Abstract
Although mesenchymal stem cell (MSC) transplantation provides an alternative strategy for end-stage liver disease (ESLD), further widespread application of MSC therapy is limited owing to low cell engraftment efficiency. Improving cell engraftment efficiency plays a critical role in enhancing MSC therapy for liver diseases. In this review, we summarize the current status and challenges of MSC transplantation for ESLD. We also outline the complicated cell-homing process and highlight how low cell engraftment efficiency is closely related to huge differences in extracellular conditions involved in MSC homing journeys ranging from constant, controlled conditions in vitro to variable and challenging conditions in vivo. Improving cell survival and homing capabilities enhances MSC engraftment efficacy. Therefore, we summarize the current strategies, including hypoxic priming, drug pretreatment, gene modification, and cytokine pretreatment, as well as splenectomy and local irradiation, used to improve MSC survival and homing capability, and enhance cell engraftment and therapeutic efficiency of MSC therapy. We hope that this review will provide new insights into enhancing the efficiency of MSC engraftment in liver diseases.
Similar content being viewed by others
Introduction
End-stage liver diseases (ESLD), including decompensated liver cirrhosis, liver failure, and hepatocellular carcinoma, have high mortality rates, and their prevalence has increased in recent years [1]. ESLD is characterized by severely abnormal liver functions including hepatic decompensation, portal hypertension, coagulation dysfunction, jaundice, hepatorenal syndrome, hepatic encephalopathy, and ascites. Although liver transplantation can effectively treat these diseases [2], most patients die waiting for transplant surgery because of a shortage of donor organs. Mesenchymal stem cells (MSCs) are adult multipotent cells with self-renewal, multi-directional differentiation, immunoregulator, and paracrine functions [3]. Recent findings have demonstrated that MSC transplantation can improve liver function in acute or chronic liver diseases, offering an alternative strategy for patients with ESLD to prolong their life [4,5,6,7,8,9]. The therapeutic functions of MSC transplantation are attributed to the following aspects. First, MSCs serve as substitutes for hepatocytes via transdifferentiation or cell fusion for liver tissue repair and regeneration. Second, MSCs exhibit paracrine functions by releasing growth factors and cytokines that inhibit hepatocyte apoptosis and stimulate liver regeneration. Third, MSCs possess immunomodulatory properties related to adaptive and innate immune responses [10].
According to the potential therapeutic mechanisms of MSC therapy, the paracrine or immunoregulatory actions of MSCs depend on their survival rate in vivo, and the hepatic differentiation or fusion function of MSCs depends on the number of viable MSCs that reached the injured liver tissues. Thus, MSC engraftment efficiency is closely related to cell survival or viability and sufficient delivery of cells to the liver. Actually, Kuo et al. found that survival of MSCs in liver tissues was less than 5% 4 weeks after transplantation [11]. Our previous work showed that a large number of MSCs die within 1 day after transplantation in fibrotic liver of mice, and the surviving MSCs almost completely disappeared 11 days after transplantation [12], indicating an extremely low MSC survival rate in vivo, leading to insufficient cell engraftment efficiency for liver diseases. Therefore, cell attrition has become a major bottleneck in MSC therapy for liver diseases. Improving cell survival and MSC homing capability to enhance cell engraftment efficiency is needed to maximize the therapeutic potential of MSC transplantation in liver diseases.
Various biological, biochemical, and biophysical factors tightly influence MSC survival and homing capabilities through reciprocal interactions between cells, the extracellular matrix, and bioactive factors both in vitro and in vivo [13]. Dramatically different conditions between in vitro and in vivo severely affect MSC survival or viability after transplantation. During in vitro expansion of MSCs, the conditions are optimally controlled including oxygen partial pressure, whereas MSCs encounter a variety of conditions in vivo, including hypoxia and oxidative stress, that affect their ability to home and effectively repopulated liver tissue during transplantation (Fig. 1). Each part of the homing process comprising rolling, activation, adhesion, crawling, and migration (Fig. 2) affects the number of the homing of MSCs to parenchymal liver tissues. Therefore, regulation of biological, biochemical, and/or biophysical factors to reduce cell injuries induced by an unfavorable environment in vivo can improve MSC survival, increase MSC homing capability, and enhance MSC engraftment efficiency. In this review, we discuss the current status of MSC therapy, the detailed cell-homing process, strategies to improve MSC survival, and homing capability to enhance MSC engraftment efficiency in liver diseases.
The dramatic difference between in vitro and in vivo conditions in MSC transplantation for liver diseases. The MSC engraftment process is tortuous, and the transplanted MSCs would encounter dramatic changes ranging from in vitro comfortable growing conditions to in vivo inclement environment (such as hypoxia, oxidative stress, and inflammation), leading to the low cell survival of MSC therapy for liver diseases. Figure designed by Adobe Illustrator CC 2018
Current status and challenges of MSC transplantation for ESLD
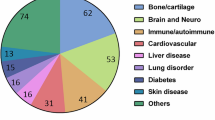
MSCs are adult and multipotent stromal cells that can be isolated from the bone marrow, adipose tissues, umbilical cord, dental tissue, synovium, placenta, and dermis [14]. According to the International Society for Cell and Gene Therapy, MSCs are defined by the following criteria: (1) the cells are adherent under standard culture conditions and grow intrinsically during in vitro expansion or culture; (2) the cell surface makers are positive for CD73, CD90, and CD105, but negative for CD14, CD34, CD45, and HLA-DR; and (3) the cells can differentiate into adipocytes, osteoblasts, or chondrocytes in vitro. In addition to the above properties, MSCs also have immune evasion ability due to low MHC-I antigen expression and lack of MHC-II antigen expression [15], which is a congenital factor for allogeneic or autogenous MSC transplantation [16]. MSC transplantation has been widely used in preclinical studies, for treating ESLD, including liver failure and cirrhosis, indicating its potential for ESLD in humans. A growing number of clinical trials have confirmed the therapeutic potential of MSC transplantation for ESLD, particularly for decompensated liver cirrhosis (DLC) and acute-on-chronic liver failure (ACLF) (Table 1). Li et al. found that the overall survival at 3-year (83.3% vs 61.8%) and 5-year (63.9% vs 43.6%) during the 13- to 75-month follow-up was significantly improved by human umbilical cord blood-derived MSC therapy for DLC patients (n = 36) [17]. In a randomized controlled clinical trial, MSC transplantation improved overall survival and liver function biomarkers (albumin, prothrombin activity, cholinesterase, and total bilirubin during 48 weeks of follow-up) during a 13–75-month follow-up in patients with DLC (n = 108) [18]. No significant side effects or cell-related complications have been observed after MSC therapy in patients with DLC. A randomized controlled trial conducted by Lin et al. found that MSC therapy could increase 24-week survival rates (73.2% vs 55.6%) by improving liver function (total bilirubin and MELD scores) and decreasing the incidence of severe infections (16.1% vs 33.3%) in ACLF patients (n = 56) [19]. However, Mohamadnejad et al. found that in a randomized controlled trial (n = 27, 12 months of follow-up) involving patients with cirrhosis, MSC transplantation did not improve child scores, MELD scores, serum albumin, INR, serum transaminases, or liver volumes [20]. Given the fact that the background and guidelines for liver diseases worldwide are not fully uniform, some large, multicenter clinical trials with long-term follow-up in MSC therapy for subcategories of liver diseases should be conducted to further confirm the clinical benefit of MSC therapy.
More importantly, cell engraftment efficiency, including the survival and number of MSC targeted deliveries into parenchymal liver tissues, should be considered when interpreting the therapeutic efficacy of MSC transplantation for liver diseases. Notably, by performing a series of liver biopsies after 6 months of MSC therapy in patients with cirrhosis (n = 25), Kantarcıoğlu et al. found that MSCs could not be delivered into liver tissues in sufficient amounts [21]. Therefore, a low cell engraftment efficiency severely affects the long-term therapeutic outcomes of MSC therapy for liver diseases. Next, we describe the cell-homing process and how to improve cell engraftment efficiency to enhance the therapeutic efficacy of MSCs for liver diseases.
