Abstract
Objective
To investigate the relationship between the elasticity of the carotid artery and the LV (left ventricle) systolic function in patients with diabetic nephropathy (DN) by using two-dimensional speckle-tracking strain echocardiography (2D-STE).
Methods
DN patients (n = 108) and control subjects (n = 112), all of whom underwent echocardiography and carotid ultrasound. Analysis of LV GLS (global longitudinal strain) from the apical two-chamber (2C), three-chamber (3C), and four-chamber (4C) views. Meanwhile, the circumferential strain (CS) of the carotid artery was obtained from the view of the short-axis right common carotid artery. The differences between the two groups were compared, and a correlation analysis between CS and GLS was performed.
Results
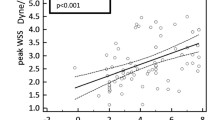
The 4CGLS, 2CGLS, 3CGLS, and CS of the DN group were significantly lower at significant levels in contrast to the control group (p < 0.05). There was a significantly positive correlation of CS with 4CGLS, 2CGLS, and 3CGLS in all subjects (r = 0.809, p = 0.000; r = 0.830, p = 0.000; r = 0.830, p = 0.000, respectively).
Conclusion
2D-STE is a relatively new technique for assessing the mechanical characteristics of the carotid artery in patients with DN. Reduced values of CS correlate with reduced LV systolic function as evaluated by strain measurements, which can predict the risk of systolic dysfunction of LV.
Similar content being viewed by others
Key points
• Increased arterial stiffness measured by 2D-STE is indicative of a potential link between vascular changes and LV systolic function.
• Reduced CS values correlate with reduced LV systolic function evaluated by strain measurements.
• 2D-STE can detect the relationship between CS and GLS in the early stage.
Introduction
Diabetes mellitus (DM) is a serious threat to human health and life. It can lead to a variety of complications [1,2,3]. Among all the complications of DM, cardiovascular complications are important causes of disability and death [4], and diabetic nephropathy (DN) is the major cause of end-stage renal failure. Renal disease is also an important cause of cardiovascular disease (CVD), including sudden cardiac death and stroke [5, 6]. Thus, DN patients have a high risk of CVD, which is identified as the leading reason of death in these patients.
It was reported that stiffness in arteries was a major and robust independent predictor of CVD [7, 8]. Arterial stiffness was recommended as a proof of damage to the target organs in the European guidelines for the hypertension diagnosis and treatment [9]. There are several methods of evaluating arterial stiffness, such as vascular catheterization, ultrasound, magnetic resonance imaging [10], and arterial tonometry [11]. 2D-STE (two-dimensional speckle-tracking strain echocardiography) is a useful technology that has been developed in recent years [12, 13]. It is an accurate, angle-independent, and noninvasive method for evaluating cardiac function [14]. It can be used to obtain myocardial deformation by tracking intramyocardial speckles, accordingly calculating the strain (S) and strain rate (Sr) of the myocardium [15]. This strain-based imaging technique has been shown to have clinical utility in a variety of settings [16]. It can predict severe coronary artery disease (CAD) in women with normal LV function [17]. It can be used to identify the ischemic etiology of LV systolic dysfunction [18]. The study by Atici et al. showed that GLS (global longitudinal strain) evaluated through 2D-STE is a potential method for predicting CAD in patients with non-ST-segment elevation myocardial infarction [19]. 2D-STE can assess the impairment of left atrial phasic function in patients with heart failure with mid-range ejection fraction (EF) [20]. At present, this technique is also used to evaluate the elasticity of the carotid artery, and the obtained strain has a good correlation with carotid elasticity [21]. The aortic circumferential strain and the rate of strain estimated by 2D strain imaging enable accurate and simple evaluation of the stiffness of the aorta [22]. However, the relationship between the elasticity of the carotid artery and the systolic function of the LV remains unclear. The study aimed to examine the association between carotid elasticity and LV systolic function in DN patients using 2D-STE.
Materials and methods
Patients
Between May 2017 and November 2019, 139 patients newly diagnosed with DN participated in this study. DN was diagnosed according to the Tervaert criteria [23]. The exclusion criteria were as follows: ①patients with congenital vascular disease and ② patients with vascular diseases secondary to hypertension, hyperlipidemia, cardiac dysfunction, or endocrine diseases. The final study consisted of 108 patients (62 women, 46 men, mean age 50.16 ± 12.30 years). Meanwhile, 112 healthy individuals served as a control group (67 women, 45 men, mean age 47.41 ± 9.72 years). All subjects did not suffer from any CVD or associated risk factors that were known. Coffee and alcohol were not administered within 24 h before examination.
