Abstract
Background
To evaluate the implementation process of structured reporting (SR) in a tertiary care institution over a period of 7 years.
Methods
We analysed the content of our image database from January 2016 to December 2022 and compared the numbers of structured reports and free-text reports. For the ten most common SR templates, usage proportions were calculated on a quarterly basis. Annual modality-specific SR usage was calculated for ultrasound, CT, and MRI. During the implementation process, we surveyed radiologists and clinical referring physicians concerning their views on reporting in radiology.
Results
As of December 2022, our reporting platform contained more than 22,000 structured reports. Use of the ten most common SR templates increased markedly since their implementation, leading to a mean SR usage of 77% in Q4 2022. The highest percentages of SR usage were shown for trauma CT, focussed assessment with ultrasound for trauma (FAST), and prostate MRI: 97%, 95%, and 92%, respectively, in 2022. Overall modality-specific SR usage was 17% for ultrasound, 13% for CT, and 6% for MRI in 2022. Both radiologists and referring physicians were more satisfied with structured reports and rated SR better than free-text reporting (FTR) on various attributes.
Conclusions
The increasing SR usage during the period under review and the positive attitude towards SR among both radiologists and clinical referrers show that SR can be successfully implemented. We therefore encourage others to take this step in order to benefit from the advantages of SR.
Key points
-
1.
Structured reporting usage increased markedly since its implementation at our institution in 2016.
-
2.
Mean usage for the ten most popular structured reporting templates was 77% in 2022.
-
3.
Both radiologists and referring physicians preferred structured reports over free-text reports.
-
4.
Our data shows that structured reporting can be successfully implemented.
-
5.
We strongly encourage others to implement structured reporting at their institutions.
Similar content being viewed by others
Background
Structured reporting (SR) in radiology is often viewed as the favourable form of reporting and is highly recommended by the professional societies [1, 2]. There are numerous advantages of structured reports compared with conventional free-text reports, including better comparability, better readability, and more detailed content [3, 4]. These have been proven for the reporting of various examination types in different imaging modalities over the past years, including trauma CT, prostate MRI, and pulmonary embolism CT [3, 5, 6].
The term SR refers to an IT-based method of importing and arranging medical content in the radiological report and should not be confused with standardised reporting [7]. SR enables the automated acquisition of large quantities of structured data, which can be used for secondary use of data [8]. Secondary use of data can facilitate epidemiologic research and even enable the development of new disease-scoring systems [9]. Structured reports can be further augmented by interactive multimedia elements, such as graphical visual aids or hyperlinks from the text to referenced images [10].
Despite its potential, SR has not become the main form of radiology reporting. Most publications on SR start off with sentences like “Most radiology reports are written as free text and lack structure” or “Traditionally, reports are written as free text” [3, 11]. Nevertheless, actual use proportions of SR in clinical routine are unclear. Evidence for the implementation of SR is scarce [12].
This might be attributed to the drawbacks of SR: reporting complex cases can be time-consuming in template-based structured reports [13]. Incidental findings different from the suspected diagnosis do not fit well in SR templates. Additionally, most templates consist of checkboxes and drop-down menus. Filling in those templates by using a mouse and keyboard instead of speech recognition, which is commonly used for free-text reporting (FTR), carries the risk of distraction from the image study [14].
The clinical implementation of SR requires relevant changes to the individual radiologist’s workflow and requires great institutional effort [15]. Obstacles in the way of success are IT workflow barriers such as poor integration of SR templates into the radiology information system (RIS) or limited interoperability of healthcare IT systems, as well as personal aversion to SR among radiologists themselves [15, 16]. The Integrating the Healthcare Enterprise Management of Radiology Report Templates (IHE MRRT) profile provides a standardised description of a technical implementation and is freely available [17]. A detailed guide to the clinical implementation of SR, which addresses mainly technical and organisational aspects, is available [18].
In recent years, an extensive amount of research has been conducted in the field of SR. The focus has mostly been on model evaluations of its advantages over FTR and the potential benefits of the acquisition of large standardised datasets, while evidence of its acceptance in real clinical practice remains sparse [12, 19]. Thus, the purpose of this study was to gain more information on the actual status of SR usage in clinical routine. Therefore, we evaluated the implementation process at our institution over a 7-year period from its beginning in 2016. We measured changes in the proportions of structured reports and free-text reports for different examinations and imaging modalities. During the implementation process, a survey among radiologists and referring physicians was conducted to learn their opinions on the different forms of reporting.
