Abstract
Background
Peptide receptor radionuclide therapy (PRRT) is routinely used for advanced or metastasized neuroendocrine tumours (NET). To prevent nephrotoxicity, positively charged amino acids (AA) are co-infused. The aim of this study was to correlate the risk for therapy-related hyperkalaemia with the total amount of AA infused.
Methods
Twenty-two patients undergoing PRRT with standard activities of 177Lu-DOTATATE/-TOC were monitored during two following treatment cycles with co-infusion of 75 and 50 g of AA (l-arginine and l-lysine), respectively. Mean serum levels of potassium and other parameters (glomerular filtration rate [GFR], creatinine, blood urea nitrogen [BUN], phosphate, chloride, lactate dehydrogenase) prior to, 4 h and 24 h after AA infusion were compared.
Results
Self-limiting hyperkalaemia (>5.0 mmol/l) resolving after 24 h occurred in 91% (20/22) of patients in both protocols. Potassium levels, BUN, creatinine, GFR, phosphate, chloride and LDH showed a similar range at 4 h after co-infusion of 75 or 50 g of AA, respectively (p?>?0.05). Only GFR and creatinine levels at 24 h varied significantly between the two co-infusion protocols (p?<?0.05).
Conclusions
Hyperkalaemia is a frequent side effect of AA infusion in PRRT. Varying the dose of co-infused amino acids did not impact on the incidence and severity of hyperkalaemia.
Similar content being viewed by others
Background
Peptide receptor radionuclide therapy (PRRT) with radiolabelled somatostatin agonists (90Y- or 177Lu-DOTATOC/-TATE) is routinely used for advanced neuroendocrine tumours (NET) or other entities such as meningioma that overexpress somatostatin receptor subtype II (SSTR II) [1]-[6]. Whereas the high-energy emitter 90Y was first considered more effective, especially in bulky disease [7], some studies reported on higher incidence and severity of side effects like myelosuppression and especially renal toxicity [4],[8]. Since the radiopeptide is reabsorbed at the proximal tubule, subsequent retention may lead to excessive radiation doses and renal failure. In order to prevent significant renal radiopeptide retention, positively charged amino acids (AA) such as l-arginine and l-lysine have been introduced and are used in different protocols for 1 or 2 days [9].
The AA bind to the tubular megalin/cubulin system (which serves as a scavenger system for the reabsorption of AA) and compete with the radiopeptide for reabsorption [10],[11]. The co-administration leads to a significant reduction in the renal absorbed dose [6],[12]. However, side effects like nausea, vomiting and hyperkalaemia have been described [13],[14]. Several authors have reported on the influence of the composition and amount of AA administered on serum potassium levels [11],[13].
The aim of this study was to compare incidence and severity of post-therapeutic hyperkalaemia (>5.0 mmol/l) in patients undergoing PRRT with two different AA infusion regimens administering 50 or 75 g of mixed l-arginine and l-lysine.
Methods
Study design and characterization of the patient cohort
Twenty-two consecutive patients (13 males, 9 females) referred for PRRT received 75 g of l-arginine and l-lysine for the first cycle and 50 g of AA for the second cycle, respectively. Mean age was 58?±?14 years (range, 24 to 82 years). The general inclusion and exclusion criteria as defined by The joint IAEA, EANM and SNMMI practical guidance were applied [9]. Table 1 gives an overview on patients' characteristics.
All patients gave written informed consent to the implementation of standard-of-care PRRT. As this study comprised exclusively retrospective analysis of routinely acquired data, our institutional review board (ethics committee of the Medical Faculty of the University of Würzburg) waived the requirement for additional approval. In October 2013, the amount of AA routinely administered was reduced from 75 to 50 g to comply with the latest joint IAEA, EANM and SNMMI practical guidance[9].
