Abstract
Background
Based on phenotypic similarities between age-related macular degeneration and the autosomal disorder Doyne honeycomb retinal dystrophy, we report on a single nanolaser treatment of a patient with genotype Doyne honeycomb retinal dystrophy confirmation and evidence of disease progression over 12 months. The case study is the first report of short-term results of subthreshold nanolaser treatment in a patient with Doyne honeycomb retinal dystrophy.
Case presentation
A 43-year-old Caucasian man with moderate loss of visual acuity in his left eye (20/40) and normal visual acuity in his right eye (20/20), with clinical Doyne honeycomb retinal dystrophy diagnosis and genetic confirmation of the common heterozygous mutation (EFEMP1) by genetic testing, underwent nanopulse subthreshold laser treatment in his left eye.
A safety examination, carried out 7 days after treatment, and clinical follow-up, conducted 60 days following laser treatment, showed improvement of visual acuity from baseline by two letters and a subjective improvement of blurring. While no apparent morphological changes were found on fundoscopy, increased autofluorescence in the treated eye was observed on imaging. In addition, 2 months after nanopulse subthreshold laser treatment, rod-mediated and cone-mediated full-field electroretinography b-wave amplitudes showed an increase from baseline in both the treated eye (300%) and untreated eye (50%). At 2 months after nanopulse subthreshold laser treatment, multifocal electroretinograms showed improvement. Acuity and full-field electroretinography improvement persisted at 6-month follow-up.
Conclusions
Sustained improvements in retinal function on electroretinography persisted in both eyes 6 months after treatment, suggesting an enhancement of phototransduction and retinoid recycling induced by nanopulse subthreshold laser treatment. The functional improvement observed in the untreated eye is hypothesized to arise from an increased expression and release of metalloproteinases that circulate systemically.
Similar content being viewed by others
Background
Doyne honeycomb retinal dystrophy (DHRD), also known as Malattia Leventinese, Online Mendelian Inheritance in Man (OMIM) 126600, is an autosomal dominant disorder caused by a single missense mutation, Arg345Trp (R345W), in the gene EGF containing fibulin-like extracellular matrix protein 1 (EFEMP1) [1,2,3,4].The disease is typically characterized by early-onset drusenoid deposits involving the posterior pole and the peripapillary area, often with a radial distribution. It has been suggested that mutant EFEMP1 may alter the extracellular matrix in Bruch’s membrane, leading to the accumulation of basal laminar deposits [1, 3]. Evidence for this lies in in vivo retinal microanatomy imaging by time-domain optical coherence tomography (OCT) showing diffuse alterations of the retinal pigment epithelium (RPE) and Bruch’s membrane, with preservation of the neurosensory layers [5,6,7]. In addition, mutations in the gene encoding tissue-inhibitor metalloproteinase-3 (TIMP3) are tightly linked to EFEMP1 and are associated with a severe form of DHRD [8,9,10]. Likewise, age-related macular degeneration (AMD) in its intermediate stage is characterized by drusen or drusenoid deposits, Bruch’s membrane thickening, and RPE atrophy (see review, Hulleman [11]). AMD and DHRD also share pathophysiologic similarities: two mouse models of DHRD showed complement activation and RPE atrophy, akin to the pathology observed in AMD [11, 12].
In 2013, Lenassi et al. showed that low-energy argon laser treatment performed just outside the drusen boundaries, but away from the fovea, induced drusen clearance and improved visual function in patients with DHRD with confirmed EFEMP1 mutation [13]. Recently, a low-energy, subthreshold nanosecond laser, the 2RT® (Ellex, Adelaide, Australia), has been utilized to induce targeted and controlled RPE injury without significant retinal neuronal damage or gliosis [14,15,16]. A clinical trial in intermediate AMD provided evidence of efficacy at 12-month follow-up, both in the treated and untreated eye, with improvement in flicker sensitivity on electroretinography (ERG) and reduction in the mean drusen area [17]. A similar effect was found in the APoE-null mouse model of AMD [18], with thinning of Bruch’s membrane and increased expression of matrix metalloproteinase-2 and matrix metalloproteinase-3 following nanolaser treatments.
Based on the phenotypic similarities between AMD and DHRD, a single application of nanopulse subthreshold laser treatment (NSLT) was attempted in a patient with Arg345Trp (R345W) genotype confirmation and clear evidence of disease progression over the previous 12 months. Treatment was delivered in one eye (the worse eye) with a modification to the standardized protocol according to Guymer et al. [17], applying 24 nanosecond laser spots. Retinal structure and function were assessed before and after the treatment. Results showed no appreciable changes in retinal morphology but an increase in autofluorescence on imaging in the treated eye. There was also a functional improvement in both the treated and untreated eye on ERG. This is the first report following NSLT of DHRD.