MSC transplantation and homing process in vivo
Following previous reviews, MSC homing can be divided into systemic and non-systemic [22, 23]. For non-systemic homing, MSCs were locally injected into the targeted sites. In systemic homing, MSCs are administered into the bloodstream, pass through the circulatory system, and finally, transmigrate to targeted sites. In liver diseases, MSC homing is systemic, as MSC transplantation is commonly achieved by intravenous (IV) injection via different routes, including the peripheral and hepatic portal veins. After IV transplantation, MSC are initially retained in the lungs and then, delivered to the liver, spleen, and kidney. Very few MSCs are located in other organs [24]. Although the delivery route affects travel of MSCs to the injured sites, the number of cells that could transmigrate into parenchymal liver tissues was not significantly different between portal and peripheral vein administrations [25,26,27]. Additionally, there were no differences in the therapeutic efficacy of MSCs between peripheral and portal vein administration in acute liver failure [25] or cirrhosis models [26]. Considering that MSC survival and homing capabilities are closely related to the therapeutic efficacy of MSC therapy, IV-injected MSC, regardless of injection site, undergo similar microenvironments in vivo and the same systemic homing process. Correlatively, it has been confirmed that systemic homing is inevitable after IV injection and involves active or passive MSC extravasation followed by chemokine-guided interstitial migration toward injured sites [23]. Similar to endogenous leukocyte migration to inflammatory sites [28, 29], systemically administered MSCs undergo rolling, activation, adhesion, crawling, and migration (Fig. 2).
As an initial step, MSC rolling is commonly facilitated by selectins expressed on endothelial cells. In 2006, Rüster et al. first found that the rolling behavior of MSCs bound to endothelial cells occurred in a P-selectin-dependent manner [30]. However, MSCs do not express P-selectin glycoprotein ligand 1 (PSGL-1), implying that other MSC ligands interact with P-selectin in the endothelial cells. Bailey et al. have identified CD24 as a candidate P-selectin ligand in adipose tissue-derived MSCs [31]. Therefore, engineering MSC surfaces with PSGL-1 and Sialyl-Lewis could increase the effectiveness of MSC therapy in multiple sclerosis [32]. Liver sinusoidal endothelial cells (LSECs) are the only gatekeepers of MSCs that homes to parenchymal liver tissue. Previously, MSC rolling was abolished by blocking CD29 (also known as VLA4, a β1-integrin) on MSCs and vascular cell adhesion molecule-1 (VCAM-1) on LSECs [33]. Hence, cell rolling during MSC therapy for liver diseases depends on CD29/VCAM-1.
Cell activation during MSC homing is usually facilitated by G protein-coupled chemokine receptors (GPCRs), which couple with cytokines secreted by wounds. Extensive evidence has shown that stromal cell-derived factor1 (SDF-1, also known as CXCL-12) in endothelial cells plays a crucial role in cell activation during MSC homing [34]. SDF-1 is also a ligand of the chemokine receptor, CXCR-4, which is commonly expressed in MSCs. Significantly, overexpression of CXCR-4 in MSCs enhanced the therapeutic effect of MSC transplantation on acute liver failure by activating the PI3K/Akt signaling pathway [35]. The number of MSC homing is closely related to SDF-1 expression in injured liver tissues [36]. Therefore, SDF-1 is an important attractant for the targeted delivery of MSCs and the SDF-1/CXCR-4 axis plays a pivotal role in MSC activation and homing. In addition to the SDF-1/CXCR-4 axis, direct interaction between other chemokines and receptors, including CCL-2/CCR-2 [37] and cannabinoid receptor-1 [38], is also involved in the cell engraftment process of MSC therapy for liver diseases. Hence, the expression of the GPCRs plays an important role in cell activation during MSC therapy for liver diseases, but the details of the underlying mechanisms require further exploration.
MSC adhesion is facilitated by integrins. Semon et al. showed that MSC adhesion to endothelial cells, including those in the pulmonary artery, cardiac-derived microvasculature, and umbilical veins, is markedly reduced by β5-integrin antibodies [39]. In liver diseases, Aldridge et al. found that blocking the β1-integrin (CD29) on MSCs significantly reduced their adhesiveness to LSECs, whereas GPCRs, including CCR-4, CCR-5, and CXCR-3, made little contribution to MSC adhesion [33]. Therefore, integrin expression in MSCs affects their adhesion capability during MSC homing.
MSCs crawl on the surface of endothelial cells along with the establishment of firm endothelial adhesion. Cell crawling, the movement along extracellular substrates or matrices (e.g., inner vessel walls), requires exogenous factors, including fluid force, and chemokines at targeted sites [23, 40]. Chamberlain et al. found that shear stress and CXCL-9 significantly enhanced MSC crawling capability on endothelial cells in vitro [29]. Lateral cell crawling is accompanied by MSC polarization, which is initiated by the crosstalk between FROUNT and CCR-2, followed by CCR-2 clustering, leading to cytoskeletal reorganization and further endothelial migration [41].
To accomplish endothelial migration, MSCs must penetrate the barriers of the endothelial cell layers by secreting MMPs (including MMP-1, MMP-2, MMP-9, and MT1-MMP), which can degrade the basement membrane of endothelial cells [42, 43]. The MMP activity is commonly regulated by TIMP-1 [44], microRNAs [45], and inflammatory factors (e.g., IL-1β [46], TGF-β1 [47], and TNFα [43]). Apart from MMPs, other cytokines including CXCR-3 and urokinase-type plasminogen activator induced by inflammatory factors such as IL-1β and IL-17, are also involved in the trans-endothelial migration of MSCs [48, 49].
Strategies for enhancing MSC survival and homing capability in liver diseases
After administration into the bloodstream, MSC will encounter a range of conditions that can influence their survival. The optimal constant conditions that support growth in vitro give way to more inclement, complex conditions in vivo, including low oxygen tensions, fluid pressure stress, and interaction with whole blood components. As a result, many MSCs die in the blood circulation after IV transplantation. Furthermore, following the tortuous homing process, the existing surviving MSCs continue to be subjected to challenging conditions such as hypoxia, oxidative stress, and inflammation in the targeted sites, leading to continuous cell death, such that only a small number of viable MSCs populate the parenchymal liver tissues. The cell attrition dramatically reduces theoretical functions of MSC transplantation in liver diseases. Considering that cell survival and cell-homing capability are closely related to MSC engraftment efficacy, it is necessary to further improve MSC survival and homing capabilities and to maximize the therapeutic efficiency of MSC therapy in liver diseases. Next, we summarized the current strategies for enhancing cell survival and homing capability of MSC transplantation (Fig. 3).
Strategies for enhancing MSC survival and homing capability. The current strategies including hypoxic priming, drug pretreatment, gene modification, cell surface engineering, cytokine pretreatment, splenectomy, nanoparticle labeling, and local irradiation have been used to improve MSC survival and cell-homing capability. Figure designed by Adobe Illustrator CC 2018
Strategies for enhancing MSC survival in vivo
Hypoxic priming
Generally, human arterial blood contains 12.3% O2, venous blood contains 5.3% O2, and the liver tissue contains approximately 4.04% O2 (30.7 mmHg of O2) [50]. Comparing in vitro expansion of normoxic cultured MSCs (NC-MSCs, approximately 19.95% O2), the oxygen dissolution in vivo and the oxygen content in liver tissues and the circulatory system are extremely low. After short-term hypoxic exposure, NC-MSCs were prone to death due to upregulation of Sug1, and the inactivation of 26S proteasome, leading to increased immunogenicity [51, 52], and inducing cell apoptosis [53]. Additionally, NC-MSC stemness is easily lost during extensive amplification in vitro [54]. Hence, it is difficult to adapt in vivo expansion of NC-MSCs to dramatic changes in oxygen pressure. To improve the ability of MSCs to adapt to changes in oxygen, hypoxic priming, an in vitro preconditioning method, has been used to increase their survival in vivo [55, 56]. Hypoxic priming can increase autocrine or paracrine factor secretion by MSCs, including IL-6, TNFα, HGF, VEGF, and prostaglandin E synthase, which promotes liver regeneration and reduces hepatocyte apoptosis [57]. In addition, it prevents MSC senescence by promoting autophagy [58], and downregulating p16, p53, and p21 [59, 60]. Therefore, hypoxic priming has been used to enhance the outcomes of MSC therapy for liver diseases [61] (Table 2).
