Abstract
Background
A limited number of studies have described thrombotic complications in pregnant women with COVID-19. Here we report on fatal pulmonary embolism in a pregnant woman with laboratory confirmed SARS-CoV-2 infection.
Case presentation
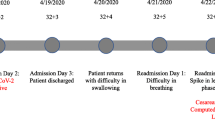
A 28-year-old Kazakh woman was hospitalized with muscle pain, dry cough and a temperature of 37.5 °C at the 29th week of gestation. Upon admission, a blood test demonstrated elevated neutrophil-to-lymphocyte ratio, decreased levels of erythrocytes and hemoglobin, as well as prolonged prothrombin and activated partial thromboplastin time. Within 14 days of admission, she experienced respiratory distress and underwent transfer to the intensive care unit, intubation and a cesarean section. The patient received intravenous antibiotics, antiviral medications, systemic corticosteroids and dual anticoagulation with aspirin and enoxaparin. Death outcome was reported on day 18 of illness despite aggressive supportive care. Histological analysis demonstrated that obstruction of the main pulmonary arthery and disseminated intravascular coagulation were the causes of death.
Conclusions
This case demonstrates that in the management of pregnancy and childbirth in patients with suspected or confirmed COVID-19 infection, special attention should be paid to coagulation system parameters and timely appropriate prophylaxis of thromboembolic complications, which has yet to be determined.
Similar content being viewed by others
Background
First registered in December, 2019 in Wuhan, Hubei Province, China, coronavirus disease 2019 (COVID-19) spread all over the world affecting more than 766 million people, as of May 22, 2023 [1]. It is caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), which primarily affects the respiratory system [2]. According to the data of Johns Hopkins University School of Medicine, the case fatality rate of COVID-19 ranges between 0.2% and 9.2% depending on the country [3]. Older people and people with underlying medical conditions are attributed to the groups at increased risk for severe illness from COVID-19. The Centers for Disease Control and Prevention (CDC) report that pregnant women are also at increased risk for severe illness from COVID-19 [4].
Information available so far suggests that COVID-19 during pregnancy rarely affects fetal and neonatal mortality [5,6,7]. The information on COVID-19-related maternal mortality continues to be updated. Initial reports from China did not indicate fatal outcomes among pregnant women with COVID-19 [8]. A systemic review of 230 cases found that the mortality of pregnant women with COVID-19 was lower than that of overall COVID-19 patients and similar to the average maternal mortality rate worldwide (1 in 180 cases) [7]. A number of national population-based cohort studies demonstrated that among women with SARS-CoV-2 infection, pregnancy was associated with increased rates of intensive care unit (ICU) admission and the need for mechanical ventilation but not death [9,10,11]. In contrast, as of November, 2020, an updated report from CDC on 409,462 women showed that COVID-19 was associated with a higher risk of death among pregnant women when compared to non-pregnant women [12]. Similar results were obtained in an anlysis of data from more than 11,400 women with confirmed or suspected COVID-19 [13]. Alarming data on high fatality rates among COVID-19-infected pregnant women have been reported in some countries [14, 15]. According to the official data, a more than twofold increase in the maternal mortality rate was observed in Kazakhstan in 2020 during the initial wave of COVID-19 (36.5 deaths per 100,000 live births as compared to 13.7 deaths per 100,000 live births in 2019) [16]. Of course, some of this mortality can be attributed to the insufficient quality of prenatal and antenatal care, as well as the lack of hospital resources (medical staff, medications) to manage critical situations due to the pandemic. Nevertheless, the statistics might also reflect the direct impact of the disease on pregnancy. Therefore, clinicians are encouraged to publish case reports providing information on the disease course, treatment and outcomes of SARS-CoV-2 infection in pregnancy with the final aim to prevent other deaths.
In this study, we report on the disease progression, delivery and lethal outcome in a 28-year-old Kazakh woman with no preexisting comorbidities admitted to a hospital at the 29th week of pregnancy with PCR-confirmed COVID-19, and then discuss the case.