All of the above candidates received detailed clinical evaluation and biochemical tests. Detailed clinical evaluation items included medical history, height, weight, BMI (body mass index), blood pressure, and cardiovascular examination. Biochemical test items included FBG (fasting blood glucose), HbA1c (hemoglobin A1c), TG (triglycerides), TC (total cholesterol), HDL-C (high-density lipoprotein cholesterol), and LDL-C (low-density lipoprotein cholesterol).
Carotid ultrasound
Carotid ultrasound was performed with a GE Vivid E9 (GE Healthcare) ultrasound system, equipped with a 10-L probe (frequency ranged 7.5~10 MHz) and M4S probe (frequency ranged 1.5~5.0 MHz). Digitized images of the right common carotid artery (CCA) were obtained by 10 L probe. Carotid IMT (intima-media thickness) was measured in right CCA at end diastole, 1.0 cm proximal to the carotid bulb [24, 25]. Plaque formation was defined as IMT ≥ 1.2 mm [26]. Patients with presented plaque were excluded from this study. Color Doppler ultrasonography was used to detect PSV (peak flow velocity), EDV (end-diastolic flow velocity), PI (pulsatility index), and RI (resistance index) of the carotid artery. Then, an inflatable balloon containing 100 ml saline was used to increase the surface contact and improve the acoustic window, and the equipment was switched to the M4S probe. Dynamic images of the short axis of the carotid artery were obtained and stored for up to three consecutive cardiac cycles.
Echocardiography
Echocardiography was also performed with the GE Vivid E9 equipped with an M4S probe. Conventional 2-D and Doppler echocardiography were carried out to exclude any unconfirmed structural disease of the heart including LV hypertrophy, valvular disease, pericardial disease, or cardiomyopathy. EF was obtained by biplane Simpson method [27]. Cine-loop clips of three consecutive cardiac cycles were obtained from the apical 4C, 2C, and 3C view.
STE imaging analysis
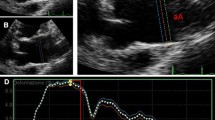
All clips were acquired at 50–70 frames/s. These images were exported from the ultrasound equipment and then analyzed offline with the EchoPAC software (GE Healthcare, IL, USA). The procedure began with manually distinguishing the endocardial at a single frame at end systole, with a region of interest that covers of the myocardial wall thickness (Figs. 1 and 2). The EchoPAC software was used to automatically calculate the strain, including 4CGLS, 2CGLS, and 3CGLS. The circumferential strain (CS) of CCA was also obtained (Figs. 3 and 4).
Statistical evaluation
Statistical evaluations were carried out using SPSS V 17.0 (SPSS Inc., Chicago, USA). Mean ± SD was used to express quantitative data. Comparisons among the two groups were accomplished with the t test of the independent samples. The relationship between CS of the CCA and 4CGLS, 2CGLS, and 3CGLS of the LV was assessed by Pearson’s correlation analysis. P < 0.05 was deemed a statistically significant difference.
Results
Detailed clinical evaluation versus biochemical test
In the DN group, FBG and glycated HbA1c in the DN group were much higher in contrast to the control group (p = 0.000). No significant variation was observed in terms of age, BMI, SBP (systolic blood pressure), DBP (diastolic blood pressure), HR (heart rate), TG, TC, HDL-C, and LDL-C among the two groups (p > 0.05) (Table 1).
The carotid ultrasound
There was no significant difference in IMT, PSV, EDV, PI, and RI between the two groups (p > 0.05) (Table 2).
STE imaging analysis
The CS in the DN group was lower at the significant levels in contrast to the control group (p = 0.000). The 4C GLS, 2C GLS, and 3C GLS in the DN group were lower at significant levels in contrast to the control group (p = 0.000, p = 0.000, p = 0.000) (Table 3).
The correlation coefficient among CS and 4CGLS was 0.809 (p = 0.000). The correlation coefficient among CS and 2CGLS was 0.830 (p = 0.000). The correlation coefficient among CS and 3CGLS was 0.830 (p = 0.000) (Fig. 5).
