18%) were treated with surgery before disease recurrence, and patients received a median of 12 cycles of nivolumab.
Anti-PD-1 therapy evaluation with iPERCIST
SCAN-2 was performed after 4 cycles of nivolumab in 20/28 patients, 3 cycles in 4/28 patients, 5 cycles in 3/28 patients, and 6 cycles in 1/28 patient. For the 28 patients at SCAN-2, 9 showed PMR (Fig. 2), 4 showed SMD, 2 showed CMR, and 13 showed UPMD. For the 2 patients with CMR, nivolumab treatment was maintained for 15.3 and 18.6 months, and the patients were still alive at the last follow-up. Among UPMD patients (13/28), only 4 were classified with SMD (n = 3) or PMR (n = 1) at SCAN-3 (Fig. 3 and Additional file 1: Figure S1). The remaining 9/13 UPMD patients showed clinical deterioration at the time of PET evaluation; thus, clinicians waived SCAN-3. Of these nine patients, five received a new chemotherapy line (docetaxel, gemcitabine, or erlotinib), three were referred for palliative care, and one was lost at follow-up.
A 64-year-old patient with metastatic lung adenocarcinoma was treated with a second line of nivolumab. SCAN-1 shows lung nodules with adrenal metastases (a, maximum intensity projection (MIP) image, arrows; b, e axial fusion). SCAN-2 at 8 weeks of treatment (4 cycles) showing partial metabolic response (PMR): complete metabolic response on the lungs and left adrenal lesions (c MIP, d axial fusion) but persistent and significant FDG uptake on the right adrenal lesion (f arrow). The classification was PMR according to iPERCIST. Nivolumab treatment was maintained for 10 months, and at the last follow-up, the patient was still alive (survival of 23.8 months)
A 45-year-old women with metastatic lymphoepithelioma-like lung carcinoma treated with a second line of nivolumab. SCAN-1 showed left lung carcinoma with liver metastases (a maximum intensity projection image, MIP, arrows). SCAN-2 at 8 weeks of treatment (4 cycles) showed UPMD: increase in size of the primary lesion and appearance of numerous liver lesions (b MIP). SCAN-3 after two more cycles of nivolumab showed the disappearance of most liver lesions and a persistent large lung mass (c MIP). See Additional file 1: Figure S1 for axial views. Pseudo-progression was retrospectively diagnosed, and the classification was PMR according to iPERCIST. Nivolumab treatment was maintained for 7.1 months, and survival was 13.8 months
Regarding semi-quantitative analysis with iPERCIST, we monitored the SULpeak of the lesion with highest uptake at SCAN-1 and SCAN-2. The average decrease in SULpeak of the highest uptake lesion was 75% for patients with CMR, 53% for patients with PMR, and 5% for patients with SMD. Among non-responders, SULpeak increased by 55%, on average. In 4/28 patients, we were unable to monitor the SULpeak because the difference between pre-treatment and post-treatment hepatic and blood pool SUL was > 20% (PERCIST recommendation [14]). Among these four patients, two were classified as UPMD due to the appearance of numerous lesions, one was classified as PMR due to the disappearance of all lesions except one, and one was classified as SMD because of the stability of the SULpeak as well as in the size of the lesions.
iPERCIST assessments in the population study are shown in Fig. 4 (responders n = 19, non-responders n = 9). Responders and non-responders did not differ in demographic characteristics (Table 3).
Anti-PD-1 therapy evaluation with iRECIST
Evaluation with iRECIST was also conducted. For the 28 patients, evaluation at SCAN-2 showed PR in 5 patients, SD in 8 patients, CR in 2 patients, and UPD in 13 patients. Among the UPD patients (13/28), 4 were classified with SMD at SCAN-3.
Differences in iPERCIST classification were observed in 11/28 patients. Table 4 illustrates the modification in classification between the two criteria. In total, 5/11 patients were reclassified as PMR instead of as SD with iPERCIST, with a corresponding mean survival higher than the mean survival of the whole population (520 vs 479 days). Two patients were reclassified as PMD instead of as SD, two as SMD instead of as PD, one as CMR instead of as PR, and one as PMR instead of as CR.