Case presentation
A 43-year-old Caucasian man presented with a moderate loss of visual acuity in his left eye (20/40) and normal right eye acuity (20/20). His medical, family, and psychosocial history was irrelevant. He did not have a history of medication use or previous diseases other than common childhood infectious diseases. For 12 months he complained of blurring, progressive alteration of night vision, and reduced contrast sensitivity in both eyes, with a much more pronounced effect in his left eye. Clinical diagnosis of DHRD was made after full ophthalmologic examination and detailed retinal imaging. Figure 1 shows OCT and fundus autofluorescence in both eyes. ERG, including mesopic and photopic full-field ERGs as well as multifocal ERGs (mfERG), were performed at baseline and 7 days after treatment. Genetic analysis confirmed the common heterozygous DHRD mutation in EFEMP1: (2p16.1) (p.R345W; c.1033C > T).
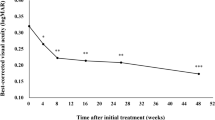
He was offered NSLT for his left eye. After written informed consent and full explanation of methods and procedure were completed, he underwent the treatment in his left eye, which applies ultra-low energy laser pulses in 24 spots around the macula of one eye (0.15–0.45 mJ), using 400 μm diameter laser spots, 3 nanosecond pulse length, 532 nm wavelength and energy titrated to the patient. Clinical follow-up was conducted at 60 and 180 days after treatment. Table 1 summarizes the clinical ophthalmological testing performed during follow-up. Visual acuity improved from baseline by two letters. There was a subjective improvement in blurring in his left eye. No morphological changes were apparent on fundoscopy, but increased autofluorescence in the treated eye was observed on imaging (Fig. 2). Rod-mediated and cone-mediated ERG b-wave amplitudes showed an increase from baseline in both the treated eye (300%) and fellow eye (50%) (Fig. 2). mfERG amplitudes did not change significantly from baseline, but the implicit time of the main positive component decreased by 8 milliseconds compared to baseline in the treated eye and by 5 milliseconds in the fellow eye (Fig. 3). Subjective and clinical improvements persisted unchanged at 6-month follow-up. The rod-mediated and cone-mediated ERG b-wave amplitude remained unchanged (300% increase) in the treated eye and returned to the pre-treatment value in the fellow eye.
a, b Mesopic and photopic electroretinography b-wave responses before 2RT® laser treatment. c, d Mesopic and photopic electroretinography b-wave responses 6 months after 2RT® laser treatment. Notice the large increase in the b-wave amplitude. e, f Optical coherence tomography imaging of the patient before and 1 month after 2RT®laser treatment, respectively. No significant changes in microanatomy were observed. g, h Autofluorescence imaging of the patient before and 1 month after 2RT®, respectively. A moderate increase in retinal autofluorescence was observed
a Multifocal electroretinography in the right eye (fellow-eye). On top: amplitude and implicit time before 2RT® laser treatment in the left eye (contralateral eye treated). Bottom: 2 months after treatment in the left eye (contralateral eye treated). b Multifocal electroretinography in left eye (treated eye). On top: amplitude and implicit time before 2RT® laser treatment in the left eye (treated eye). Bottom: 2 months after treatment in the left eye (treated eye). OD right eye, OS left eye
Discussion and conclusion
To the best of our knowledge, this is the first report describing the short-term results of NSLT in DHRD. The treatment was well tolerated and transpired without adverse events or complications up to the 6-month post-intervention time point, with sustained improvement in retinal function on ERG in both eyes. The improvement in ERG testing suggests enhanced phototransduction and retinoid recycling and aligns with the mechanism of action of this treatment, which in preclinical models was shown to reduce the thickness of Bruch’s membrane and increase the expression of metalloproteinases, thus resulting in improved retinoid recycling. The functional improvement observed in the untreated eye is consistent with other studies on this device and is hypothesized to arise from an increased expression and release of metalloproteinases that circulate systemically. The present results encourage further long-term studies with the subthreshold nanosecond laser as a potential treatment of retinal and RPE abnormalities associated with DHRD and similar conditions such as AMD.
References
Marmorstein LY, et al. Aberrant accumulation of EFEMP1 underlies drusen formation in Malattia Leventinese and age-related macular degeneration. Proc Natl Acad Sci. 2002;99:13067–72.