Methods
At our institution, an IHE MRRT–compliant web-based platform for SR was first implemented in 2016 [20]. Since then, several SR templates for various examinations in different imaging modalities have been created and have been established in clinical routine. The content of our SR templates is oriented on the basis of proposals for SR by the German Society of Radiology (Deutsche Röntgengesellschaft) and the RSNA RadReport library, which are both freely available online [11, 21]. Being in html form, our reporting templates are easily adjustable. All reports are stored in a database, which makes versatile evaluations feasible. The reporting templates for cardiac CT, urolithiasis CT, CT-A of the lower extremities, and prostate MRI were enhanced with interactive multimedia reporting features. For example, our urolithiasis template offers a graphical representation of the urinary tract, in which radiologists can highlight renal and ureteral calculi in different colours and dimensions according to their density and size (Fig. 1). The figures are automatically sent to the picture archiving and communication system (PACS) as a digital imaging and communications in medicine (DICOM) secondary capture along with the final report. The template development is an iterative process which also involves clinical referrers in order to tailor templates to their needs. Meetings of an expert group for SR consisting of consultants, residents, and IT specialists are held weekly. Their goal is the maintenance and adaptation of existing SR templates as well as the development of new ones. SR usage is encouraged and recommended at our institution, but not mandatory.
Evaluation of the SR database
We queried the SR platform for all frequently used SR templates. For the ten most frequently used templates, the number of reports stored in our reporting platform was calculated on a quarterly basis. Between January 2016 and December 2022, the total number of reports for these examinations (the sum of structured reports and free-text reports) was queried from the RIS (Mesalvo RadCentre, Mannheim, Germany). We analysed the proportions of free-text reports and structured reports on a quarterly basis. The number of free-text reports was calculated by subtracting the number of structured reports from the total number of radiological reports. We also calculated annual proportion of SR for the following examinations: trauma CT, pulmonary embolism CT, focussed assessment with ultrasound in trauma (FAST), PET/CT, carotid ultrasound, and prostate MRI from 2016 to 2022. The proportion of reports using SR was also calculated for the imaging modalities CT, MRI, and ultrasound.
Survey
An online survey (www.soscisurvey.de) was conducted to ask radiologists and referring physicians (urologists, trauma surgeons, orthopaedic surgeons, and doctors from internal medicine) for their opinions on forms of radiology reports.
A cognitive pre-test was performed with three final-year medical students and a board-certified radiologist to ensure the comprehensibility of the questionnaire. After minor reformulations, a standard pre-test was performed. Standard pre-testing led to technical modifications to ensure optimal visualisation on mobile phones.
The link to the finalised survey was e-mailed to the consultants of the above-mentioned departments with the request to forward it to all doctors in their departments and to all doctors in the radiology department.
The survey took place from August to September 2021 and was conducted in the German language.
First, the participants were surveyed regarding their gender, age, professional experience, specialisation, and board certification.
Second, they were asked about the characteristics of free-text reports and structured reports (“…are complete”; “…are clear”; “…enable fast extraction of relevant information”; “…facilitate decision-making”; “…enable research”) and to evaluate statements concerning reporting (“findings sections should be structured”; “impression sections should be structured”; “graphics and/or images embedded in structured reports would help to visualise findings/results”; “besides structured content, content in unstructured form will always be necessary”; “it is not possible to use SR for each examination”). Participants rated their agreement with these statements, using a 7-point scale (“do not agree at all”; “disagree”; “rather disagree”; “neutral”; “rather agree”; “agree”; “totally agree”). A 7-point scale leads to high variance among answers and thus to higher reliability and more nuanced trend analysis [22].
Lastly, the participants were queried about the optimal proportional use of structured reports and free-text reports with a slider indicating percentages.
Statistical analysis
For statistical analysis, database entries were extracted as a CSV file and subsequently analysed using Excel 2016 (Microsoft, Redmond, USA). Results are reported in absolute numbers and as percentages as mentioned above.