Objectivs and study design
We retrospectively reviewed medical records of a pregnant woman diagnosed with COVID-19. The woman spent the entire diagnosis and treatment process at the Rudny City Hospital, Kazakhstan, under the care of medical staff. This study was reviewed and approved by the Ethics Committee of the National Center for Biotechnology (approval #4 issued on September 8, 2020).
Case presentation
On June 23, 2020, the patient, a 28-year-old Kazakh woman at the 29th week of pregnancy, Gravida 3 Para 3, developed a dry cough, followed by an elevated temperature of 37.5 °C and muscle pain on the next day. Antipyretics had no effect, and the cough worsened.
On day 5 of illness, she was admitted to the hospital with a diagnosis of acute viral respiratory infection, presumably COVID-19. On examination, she looked pale, had shortness of breath at rest that worsened with mild exertion, and cough with mucopurulent sputum that was difficult to clear. The pharynx was moderately hyperemic. The patient had a temperature of 37.1 °C, a pulse of 89/minute, a blood pressure of 100/60 mmHg, 18 breaths per minute at rest, a normal chest auscultation, and an oxygen saturation (SpO2) of 99% on room air. Body mass index, calculated as weight in kilograms divided by height in meters squared, was 18.9. The liver and spleen were not enlarged. No swelling in the lower extremities were observed. Bimanual examination showed soft uterus enlarged to the size of 29 weeks of gestation and a normal longitudinal position of the fetus. Neurologic examination revealed no abnormalities, the patient was conscious and able to make contacts without difficulty. She had a history of mild chronic iron-deficiency anemia and positive ELISA-test results for IgG to cytomegalovirus and herpes simplex virus, but no other significant medical history. The patient was employed in a nursing home. She lived with her husband and three children. The patient did not smoke or consume alcohol and denied any family history of vascular or other chronic problems. No problems were noted during regular prenatal examinations, so she was not receiving any medications prior hospitalization.
Upon admission, a SARS-CoV-2 PCR test of a nasopharyngeal swab confirmed the diagnosis COVID-19. According to the protocols established in Kazakhstan at that time for the treatment of COVID-19 in pregnant women, antimicrobal treatment (1.0 g ceftriaxone intramuscularly twice daily for 3 days, then 1.0 g ertapenem intravenously once daily for 11 days and 400 mg moxifloxacin intravenously twice daily for 11 days, 100 ml fluconazole 2 mg/ml intravenously once) was initiated.
On day 7 after onset of symptoms, the patient's condition worsened with a respiratory rate of 27–31 breaths per minute at rest, tachycardia up to 120/min and 93% SpO2. Performed chest radiography showed 2-sided total pneumonia. The patient was transferred to the ICU, where non-invasive ventilation was initiated. The laboratory findings included elevated neutrophil-to-lymphocyte ratio and erythrocyte sedimentation rate, decreased erythrocytes and hemoglobin, as well as prolonged prothrombin (PT) and activated partial thromboplastin (APTT) time (Table 1). The patient received antiretroviral drugs (200 mg lopinavir and 50 mg ritonavir orally twice daily for 9 days), glucocorticosteroids (8 mg dexamethasone intravenously twice daily for 11 days) and anticoagulants (100 mg aspirin orally once daily for 11 days and 40 mg enoxaparin subcutaneously once daily for 11 days).
On day 8 of illness, the patient’s respiratory status acutely deteriorated. The oxygen saturation dropped to 85% SpO2 prompting further investigation with computed tomography (CT). A CT scan showed multiple ground-glass opacities located in the subpleural and middle zones of multiple lobes of both lungs (Fig. 1). A total of 84% of both lungs was affected. No pathological changes in the large vessels of the upper mediastinum, heart, pericardium or esophagus were found. Lymph nodes (paratracheal and aortopulmonary) were not enlarged. The patient was intubated. Puncture and catheterization of the right jugular vein were performed.