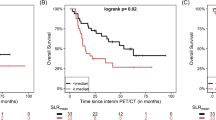
Survival analysis
The median follow-up was 16.7 months (range 3.6–32.2). At the last follow-up, 2/28 patients were still receiving nivolumab. For the other 26 patients, nivolumab was administered for a median of 6.6 months (range 1.1–26.3). Overall, 18/28 patients died during follow-up, and 10 patients were still alive at the end of follow-up (2 patients were still receiving nivolumab at the end of data collection). Responders continued treatment for a mean of 10.7 months (range 3.8–26.3). The 1-year survival rate was 94% for responders and 11% for non-responders. Additionally, OS significantly differed between responders and non-responders (19.9 and 3.6 months, p = 0.0003; Fig. 5). OS curves with iRECIST are shown in Additional file 2: Figure S3.
PET studies evaluating treatment toxicities
One patient had thyroiditis at SCAN-2 (1/28). After the third injection of nivolumab, the thyroid stimulating hormone level decreased from 1.36 to 0.18 mUI/L (normally > 0.27 mUI/L). The patient did not show any symptoms. We did not observe any other features suggestive of adverse autoimmune disease associated with nivolumab (colitis, pancreatitis, hypophysitis, etc.).
Discussion
In this study, FDG PET monitoring with iPERCIST was an effective tool for discerning NSCLC patients who could benefit from treatment with nivolumab. For responders to nivolumab according to iPERCIST (CMR, PMR, or SMD at SCAN-2, or with pseudo-progression confirmed by SCAN-3), the 1-year survival rate was greater than 90%, against 11% for non-responders. Additionally, OS was better for responders than non-responders at 19.9 vs. 3.6 months, p = 0.0003. Therefore, the prognostic value of iPERCIST might help physicians monitor immunotherapy in NSCLC patients.
FDG PET is currently the most widely used molecular imaging modality in clinical practice for staging and restaging NSCLC. However, few data are available for evaluating immunotherapy with FDG PET, especially in lung cancer, for which anti-PD-1 or anti-PDL-1-based immunotherapies are taking a crucial role in treating locally advanced or metastatic tumors [15]. Moreover, because the antineoplastic activity of immunotherapy is related to the activation of T cells against tumor cells, FDG accumulation might cause false-positive findings, as was underlined in RECIST 1.1, evolving the criteria toward iRECIST [8]. Consequently, implementing and evaluating PET-based criteria for immunomodulatory therapy [16] is needed.
We proposed to use iPERCIST derived from PERCIST, which was introduced by R. Wahl in 2009 [13, 14]. We modified iPERCIST by introducing two new categories of response derived from iRECIST: UPMD and CPMD, indicating that all metabolic progression observed at 8 weeks should be confirmed by another PET study 4 weeks later. However, the decision to continue immunotherapy treatment after the first evaluation is based on both clinical and imaging data. As recommended and discussed in the paper from Seymour et al. [8], the continuation of treatment beyond imaging progression (UPMD in iPERCIST) is permitted in patients who are clinically stable until the next assessment. Pseudo-progression is a rare but clearly described condition under PD1 inhibitor treatment in lung cancer [17]. At the time of the study, most of the described cases of pseudo-progression in lung cancer occurred in patients with clinical improvement or stabilization. The available data suggested that the UPMD patients with clinical deterioration had a progressive disease. Although these patients had no SCAN-3, they were followed after stopping immunotherapy; 6/9 UPMD patients showed tumoral progression on their CT scan approximately 2 months after the start of salvage chemotherapy, 2/9 patients died shortly (approximately 1 month) after the stopping nivolumab due to sepsis, and one patient had passed away at follow-up. Nevertheless, since the end of our study, a few case reports of patients with initial clinical worsening followed by a durable response were reported [18].
One important point that should be highlighted is that SMD patients after UPMD are considered metabolic responders with iPERCIST in our study. Indeed, we observed that most SMD patients evaluated by PET after 4–6 cycles of nivolumab treatment had a possible sustained metabolic response. As illustrated in the survival curve in Additional file 3: Figure S2, OS did not significantly differ between SMD patients and CMR + PMR patients when evaluated by iPERCIST.