Final survey results were extracted as a CSV file and subsequently analysed using R 4.0.3 (R Foundation for Statistical Computing, Vienna, Austria). Mean values and standard deviation values were calculated to analyse the survey results. Data distribution was tested using the Shapiro–Wilk test. As the variables were not normally distributed, the non-parametric Mann–Whitney U test was used to identify differences. A p value < 0.05 was considered statistically significant.
Results
Evaluation of the SR database
As of December 2022, our reporting platform contained 22,902 structured reports. The ten most frequently used templates accounted for 20,932 (91% of all) reports. Table 1 lists these ten templates with the total number of reports and the dates of implementation into the clinical workflow. The liver transplant evaluation template was the first to be established, in Q2 2016. For this template, we successfully implemented electronic report sheets that are required by German law for organ transplantation in clinical routine [23].
The most frequently used SR template at our institution is for PET-CT, followed by those for urolithiasis CT and focussed assessment with sonography in trauma (FAST). The latest SR templates to be implemented are for CT-angiography of the lower extremities, in Q2 2022, and for pre-procedural CT for transcatheter aortic valve replacement, in Q3 2022.
Quarterly analysis of the proportions of structured reports and free-text reports for these ten examination types for which SR is most used showed a steady increase of SR usage up to 77% in Q4 2022, while the total numbers for these examination types showed an increase of 49%, from 1248 in Q2 2016 to 1862 in Q4 2022 (Fig. 2).
Further analysis of single examinations showed that in trauma CT, FAST, and prostate MRI, SR usage was the highest (97%, 95%, and 92%, respectively, in 2022), followed by urolithiasis CT and carotid ultrasound with SR use at 91% and 84%, respectively (Fig. 3). In pulmonary embolism CTs, some radiologists still tend to report in a free-text form (SR usage 58% in 2022). For all examinations, an increase in the use of structured reports since their implementation was shown. Liver transplant evaluation was excluded from the analysis, since it is required to be in a structured form by German law (SR usage 100%).
Absolute numbers of all radiological reports (grey) and structured reports (blue) as well as the proportion of structured reports (red) over a 7-year period, shown for (a) trauma CT, (b) focussed assessment with ultrasound in trauma (FAST), (c) prostate MRI, (d) urolithiasis CT, (e) carotid ultrasound, and (f) pulmonary embolism CT
Analysis of annual modality-specific use of SR showed increasing values for CT, MRI, and ultrasound. Figure 4 shows the modality-specific use of SR at the end of the period under review (2022), on the one hand for all examinations carried out in each modality (A) and on the other hand for all examinations for which SR was available (B). Overall, SR was used in reporting ultrasound, CT, and MRI in 17%, 13%, and 6% of reports, respectively. Regarding only examination types for which SR was available, modality-specific SR use was much higher, at 92%, 69%, and 92% for ultrasound, CT, and MRI, respectively. No use proportions for x-ray examinations, mammographies, and angiographic procedures were calculated since, as yet, no SR templates have been developed for any examinations in these modalities at our institution.
Survey results
A total of 51 physicians (15 radiologists and 36 referring physicians) from our institution took part in the survey. The study participants’ demographic information is shown in Table 2. The mean professional experience of the participants was 9 years in both groups. The mean age of radiologists was 36 years and mean age of referring physicians was 37 years. In both groups, residents and board-certified physicians took part in the survey.
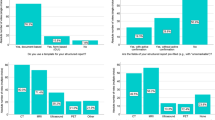
Radiologists and referring physicians both rated structured reports as significantly better than free-text reports for the following attributes: completeness, clarity, enabling fast extraction of relevant information, facilitating decision-making, and enabling research (Fig. 5).
Radiologists and referring physicians agreed that the findings section of reports, especially, should be structured. Nevertheless, they stated that unstructured content will always be necessary in radiological reports and that structured reporting will not be possible for every indication. Radiologists agreed more with the statement that graphics and/or images embedded in a structured report help to visualise the imaging results (p = 0.003). Table 3 shows the ratings of all statements by radiologists and referring physicians.
Radiologists predicted that SR leads to a significantly higher referring-physician satisfaction compared with FTR. Referring physicians reported themselves to be more satisfied with SR than with FTR (Fig. 6).
We did not find a significant difference between radiologists’ and referring physicians’ views regarding the optimal proportions of free-text and structured reports (p = 0.64). Radiologists estimated the respective optimums as 32% and 68%, and referring physicians as 36% and 64%.