On day 10, the patient complained of weakness, increased fetal activity and recurrent frequent moderate pain in the lower abdomen. A cough with difficulty separating mucopurulent sputum was noticed. Given the threatening condition for the fetus, an emergency delivery through a cesarean section was performed. A 1,400 g female newborn was delivered at the 30th week of gestation. SARS-CoV2 PCR test was performed with a nasopharyngeal swab and the result was negative. After the surgery, the patient was transported back to the ICU for continued ventilation and supportive care. A standard of care included 200 ml normal saline once, 100 ml of 20% albumin intravenously once, 5% ketamine intramuscularly once daily for 3 days, 100 mg ketoprofen intramuscularly twice daily for 6 days, arduan once, 25 mg atracurium besilate intravenously once daily for 5 days, 5 IU oxytocin intramuscularly once daily for 4 days, 5 mg metoclopramide intravenously once.
On day 13 of illness, arterial blood gasses demonstrated worsening metabolic acidosis. The laboratory analysis showed increased alanine transaminase and aspartate transaminase together with a decreased total protein level suggesting multiple organ failure (Table 1). The patient was placed in the prone position.
On day 17 of illness, the patient's condition remained critical. Prolonged mechanical ventilation with sedation by propofol was initiated (500 mg propofol twice daily). Monitoring of blood pressure showed fluctuations from 90/60 mmHg to 100/65 mmHg and a pulse of 89/min.
On day 18, the patient experienced acute hypotension (blood pressure of 70/45 mmHg), tachycardia (pulse of 167/min) and a fever of 40.0 °C. Later that day, despite maximal ventilator support a lethal outcome was reported. The clinical details of the patient are shown in Table 1 and the chest CT image is shown in Fig. 1.
Performed autopsy demonstrated complete thrombotic occlusion of the main pulmonary arthery lumen. Widespread hemorrhage and vascular thrombosis in the lungs, kidneys, uterus, heart and liver were detected. Lung histological findings included pulmonary atelectasis, exudate with erythrocytes, fibrin filaments in the lumen of the alveoli, eosinophilic deposits on the walls of the alveoli, hyalinosis, and blood clots in the vessels.
After rehabilitation, the newborn was released to the care of his father in satisfactory condition. Subsequently, he developed normally.
Discussion
Here, we present the fatal case of a 28-year-old female patient Gravida 3 Para 3 at 29-week gestation, with a normal body mass index, and no vascular history, who was hospitalized in 2020 with COVID-19. Despite treatment with prophylactic doses of enoxaparin, she died 8 days after cesarean section from pulmonary embolism and disseminated intravascular coagulation. This case represents one of the few available reports of maternal death due to thromboembolic disorders despite thromboprophylaxis.
It is now clear that SARS-CoV-2 elicits systemic inflammation, which results in an imbalance between procoagulant and anticoagulant homeostatic mechanisms leading to thromboembolic disorders [17]. The cumulative rate of thromboembolic events in COVID-19 patients reaches 21%, rising from 7% of patients admitted to the general ward to 28% of patients in the ICU [18]. We believe that the hypercoagulability associated with pregnancy may increase the risk for thromboembolic disorders associated with COVID-19 even more in pregnant women. Large-scale epidemiological studies are needed to confirm or deny this pressing statement. The aim of this study was to demonstrate an urgent need for development of a standardized protocol for thrombosis monitoring and thromboprophylaxis in pregnant women with COVID-19.
Our patient was a 28-year-old pregnant woman who presented with a cough and muscle aches, which alongside with fever have been earlier found to be the most frequently reported symptoms of COVID-19 in both pregnant and non-pregnant women [13]. No serious preexisting comorbidities putting the patient above baseline population risk (gestational diabetes mellitus and subclinical hypothyroidism, hypertension, obesity, cardiovascular diseases, asthma or renal diseases) or previous thrombotic complications have been reported in the patient's history. A 30-week newborn delivered through a cesarean section had normal birth weight and a negative COVID-19 status. Vertical transmission is rarely reported in COVID-19 patients [7] and was not the case in this study.
Laboratory examination of coagulation indicators upon patient’s admission demonstrated slightly elevated D-dimer levels, prolonged PT and APTT, alongside with fibrinogen levels and platelet counts within the normal range. Given the disorder of three coagulation indicators, therapy with prophylactic doses of low molecular weight heparin (LMWH) and aspirin was initiated. However, despite the young age, negative history for thrombosis and adequate antithrombotic prophylaxis with both anticoagulant and antiplatelet drugs, on the eighth day after cesarean delivery she developed a large pulmonary artery embolus and disseminated intravascular coagulation, which led to her death.