The comparison of the results obtained with iRECIST and iPERCIST suggests that iPERCIST might be more relevant than iRECIST in terms of prognostic information. Indeed, 11/28 patients (39%) were classified differently with iPERCIST. In a review of the 2016 literature (6 series, 268 patients), discrepancies between RECIST and PERCIST were observed in approximately 38% of tumor responses, in line with our rate of disagreement [19]. In our study, PERCIST allowed five morphologically stable patients to be reclassified as PMR. The OS of these five patients was longer than the OS of the whole study population (520 vs. 459 days, respectively). Similarly, 2/11 patients were reclassified from progressive disease to stable disease, with their OS longer than the OS of the whole study population (573 vs. 459 days, respectively). Two other morphologically stable patients were reclassified as PMD, with their OS shorter than the OS of the whole study population (360 vs. 459 days). These data suggest that reclassification using PERCIST provides additional prognostic information compared to iRECIST in this setting.
Several studies have documented the value of FDG PET in patients receiving nivolumab, whether with large-cell B lymphomas [20] or melanomas [9]. In NSCLC, Kaira et al. recently investigated the role of FDG PET as a biomarker of therapeutic efficacy in a prospective study of 24 patients [21]. The authors showed that changes in FDG uptake evaluated by total lesion glycolysis 1 month after the start of nivolumab had significant prognostic value. Of note, SUVmax or metabolic tumor volumes failed to have prognostic value in multivariate analyses in their study. In addition, PERCIST using SULpeak was not evaluated in their study, although we considered PERCIST to be the most reliable criteria available. Indeed, the superiority of PERCIST over SUVmax has been demonstrated, especially in NSCLC treated with radiotherapy [22] or chemotherapy [23].
However, other authors showed that increased FDG uptake during immunotherapy predicted immune activation and could predict the best overall response [9]. Cho et al. studied the prognostic value of FDG PET 1 month after the start of treatment in patients with melanoma. In patients with stable disease at month 1 according to RECIST 1.1, PET could differentiate between two populations where an increase of 15.5% in SULpeak of the lesion with the highest uptake was associated with eventual clinical benefit (i.e., partial or complete response at 4 months or stable disease ≥ 6 months). The authors interpreted their findings by suggesting that an early inflammatory response at the site of the tumor, induced by boosting immunity, is a marker of a sustained response. This study lacked additional PET imaging after SCAN-2 to confirm the presence of an immune reaction rather than tumoral progression, which could explain the low accuracy and negative predictive value of PERCIST (70% and 42%, respectively) for predicting the best overall response after 4 months, because of the possible misclassification of pseudo-progression in PMD.
Recent studies of melanoma patients receiving ipilimumab and those evaluated by FDG PET suggested the use of new criteria for imaging evaluation [10, 11]. The PET Response Evaluation Criteria for Immunotherapy (PERCIMT) added new criteria defining a threshold of two to four new lesions in an evaluation scan to classify patients under immunotherapy as PMD. Again, a single-time-point evaluation here does not seem reliable enough in the setting of immunotherapy and can lead to a risk of misclassifying pseudo-progression as disease progression. This issue was observed in initial observations, which found that 10% of patients who received ipilimumab for melanoma showed a clinical response (including partial response and stable disease) that would have been misclassified as disease progression by World Health Organization criteria [24]. Using FDG PET, we assumed that the risk of misclassification might be even higher because of the better sensitivity of FDG PET, particularly for detecting small lymph nodes or bone metastasis. Notably, we identified 1 patient (1/28, 4%) with a pseudo-progression, which is in accordance with the rate from the literature that ranges from 0 to 6% [25].
Our study is mainly limited by its retrospective design and potential recruitment bias. Of note, the response rate in our study was higher than that usually reported with studies of nivolumab at 40% compared with 20% reported in a recent publication [4]. The choice of the most relevant imaging test evaluation in the context of immunotherapy treatment is an important issue, particularly considering that CT scans are less expensive and more widely available compared to PET scans. Prospective studies will need to validate the cost-effectiveness of a whole-body metabolic evaluation with FDG PET compared to conventional anatomical assessment. Finally, we did not compare FDG PET with predictive biomarkers, such as PD-L1 expression in tissue sampling [16], because of its unavailability at the time of the study.
Conclusions
FDG PET might be a powerful tool for evaluating the response to anti-PD-1-based immunotherapy, with the ability to identify patients who will benefit the most from treatment. The prognostic value of the newly introduced iPERCIST should be confirmed in large prospective multicentric studies.