Discussion
In this study, we evaluated the clinical implementation of SR at our institution over the last 7 years. A steadily increasing total number of structured reports as well as an increasing percentage of SR in radiology reports could be observed. In the survey, radiologists and referring physicians both agreed on many advantages of SR over free-text reporting. The data show that SR implementation is a long-term process requiring great effort but that it is ultimately successful in terms of SR usage in clinical routine.
Explicit data on actual rates of SR usage in clinical routine are very limited. Published surveys on SR usage deal mostly with the question of how many institutions are or are not using SR in clinical routine, but do not reveal specific use ratios [19, 24]. A few older publications on successful implementations at U.S. institutions do describe high SR usage and compliance among radiologists [18, 25, 26]. Nevertheless, their definition of SR would be classified as standardised reporting according to the current state of knowledge and does not refer to an IT-based method [7].
For those examinations for which SR templates are available, we demonstrated high proportions of SR use of up to 97% (trauma CT template in 2022), even though SR use is not mandatory at our institution. This confirms the growing acceptance of SR among radiologists, which is further underlined by the positive attitude towards SR revealed in the survey part of this study. The positive results of our survey highlight the success of the implementation process and coincide with other surveys that have evaluated SR for examinations including pulmonary embolism CT, trauma CT, and many others [3, 5, 6]. Nevertheless, these previous surveys dealt with out-of-hospital evaluations to determine the value of SR for particular examinations and had mostly small numbers of participants. Our survey, on the other hand, was conducted during an actual clinical implementation of SR for many examinations and had a larger participant count (51) than the prior ones.
Differences in the use of SR between single examination types, such as the high rate seen in prostate MRI compared with the relatively lower rate in pulmonary embolism CT (92% vs. 58% in 2022) may be due to the nature of the examinations. After all, the implementation of SR is highly case specific [12]. Our prostate MRI template offers decision support on how to classify lesions according to PI-RADS and contains a map of the prostate sectors as an interactive multimedia reporting feature. Users are guided through the report, which makes SR the favoured form of reporting for most of them. In pulmonary embolism CT, findings that point toward an alternative diagnosis are found in up to 33% of the examinations [27]. Radiologists might find the template unsuitable for properly describing alternative diagnoses.
The need for interactive multimedia reporting features like graphical visual aids is addressed by various publications [10, 28]. Some of our templates are supported by those features, and commercial vendors have already started integrating them into their SR solutions. To date, no investigations have objectively assessed their benefits. In our survey, radiologists and referrers agreed that they are helpful. Especially in interdisciplinary meetings, graphic visual aids have the potential to accelerate and facilitate workflow and communication [29].
Obstacles in the way of successfully implementing SR in clinical routine have been discussed in the literature and are mostly of an organisational, technical, or personal nature [15, 16, 18]. Organisational difficulties could be mitigated by weekly expert meetings and the iterative form of template development.
A major technical obstacle is the limited integration of SR into the RIS. Our SR platform successfully communicates with the RIS via an HTTP and XML interface [20]. Since its implementation, various customisations of the RIS have been made in collaboration with the vendor, and these have further improved the integration of the reporting platform. For example, changes to the RIS user interface that facilitated access to the reporting templates were made, and loading times for templates could be reduced.
The data on high SR usage and the positive attitude towards SR indicate that personal aversions to SR among radiologists are low at our institution. On the contrary, radiologists desire more SR, and currently the limiting factor is the availability of templates. Over a 7-year process, radiologists have become accustomed to SR. Aversions from the early days might have faded and are addressed by subsequent teaching on how to use SR.
In order to reach higher overall SR use, the directed development of more templates is inevitable. Nevertheless, SR will probably not be applicable to all kinds of examinations. Radiologists and referring physicians agreed on this statement in the study survey and stated that the ratio between structured and free-text reports should be approximately 2:1.
SR is not equally suitable for all examinations, and a practical application to every examination might not be possible at all. Nevertheless, the estimated equilibrium should be reachable in the near future. Therefore, the few remaining disadvantages of SR have to be resolved. For example, natural language processing has the potential to integrate speech recognition into SR and thus could further boost SR usage.