Drug pretreatment
Accumulating evidence suggests that oxidative stress characterized by the excess generation of reactive oxygen species is a key factor in the low cell survival rate of transplanted MSCs [62]. Antioxidant drugs have been used to overcome oxidative stress and enhance MSC survival in vitro (Table 3). Indeed, our group found that a low dose of reduced glutathione (GSH) and melatonin could be used to preserve MSC functions (including cell proliferation, and stemness) and to reduce cell senescence during long-term in vitro passaging [63]. Importantly, antioxidant pretreatment increased MSC survival by reducing cell apoptosis in an H2O2 injury model [64] and enhanced therapeutic outcomes of MSC therapy for liver fibrosis [64, 65]. Pretreatment with other antioxidants, including edaravone [66], zeaxanthin dipalmitate [67], and vitamin E [68], can also be used to enhance MSC survival and therapeutic efficacy for liver failure.
Similar to oxidative stress, inflammation is another factor affecting MSC survival in vivo. We previously used a ratiometric near infrared-II fluorescence probe to track MSC viability and found that dexamethasone pretreatment could improve MSC cell survival and enhance the hepatic protection of MSC transplantation for liver fibrosis [12]. Moreover, juzentaihoto, a chemical drug with both anti-inflammatory and anti-oxidative functions, has also been used to improve cell survival and to enhance the therapeutic efficiency of MSC transplantation for liver cirrhosis [69]. Considering that some antioxidant and anti-inflammatory drugs (e.g., GSH) have been used clinically in patients with ESLD, drug pretreatment is a promising clinical strategy for enhancing MSC survival and therapeutic efficacy for liver diseases.
Gene modification
Given that miR-210 is closely involved in cell survival under hypoxia or oxidative stress, its overexpression has been used to enhance MSC survival under hypoxic conditions [67] or oxidative stress induced by H2O2 [70], thereby improving the repair function of MSC transplantation. Overexpression of anti-apoptotic, antioxidant, or pro-survival genes including BCL-2 [71, 72], Akt1 [73], HGF [74], GATA-4 [75], and erythropoietin (EPO) [76], significantly enhanced MSC survival in vitro and in vivo. In addition, down-regulation of miR-34a [77], and miR-16 [78] enhanced MSC survival by reducing apoptosis. Therefore, modifying gene expression to reduce cell apoptosis and/or improve the adaptability to hypoxia and oxidative stress is an alternative method for enhancing MSC survival in vivo.
Strategies for enhancing MSC homing capability in vivo
MSC modification in vitro
Gene modification
The entire process of MSC homing is medicated by the crosstalk between ligands and receptors. Increasing the expression ligands or receptors on MSCs improves their homing capability. Overexpression migration-related genes, including CXCR-4 [79], CCR-2 [80], CXCL-9 [81], and c-Met [82], have been used to increase MSC homing. Gene modification also significantly enhances the therapeutic efficacy of MSCs for acute or chronic liver diseases (Table 4).
Cell surface engineering
Cell surface engineering to decorate a targeted molecule on the cell surface has been used to enhance MSC delivery to the target sites [83]. Previously, human adipose tissue-derived MSC surfaces were engineered with lipid-conjugated heparin to increase hepatic homing of MSCs and improve MSC therapy for acute liver failure [84,85,86]. Given that LSECs are a specific permeable barrier of the hepatic sinusoidal endothelium for trans-endothelial migration of MSC transplantation, we used bioorthogonal click chemistry to modify the MSC surface with an LSEC-targeted peptide (RLTRKRGLK) to increase MSC homing capability to enhance MSC therapy for acute liver failure and liver fibrosis [87]. Importantly, neither heparin-functionalization nor the bioorthogonal click chemistry approach affected the biological characteristics of the MSCs. Therefore, these cell surface engineering strategies are a promising for enhancing MSC homing capability.
Cytokine pretreatment
Pretreatment with cytokines, including IL-17 [88] and HGF [89], improved MSC migration and homing ability in vivo. Recently, Nie et al. found that IL-1β pretreatment increased CXCR-4 expression and enhanced MSC homing capability and therapeutic outcomes for acute liver failure [46]. Pretreatment with TGFβ1 enhanced the homing and engraftment of MSCs to human and murine hepatic sinusoidal endothelia in vivo and in vitro, which was mediated by increased expression of CXCR-3. In particular, pretreatment with cytokine can enhance the anti-inflammatory effects of MSC therapy in acute liver injury [90]. Because cytokines can be easily controlled within the GMP grade, cytokine pretreatment provides translational potential for improving the MSC homing capacity for liver diseases.
Nanoparticle labeling
Nanoparticle-based imaging has been widely used for in vivo assessment of MSC biodistribution. Huang et al. developed an iron-based nanocluster for MSC labeling and found that it enhanced MSC migration by promoting CXCR-4 expression [91]. Similarly, Vitale et al. developed silica nanoparticles (SiO2-NPs) for MSC tracking and found that their internalization enhanced MSC migration by increasing CXCR-4 expression [92]. Hence, silica nanoparticle labeling is a novel method for improving the homing capabilities of MSCs. Nevertheless, the detailed mechanism and safety profile of nanoparticle labeling for increasing CXCR-4 expression remain unknown.
Host environment regulation
Splenectomy
Portal hypertension is a typical physical condition aggravated by cirrhosis. Previously, it was suggested that the flow shear stress benefits the osteogenic, cardiovascular, chondrogenic, adipogenic, and neurogenic differentiation of MSCs [93]. However, high shear stress and portal hypertension hamper the adhesion and migration of MSCs. Splenectomy is a therapeutic option for increasing platelet count and promoting liver regeneration in patients with portal hypertension and cirrhosis. In particular, Tang et al. found that splenectomy enhanced MSC homing capability and therapeutic efficacy for cirrhosis of the liver in rats by upregulating of SDF-1 and HGF [94]. Nevertheless, the detailed mechanism and safety of this approach still need to be verified before clinical application.
Transient local irradiation
Considering that transient local irradiation (TLR) can disturb the LSEC barrier and inhibit the phagocytic function of Kupffer cells, TLR has been used to enhance hepatocyte engraftment in hepatectomized mice [95]. Inspired by this, Shao et al. used hepatic TLR to enhance MSC homing and therapeutic outcomes for thioacetamide-induced fibrosis in rats [96]. Hence, TLR is an alternative method for improving the MSC homing capability. However, this approach increases the risk of tissue injury, and its clinical benefits should be fully evaluated before further application.
Conclusions and future directions
Here, we review the whole cell-homing process of MSC transplantation and the current clinical status of MSC therapy for liver diseases, emphasizing that low cell engraftment efficiency is a major challenge to the use and the long-term therapeutic efficacy of MSC therapy. We also highlighted that cell survival and MSC transmigration into the parenchymal liver tissues is closely related to the efficiency of MSC engraftment. Therefore, we summarized the current strategies to enhance cell survival and homing capability for MSC transplantation in liver diseases. Nevertheless, there are many unanswered questions regarding the safety and the clinical potential of these strategies. First, although pretreatment with drugs, hypoxia, and cytokines can improve MSC survival or homing capability, they also affect the paracrine functions of MSCs; hence, future studies are still needed. Second, modifying MSCs to enhance their homing capability through gene editing, nanoparticle labeling, or chemical methods is an alternative approach for enhancing MSC engraftment efficiency; however, biosafety issues and how to achieve GMP-grade cell production requires further exploration. Third, splenectomy or TLR poses an external risk to patients, and the clinical benefit should be fully verified before implementation in clinical settings. Finally, the current strategies are supported by in vitro and animal studies, but their clinical translational potentials for improving cell survival and homing capability of MSC therapy in liver diseases remain to be tested.