Abbreviations
- CMR:
-
Complete metabolic response
- CPMD:
-
Confirmed progressive metabolic disease
- CT:
-
Computed tomography
- FDG:
-
Fluorodeoxyglucose
- iPERCIST:
-
Immune PET Response Criteria in Solid Tumors
- iRECIST:
-
Immune Response Evaluation Criteria in Solid Tumors
- NSCLC:
-
Non-small cell lung carcinoma
- PET:
-
Positron emission tomography/computed tomography
- PMD:
-
Progressive metabolic disease
- PMR:
-
Partial metabolic response
- RECIST:
-
Response Evaluation Criteria in Solid Tumors
- SMD:
-
Stable metabolic disease
- SULpeak:
-
Peak standardized uptake values normalized by lean body mass
- UPMD:
-
Unconfirmed progressive metabolic disease
References
Boyle P, Ferlay J. Cancer incidence and mortality in Europe, 2004. Ann Oncol. 2005;16(3):481–8.
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):359–86.
Molina JR, Yang P, Cassivi SD, Schild SE, Adjei AA. Non-small cell lung cancer: epidemiology, risk factors, treatment, and survivorship. Mayo Clin Proc. 2008;83(5):584–94.
Ramos-Esquivel A, van der Laat A, Rojas-Vigott R, Juárez M, Corrales-Rodríguez L. Anti-PD-1/anti-PD-L1 immunotherapy versus docetaxel for previously treated advanced non-small cell lung cancer: a systematic review and meta-analysis of randomised clinical trials. ESMO Open. 2017;2:e000236.
Borghaei H, Paz-Ares L, Horn L, Spigel DR, Steins M, Ready NE, et al. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med. 2015;373(17):1627–39.
Brahmer J, Reckamp KL, Baas P, Crino L, Eberhardt WE, Poddubskaya E, et al. Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med. 2015;373(2):123–35.
Tsai KK, Pampaloni MH, Hope C, Algazi AP, Ljung B-M, Pincus L, et al. Increased FDG avidity in lymphoid tissue associated with response to combined immune checkpoint blockade. J ImmunoTher Cancer. 2016;4(58):20.
Seymour L, Bogaerts J, Perrone A, Ford R, Schwartz LH, Mandrekar S, et al. iRECIST: guidelines for response criteria for use in trials testing immunotherapeutics. Lancet Oncol. 2017;18(3):143–52.
Cho SY, Lipson EJ, Im H-J, Rowe SP, Gonzalez EM, Blackford A, et al. Prediction of response to immune checkpoint inhibitor therapy using early-time-point (18)F-FDG PET/CT imaging in patients with advanced melanoma. J Nucl Med. 2017;58(9):1421–8.
Anwar H, Sachpekidis C, Winkler J, Kopp-Schneider A, Haberkorn U, Hassel JC, et al. Absolute number of new lesions on (18)F-FDG PET/CT is more predictive of clinical response than SUV changes in metastatic melanoma patients receiving ipilimumab. Eur J Nucl Med Mol Imaging. 2018;45(3):376–83.
Sachpekidis C, Anwar H, Winkler J, Kopp-Schneider A, Larribere L, Haberkorn U, et al. The role of interim (18)F-FDG PET/CT in prediction of response to ipilimumab treatment in metastatic melanoma. Eur J Nucl Med Mol Imaging. 2018;45(8):1289–96.
Pinker K, Riedl C, Weber WA. Evaluating tumor response with FDG PET: updates on PERCIST, comparison with EORTC criteria and clues to future developments. Eur J Nucl Med Mol Imaging. 2017;44(1):55–66.
JH O, Lodge MA, Wahl RL. Practical PERCIST: a simplified guide to PET response criteria in solid tumors 1.0. Radiology. 2016;280(2):576–84.
Wahl RL, Jacene H, Kasamon Y, Lodge MA. From RECIST to PERCIST: evolving considerations for PET response criteria in solid tumors. J Nucl Med. 2009;50(Suppl 1):122S–50S.
Assi HI, Kamphorst AO, Moukalled NM, Ramalingam SS. Immune checkpoint inhibitors in advanced non-small cell lung cancer. Cancer. 2017;124(2):248–61.
Rossi S, Toschi L, Castello A, Grizzi F, Mansi L, Lopci E. Clinical characteristics of patient selection and imaging predictors of outcome in solid tumors treated with checkpoint-inhibitors. Eur J Nucl Med Mol Imaging. 2017;44(13):2310–25.