Narendran N, Guymer RH, Cain M, Baird PN. Analysis of the EFEMP1 gene in individuals and families with early onset drusen. Eye. 2005;19:11–5.
Stone EM, et al. A single EFEMP1 mutation associated with both Malattia Leventinese and Doyne honeycomb retinal dystrophy. Nat Genet. 1999;22:199–202.
Gregory CY, et al. The gene responsible for autosomal dominant Doyne’s honeycomb retinal dystrophy (DHRD) maps to chromosome 2p16. Hum Mol Genet. 1996;5:1055–9.
Souied EH, et al. Optical coherent tomography features of malattia leventinese. Am J Ophthalmol. 2006;141:404–7.
Gaillard MC, et al. Optical coherence tomography in Malattia Leventinese. Klin Monatsbl Augenheilkd. 2005;222:180–5.
Querques G, et al. Multimodal morphological and functional characterization of Malattia Leventinese. Graefes Arch Clin Exp Ophthalmol. 2013;251:705–14.
Klenotic PA, Munier FL, Marmorstein LY, Anand-Apte B. Tissue inhibitor of metalloproteinases-3 (TIMP-3) is a binding partner of epithelial growth factor-containing fibulin-like extracellular matrix protein 1 (EFEMP1): Implications for macular degenerations. J Biol Chem. 2004;279:30469–73.
Kobayashi N, et al. A comparative analysis of the fibulin protein family. Biochemical characterization, binding interactions, and tissue localization. J Biol Chem. 2007;282:11805–16.
Giltay R, Timpl R, Kostka G. Sequence, recombinant expression and tissue localization of two novel extracellular matrix proteins, fibulin-3 and fibulin-4. Matrix Biol. 1999;18:469–80.
Hulleman JD. Malattia Leventinese/Doyne Honeycomb Retinal Dystrophy: Similarities to Age-Related Macular Degeneration and Potential Therapies. Adv Exp Med Biol. 2016;854:153–8.
Sohn EH, et al. Comparison of drusen and modifying genes in autosomal dominant radial drusen and age-related macular degeneration. Retina. 2015;35:48–57.
Lenassi E, et al. Laser clearance of drusen deposit in patients with autosomal dominant drusen (p.Arg345Trp in EFEMP1). Am J Ophthalmol. 2013;155:190–8.
Wood JPM, Plunkett M, Previn V, Chidlow G, Casson RJ. Nanosecond pulse lasers for retinal applications. Lasers Surg Med. 2011;43:499–510.
Wood JPM, Shibeeb O, Plunkett M, Casson RJ, Chidlow G. Retinal damage profiles and neuronal effects of laser treatment: Comparison of a conventional photocoagulator and a novel 3-nanosecond pulse laser. Investig Ophthalmol Vis Sci. 2013;54:2305–18.
Chidlow G, Shibeeb O, Plunkett M, Casson RJ, Wood JPM. Glial cell and inflammatory responses to retinal laser treatment: Comparison of a conventional photocoagulator and a novel, 3-nanosecond pulse laser. Investig Ophthalmol Vis Sci. 2013;54:2319–32.
Guymer RH, et al. Nanosecond-laser application in intermediate AMD: 12-month results of fundus appearance and macular function. Clin Exp Ophthalmol. 2014;42:466–79.
Jobling AI, et al. Nanosecond laser therapy reverses pathologic and molecular changes in age-related macular degeneration without retinal damage. FASEB J. 2015;29:696–710.
Acknowledgements
Not applicable.
Funding
The authors report no funding.
Availability of data and materials
All data generated or analyzed during this study are available from the corresponding author on request.
Author information
Authors and Affiliations
Contributions
AC, BF, EG, and JM made substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data. AC and BF were involved in drafting the manuscript or revising it critically for important intellectual content. AC, BF, EG, JS, and JM gave final approval of the version to be published. Each author should have participated sufficiently in the work to take public responsibility for appropriate portions of the content. AC, BF, EG, and JM agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was not required. The patient gave written, informed consent. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Consent for publication
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
Prof. John Marshall is a consultant for Ellex. There are no other competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Cusumano, A., Falsini, B., Giardina, E. et al. Doyne honeycomb retinal dystrophy – functional improvement following subthreshold nanopulse laser treatment: a case report. J Med Case Reports 13, 5 (2019). https://doi.org/10.1186/s13256-018-1935-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-018-1935-1