Apart from cell survival and homing capability, there are a large number of variables, including the heterogeneity of MSCs derived from different tissues and individual differences in patients, which affect cell engraftment efficiency and personalized MSC therapy for liver diseases. There is a clear need to develop personalized models to address therapeutic efficacy of MSC transplantation in liver diseases.
Availability of data and materials
Not applicable.
Abbreviations
- α-SMA:
-
α-Smooth muscle actin
- ACLF:
-
Acute-on-chronic liver failure
- ADSC:
-
Adipose-derived MSC
- AF-MSC:
-
Amniotic-fluid-derived MSC
- ALB:
-
Albumin
- ALF:
-
Acute liver failure
- ALT:
-
Alanine aminotransferase
- AKT:
-
Protein kinase B
- AMM:
-
Amniotic mesenchymal stem cell
- AST:
-
Aspartate transaminase
- BCAT1:
-
Branched‐chain amino acid transaminase‐1
- BM-MSC:
-
Bone marrow-derived MSC
- CCR-2:
-
CC Chemokine receptor 2
- CD29:
-
β1-Integrin
- CHE:
-
Cholinesterase
- CI:
-
Central intravenous
- C-met:
-
Cellular-mesenchymal epithelial transition factor
- CXCR-4:
-
C-X-C chemokine receptor type 4
- CXCL-2:
-
C-X-C chemokine ligand 2
- CXCL-9:
-
C-X-C chemokine ligand 9
- DLC:
-
Decompensated liver cirrhosis
- ESLD:
-
End-stage liver diseases
- EPO:
-
Erythropoietin
- FGF4:
-
Fibroblast growth factor 4
- FOXO:
-
Forkhead box O
- GSH:
-
Glutathione
- HBV:
-
Hepatic B virus
- HCC:
-
Hepatocellular carcinoma
- HCV:
-
Hepatic C virus
- hFoxa2:
-
Human Forkhead box A2
- HGF:
-
Hepatocyte growth factor
- HSC:
-
Hepatic stellate cell
- IAI:
-
Intrahepatic arterial injection
- IL-1Ra:
-
Interleukin-1-receptor antagonist
- IL-6:
-
Interleukin-6
- IL-10:
-
Interleukin 10
- INR:
-
International normalized ratio
- ISI:
-
Intrasplenic injection
- IV:
-
Intravenous injection
- LC:
-
Liver cirrhosis
- LF:
-
Liver failure
- LPS:
-
Lipopolysaccharides
- LT:
-
Liver transplantation
- LSECs:
-
Liver sinusoidal endothelial cells
- MELD:
-
Model for end-stage liver disease
- MMP-9:
-
Matrix metalloproteinase 9
- MSC:
-
Mesenchymal stem cell
- NRF-2:
-
Nuclear factor erythroid 2-related factor 2
- OS:
-
Overall survival
- PBC:
-
Primary biliary cirrhosis
- PC:
-
Prothrombin concentration
- PCNA:
-
Proliferating cell nuclear antigen
- PGE-2:
-
Prostaglandin E2
- PD-MSC:
-
Placenta-derived MSC
- PI:
-
Portal injection
- PRL-1:
-
Phosphatase of regenerating liver-1
- PSGL-1:
-
P-selectin glycoprotein ligand 1
- PT:
-
Prothrombin time
- PVI:
-
Peripheral vein injection
- ROS:
-
Reactive oxygen species
- SDF-1:
-
Stromal cell-derived factor1
- Tbil:
-
Total bilirubin
- TGFβ1:
-
Transforming growth factorβ1
- TLR:
-
Transient local irradiation
- TNF-α:
-
Tumor necrosis factor α
- UC-MSC:
-
Umbilical cord-derived mesenchymal stem cell
- VCAM-1:
-
Vascular cell adhesion molecule-1
- VEGF:
-
Vascular endothelial growth factor
- VEGF165 :
-
Vascular endothelial growth factor 165
References
Asrani SK, Devarbhavi H, Eaton J, Kamath PS. Burden of liver diseases in the world. J Hepatol. 2019;70:151–71.
Forbes SJ, Gupta S, Dhawan A. Cell therapy for liver disease: from liver transplantation to cell factory. J Hepatol. 2015;62:S157–69.
Yang X, Meng Y, Han Z, Ye F, Wei L, Zong C. Mesenchymal stem cell therapy for liver disease: full of chances and challenges. Cell Biosci. 2020;10:123.
Zhang L, Ma XJ, Fei YY, Han HT, Xu J, Cheng L, et al. Stem cell therapy in liver regeneration: focus on mesenchymal stem cells and induced pluripotent stem cells. Pharmacol Ther. 2022;232:108004.
Hu X-H, Chen L, Wu H, Tang Y-B, Zheng Q-M, Wei X-Y, et al. Cell therapy in end-stage liver disease: replace and remodel. Stem Cell Res Ther. 2023;14:141.
Khan S, Mahgoub S, Fallatah N, Lalor PF, Newsome PN. Liver disease and cell therapy: advances made and remaining challenges. Stem Cells. 2023;41:739–61.
Cardinale V, Lanthier N, Baptista PM, Carpino G, Carnevale G, Orlando G, et al. Cell transplantation-based regenerative medicine in liver diseases. Stem Cell Rep. 2023;18:1555–72.
Chen L, Zhang N, Huang Y, Zhang Q, Fang Y, Fu J, Yuan Y, Chen L, Chen X, Xu Z, Li Y, Izawa H, Xiang C. Multiple Dimensions of using Mesenchymal Stem Cells for Treating Liver Diseases: From Bench to Beside. Stem Cell Rev Rep. 2023. https://doi.org/10.1007/s12015-023-10583-5
Yang X, Li Q, Liu W, Zong C, Wei L, Shi Y, et al. Mesenchymal stromal cells in hepatic fibrosis/cirrhosis: from pathogenesis to treatment. Cell Mol Immunol. 2023;20:583–99.
Liu WH, Song FQ, Ren LN, Guo WQ, Wang T, Feng YX, et al. The multiple functional roles of mesenchymal stem cells in participating in treating liver diseases. J Cell Mol Med. 2014;19:511–20.
Kuo TK, Hung SP, Chuang CH, Chen CT, Shih YR, Fang SC, et al. Stem cell therapy for liver disease: parameters governing the success of using bone marrow mesenchymal stem cells. Gastroenterology. 2008;134:2111–21.
Liao NS, Su L, Cao Y, Qiu L, Xie R, Peng F, et al. Tracking cell viability for adipose-derived mesenchymal stem cell-based therapy by quantitative fluorescence Imaging in the second near-Infrared window. ACS Nano. 2022;16:2889–900.
Noronha NC, Mizukami A, Caliari-Oliveira C, Cominal JG, Rocha JLM, Covas DT, et al. Priming approaches to improve the efficacy of mesenchymal stromal cell-based therapies. Stem Cell Res Ther. 2019;10:131.
Keating A. Mesenchymal stromal cells: new directions. Cell Stem Cell. 2012;10:709–16.
Ankrum JA, Ong JF, Karp JM. Mesenchymal stem cells: immune evasive, not immune privileged. Nat Biotechnol. 2014;32:252–60.
Gebler A, Zabel O, Seliger B. The immunomodulatory capacity of mesenchymal stem cells. Trends Mol Med. 2012;18:128–34.
Li Z, Zhou X, Han L, Shi M, Xiao H, Lin M, et al. Human umbilical cord blood-derived mesenchymal stem cell transplantation for patients with decompensated liver cirrhosis. J Gastrointest Surg. 2023;27:926–31.
