Abstract
Background
Nausea and vomiting during pregnancy (NVP) is thought to be caused by changes in maternal hormones during pregnancy. Differences in hormone exposure during prenatal life have been implicated in the causal pathways for some cases of autism spectrum disorder (ASD). However, no study has investigated whether the presence and severity of NVP may be related to symptom severity in offspring with ASD.
Methods
A large sample of children with ASD (227 males and 60 females, aged 2 to 18 years) received a clinical assessment, during which parents completed questionnaires regarding their child’s social (Social Responsiveness Scale, SRS) and communication (Children’s Communication Checklist–2nd edition, CCC-2) symptoms. Parents also reported on a 5-point scale the frequency and severity of NVPs during the pregnancy of the child being assessed: (1) no NVP during the pregnancy, (2) occasional nausea, but no vomiting, (3) daily nausea, but no vomiting, (4) occasional vomiting, with or without nausea, and (5) daily nausea and vomiting.
Results
Impairments in social responsiveness in offspring, as indexed by SRS total score, significantly increased as a function of the frequency and severity of their mothers’ NVP, as did the level of language difficulties as indexed by the Global Communication Composite of the CCC-2.
Conclusions
The strong, positive association between increasing frequency and severity of NVP and ASD severity in offspring provides further evidence that exposure to an atypical hormonal environment during prenatal life may affect neurodevelopment and contribute to the ASD phenotype. Given that the measure of NVP symptoms in the current study was based on retrospective recall, replication of this finding is required before strong conclusions can be drawn.
Similar content being viewed by others
Background
Autism spectrum disorder (ASD) is the collective term for developmental disabilities characterized by impairments in social interaction and verbal and nonverbal communication and by repetitive patterns of behavior. While the biological pathways contributing to ASD remain unclear, current consensus is for a multifactorial etiology, incorporating a constellation of genetic risk variants that may interact with environmental factors [1]. The in utero hormone environment is critical to development of the structure and function of the central nervous system, and there is increasing evidence that prenatal endocrine factors may also play a key role in the etiology of some cases of ASD [2]. A particular focus of previous research has been on fetal exposure to elevated levels of androgens, measured via sampling of amniotic fluid during the second trimester [3] and umbilical cord blood at birth [4]. Exposure to elevated concentrations of prenatal androgens has been found to be related to a diagnosis of clinical ASD in offspring [3], as well as autistic-like traits in the general population [5, 6], particularly communication difficulties [7, 8]. While it is important to highlight that these findings have not always been replicated [4, 9], further support for the potential role of the prenatal hormone environment in the etiological pathways contributing to ASD has been observed through associations with factors known to influence maternal hormone status, such as maternal age at menarche [10], pre-pregnancy BMI [11], and infertility and its treatments [10, 12]. This evidence strongly supports the further examination of how prenatal endocrine factors may contribute to ASD.
Nausea and vomiting during pregnancy (NVP) is experienced by approximately 70 to 80% of pregnant women [13]. The timing, frequency, and duration of NVP varies between women and, in its most extreme form (hyperemesis gravidarum), is characterized by severe and persistent nausea and vomiting that results in a significant loss in body weight [14]. While NVP is known to involve a heritable component [15, 16], the biological mechanisms underpinning the maternal experience of severe NVP are thought to involve the dysregulation of maternal human chorionic gonadotropin (hCG), thyroid hormones (particularly thyroxine and thyroid-stimulating hormone), and estrogens [14, 17]. There are a number of reasons to hypothesize a link between NVP and the ASD phenotype among offspring. First, women who experience hyperemesis gravidarum have a greater risk of having a child with behavioral and neurodevelopmental conditions [18, 19]. While no study has been sufficiently powered to investigate offspring risk for ASD, an increased risk has been observed for common neurodevelopmental comorbidities for ASD, such as intellectual disability, developmental language disorder, and attentional deficit hyperactivity disorder [20]. Second, differential levels of hCG during pregnancy have been associated with later ASD in offspring. A recent study of Californian state records examined the association between hCG levels during pregnancy (collected for routine screening between 15 and 20 weeks’ pregnancy) and the prevalence of ASD among offspring [21]. An increased risk of offspring ASD was identified for women with the highest and lowest decile of hCG concentration distribution, suggesting a link between atypical hCG regulation and offspring ASD. Third, a number of large studies have identified an association between maternal autoimmune thyroid disease during pregnancy and risk for ASD [22, 23], with a recent meta-analysis reporting a pooled odds ratio of 1.29 (95% confidence interval 1.14–1.45) [24].