Similarly to our case, a recently published case report presented a COVID-19-positive 29-year old women at the 38th week of pregnancy who developed a pulmonary embolism after cesarean delivery despite prophylaxis [19]. Antithrombotic treatment with intermediate doses of LMWH (enoxaparin subcutaneously 60 mg daily) was started in view of her pregnancy and an elevated D-dimer level (1.50 µg/mL). However, on the second day after cesarean delivery the patient was diagnosed with pulmonary thromboembolism in the right lower lobar pulmonary artery. Both cases strongly demonstrate that high degree of clinical suspicion of venous thromboembolism should be adopted for pregnant patients even if they receive antithrombotic prophylaxis.
Lessons to be learned from the case study: D-dimer plays a key role in thromboembolism events [20]. It has been shown that D-dimer levels greater than 1 μg/mL upon admission predict poor prognosis in nonpregnant patients with COVID-19 [21]. One recent study found a sensitivity of 85.0% and specificity of 88.5% for diagnosing VTE in patients with D-dimer levels greater than 1.5 μg/mL [22]. However, D-dimer is difficult to interpret in pregnancy. It has been demonstrated that D-dimer levels were above the conventional cut-off point (0.5 µg/mL) in 99% of pregnant women in the third trimester [23]. In our patient, the levels of D-dimer were shown to be slightly elevated upon admission, suggesting that pulmonary embolism occurred later. Unfortunately, the test was not performed in the later period of hospitalization, which did not let the physicians fully address hemostatic changes after the cesarean section and augment anticoagulation. D-dimer alongside with other coagulation markers have to be vigorously monitored in pregnant women with COVID-19 on a daily basis especially after cesarean delivery due to coexisting prothrombotic conditions. Increased D-dimer levels may prompt pulmonary angiography examination and intensification of anticoagulation. The use of intermediate therapeutic doses of LMWH should be considered on an individual basis in such patients.
The study also demonstrates that in agreement with recommendations of the International Society on Thrombosis and Haemostasis Subcommittee for Women's Health Issues in Thrombosis and Hemostasis [24], prolonged PT and APTT at any stage of hospitalization should not be considered as a contraindication for thromboprophylaxis in pregnant women, but should prompt further evaluation of other coagulation markers.
Another factor to consider is the use of corticosteroids in pregnant women. It has been shown that mortality at 28 days was significantly lower in patients with COVID-19 who received dexamethasone than in those who received standard treatment alone [25]. Regarding the dose of dexamethasone prescribed to the patient in this study (8 mg twice daily), a lower incidence of adverse events was observed in patients with COVID-19 who received 8 mg once daily than in patients who received higher doses of dexamethasone [26]. On the other hand, the beneficial effects of glucocorticoid treatment received by the patient may have been counteracted by adverse effects on coagulation and fibrinolysis. A number of studies have identified glucocorticoid as a risk factor for venous thromboembolism [27,28,29]. It is difficult to evaluate the risk–benefit of glucocorticoid treatment in this particular case, especially since there are no adequate and well-controlled studies of corticosteroid treatment in pregnant women. Nevertheless, special caution should be exercised when prescribing corticosteroids in preganat women, especially in those with impaired coagulation parameters.
Conclusion
The risk of thromboembolic events associated with pregnancy is approximately ten times higher than outside of pregnancy. Cesarean delivery is another risk factor for development of venous thromboembolism. On the other hand, it has been shown that COVID-19 is also associated with coagulation dysfunctions. Thus, pregnant women with COVID-19 have at least two risk factors, and cesarean delivery is the third risk factor for developing thromboembolic complications. Therefore, management of pregnancy and childbirth in the presence of suspected or confirmed COVID-19 infection requires a special attention to the monitoring of coagulation markers and timely appropriate prophylaxis of thromboembolic complications, especially when deciding on a cesarean section.
Availability of data and materials
Not applicable.