All patients were observed for two consecutive treatment cycles. Admission occurred one day prior to PRRT itself to allow for adequate hydration. During the first treatment cycle, 1,500 ml of standard solution containing 37.5 g of arginine hydrochloride and 37.5 g of lysine hydrochloride (pH, 7.0) was administered within 4 h (0.5 to 1 h prior to PRRT and for a total of 3 to 3.5 h after therapy; infusion rate, 375 ml/h). For the second cycle, 25 g of each AA in a total of 2,000 ml saline was infused within the same time period (0.5 to 1 h prior to PRRT and for a total of 3 to 3.5 h after therapy; infusion rate, 500 ml/h) according to the most recent practical guidance [9]. The AA solutions were produced in-house according to GMP criteria.
For the first treatment cycle, a mean of 7.5?±?0.7 GBq of 177Lu-DOTATATE in 12 ml of normal saline was intravenously infused over 30 min; for the second cycle, 7.6?±?0.3 GBq of 177Lu-DOTATOC was administered.
Preparation of 177Lu-DOTATATE/-TOC
177Lu-DOTATATE/-TOC was prepared using a radiotracer synthesis module (Scintomics, Fürstenfeldbruck, Germany) with minor modifications as described before [15]. Briefly, a solution of 200 ?g DOTATATE/-TOC-acetate (ABX, Radeberg, Germany) and 7 mg gentisic acid in 600 ?l sodium acetate buffer (pH?=?4 to 5) was added to a solution of 8 GBq 177LuCl3 in 0.04 M hydrochloric acid (Isotope Technologies Garching, Garching, Germany) and heated for 30 min at 95°C. The product was diluted with saline and passed through a sterile filter (0.22 ?m) into a sterile vial. Radiochemical purity was determined by gradient high-performance liquid chromatography and thin layer chromatography. Additionally, the product was also tested for pH, sterility and endotoxins.
Pre- and post-therapeutic blood samples
Blood samples of each patient were drawn to assess standard blood values one day before PRRT and 4 and 24 h after AA infusion. Serum levels of potassium and other parameters (glomerular filtration rate [GFR], creatinine, blood urea nitrogen [BUN], phosphate, chloride, lactate dehydrogenase [LDH]) were compared. Whereas hyperkalaemia is routinely defined by our laboratories as serum K+ levels >5.0 mmol/l, severe hyperkalaemia was arbitrarily defined as serum values ?6.0 mmol. Serum potassium levels were measured by indirect ion-sensitive electrode (ISE) (Cobas 8000 system, Roche Diagnostics, Mannheim, Germany). All samples were screened for haemolysis. Absorbances of the diluted serum samples (dilution 1:26) were measured at 570 nm (primary wavelength) and at 600 nm (secondary wavelength), and the haemolysis indices were calculated according to the manufacturer's instruction. Serum samples with haemolysis indices above 90 (equaling 90 mg/dl of free haemoglobin) were considered to be haemolytic and excluded from further evaluation (<5%).
Analysis and statistics
Statistical analyses were performed using PASW Statistics software (version 22.0; SPSS, Inc. Chicago, IL, USA). Quantitative values were expressed as mean?±?standard deviation and range as appropriate. Comparisons of related metric measurements were performed using Wilcoxon signed rank test.
Results
Post-PRRT clinical symptoms
After completion of PRRT, three patients of the 75 g group presented with palpitations, chest pain and/or general discomfort. Evaluation of ECG revealed flattened P waves and high peaked T waves. Two of those three patients also became symptomatic after administration of 50 g AA, whereas the remaining tolerated this regimen without discomfort. In all symptomatic cases, serum potassium levels were ?6.1 mmol/l with peak values of 7.9 mmol/l and required prompt intervention by infusion of 20 IU insulin with 20% glucose in 500 ml saline.
Besides, other side effects being not related to hyperkalaemia were observed in both patient cohorts (e.g. nausea, vomiting and decrease of kidney function).