Our study has several limitations. It was conducted as a single-centre study and therefore carries associated risks, such as potentially limited external validity [30]. Most other institutions that work with an IHE MRRT-compliant reporting platform do not have a comparably large number of structured reports in their databases, which makes detailed validation difficult. Moreover, we ourselves chose the examinations for which we would develop SR templates. This might carry a slight selection bias, since SR usage might be more feasible for the chosen examinations than for others.
Conclusion
The data on high SR usage along with the positive attitudes of both radiologists and clinical referrers towards SR shows that the clinical implementation of SR can be successful. We therefore strongly encourage others to take this step. Ultimately, the added value that SR provides is definitely worth the effort.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CT:
-
Computed tomography
- DICOM:
-
Digital imaging and communications in medicine
- FAST:
-
Focussed assessment with ultrasound in trauma
- FTR:
-
Free-text reporting
- IHE MRRT:
-
Integrating the Healthcare Enterprise Management of Radiology Report Templates
- IT:
-
Information technology
- MRI:
-
Magnetic resonance imaging
- PACS:
-
Picture archiving and communication system
- PET:
-
Positron emission tomography
- PI-RADS:
-
Prostate imaging reporting and data system
- RIS:
-
Radiology information system
- SR:
-
Structured reporting
References
European Society of Radiology (ESR) (2021) paper on structured reporting in radiology European Society of Radiology (ESR). Insights Imaging 9:1–7. https://doi.org/10.1007/s13244-017-0588-8
Dunnick NR, Langlotz CP (2008) The radiology report of the future: a summary of the 2007 intersociety conference. J Am Coll Radiol 5:626–629. https://doi.org/10.1016/j.jacr.2007.12.015
Jorg T, Heckmann JC, Mildenberger P et al (2021) Structured reporting of CT scans of patients with trauma leads to faster, more detailed diagnoses: an experimental study. Eur J Radiol 144:109954. https://doi.org/10.1016/j.ejrad.2021.109954
Brook OR, Brook A, Vollmer CM et al (2015) Health policy and practice: structured reporting of multiphasic CT for pancreatic cancer. Radiology 274:464–472. https://doi.org/10.1148/radiol.14140206
Sabel BO, Plum JL, Kneidinger N et al (2017) Structured reporting of CT examinations in acute pulmonary embolism. J Cardiovasc Comput Tomogr 11:188–195. https://doi.org/10.1016/j.jcct.2017.02.008
Wetterauer C, Winkel DJ, Federer-Gsponer JR et al (2018) Structured reporting of prostate magnetic resonance imaging improves interdisciplinary communication. Eur Urol Suppl 17:e2562. https://doi.org/10.1016/s1569-9056(18)33039-2
Nobel JM, Kok EM, Robben SGF (2020) Redefining the structure of structured reporting in radiology. Insights Imaging 11:10. https://doi.org/10.1186/s13244-019-0831-6
Pinto Dos Santos D, Scheibl S, Arnhold G et al (2018) A proof of concept for epidemiological research using structured reporting with pulmonary embolism as a use case. Br J Radiol 91:1088. https://doi.org/10.1259/bjr.20170564
Fink MA, Mayer VL, Schneider T et al (2022) CT angiography clot burden score from data mining of structured reports for pulmonary embolism. Radiology 302:175–184. https://doi.org/10.1148/radiol.2021211013
Roth CJ, Clunie DA, Vining DJ et al (2021) Multispecialty enterprise imaging workgroup consensus on interactive multimedia reporting current state and road to the future: HIMSS-SIIM collaborative white paper. J Digit Imaging 34:495–522. https://doi.org/10.1007/s10278-021-00450-5
Pinto Dos Santos D, Hempel JM, Mildenberger P et al (2019) Structured reporting in clinical routine. Rofo 191:33–39. https://doi.org/10.1055/a-0636-3851
Nobel JM, van Geel K, Robben SGF (2022) Structured reporting in radiology: a systematic review to explore its potential. Eur Radiol 32:2837–2854. https://doi.org/10.1007/s00330-021-08327-5
Haroun RR, Al-Hihi MM, Abujudeh HH (2019) The pros and cons of structured reports. Curr Radiol Rep 7:1–4. https://doi.org/10.1007/s40134-019-0342-8
Sistrom CL (2005) Conceptual approach for the design of radiology reporting interfaces: the talking template. J Digit Imaging 18:176–187. https://doi.org/10.1007/s10278-005-5167-8
Pinto dos Santos D, Kotter E (2018) Structured radiology reporting on an institutional level—benefit or new administrative burden? Ann N Y Acad Sci 1434:274–281. https://doi.org/10.1111/nyas.13741
Tran L, Wadhwa A, Mann E (2016) Implementation of structured radiology reports. J Am Coll Radiol 13:296–299. https://doi.org/10.1016/j.jacr.2015.06.040
Langlotz C (2013) IHE radiology technical framework supplement management of radiology report templates (MRRT) draft for public comment
Larson DB (2018) Strategies for implementing a standardized structured radiology reporting program. Radiographics 38:1705–1716. https://doi.org/10.1148/rg.2018180040
Powell DK, Silberzweig JE (2015) State of structured reporting in radiology, a survey. Acad Radiol 22:226–233. https://doi.org/10.1016/j.acra.2014.08.014
Pinto dos Santos D, Klos G, Kloeckner R et al (2017) Development of an IHE MRRT-compliant open-source web-based reporting platform. Eur Radiol 27:424–430. https://doi.org/10.1007/s00330-016-4344-0
Radiological Society of North America (2020) RadReport Template Library. https://www.radreport.org/. Accessed 19 Dec 2022.