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus-2
- CDC:
-
The Centers for Disease Control and Prevention
- ICU:
-
Intensive care unit
- PCR:
-
Polymerase chain reaction
- ELISA:
-
Enzyme-linked immunosorbent assay
- PT:
-
Prothrombin time
- APTT:
-
Activated partial thromboplastin time
- CT:
-
Computed tomography
- LMWH:
-
Low molecular weight heparin
References
WHO Coronavirus (COVID-19) dashboard. World Health Organisation. https://covid19.who.int. Accessed 24 Aug 2021.
Hu B, Guo H, Zhou P, Shi ZL. Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol. 2020;19:145–54.
Mortality analysis. Johns Hopkins Coronavirus resourse center. https://coronavirus.jhu.edu/data/mortality. Accessed 24 Aug 2021.
Pregnant people. About COVID-19. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/pregnant-people.html. Accessed 24 Aug 2021.
Yoon SH, Kang JM, Ahn JG. Clinical outcomes of 201 neonates born to mothers with COVID-19: a systemic review. Eur Rev Med Pharmacol Sci. 2020;24(14):7804–15.
Shmakov RG, Prikhodko A, Polushkina E, Shmakova E, Pyregov A, Bychenko V, et al. Clinical course of novel COVID-19 infection in pregnant women. J Matern Fetal Neonatal Med. 2020;35:1–7.
Chi J, Gong W, Gao Q. Clinical characteristics and outcomes of pregnant women with COVID-19 and the risk of vertical transmission: a systemic review. Arch Gynecol Obstet. 2020;303:337–45.
Sulentic RO, Seferovic MD, Aagaard KM, Valentine GC. Perinatal COVID-19 outcomes: evaluating the strength of current evidence. J Matern Fetal Neonatal Med. 2020;35:1–7.
Collin J, Byström E, Carnahan A, Ahrne M. Public Health Agency of Sweden’s brief report: pregnant and postpartum women with SARS-CoV-2 infection in intensive care in Sweden. Acta Obstet Gynecol. 2020;99(7):819–22.
Ellington S, Strid P, Tong VT, Woodworth K, Galang RR, Zambrano LD, et al. Characteristics of women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status–United States, January 22–June 7, 2020. CDC Morb Mortal Wkly Rep. 2020;69(25):769–75.
Knight M, Bunch K, Vousden N, Morris E, Simpson N, Gale C, et al. UK obstetric surveillance system SARS-CoV-2 infection in pregnancy collaborative group. Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: national population based cohort study. BMJ. 2020;369:m2107.
Zambrano LD, Ellington S, Strid P, Galang RR, Oduyebo T, Tong VT, et al. Update: Characteristics of symptomatic women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status–United States, January 22–October 3, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(44):1641.
Allotey J, Stallings E, Bonet M, Yap M, Chatterjee S, Kew T, et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ. 2020;370: m3320.
Marquez MI, Campos-Zamora M, Lizaola-Diaz de Leon H, Farber MK. Maternal mortality from COVID-19 in Mexico. Int J Gynaecol Obstet. 2020;150(2):266–7.
Takemoto MLS, Menezes MO, Andreucci CB, Nakamura-Pereira M, Amorim MMR, Katz L, et al. The tragedy of COVID-19 in Brazil: 124 maternal deaths and counting. Int J Gynaecol Obstet. 2020;151(1):154–6.
Analysis of mortality caused by major diseases in the Republic of Kazakhstan, maternal and infant mortality. Critical issues and solutions. Nur-Sultan (Kazakhstan): Ministry of Healthcare of the Republic of Kazakhstan; 2021. http://www.rcrz.kz/files/nauka/MZ/%D0%93%D0%B8%D0%BD%D0%B8%D1%8F%D1%82%20%D0%90.pdf. Accessed 5 Apr 2021.
Giannis D, Ziogas IA, Gianni P. Coagulation disorders in coronavirus infected patients: COVID-19, SARS-CoV-1, MERS-CoV and lessons from the past. J Clin Virol. 2020;127: 104362.