At baseline, mean K+ levels were 4.4?±?0.4 mmol/l (75 g) and 4.3?±?0.4 mmol/l (50 g), respectively. At 4 h, 20/22 subjects (91%) in both groups had serum potassium levels ?5.0 mmol/l with a mean of 5.8?±?0.7 mmol/l (75 g) and 5.7?±?0.8 mmol/l (50 g), respectively. Increases in K+ levels were comparable (25% for 75 g, p?<?0.001 and 24% for 50 g AA, p?<?0.001).
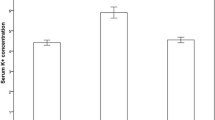
In both groups, severe hyperkalaemia defined as K+ >6.0 mmol/l was observed in 8/22 (36%) patients. After 24 h, K+ levels almost returned to baseline (mean, 4.5?±?0.4 mmol/l (75 g AA) vs. mean, 4.6?±?0.4 (50 g AA)) (Figure 1). No significant differences between both AA protocols were found at any time point.
Serum K+levels. Serum K+ levels at baseline, 4 h post-infusion and 24 h post-infusion (mmol/l; 50 g amino acid vs. 75 g amino acid). **4 h in comparison to baseline (50 g/75 g): p?<?0.001; #4 h in comparison to 24 h (50 g/75 g): p?<?0.001; *24 h in comparison to baseline (50 g): p?<?0.05. Empty bars show serum K+ concentrations after administration of 50 g AA, and full bars show serum K+ concentrations after administration of 75 g AA.
At 4 h post-infusion, all other parameters investigated showed only minor differences. Only glomerular filtration rates (p?=?0.011) and creatinine levels at 24 h (p?=?0.016) varied significantly between 50 g of AA and 75 g of AA (24 h post-infusion, 75 g vs. 50 g). Table 2 gives an overview of all biochemical parameters.
Discussion
This is the first intra-individual comparison of hyperkalaemia induced by 50 or 75 g of nephroprotective amino acids (Arg-Lys) in patients with neuroendocrine tumours undergoing PRRT. Incidence and severity of hyperkalaemia (>5.0 mmol/l) were comparable for both protocols.
In PRRT, AA-induced hyperkalaemia is believed to result from the ketogenic characteristics of lysine, lowering intracellular pH and thereby causing an outwardly directed K+ flux [14]. Various publications have previously reported on AA-induced increase of serum potassium levels. For example, Barone and colleagues found just marginal increase in K+ levels in patients treated with a mixture of arginine and lysine totaling 50 g [11]. However, only six patients were included in this study and blood samples were drawn at an early time point (2.5 h after the start of infusion). Recently, a group from Switzerland reported on hyperkalaemia after administration of 25 g lysine and 25 g arginine. In their cohort, serum potassium levels increased significantly 4 h after the beginning of AA infusion [16]. Last, Rolleman et al. reported on even more pronounced K+ increases induced by 75 g of lysine, warning of AA-induced hyperkalaemia. In our cohort, we observed higher values of potassium than previously reported [13]. The reason for this observation is not fully understood. In order to rule out spurious hyperkalaemia, blood haemolysis indices were calculated. One possible explanation might be the pH value of the amino acid solution administered, which in our department is 7.0. Serum acidosis is known to be associated with potassium movement from the cellular space into the extracellular fluid in order to buffer excess hydrogen ions. The rather high volume infusion of 1,500 ml of AA might affect serum pH and thereby subsequently influence serum potassium. The total amount of AA solution administered did not influence incidence or severity of hyperkalaemia. Therefore, our data hint at a major contribution of the pH of the AA solution which was the same in all cycles.
Both infusion protocols were equally well tolerated. Most of the patients experienced asymptomatic rises in K+, and symptoms resolved quickly within 24 h without any further intervention. Three patients became symptomatic including palpitations, chest pain and general discomfort. Two of those three patients suffered from hyperkalaemia-related side effects regardless of the amount of AA infused, whereas the remaining subject only experienced discomfort with 75 g of AA. Interestingly, this subject had lower K+ values after administration of 50 g AA (6.1 mmol/l) as compared to 75 g AA (7.0 mmol/l). In all, treatment with insulin and glucose was highly effective and symptoms were relieved quickly.