Shi M, Li YY, Xu RN, Meng FP, Yu SJ, Fu JL, et al. Mesenchymal stem cell therapy in decompensated liver cirrhosis: a long-term follow-up analysis of the randomized controlled clinical trial. Hepatol Int. 2021;15:1431–41.
Lin BL, Chen JF, Qiu WH, Wang KW, Xie DY, Chen XY, et al. Allogeneic bone marrow-derived mesenchymal stromal cells for hepatitis B virus-related acute-on-chronic liver failure: a randomized controlled trial. Hepatology. 2017;66:209–19.
Mohamadnejad M, Alimoghaddam K, Bagheri M, Ashrafi M, Abdollahzadeh L, Akhlaghpoor S, et al. Randomized placebo-controlled trial of mesenchymal stem cell transplantation in decompensated cirrhosis. Liver Int. 2013;33:1490–6.
Kantarcioglu M, Demirci H, Avcu F, Karslioglu Y, Babayigit MA, Karaman B, et al. Efficacy of autologous mesenchymal stem cell transplantation in patients with liver cirrhosis. Turk J Gastroenterol. 2015;26:244–50.
Ullah M, Liu DD, Thakor AS. Mesenchymal stromal cell homing: mechanisms and strategies for improvement. iScience. 2019;15:421–38.
Nitzsche F, Muller C, Lukomska B, Jolkkonen J, Deten A, Boltze J. Concise review: MSC adhesion cascade-insights into homing and transendothelial migration. Stem Cells. 2017;35:1446–60.
Sanchez-Diaz M, Quinones-Vico MI, Sanabria de la Torre R, Montero-Vilchez T, Sierra-Sanchez A, Molina-Leyva A, et al. Biodistribution of mesenchymal stromal cells after administration in animal models and humans: a systematic review. J Clin Med. 2021;10:2925.
Sun L, Fan X, Zhang L, Shi G, Aili M, Lu X, et al. Bone mesenchymal stem cell transplantation via four routes for the treatment of acute liver failure in rats. Int J Mol Med. 2014;34:987–96.
Truong NH, Nguyen NH, Le TV, Vu NB, Huynh N, Nguyen TV, et al. Comparison of the treatment efficiency of bone marrow-derived mesenchymal stem cell transplantation via tail and portal veins in CCl4-induced mouse liver fibrosis. Stem Cells Int. 2016;2016:5720413.
Idriss NK, Sayyed HG, Osama A, Sabry D. Treatment efficiency of different routes of bone marrow-derived mesenchymal stem cell injection in rat liver fibrosis model. Cell Physiol Biochem. 2018;48:2161–71.
Uchida N, Nassehi T, Drysdale CM, Gamer J, Yapundich M, Bonifacino AC, et al. Busulfan combined with immunosuppression allows efficient engraftment of gene-modified cells in a rhesus macaque model. Mol Ther. 2019;27:1586–96.
Chamberlain G, Smith H, Rainger GE, Middleton J. Mesenchymal stem cells exhibit firm adhesion, crawling, spreading and transmigration across aortic endothelial cells: effects of chemokines and shear. PLoS ONE. 2011;6:e25663.
Ruster B, Gottig S, Ludwig RJ, Bistrian R, Muller S, Seifried E, et al. Mesenchymal stem cells display coordinated rolling and adhesion behavior on endothelial cells. Blood. 2006;108:3938–44.
Bailey AM, Lawrence MB, Shang H, Katz AJ, Peirce SM. Agent-based model of therapeutic adipose-derived stromal cell trafficking during ischemia predicts ability to roll on P-selectin. PLoS Comput Biol. 2009;5:e1000294.
Liao W, Pham V, Liu L, Riazifar M, Pone EJ, Zhang SX, et al. Mesenchymal stem cells engineered to express selectin ligands and IL-10 exert enhanced therapeutic efficacy in murine experimental autoimmune encephalomyelitis. Biomaterials. 2016;77:87–97.
Aldridge V, Garg A, Davies N, Bartlett DC, Youster J, Beard H, et al. Human mesenchymal stem cells are recruited to injured liver in a beta1-integrin and CD44 dependent manner. Hepatology. 2012;56:1063–73.
Liepelt A, Tacke F. Stromal cell-derived factor-1 (SDF-1) as a target in liver diseases. Am J Physiol Gastrointest Liver Physiol. 2016;311:G203–9.
Xiu G, Li X, Yin Y, Li J, Li B, Chen X, et al. SDF-1/CXCR4 augments the therapeutic effect of bone marrow mesenchymal stem cells in the treatment of lipopolysaccharide-induced liver injury by promoting their migration through PI3K/Akt signaling pathway. Cell Transplant. 2020;29:1–12.
Jin W, Liang X, Brooks A, Futrega K, Liu X, Doran MR, et al. Modelling of the SDF-1/CXCR4 regulated in vivo homing of therapeutic mesenchymal stem/stromal cells in mice. PeerJ. 2018;6:e6072.
Xu R, Ni B, Wang L, Shan J, Pan L, He Y, et al. CCR2-overexpressing mesenchymal stem cells targeting damaged liver enhance recovery of acute liver failure. Stem Cell Res Ther. 2022;13:55.
Wang L, Yang L, Tian L, Mai P, Jia S, Yang L, et al. Cannabinoid receptor 1 mediates homing of bone marrow-derived mesenchymal stem cells triggered by chronic liver injury. J Cell Physiol. 2017;232:110–21.
Semon JA, Nagy LH, Llamas CB, Tucker HA, Lee RH, Prockop DJ. Integrin expression and integrin-mediated adhesion in vitro of human multipotent stromal cells (MSCs) to endothelial cells from various blood vessels. Cell Tissue Res. 2010;341:147–58.
Bershadsky AD, Kozlov MM. Crawling cell locomotion revisited. Proc Natl Acad Sci U S A. 2011;108:20275–6.
Belema-Bedada F, Uchida S, Martire A, Kostin S, Braun T. Efficient homing of multipotent adult mesenchymal stem cells depends on FROUNT-mediated clustering of CCR2. Cell Stem Cell. 2008;2:566–75.
Kim HY, Yoon HS, Lee Y, Kim YH, Cho KA, Woo SY, et al. Matrix metalloproteinase 1 as a marker of tonsil-derived mesenchymal stem cells to assess bone marrow cell migration. Tissue Eng Regen Med. 2023;20:271–84.
Almalki SG, Agrawal DK. Effects of matrix metalloproteinases on the fate of mesenchymal stem cells. Stem Cell Res Ther. 2016;7:129.
Ries C, Egea V, Karow M, Kolb H, Jochum M, Neth P. MMP-2, MT1-MMP, and TIMP-2 are essential for the invasive capacity of human mesenchymal stem cells: differential regulation by inflammatory cytokines. Blood. 2007;109:4055–63.
Lv C, Yang S, Chen X, Zhu X, Lin W, Wang L, et al. MicroRNA-21 promotes bone mesenchymal stem cells migration in vitro by activating PI3K/Akt/MMPs pathway. J Clin Neurosci. 2017;46:156–62.
Nie H, An F, Mei J, Yang C, Zhan Q, Zhang Q. IL-1beta pretreatment improves the efficacy of mesenchymal stem cells on acute liver failure by enhancing CXCR4 expression. Stem Cells Int. 2020;2020:1498315.
Zhao W, Wang C, Liu R, Wei C, Duan J, Liu K, et al. Effect of TGF-beta1 on the migration and recruitment of mesenchymal stem cells after vascular balloon injury: involvement of matrix metalloproteinase-14. Sci Rep. 2016;6:21176.
Krstic J, Obradovic H, Jaukovic A, Okic-Dordevic I, Trivanovic D, Kukolj T, et al. Urokinase type plasminogen activator mediates Interleukin-17-induced peripheral blood mesenchymal stem cell motility and transendothelial migration. Biochim Biophys Acta. 2015;1853:431–44.