Considered together, the accumulating body of research presents the hypothesis that an atypical profile of pregnancy-related hormones may be involved in the etiological pathway for some cases of ASD, and that this may be indexed by NVP. The current study provides the first investigation of whether maternal NVP relates to symptom severity in children with ASD. Given evidence linking the experience of any nausea or vomiting symptoms during pregnancy to hormone dysregulation [25], the study examined ASD symptomatology in relation to the full severity of NVP symptoms. Based on previous findings linking NVP to neurodevelopmental delay and disorder [20], and the association between hormones implicated in NVP and risk for offspring ASD [21], we hypothesized that increased frequency and severity of maternal NVP would relate to more severe ASD symptoms among children.
Methods
Participant sample
Participants were part of the Western Australian Autism Biological Registry, which is an ongoing study of children with ASD and their families taking place at the Telethon Kids Institute in Perth, Western Australia [26]. Participants were recruited via newspaper advertisements, and children with a clinical diagnosis of an ASD were included in the study. In Western Australia, diagnosis of ASD is strictly regulated and obtained by consensus following a multidisciplinary assessment by a team comprising a pediatrician, clinical psychologist, and speech pathologist [27]. Ethics approval for the WAABR was granted by the Human Ethics Committee at Princess Margaret Hospital for Children in Perth, Western Australia. The primary caregiver provided informed consent to be a part of the study. The sample included 227 males and 60 females with ASD aged 2 to 18 years at the time of data collection (mean = 8.28 years; SD = 3.89 years).
Procedure
Parents and their child(ren) with ASD were invited to the Telethon Kids Institute for a face-to-face assessment. One week prior to this assessment, parents were mailed several questionnaires, which they were asked to complete and return to the research team at the time of the research appointment.
Obstetric history
A primary caregiver completed a family history questionnaire, which included questions about demographic characteristics and the social and medical history of the family. A section in the questionnaire asked questions about the history of the pregnancy that resulted in the child with ASD, including questions about any obstetric complications that occurred. The child’s biological mother was specifically asked to complete this section. Fetal growth restriction was defined as a birthweight lower than the 10th percentile for gestational age, according to Australian norms [28]. A specific question in the questionnaire asked whether the mother experienced nausea and/or vomiting during pregnancy, and respondents were asked to answer on a 5-point scale: (1) no nausea or vomiting, (2) occasional nausea, but no vomiting, (3) daily nausea, but no vomiting, (4) occasional vomiting, with or without nausea, and (5) daily nausea and vomiting.
ASD symptom severity
The primary caregiver was asked to complete two questionnaires relating to their child’s ASD symptomatology.
Social Responsiveness Scale–Parent Report Form
The Social Responsiveness Scale (SRS) is a 65-item caregiver report questionnaire designed to measure social behavior, language, and repetitive behavior/restricted interests in children [29]. Each item asks about a social behavior, which respondents rate on a scale from 0 (never true) to 3 (almost always true). In addition to the SRS total score, there are five subscales assessing social awareness, social cognition, social communication, social motivation, and autistic mannerisms. Analyses were conducted on the raw scores for the total scale and for the subscales since these scores were normally distributed, whereas the distributions for norm-based T scores were skewed, containing a substantial proportion of cases scoring at the maximum T scores (T ≥ 90). Higher scores indicate more pronounced ASD symptoms. SRS total scores were available for 282 of the cases (223 males, 59 females).
Children’s Communication Checklist–2nd edition.
The Children’s Communication Checklist–2nd edition (CCC-2) [30] is a 70-item parent report questionnaire designed to screen for communication difficulties in children with phrase speech. The scale is comprised of ten subscales that measure general communication difficulties (speech, syntax, semantics and coherence), pragmatic language (inappropriate initiation, stereotyped language, use of context, and nonverbal communication), and behaviors commonly associated with ASD (social behavior and interests). Age-referenced standard scores with a mean of 10 (SD = 3) can be derived for each subscale for participants aged between 4 and 18 years. A composite measure of communication ability is also obtained (Global Communication Composite, GCC), which is a summed score of the eight subscales relating to general communication difficulties and pragmatic language. On all scales, lower scores equate to greater difficulties. GCC scores were available for 209 participants (166 males, 43 females) aged 4–18 years.