Changes in other serum parameters included a non-significant decrease in phosphate, increase in BUN or changes in chloride which were also not significant, consistent with studies published before [16]. Also, no significant changes in kidney function were observed. According to our study, only a transient increase of serum creatinine after start of the AA infusion has been reported [11] and might be associated with higher doses of AA due to non-specific tubular cell blockade. Resolution was observed after 24 h. In short, hyperkalaemia as an adverse event to a potentially life-threatening degree has to be kept in mind regardless of the AA protocol used for PRRT.
The following limitations have to be considered: firstly, the retrospective study design and the low patient number may be associated with a significant sample bias. Secondly, this study does not allow any conclusions regarding the nephroprotective effect of the different AA amounts. Therefore, future prospective studies with larger patient numbers need to be performed, potentially also investigating the long-term effectiveness and safety of AA co-infusion protocols with even lower AA amounts. However, to the best of our knowledge, this is the first report on an intra-individual comparison of two different AA protocols.
Conclusions
Transient hyperkalaemia is a frequent side effect of AA co-infusion during PRRT. In contrast to previous reports, incidence and severity of hyperkalaemia do not significantly vary between different amounts of AA administered.
References
Modlin IM, Moss SF, Chung DC, Jensen RT, Snyderwine E: Priorities for improving the management of gastroenteropancreatic neuroendocrine tumors. J Natl Cancer Inst 2008, 100: 1282–1289. 10.1093/jnci/djn275
Waser B, Tamma ML, Cescato R, Maecke HR, Reubi JC: Highly efficient in vivo agonist-induced internalization of sst2 receptors in somatostatin target tissues. J Nucl Med 2009, 50: 936–941. 10.2967/jnumed.108.061457
Bergsma H, van Vliet EI, Teunissen JJ, Kam BL, de Herder WW, Peeters RP, Krenning EP, Kwekkeboom DJ: Peptide receptor radionuclide therapy (PRRT) for GEP-NETs. Best Pract Res Clin Gastroenterol 2012, 26: 867–881. 10.1016/j.bpg.2013.01.004
Imhof A, Brunner P, Marincek N, Briel M, Schindler C, Rasch H, Macke HR, Rochlitz C, Muller-Brand J, Walter MA: Response, survival, and long-term toxicity after therapy with the radiolabeled somatostatin analogue [90Y-DOTA]-TOC in metastasized neuroendocrine cancers. J Clin Oncol 2011, 29: 2416¿2423.
Kwekkeboom DJ, de Herder WW, Kam BL, van Eijck CH, van Essen M, Kooij PP, Feelders RA, van Aken MO, Krenning EP: Treatment with the radiolabeled somatostatin analog [177Lu-DOTA0, Tyr3] octreotate: toxicity, efficacy, and survival. J Clin Oncol 2008, 26: 2124¿2130.
Bodei L, Cremonesi M, Grana C, Rocca P, Bartolomei M, Chinol M, Paganelli G: Receptor radionuclide therapy with 90Y-[DOTA] 0-Tyr3-octreotide (90Y-DOTATOC) in neuroendocrine tumours. Eur J Nucl Med Mol Imaging 2004, 31: 1038–1046. 10.1007/s00259-004-1571-4
Forrer F, Waldherr C, Maecke HR, Mueller-Brand J: Targeted radionuclide therapy with90Y-DOTATOC in patients with neuroendocrine tumors. Anticancer Res 2006, 26: 703¿707.