Dudnik E, Moskovitz M, Daher S, Shamai S, Hanovich E, Grubstein A, et al. Effectiveness and safety of nivolumab in advanced non-small cell lung cancer: the real-life data. Lung Cancer. 2017;126:217–23.
Hochmair MJ, Schwab S, Burghuber OC, Krenbek D, Prosch H. Symptomatic pseudo-progression followed by significant treatment response in two lung cancer patients treated with immunotherapy. Lung Cancer. 2017;113:4–6.
Min SJ, Jang HJ, Kim JH. Comparison of the RECIST and PERCIST criteria in solid tumors: a pooled analysis and review. Oncotarget. 2016;7(19):27848–54.
Dercle L, Seban R-D, Lazarovici J, Schwartz L, Houot R, Ammari S, et al. 18F-FDG PET and CT-scan detect new imaging patterns of response and progression in patients with Hodgkin lymphoma treated by anti-PD1 immune checkpoint inhibitor. J Nucl Med. 2017;59(1):15–24.
Kaira K, Higuchi T, Naruse I, Arisaka Y, Tokue A, Altan B, et al. Metabolic activity by (18)F-FDG-PET/CT is predictive of early response after nivolumab in previously treated NSCLC. Eur J Nucl Med Mol Imaging. 2017;45(1):56–66.
Pierson C, Grinchak T, Sokolovic C, Holland B, Parent T, Bowling M, et al. Response criteria in solid tumors (PERCIST/RECIST) and SUVmax in early-stage non-small cell lung cancer patients treated with stereotactic body radiotherapy. Radiat Oncol. 2018;13(1):34.
Shang J, Ling X, Zhang L, Tang Y, Xiao Z, Cheng Y, et al. Comparison of RECIST, EORTC criteria and PERCIST for evaluation of early response to chemotherapy in patients with non-small-cell lung cancer. Eur J Nucl Med Mol Imaging. 2016;43(11):1945–53.
Wolchok JD, Hoos A, O’Day S, Weber JS, Hamid O, Lebbe C, et al. Guidelines for the evaluation of immune therapy activity in solid tumors: immune-related response criteria. Clin Cancer Res. 2009;15(23):7412–20.
Vrankar M, Unk M. Immune RECIST criteria and symptomatic pseudoprogression in non-small cell lung cancer patients treated with immunotherapy. Radiol Oncol. 2018;18;52(4):365–9.
Zheng M. Classification and pathology of lung cancer. Surg Oncol Clin N Am. 2016;25(3):447–68.
Acknowledgements
Not applicable.
Funding
None.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Author information
Authors and Affiliations
Contributions
LG performed the PET scans, analyzed and interpreted the patient data, and was a major contributor in writing the manuscript. BD performed the clinical evaluations, treatments and follow-up evaluations of the patients, analyzed and interpreted the patient data, and contributed to writing the manuscript. KC performed the clinical evaluations, treatments and follow-up evaluations of the patients, analyzed and interpreted the patient data, and contributed to writing the manuscript. LZ performed the clinical evaluations, treatments and follow-up evaluations of the patients, analyzed and interpreted the patient data, and contributed to writing the manuscript. MS conceived the study, performed the PET scans, analyzed and interpreted the patient data, and was a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The institutional review board approved this retrospective study (Protocol number CLEA-2018-047), and the requirement to obtain informed consent was waived.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Figure S1. 45-year-old women with metastatic lymphoepithelioma-like lung carcinoma treated with a second line of nivolumab. (DOCX 440 kb)
Additional file 2:
Figure S3. Kaplan-Meier curves of overall survival for iRECIST groups: CR+PR, SD and PD (log rank test, p=0.023). (DOCX 67 kb)
Additional file 3:
Figure S2. Kaplan-Meier curves for overall survival with stable metabolic disease (SMD) vs. partial metabolic response (PMR) + complete metabolic response (CMR) (p=0.78). (DOCX 63 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Goldfarb, L., Duchemann, B., Chouahnia, K. et al. Monitoring anti-PD-1-based immunotherapy in non-small cell lung cancer with FDG PET: introduction of iPERCIST. EJNMMI Res 9, 8 (2019). https://doi.org/10.1186/s13550-019-0473-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13550-019-0473-1