Statistical analyses
SRS raw and CCC-2 standard scores were checked for outliers using the criterion |z| ≥ 3.29. No more than two outliers were identified for any single measure. These scores were removed prior to the further analysis. The principal analyses consisted of two ANCOVAs conducted on the SRS total scores and CCC-2 GCC standard scores, with four covariates: paternal age, maternal age, child sex, and the child’s age at assessment (which either differed across NVP groups or correlated with the key symptom variables; see below). In follow-up analyses, linear, quadratic, cubic, and quartic trends were calculated for the NVP factor. A power analysis (Additional file 1) indicated that the study was not sufficiently powered (d < 0.8) to examine the data separately by sex, due to the relatively small number of females (n = 60). Given the increasing interest in sex differences in ASD [31], the sex-specific descriptive statistics for the SRS and CCC-2 (total/GCC and subscales) have been included as Additional file 1. However, we urge caution in the interpretation of these data given the concerns pertaining to low statistical power and multiple comparisons.
Results
Demographic characteristics of NVP groups
Table 1 provides descriptive statistics for the five groups defined by frequency and severity of the mothers’ NVP. The distribution of cases across the NVP groups differed for males and females, χ2(4) = 12.24, p < .05 (see Table 1). In particular, the most severe form of NVP was experienced by 31.67% of the mothers of females but by only 17.62% of the mothers of males, with χ2(1) = 5.73, p < .05, for this comparison. In the current sample, the distribution of cases across the NVP categories did not depend on whether the mother had preeclampsia during pregnancy, χ2(4) = 4.58, p = .33, or whether, at birth, the child was assisted in breathing, χ2(4) = 2.57, p = .63, or required special nursery care, χ2(4) = 4.07, p = .40. The NVP group was also unrelated to fetal growth restriction in males, χ2(4) = 2.15, p = .71, or females, χ2(4) = .52, df = 4, p = .97. Comparisons using one-way ANOVA also showed that the NVP groups did not differ on age at time of data collection, F(4,282) = 1.14, p = .34, \( {\eta}_p^2 \) = .016, age when ASD was diagnosed, F(4,270) = 1.55, p = .19, \( {\eta}_p^2 \) = .022, and gestational age at birth, F(4,274) = 0.76, p = .56, \( {\eta}_p^2 \) = .011. However, the NVP groups did differ significantly on paternal age at conception of the child, F(4,279) = 2.91, p < .05, \( {\eta}_p^2 \) = .040, and the analysis comparing the groups on maternal age at conception yielded a marginally significant result, F(4,281) = 2.02, p = .09, \( {\eta}_p^2 \) = .028 (see Table 1 for means).
Relationships of ASD symptom severity measures to demographic variables
SRS total and CCC-2 GCC scores were correlated with the child’s age at assessment, maternal and paternal age at conception of the child, and child’s gestational age at birth. SRS total score correlated significantly with both the child’s age at assessment, r = 0.21, p < .001, and maternal age, r = − .16, p < .01, and CCC-2 GCC scores also correlated with the child’s age at assessment, r = − .44, p < .001. No other correlations were significant. Neither of the two key symptom measures differed significantly as a function of whether the mother had preeclampsia during pregnancy, larger t(207) = 1.26, p = .21, nor whether the newborn was assisted in breathing at birth, larger t(278) = .37, p = .71, required special nursery care, larger t(277) = .77, p = .44, or was of restricted growth at birth, larger t(252) = .73, p = .19.
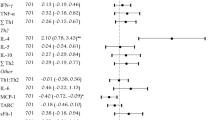
ASD symptom severity as a function of maternal NVP
Table 2 presents SRS total score and the CCC-2 GCC according to the NVP variable. The ANCOVA conducted on the SRS total scores yielded a significant main effect of NVP group, F(4,277) = 4.15, p .003, \( {\eta}_p^2 \) = .057. Figure 1a illustrates how social difficulties increase as a function of more severe levels of NVP, with the linear trend yielding t(277) = 3.36, p < .001, ηp2 = .039. The ANCOVA of the CCC-2 GCC data also revealed a significant main effect of the NVP group, F(4,204) = 2.65, p < .035, \( {\eta}_p^2 \) = .049, with lower GCC scores (i.e., greater language difficulties) associated with more severe maternal NVP (see Fig. 1b). Most of the variance in GCC scores across levels of NVP accounted for by the linear trend, t(204) = 3.13, p = .002, ηp2 = .046.