Valkema R, Pauwels SA, Kvols LK, Kwekkeboom DJ, Jamar F, de Jong M, Barone R, Walrand S, Kooij PP, Bakker WH, Lasher J, Krenning EP: Long-term follow-up of renal function after peptide receptor radiation therapy with(90)Y-DOTA(0), Tyr(3)-octreotide and(177)Lu-DOTA(0), Tyr(3)-octreotate. J Nucl Med 2005, 46(Suppl 1):83S¿91S.
Bodei L, Mueller-Brand J, Baum RP, Pavel ME, Horsch D, O'Dorisio MS, O'Dorisio TM, Howe JR, Cremonesi M, Kwekkeboom DJ, Zaknun JJ: The joint IAEA, EANM, and SNMMI practical guidance on peptide receptor radionuclide therapy (PRRNT) in neuroendocrine tumours. Eur J Nucl Med Mol Imaging 2013, 40: 800–816. 10.1007/s00259-012-2330-6
Behr TM, Goldenberg DM, Becker W: Reducing the renal uptake of radiolabeled antibody fragments and peptides for diagnosis and therapy: present status, future prospects and limitations. Eur J Nucl Med 1998, 25: 201–212. 10.1007/s002590050216
Barone R, Pauwels S, De Camps J, Krenning EP, Kvols LK, Smith MC, Bouterfa H, Devuyst O, Jamar F: Metabolic effects of amino acid solutions infused for renal protection during therapy with radiolabelled somatostatin analogues. Nephrol Dial Transplant 2004, 19: 2275–2281. 10.1093/ndt/gfh362
de Jong M, Krenning E: New advances in peptide receptor radionuclide therapy. J Nucl Med 2002, 43: 617–620.
Rolleman EJ, Valkema R, de Jong M, Kooij PP, Krenning EP: Safe and effective inhibition of renal uptake of radiolabelled octreotide by a combination of lysine and arginine. Eur J Nucl Med Mol Imaging 2003, 30: 9–15. 10.1007/s00259-002-0982-3
Bernard BF, Krenning EP, Breeman WA, Rolleman EJ, Bakker WH, Visser TJ, Macke H, de Jong M: D-lysine reduction of indium-111 octreotide and yttrium-90 octreotide renal uptake. J Nucl Med 1997, 38: 1929–1933.
Kwekkeboom DJ, Bakker WH, Kooij PP, Konijnenberg MW, Srinivasan A, Erion JL, Schmidt MA, Bugaj JL, de Jong M, Krenning EP: [177Lu-DOTAOTyr3] octreotate: comparison with [111In-DTPAo] octreotide in patients. Eur J Nucl Med 2001, 28: 1319–1325. 10.1007/s002590100574
Giovacchini G, Nicolas G, Freidank H, Mindt TL, Forrer F: Effect of amino acid infusion on potassium serum levels in neuroendocrine tumour patients treated with targeted radiopeptide therapy. Eur J Nucl Med Mol Imaging 2011, 38: 1675–1682. 10.1007/s00259-011-1826-9
Acknowledgements
We thank Dirk Oliver Mügge (graduate computer scientist, research assistant), University of Innsbruck, Institute of Psychology, Innsbruck, Austria for his valuable contribution in the statistical analysis of the data. This publication was funded by the German Research Foundation (DFG) and the University of Wuerzburg in the funding programme Open Access Publishing.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that there are no competing interests.
Authors¿ contributions
KL, AnS, AKB and KH conceived and designed the study. CB and AlS acquired the data. CL and RAW analyzed and interpreted the data. CL, RAW, CB and AlS were involved in the drafting of the manuscript, and KL, AnS, AKB and KH revised it critically for important intellectual content. All authors gave final approval of the version to be published and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lapa, C., Werner, R.A., Bluemel, C. et al. Influence of the amount of co-infused amino acids on post-therapeutic potassium levels in peptide receptor radionuclide therapy. EJNMMI Res 4, 46 (2014). https://doi.org/10.1186/s13550-014-0046-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13550-014-0046-2