Discussion
Atherosclerosis includes structural and functional abnormalities. Carotid IMT has long been regarded as a good indicator of structural abnormalities and can be used to evaluate atherosclerosis [24,25,26]. Functional abnormalities include a reduction in the distensibility coefficient, an increase in stiffness index, and an incremental increase in elastic modulus [28]. Functional abnormalities occur earlier than structural changes do [28]. 2D-STE has been used to evaluate aortic stiffness [22]. The strain and strain rate obtained from 2D-STE are widely used in the evaluation of myocardial and vascular wall deformation [15, 21, 22]. In this study, the carotid CS in the DN group were lower at significant levels in contrast to the control group, but the difference in IMT among the two groups was not significant. This indicated that the carotid artery stiffness increased in patients with DN, and the functional changes occurred earlier than structural changes, which was consistent with previous studies [28].
The myocardium is divided into three layers: shallow, middle, and deep. The shallow layer is left-handed spiral, the middle layer is circular, and the deep layer is right-handed spiral. The special structure of the myocardial fiber determines that the myocardium has radial contraction, longitudinal contraction, circumferential movement, and rotational movement [29]. Longitudinal contraction of myocardial fibers plays an important role in cardiac movement and has important clinical significance [30]. It was reported that the GLS of the myocardium can be used to evaluate the early systolic function of the heart [30,31,32]. Radwan and Hussein found a positive correlation at significant levels between GLS and EF, and measurement of GLS using 2D-STE to be accurate and sensitive tool in severe CAD prediction [33]. The study by Shiino et al. showed that GLS is more sensitive than conventional LV EF to detect early improvement in systolic function of the LV after severe aortic valve stenosis patients underwent transcatheter aortic valve implantation and preserved LV systolic function [34]. In our study, the GLS in the DN group were lower at significant levels in contrast to the control group, which indicated that the systolic function of LV was impaired in patients with DN.
Some studies have shown a close relation between arterial stiffness to left ventricular diastolic function [8, 35]. However, there are only few reports on the association between left ventricular systolic function and arterial stiffness. In this study, the outcomes revealed that there was a positive correlation at significant levels between the CS of the carotid artery and the GLS of LV, which indicated that the greater the stiffness of the carotid artery, the greater the impairment of cardiac systolic function. This reason may be that the carotid artery belongs to the elastic artery and is rich in elastic fibers. When LV ejection occurs, the intra-arterial pressure increases, the large artery dilates passively, and the volume increases, so the deformation in the circumferential direction is increased. When arterial stiffness increases, the mean elasticity decreases, the burden of the LV contraction is increased, and the systolic function is impaired.
In conclusion, increased arterial stiffness measured by 2D-STE is indicative of a potential link between vascular changes and LV systolic function. When the CS decreases, the GLS is impaired. The CS has a certain predictive effect on the early reduction of LV systolic function. 2D-STE can detect the relationship between CS and GLS in the early stage.
Availability of data and materials
The analyzed and/or used datasets in this study can be obtained on reasonable request to the corresponding author.
Abbreviations
- 2C:
-
Two-chamber
- 2D-STE:
-
Two-dimensional speckle-tracking strain echocardiography
- 3C:
-
Three-chamber
- 4C:
-
Four-chamber
- BMI:
-
Body mass index
- CAD:
-
Coronary artery disease
- CCA:
-
Common carotid artery
- CS:
-
Circumferential strain
- CVD:
-
Cardiovascular disease
- DBP:
-
Diastolic blood pressure
- DM:
-
Diabetes mellitus
- DN:
-
Diabetic nephropathy
- EDV:
-
End-diastolic flow velocity
- FBG:
-
Fasting blood glucose
- GLS:
-
Global longitudinal strain
- HbA1c:
-
Glycated hemoglobin A1c
- HDL-C:
-
High-density lipoprotein cholesterol
- HR:
-
Heart rate
- IMT:
-
Intima-media thickness
- LDL-C:
-
Low-density lipoprotein cholesterol
- LV:
-
Left ventricle
- PI:
-
Pulsatility index
- PSV:
-
Peak flow velocity
- RI:
-
Resistance index