Guo YC, Chiu YH, Chen CP, Wang HS. Interleukin-1beta induces CXCR3-mediated chemotaxis to promote umbilical cord mesenchymal stem cell transendothelial migration. Stem Cell Res Ther. 2018;9:281.
Carreau A, El Hafny-Rahbi B, Matejuk A, Grillon C, Kieda C. Why is the partial oxygen pressure of human tissues a crucial parameter? Small molecules and hypoxia. J Cell Mol Med. 2011;15:1239–53.
Abu-El-Rub E, Sareen N, Lester Sequiera G, Ammar HI, Yan W, ShamsEldeen AM, et al. Hypoxia-induced increase in Sug1 leads to poor post-transplantation survival of allogeneic mesenchymal stem cells. FASEB J. 2020;34:12860–76.
Abu-El-Rub E, Sequiera GL, Sareen N, Yan W, Moudgil M, Sabbir MG, et al. Hypoxia-induced 26S proteasome dysfunction increases immunogenicity of mesenchymal stem cells. Cell Death Dis. 2019;10:90.
Zhang F, Luo H, Peng W, Wang L, Wang T, Xie Z, et al. Hypoxic condition induced H3K27me3 modification of the LncRNA Tmem235 promoter thus supporting apoptosis of BMSCs. Apoptosis. 2022;27:762–77.
Choi W, Kwon SJ, Jin HJ, Jeong SY, Choi SJ, Oh W, et al. Optimization of culture conditions for rapid clinical-scale expansion of human umbilical cord blood-derived mesenchymal stem cells. Clin Transl Med. 2017;6:38.
Hu C, Wu Z, Li L. Pre-treatments enhance the therapeutic effects of mesenchymal stem cells in liver diseases. J Cell Mol Med. 2020;24:40–9.
Zhang Z, Yang C, Shen M, Yang M, Jin Z, Ding L, et al. Autophagy mediates the beneficial effect of hypoxic preconditioning on bone marrow mesenchymal stem cells for the therapy of myocardial infarction. Stem Cell Res Ther. 2017;8:89.
Kojima Y, Tsuchiya A, Ogawa M, Nojiri S, Takeuchi S, Watanabe T, et al. Mesenchymal stem cells cultured under hypoxic conditions had a greater therapeutic effect on mice with liver cirrhosis compared to those cultured under normal oxygen conditions. Regen Ther. 2019;11:269–81.
Liu J, He J, Ge L, Xiao H, Huang Y, Zeng L, et al. Hypoxic preconditioning rejuvenates mesenchymal stem cells and enhances neuroprotection following intracerebral hemorrhage via the mir-326-mediated autophagy. Stem Cell Res Ther. 2021;12:413.
Kim Y, Jin HJ, Heo J, Ju H, Lee HY, Kim S, et al. Small hypoxia-primed mesenchymal stem cells attenuate graft-versus-host disease. Leukemia. 2018;32:2672–84.
Liu H, Xue W, Ge G, Luo X, Li Y, Xiang H, et al. Hypoxic preconditioning advances CXCR4 and CXCR7 expression by activating HIF-1alpha in MSCs. Biochem Biophys Res Commun. 2010;401:509–15.
Yu J, Yin S, Zhang W, Gao F, Liu Y, Chen Z, et al. Hypoxia preconditioned bone marrow mesenchymal stem cells promote liver regeneration in a rat massive hepatectomy model. Stem Cell Res Ther. 2013;4:83.
Yang YX, Fei WY, Liu MS, Zhang YC, Gao RS, Hu YY, et al. Molecular hydrogen promotes adipose-derived stem cell myogenic differentiation via regulation of mitochondria. Curr Stem Cell Res Ther. 2022;18:864–75.
Liao N, Shi Y, Zhang C, Zheng Y, Wang Y, Zhao B, et al. Antioxidants inhibit cell senescence and preserve stemness of adipose tissue-derived stem cells by reducing ROS generation during long-term in vitro expansion. Stem Cell Res Ther. 2019;10:306.
Liao N, Shi Y, Wang Y, Liao F, Zhao B, Zheng Y, et al. Antioxidant preconditioning improves therapeutic outcomes of adipose tissue-derived mesenchymal stem cells through enhancing intrahepatic engraftment efficiency in a mouse liver fibrosis model. Stem Cell Res Ther. 2020;11:237.
Mortezaee K, Khanlarkhani N, Sabbaghziarani F, Nekoonam S, Majidpoor J, Hosseini A, et al. Preconditioning with melatonin improves therapeutic outcomes of bone marrow-derived mesenchymal stem cells in targeting liver fibrosis induced by CCl4. Cell Tissue Res. 2017;369:303–12.
Zeng W, Xiao J, Zheng G, Xing F, Tipoe GL, Wang X, et al. Antioxidant treatment enhances human mesenchymal stem cell anti-stress ability and therapeutic efficacy in an acute liver failure model. Sci Rep. 2015;5:11100.
Liu Y, Xiong Y, Xing F, Gao H, Wang X, He L, et al. Precise regulation of mir-210 is critical for the cellular homeostasis maintenance and transplantation efficacy enhancement of mesenchymal stem cells in acute liver failure therapy. Cell Transplant. 2017;26:805–20.
Baig MT, Ghufran H, Mehmood A, Azam M, Humayun S, Riazuddin S. Vitamin E pretreated Wharton’s jelly-derived mesenchymal stem cells attenuate CCl(4)-induced hepatocyte injury in vitro and liver fibrosis in vivo. Biochem Pharmacol. 2021;186:114480.
Iwasawa T, Nojiri S, Tsuchiya A, Takeuchi S, Watanabe T, Ogawa M, et al. Combination therapy of Juzentaihoto and mesenchymal stem cells attenuates liver damage and regresses fibrosis in mice. Regen Ther. 2021;18:231–41.
Xu J, Huang Z, Lin L, Fu M, Gao Y, Shen Y, et al. miR-210 over-expression enhances mesenchymal stem cell survival in an oxidative stress environment through antioxidation and c-Met pathway activation. Sci China Life Sci. 2014;57:989–97.
Jin S, Li H, Han M, Ruan M, Liu Z, Zhang F, et al. Mesenchymal stem cells with enhanced Bcl-2 expression promote liver recovery in a rat model of hepatic cirrhosis. Cell Physiol Biochem. 2016;40:1117–28.
Ni X, Ou C, Guo J, Liu B, Zhang J, Wu Z, et al. Lentiviral vector-mediated co-overexpression of VEGF and Bcl-2 improves mesenchymal stem cell survival and enhances paracrine effects in vitro. Int J Mol Med. 2017;40:418–26.
Zhou L, Liu S, Wang Z, Yao J, Cao W, Chen S, et al. Bone marrow-derived mesenchymal stem cells modified with Akt1 ameliorates acute liver GVHD. Biol Proced Online. 2019;21:24.
Zhao L, Liu X, Zhang Y, Liang X, Ding Y, Xu Y, et al. Enhanced cell survival and paracrine effects of mesenchymal stem cells overexpressing hepatocyte growth factor promote cardioprotection in myocardial infarction. Exp Cell Res. 2016;344:30–9.
Yu B, Gong M, He Z, Wang YG, Millard RW, Ashraf M, et al. Enhanced mesenchymal stem cell survival induced by GATA-4 overexpression is partially mediated by regulation of the miR-15 family. Int J Biochem Cell Biol. 2013;45:2724–35.
Wang X, Wang H, Lu J, Feng Z, Liu Z, Song H, et al. Erythropoietin-modified mesenchymal stem cells enhance anti-fibrosis efficacy in mouse liver fibrosis model. Tissue Eng Regen Med. 2020;17:683–93.
Liu Y, Zhang X, Chen J, Li T. Inhibition of mircoRNA-34a enhances survival of human bone marrow mesenchymal stromal/stem cells under oxidative stress. Med Sci Monit. 2018;24:264–71.