Saris WE, Gallhofer IN (2007) Design, Evaluation, and Analysis of Questionnaires for Survey. Research Wiley Series in Survey Methodology. Wiley, Hoboken, New Jersey.
Pinto Dos Santos D, Arnhold G, Mildenberger P et al (2017) Guidelines regarding §16 of the German transplantation act—initial experiences with structured reporting, RoFo fortschritte auf dem gebiet der rontgenstrahlen und der Bildgeb. Verfahren. https://doi.org/10.1055/s-0043-118129.
Faggioni L, Coppola F, Ferrari R et al (2017) Usage of structured reporting in radiological practice: results from an Italian online survey. Eur Radiol 27:1934–1943. https://doi.org/10.1007/s00330-016-4553-6
Larson DB, Towbin AJ, Pryor RM et al (2013) Improving consistency in radiology reporting through the use of department-wide standardized structured reporting. Radiology 267:240–250. https://doi.org/10.1148/radiol.12121502
Goldberg-Stein S, Walter WR, Amis ES et al (2017) Implementing a structured reporting initiative using a collaborative multistep approach. Curr Probl Diagn Radiol 46:295–299. https://doi.org/10.1067/j.cpradiol.2016.12.004
Hall WB, Truitt SG, Scheunemann LP et al (2009) The prevalence of clinically relevant incidental findings on chest computed tomographic angiograms ordered to diagnose pulmonary embolism. Arch Intern Med 169:1961–1965. https://doi.org/10.1001/archinternmed.2009.360
Machado LB, Dwyer AJ (2018) Multimedia-enhanced radiology reports: concept, components, and challenges. Radiographics 38:462–482
Jorg T, Mildenberger P, Stöhr F (2023) Interdisziplinäre Besprechungen. Die Radiol. https://doi.org/10.1007/s00117-023-01114-x
Bellomo R, Warrillow SJ, Reade MC (2009) Why we should be wary of single-center trials. Crit Care Med 37:3114–3119. https://doi.org/10.1097/CCM.0b013e3181bc7bd5
Funding
Open Access funding enabled and organised by Projekt DEAL. This study received no outside funding.
Author information
Authors and Affiliations
Contributions
Conceptualisation and data collection were performed by TJ, LM, GA, and FJ. Statistical analysis was performed by LM. The first draft of the manuscript was written by TJ. Writing and editing were performed by DPS, MH, LM, FJ, RK, and PM. Project administration was done by PM and CD. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional review board approval was waived by the Ethics Committee of the Medical Association of Rhineland-Palatinate. Written informed consent was not necessary/applicable. The survey participants were informed that participation was voluntary, that the survey results would be anonymous, and that they were collected for research purposes only. All analysed patient data were fully de-identified.
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no competing interests regarding this study. DPS is a member of the Insights into Imaging Editorial Board. He has not taken part in the review or selection process of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jorg, T., Halfmann, M.C., Arnhold, G. et al. Implementation of structured reporting in clinical routine: a review of 7 years of institutional experience. Insights Imaging 14, 61 (2023). https://doi.org/10.1186/s13244-023-01408-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13244-023-01408-7