- SBP:
-
Systolic blood pressure
- TC:
-
Total cholesterol
- TG:
-
Triglycerides
References
Chen R, Ovbiagele B, Feng W (2016) Diabetes and stroke: epidemiology, pathophysiology, pharmaceuticals and outcomes. Am J Med Sci 351:380–386
Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE (2014) Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract 103:137–149
Kharroubi AT, Darwish HM (2015) Diabetes mellitus: the epidemic of the century. World J Diabetes 6:850–867
Wang J, Wang F, Liu S, Zhou M, Zhang L, Zhao M (2017) Reduced kidney function, albuminuria, and risks for all-cause and cardiovascular mortality in China: a population-based cohort study. BMC Nephrol 18:188
Chronic Kidney Disease Prognosis Consortium, Matsushita K, van der Velde M et al (2010) Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet 375:2073–2081
Sasso FC, Chiodini P, Carbonara O et al (2012) High cardiovascular risk in patients with type 2 diabetic nephropathy: the predictive role of albuminuria and glomerular filtration rate. The NID-2 Prospective Cohort Study. Nephrol Dial Transplant 27:2269–2274
Laurent S, Katsahian S, Fassot C et al (2003) Aortic stiffness is an independent predictor of fatal stroke in essential hypertension. Stroke 34:1203–1206
Chow B, Rabkin SW (2015) The relationship between arterial stiffness and heart failure with preserved ejection fraction: a systemic meta-analysis. Heart Fail Rev 20:291–303
Mancia G, De Backer G, Dominiczak A et al (2007) 2007 Guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 28:1462–1536
Groenink M, de Roos A, Mulder BJ, Spaan JA, van der Wall EE (1998) Changes in aortic distensibility and pulse wave velocity assessed with magnetic resonance imaging following beta-blocker therapy in the Marfan syndrome. Am J Cardiol 82:203–208
Mackenzie IS, Wilkinson IB, Cockcroft JR (2002) Assessment of arterial stiffness in clinical practice. QJM 95:67–74
Chan J, Shiino K, Obonyo NG et al (2017) Left ventricular global strain analysis by two-dimensional speckle-tracking echocardiography: the learning curve. J Am Soc Echocardiogr 30:1081–1090
Favot M, Courage C, Ehrman R, Khait L, Levy P (2016) Strain echocardiography in acute cardiovascular diseases. West J Emerg Med 17:54–60
Ryczek R, Krzesinski P, Krzywicki P, Smurzynski P, Cwetsch A (2011) Two-dimensional longitudinal strain for the assessment of the left ventricular systolic function as compared with conventional echocardiographic methods in patients with acute coronary syndromes. Kardiol Pol 69:357–362
Moreira HT, Nwabuo CC, Armstrong AC et al (2017) Reference ranges and regional patterns of left ventricular strain and strain rate using two-dimensional speckle-tracking echocardiography in a healthy middle-aged black and white population: the CARDIA study. J Am Soc Echocardiogr 30:647–658
Collier P, Phelan D, Klein A (2017) A test in context: myocardial strain measured by speckle-tracking echocardiography. J Am Coll Cardiol 69:1043–1056
Hubbard RT, Arciniegas Calle MC, Barros-Gomes S et al (2017) 2-dimensional speckle tracking echocardiography predicts severe coronary artery disease in women with normal left ventricular function: a case-control study. BMC Cardiovasc Disord 17:231
Kowalczyk E, Kasprzak JD, Wejner-Mik P, Wdowiak-Okrojek K, Lipiec P (2019) Diagnostic utility of two-dimensional speckle tracking echocardiography to identify ischemic etiology of left ventricular systolic dysfunction. Echocardiography 36:702–706
Atici A, Barman HA, Durmaz E et al (2019) Predictive value of global and territorial longitudinal strain imaging in detecting significant coronary artery disease in patients with myocardial infarction without persistent ST-segment elevation. Echocardiography 36:512–520
Al Saikhan L, Hughes AD, Chung WS, Alsharqi M, Nihoyannopoulos P (2019) Left atrial function in heart failure with mid-range ejection fraction differs from that of heart failure with preserved ejection fraction: a 2D speckle-tracking echocardiographic study. Eur Heart J Cardiovasc Imaging 20:279–290
Zou C, Jiao Y, Li X, Zheng C, Chen M, Hu C (2015) Role of ultrasonography in the evaluation of correlation between strain and elasticity of common carotid artery in patients with diabetic nephropathy. Int J Clin Exp Med 8:17765–17772
Oishi Y, Mizuguchi Y, Miyoshi H, Iuchi A, Nagase N, Oki T (2008) A novel approach to assess aortic stiffness related to changes in aging using a two-dimensional strain imaging. Echocardiography 25:941–945
Tervaert TW, Mooyaart AL, Amann K et al (2010) Pathologic classification of diabetic nephropathy. J Am Soc Nephrol 21:556–563