Prakash A, Garcia-Moreno JF, Brown JAL, Bourke E. Clinically applicable inhibitors impacting genome stability. Molecules. 2018;23:1166.
Du Z, Wei C, Yan J, Han B, Zhang M, Peng C, et al. Mesenchymal stem cells overexpressing C-X-C chemokine receptor type 4 improve early liver regeneration of small-for-size liver grafts. Liver Transpl. 2013;19:215–25.
Zheng J, Li H, He L, Huang Y, Cai J, Chen L, et al. Preconditioning of umbilical cord-derived mesenchymal stem cells by rapamycin increases cell migration and ameliorates liver ischaemia/reperfusion injury in mice via the CXCR4/CXCL12 axis. Cell Prolif. 2019;52:e12546.
Li Y, Dong J, Zhou Y, Ye X, Cai Z, Zhang X, et al. Therapeutic effects of CXCL9-overexpressing human umbilical cord mesenchymal stem cells on liver fibrosis in rats. Biochem Biophys Res Commun. 2021;584:87–94.
Wang K, Li Y, Zhu T, Zhang Y, Li W, Lin W, et al. Overexpression of c-Met in bone marrow mesenchymal stem cells improves their effectiveness in homing and repair of acute liver failure. Stem Cell Res Ther. 2017;8:162.
Won YW, Patel AN, Bull DA. Cell surface engineering to enhance mesenchymal stem cell migration toward an SDF-1 gradient. Biomaterials. 2014;35:5627–35.
Hwang Y, Kim JC, Tae G. Significantly enhanced recovery of acute liver failure by liver targeted delivery of stem cells via heparin functionalization. Biomaterials. 2019;209:67–78.
Liao L, Shi B, Chang H, Su X, Zhang L, Bi C, et al. Heparin improves BMSC cell therapy: anticoagulant treatment by heparin improves the safety and therapeutic effect of bone marrow-derived mesenchymal stem cell cytotherapy. Theranostics. 2017;7:106–16.
Kim J, Tae G. The modulation of biodistribution of stem cells by anchoring lipid-conjugated heparin on the cell surface. J Control Release. 2015;217:128–37.
Liao N, Zhang D, Wu M, Yang H, Liu X, Song J. Enhancing therapeutic effects and in vivo tracking of adipose tissue-derived mesenchymal stem cells for liver injury using bioorthogonal click chemistry. Nanoscale. 2020;13:1813–22.
Ma T, Wang X, Jiao Y, Wang H, Qi Y, Gong H, et al. Interleukin 17 (IL-17)-induced mesenchymal stem cells prolong the survival of allogeneic skin grafts. Ann Transplant. 2018;23:615–21.
Liu J, Pan G, Liang T, Huang P. HGF/c-Met signaling mediated mesenchymal stem cell-induced liver recovery in intestinal ischemia reperfusion model. Int J Med Sci. 2014;11:626–33.
Garg A, Khan S, Luu N, Nicholas DJ, Day V, King AL, et al. TGFbeta(1) priming enhances CXCR3-mediated mesenchymal stromal cell engraftment to the liver and enhances anti-inflammatory efficacy. J Cell Mol Med. 2023;27:864–78.
Huang X, Zhang F, Wang Y, Sun X, Choi KY, Liu D, et al. Design considerations of iron-based nanoclusters for noninvasive tracking of mesenchymal stem cell homing. ACS Nano. 2014;8:4403–14.
Vitale E, Rossin D, Perveen S, Miletto I, Lo Iacono M, Rastaldo R, et al. Silica nanoparticle internalization improves chemotactic behaviour of human mesenchymal stem cells acting on the SDF1alpha/CXCR4 axis. Biomedicines. 2022;10:336.
Arora S, Srinivasan A, Leung CM, Toh YC. Bio-mimicking shear stress environments for enhancing mesenchymal stem cell differentiation. Curr Stem Cell Res Ther. 2020;15:414–27.
Tang WP, Akahoshi T, Piao JS, Narahara S, Murata M, Kawano T, et al. Splenectomy enhances the therapeutic effect of adipose tissue-derived mesenchymal stem cell infusion on cirrhosis rats. Liver Int. 2016;36:1151–9.
Yamanouchi K, Zhou H, Roy-Chowdhury N, Macaluso F, Liu L, Yamamoto T, et al. Hepatic irradiation augments engraftment of donor cells following hepatocyte transplantation. Hepatology. 2009;49:258–67.
Shao CH, Chen SL, Dong TF, Chai H, Yu Y, Deng L, et al. Transplantation of bone marrow-derived mesenchymal stem cells after regional hepatic irradiation ameliorates thioacetamide-induced liver fibrosis in rats. J Surg Res. 2014;186:408–16.
Alimoghaddam K, Mohamadnejad M, Mohyedin Bonab M, Bagheri M, Bashtar M, Ghanati H, et al. Phase 1 Trial of autologous bone marrow mesenchymal stem cell transplantation in patients with decompensated liver cirrhosis. Arch Iran Med. 2008;10:459–66.
Terai S, Ishikawa T, Omori K, Aoyama K, Marumoto Y, Urata Y, et al. Improved liver function in patients with liver cirrhosis after autologous bone marrow cell infusion therapy. Stem Cells. 2006;24:2292–8.
Amin MA, Sabry D, Rashed LA, Aref WM, el-Ghobary MA, Farhan MS, et al. Short-term evaluation of autologous transplantation of bone marrow-derived mesenchymal stem cells in patients with cirrhosis: Egyptian study. Clin Transplant. 2013;27:607–12.
Jang YO, Kim YJ, Baik SK, Kim MY, Eom YW, Cho MY, et al. Histological improvement following administration of autologous bone marrow-derived mesenchymal stem cells for alcoholic cirrhosis: a pilot study. Liver Int. 2014;34:33–41.
Wang L, Li J, Liu H, Li Y, Fu J, Sun Y, et al. Pilot study of umbilical cord-derived mesenchymal stem cell transfusion in patients with primary biliary cirrhosis. J Gastroenterol Hepatol. 2013;28(Suppl 1):85–92.
Zhang Z, Lin H, Shi M, Xu R, Fu J, Lv J, et al. Human umbilical cord mesenchymal stem cells improve liver function and ascites in decompensated liver cirrhosis patients. J Gastroenterol Hepatol. 2012;27(Suppl 2):112–20.
Wang L, Han Q, Chen H, Wang K, Shan GL, Kong F, et al. Allogeneic bone marrow mesenchymal stem cell transplantation in patients with UDCA-resistant primary biliary cirrhosis. Stem Cells Dev. 2014;23:2482–9.
El-Ansary M, Abdel-Aziz I, Mogawer S, Abdel-Hamid S, Hammam O, Teaema S, et al. Phase II trial: undifferentiated versus differentiated autologous mesenchymal stem cells transplantation in Egyptian patients with HCV induced liver cirrhosis. Stem Cell Rev Rep. 2012;8:972–81.
Kharaziha P, Hellstrom PM, Noorinayer B, Farzaneh F, Aghajani K, Jafari F, et al. Improvement of liver function in liver cirrhosis patients after autologous mesenchymal stem cell injection: a phase I-II clinical trial. Eur J Gastroenterol Hepatol. 2009;21:1199–205.
Terai S, Tanimoto H, Maeda M, Zaitsu J, Hisanaga T, Iwamoto T, et al. Timeline for development of autologous bone marrow infusion (ABMi) therapy and perspective for future stem cell therapy. J Gastroenterol. 2012;47:491–7.
Salama H, Zekri AR, Medhat E, Al Alim SA, Ahmed OS, Bahnassy AA, et al. Peripheral vein infusion of autologous mesenchymal stem cells in Egyptian HCV-positive patients with end-stage liver disease. Stem Cell Res Ther. 2014;5:70.
Xue HL, Zeng WZ, Wu XL, Jiang MD, Zheng SM, Zhang Y, et al. Clinical therapeutic effects of human umbilical cord-derived mesenchymal stem cells transplantation in the treatment of end-stage liver disease. Transplant Proc. 2015;47:412–8.