Lodigiani C, Iapichino G, Carenzo L, Cecconi M, Ferrazzi P, Sebastian T, et al. Humanitas COVID-19 task force. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan. Italy Thromb Res. 2020;191:9–14.
Kripalani Y, Parulekar L. Pulmonary embolism in a COVID-19-positive primigravida after caesarean section despite prophylaxis. Eur J Case Rep Intern Med. 2021. https://doi.org/10.12890/2021_002684.
Leonard-Lorant I, Delabranche X, Severac F, Helms J, Pauzet C, Collange O, et al. Acute pulmonary embolism in patients with COVID-19 at CT angiography and relationship to d-Dimer levels. Radiology. 2020;296(3):E189–91.
Zhou F, Yu T, Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–62.
Cui S, Chen S, Li X, Liu S, Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost JTH. 2020;18(6):1421–4.
Gutiérrez García I, Pérez Cañadas P, Martínez Uriarte J, García Izquierdo O, Angeles Jódar Pérez M, García de Guadiana Romualdo L. D-dimer during pregnancy: establishing trimester-specific reference intervals. Scand J Clin Lab Invest. 2018;78(6):439–42.
Kadir RA, Kobayashi T, Iba T, Erez O, Thachil J, Kazi S, et al. COVID-19 coagulopathy in pregnancy: critical review, preliminary recommendations, and ISTH registry - Communication from the ISTH SSC for Women’s Health. J Thromb Haemost. 2020;18:3086–98.
RECOVERY Collaborative Group, Horby P, Lim WS, Emberson JR, Mafham M. Dexamethasone in hospitalized patients with COVID-19. N Engl J Med. 2021;384(8):693–704.
Toroghi N, Abbasian L, Nourian A, et al. Comparing efficacy and safety of different doses of dexamethasone in the treatment of COVID-19: a three-arm randomized clinical trial. Pharmacol Rep. 2022;74(1):229–40.
Stolz E, Klotzsch C, Schlachetzki F, Rahimi A. High-dose corticosteroid treatment is associated with an increased risk of developing cerebral venous thrombosis. Eur Neurol. 2003;49:247–8.
van Zaane B, Nur E, Squizzato A, Dekkers OM, Twickler MT, Fliers E, Gerdes VE, Buller HR, Brandjes DP. Hypercoagulable state in Cushing’s syndrome: a systematic review. J Clin Endocrinol Metab. 2009;94:2743–50.
Yale SH, Medlin SC, Liang H, Peters T, Glurich I, Mazza JJ. Risk assessment model for venothromboembolism in post-hospitalized patients. Int Angiol. 2005;24:250–4.
Acknowledgements
We thank Dr. Mel Underbakke for critical reading of the manuscript.
Funding
This work was funded by the Science Committee of the Ministry of Science and Higher Education of Kazakhstan [state grant #AP09259103 “Genomic and subgenomic characterization of SARS-CoV-2 strains, circulating in Kazakhstan, for the development of scientific approaches to COVID-19 diagnostics”].
Author information
Authors and Affiliations
Contributions
Conseptualization: Dmitrovskiy AM, Perfilyeva YV. Writing—original draft: Dmitrovskiy AM, Perfilyeva YV. Data collection: Smail EM, Maukaeva SB. Data analysis: Perfilyeva YV, Zhigailov AV. Writing—review & editing: Ostapchuk YO, Nizkorodova AS, Perfilyeva AV, Berdygulova ZA, Naizabayeva DA, Maltseva ER. Visualisation: Kamytbekova KZ. Funding acquisition: Zhigailov AV, Skiba YA.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was reviewed and approved by the Ethics Committee of the National Center for Biotechnology (approval #4 issued on September 8, 2020).
Consent for publication
Written informed consent was obtained from the parents of the deceased patient for publication of this case report and the accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal by request.
Competing interests
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Perfilyeva, Y.V., Maukayeva, S.B., Smail, Y.M. et al. Lethal pulmonary embolism in a pregnant woman with severe acute respiratory syndrome coronavirus-2 receiving prophylactic anticoagulation: a case report. J Med Case Reports 17, 455 (2023). https://doi.org/10.1186/s13256-023-04180-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-023-04180-w