Li R, Cai J, Tegeler C, Sorlie P, Metcalf PA, Heiss G (1996) Reproducibility of extracranial carotid atherosclerotic lesions assessed by B-mode ultrasound: the Atherosclerosis Risk in Communities Study. Ultrasound Med Biol 22:791–799
Nambi V, Chambless L, He M et al (2012) Common carotid artery intima-media thickness is as good as carotid intima-media thickness of all carotid artery segments in improving prediction of coronary heart disease risk in the Atherosclerosis Risk in Communities (ARIC) study. Eur Heart J 33:183–190
Johnson HM, Turke TL, Grossklaus M et al (2011) Effects of an office-based carotid ultrasound screening intervention. J Am Soc Echocardiogr 24:738–747
Polak JF, Alessi-Chinetti JM, Estes JM, Patel AR (2015) Left ventricular ejection time derived from the common carotid artery Doppler waveform: association with left ventricular ejection fraction and prediction of heart failure. J Ultrasound Med 34:1237–1242
Rhee MY, Chang HK, Kim SK (2007) Intima-media thickness and arterial stiffness of carotid artery in Korean patients with Behcet’s disease. J Korean Med Sci 22:387–392
Price DJ, Wallbridge DR, Stewart MJ (2000) Tissue Doppler imaging: current and potential clinical applications. Heart 84(Suppl 2):II11–II18
Triantafyllou KA, Karabinos E, Kalkandi H, Kranidis AI, Babalis D (2009) Clinical implications of the echocardiographic assessment of left ventricular long axis function. Clin Res Cardiol 98:521–532
Shanks M, Thompson RB, Paterson ID et al (2013) Systolic and diastolic function assessment in fabry disease patients using speckle-tracking imaging and comparison with conventional echocardiographic measurements. J Am Soc Echocardiogr 26:1407–1414
Mizuguchi Y, Oishi Y, Miyoshi H, Iuchi A, Nagase N, Oki T (2008) The functional role of longitudinal, circumferential, and radial myocardial deformation for regulating the early impairment of left ventricular contraction and relaxation in patients with cardiovascular risk factors: a study with two-dimensional strain imaging. J Am Soc Echocardiogr 21:1138–1144
Radwan H, Hussein E (2017) Value of global longitudinal strain by two dimensional speckle tracking echocardiography in predicting coronary artery disease severity. Egypt Heart J 69:95–101
Shiino K, Yamada A, Scalia GM et al (2019) Early changes of myocardial function after transcatheter aortic valve implantation using multilayer strain speckle tracking echocardiography. Am J Cardiol 123:956–960
Vriz O, Bossone E, Bettio M, Pavan D, Carerj S, Antonini-Canterin F (2011) Carotid artery stiffness and diastolic function in subjects without known cardiovascular disease. J Am Soc Echocardiogr 24:915–921
Acknowledgements
The authors acknowledge the National Natural Science Foundation of China (No. 81670777), the Natural Science Foundation of Zhejiang Province (No. LY18H310010), the Natural Science Foundation of Zhejiang Province (No. LZ19H020001), and Key Medical Science and Technology Plan of Zhejiang Province (No. WKJ-ZJ-1625). The authors also thank their colleagues in the Department of Endocrinology for their cooperations.
Ethics approval and consent participate
This study was conducted as per the Declaration of Helsinki. The approval to the protocol was done by our institutional Research Ethics Committee and each regulation was followed. Each patient was made aware of the procedures and then consent was obtained from them.
Funding
This study was supported by the National Natural Science Foundation of China (No. 81670777), the Natural Science Foundation of Zhejiang Province (No. LY18H310010), the Natural Science Foundation of Zhejiang Province (No. LZ19H020001), and Key Medical Science and Technology Plan of Zhejiang Province (No. WKJ-ZJ-1625).
Author information
Authors and Affiliations
Contributions
LW and CZ designed this study. XL and HK acquired the data. LW, YD, CZH, PW, and MX interpreted the data. XL wrote and edited the manuscript. All authors reviewed the manuscript. The authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Consent for publication
Each participant gave a signed consent to publish.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, X., Kou, H., Dong, Y. et al. The value of 2D speckle-tracking strain echocardiography in evaluating the relationship between carotid elasticity and left ventricular systolic function in patients with diabetic nephropathy. Insights Imaging 11, 95 (2020). https://doi.org/10.1186/s13244-020-00897-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13244-020-00897-0