Suk KT, Yoon JH, Kim MY, Kim CW, Kim JK, Park H, et al. Transplantation with autologous bone marrow-derived mesenchymal stem cells for alcoholic cirrhosis: phase 2 trial. Hepatology. 2016;64:2185–97.
Rajaram R, Subramani B, Abdullah BJJ, Mahadeva S. Mesenchymal stem cell therapy for advanced liver cirrhosis: a case report. JGH Open. 2017;1:153–5.
Fang X, Liu L, Dong J, Zhang J, Song H, Song Y, et al. A study about immunomodulatory effect and efficacy and prognosis of human umbilical cord mesenchymal stem cells in patients with chronic hepatitis B-induced decompensated liver cirrhosis. J Gastroenterol Hepatol. 2018;33:774–80.
Sakai Y, Fukunishi S, Takamura M, Kawaguchi K, Inoue O, Usui S, et al. Clinical trial of autologous adipose tissue-derived regenerative (stem) cells therapy for exploration of its safety and efficacy. Regen Ther. 2021;18:97–101.
Sakai Y, Takamura M, Seki A, Sunagozaka H, Terashima T, Komura T, et al. Phase I clinical study of liver regenerative therapy for cirrhosis by intrahepatic arterial infusion of freshly isolated autologous adipose tissue-derived stromal/stem (regenerative) cell. Regen Ther. 2017;6:52–64.
Peng L, Xie DY, Lin BL, Liu J, Zhu HP, Xie C, et al. Autologous bone marrow mesenchymal stem cell transplantation in liver failure patients caused by hepatitis B: short-term and long-term outcomes. Hepatology. 2011;54:820–8.
Amer ME, El-Sayed SZ, El-Kheir WA, Gabr H, Gomaa AA, El-Noomani N, et al. Clinical and laboratory evaluation of patients with end-stage liver cell failure injected with bone marrow-derived hepatocyte-like cells. Eur J Gastroenterol Hepatol. 2011;23:936–41.
Detry O, Vandermeulen M, Delbouille MH, Somja J, Bletard N, Briquet A, et al. Infusion of mesenchymal stromal cells after deceased liver transplantation: a phase I–II, open-label, clinical study. J Hepatol. 2017;67:47–55.
Li Y, Xu Y, Wu HM, Yang J, Yang LH, Yue-Meng W. Umbilical cord-derived mesenchymal stem cell transplantation in hepatitis B virus related acute-on-chronic liver failure treated with plasma exchange and entecavir: a 24-month prospective study. Stem Cell Rev Rep. 2016;12:645–53.
Shi M, Zhang Z, Xu R, Lin H, Fu J, Zou Z, et al. Human mesenchymal stem cell transfusion is safe and improves liver function in acute-on-chronic liver failure patients. Stem Cells Transl Med. 2012;1:725–31.
Nolta JA, Meyerrose TE, Rosova I. Working toward better tissue repair therapies: exposure of MSC to hypoxic conditions in vitro increases levels of the hepatocyte growth factor receptor c-met, improves motility, and induces phosphorylation of the pro-survival protein AKT. Blood. 2005;106:2313.
Wang Z, Wang L, Jiang R, Li C, Chen X, Xiao H, et al. Ginsenoside Rg1 prevents bone marrow mesenchymal stem cell senescence via NRF2 and PI3K/Akt signaling. Free Radic Biol Med. 2021;174:182–94.
Li X, Wang T, Liu J, Liu Y, Zhang J, Lin J, et al. Effect and mechanism of wedelolactone as antioxidant-coumestan on OH-treated mesenchymal stem cells. Arab J Chem. 2020;13:184–92.
Mohammadi S, Barzegari A, Dehnad A, Barar J, Omidi Y. Astaxanthin protects mesenchymal stem cells from oxidative stress by direct scavenging of free radicals and modulation of cell signaling. Chem Biol Interact. 2021;333:109324.
Zhou H, Yang J, Xin T, Li D, Guo J, Hu S, et al. Exendin-4 protects adipose-derived mesenchymal stem cells from apoptosis induced by hydrogen peroxide through the PI3K/Akt-Sfrp2 pathways. Free Radic Biol Med. 2014;77:363–75.
Li X, Xie H, Jiang Q, Wei G, Lin L, Li C, et al. The mechanism of (+) taxifolin’s protective antioxidant effect for *OH-treated bone marrow-derived mesenchymal stem cells. Cell Mol Biol Lett. 2017;22:31.
Li S, Bian H, Liu Z, Wang Y, Dai J, He W, et al. Chlorogenic acid protects MSCs against oxidative stress by altering FOXO family genes and activating intrinsic pathway. Eur J Pharmacol. 2012;674:65–72.
Huang CK, Lee SO, Lai KP, Ma WL, Lin TH, Tsai MY, et al. Targeting androgen receptor in bone marrow mesenchymal stem cells leads to better transplantation therapy efficacy in liver cirrhosis. Hepatology. 2013;57:1550–63.
Zheng YB, Zhang XH, Huang ZL, Lin CS, Lai J, Gu YR, et al. Amniotic-fluid-derived mesenchymal stem cells overexpressing interleukin-1 receptor antagonist improve fulminant hepatic failure. PLoS ONE. 2012;7:e41392.
Kim JY, Jun JH, Park SY, Yang SW, Bae SH, Kim GJ. Dynamic regulation of miRNA expression by functionally enhanced placental mesenchymal stem cells promotes hepatic regeneration in a rat model with bile duct ligation. Int J Mol Sci. 2019;20:5299.
Wang J, Xu L, Chen Q, Zhang Y, Hu Y, Yan L. Bone mesenchymal stem cells overexpressing FGF4 contribute to liver regeneration in an animal model of liver cirrhosis. Int J Clin Exp Med. 2015;8:12774–82.
Lai L, Chen J, Wei X, Huang M, Hu X, Yang R, et al. Transplantation of MSCs overexpressing HGF into a rat model of liver fibrosis. Mol Imaging Biol. 2016;18:43–51.
Cho JW, Lee CY, Ko Y. Therapeutic potential of mesenchymal stem cells overexpressing human forkhead box A2 gene in the regeneration of damaged liver tissues. J Gastroenterol Hepatol. 2012;27:1362–70.
Choi JS, Jeong IS, Han JH, Cheon SH, Kim SW. IL-10-secreting human MSCs generated by TALEN gene editing ameliorate liver fibrosis through enhanced anti-fibrotic activity. Biomater Sci. 2019;7:1078–87.
Hu G, Cui Z, Chen X, Sun F, Li T, Li C, et al. Suppressing mesenchymal stromal cell ferroptosis via targeting a metabolism-epigenetics axis corrects their poor retention and insufficient healing benefits in the injured liver milieu. Adv Sci (Weinh). 2023;10(13):e2206439.
Chen H, Tang S, Liao J, Liu M, Lin Y. VEGF165 gene-modified human umbilical cord blood mesenchymal stem cells protect against acute liver failure in rats. J Gene Med. 2021;23(10):e3369.
Acknowledgements
Not applicable.
Funding
This study was supported by the National Natural Science Foundation of Fujian (No. 2020J011152), Major Scientific Research Program for Young and Middle-aged Health Professionals of Fujian Province,China (No. 2021ZQNZD014), and the Project of Fuzhou Science and Technology Department (No. 2020-WS-56).
Author information
Authors and Affiliations
Contributions
SY, SaY and HL searched literatures, collected data. SY and NL and wrote the initial draft of the manuscript. NL and XL designed tables and revised the manuscript. All the authors reviewed and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yu, S., Yu, S., Liu, H. et al. Enhancing mesenchymal stem cell survival and homing capability to improve cell engraftment efficacy for liver diseases. Stem Cell Res Ther 14, 235 (2023). https://doi.org/10.1186/s13287-023-03476-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13287-023-03476-4