Discussion
This is the first study to report the relationship between maternal experience of NVP and ASD severity in offspring. Increasing frequency and severity of NVP was positively related to the severity of social difficulties (SRS total score) and communication impairments (CCC-2 GCC scale) in offspring. The difference in the average SRS total and CCC-2 GCC scores between the offspring of mothers who experienced no NVP and those whose mothers had daily nausea and vomiting was approximately 0.8 of a standard deviation for each measure. While no study has quantified a clinically significant difference using these measures, a difference of this magnitude is highly likely to reflect clinically relevant differences in the severity of each phenotype. The cause of NVP is multifactorial and most likely involves pregnancy-related changes in the maternal hormone milieu. While the current study did not directly measure maternal hormones during pregnancy, there is considerable evidence linking the maternal experience of NVP to dysregulation of hCG, thyroid hormones, and estrogens. Several studies have reported an increased risk for offspring ASD among women experiencing dysregulation of hCG [21] and thyroid hormones [22,23,24] during pregnancy. The current study is the first to identify a link between NVP and the severity of ASD phenotype and provides further evidence for the possible involvement of prenatal hormone exposure in the causal pathway(s) for the ASD behavioral phenotype [3].
It is important to highlight that non-hormonal factors have also been linked to the onset of NVP. For example, twin studies have reported high heritability for NVP both within the normal range [32] and at the clinical extreme (hyperemesis gravidarum) [33]. A potentially fruitful line of research would be to examine how NVP may co-occur with heritable autistic traits—the so called broader autism phenotype [34]—in mothers of children with ASD. The co-occurrence of these two phenotypes at above chance levels may afford further insights into the pattern of findings identified in the current study. Furthermore, several studies have found that between 90 and 95% of women with hyperemesis gravidarum are seropositive for Helicobacter pylori (H. pylori) compared to between 45 and 50% of women who do not experience NVP [35, 36]. While these prevalence figures have not always been replicated [37], a meta-analysis of 25 case-control studies reported a pooled odds ratio of 3.32 (95% confidence interval 2.25–4.90) for H. pylori infection in women with hyperemesis gravidarum [38]. Unlike hormonal theories for NVP, the biological pathways linking maternal H. pylori infection and disrupted fetal neurodevelopment are less clear. Recent evidence from both preclinical [39] and human studies [40] suggests that maternal infection with H. pylori is associated with a higher risk of fetal growth restriction, which may implicate poor placental function [41]. Furthermore, numerous epidemiological studies have found that maternal H. pylori infection increases risk for pre-eclampsia [42, 43], potentially through negative effects on early placental development and function [44]. However, it is important to emphasize that H. pylori was not measured in this study and the rate of gestational hypertension and preeclampsia in the study sample was low, and thus, it was difficult to ascertain its relationship with maternal NVP. An alternative potential mechanism is the possible effect that a maternal inflammatory reaction (in response to H. pylori infection) may have on the developing fetus [45]. There is a strong literature describing the effects of maternal immune activation during pregnancy on fetal neurodevelopment [46], with a particular focus on the increased risk of offspring ASD [47,48,49]. However, no study has examined maternal H. pylori infection in relation to offspring ASD, and it remains unclear how bacteria that infects the stomach of half of the human population [50] may cause an inflammatory response that disrupts neurodevelopment in only a relatively small proportion of children.
Another area of growing research interest is how the sex of the fetus may influence vulnerability to differences in the prenatal environment. While the majority of research in this area has highlighted the vulnerability of male fetuses to prenatal perturbations, the effects of NVP and associated hormones on fetal outcomes has predominantly identified effects for female offspring. Numerous epidemiological studies have found that NVP is more common when gestating a female fetus [51,52,53], and this finding was replicated in the current study. Several studies have also reported that maternal experience of NVP [53] and increased hCG concentrations during pregnancy [54] influence growth rates in female but not male fetuses. The mechanisms by which biological sex may impart vulnerability or protection on the fetal nervous system remain largely unknown [55]. Fetal growth rate is reflective of intrauterine conditions, and fetal growth restriction is known to be associated with poor placental function [56]. There is increasing evidence that the placenta functions in a sex-specific manner and has different interactions with steroid pathways, growth factor pathways, and the fetal-placental immune system depending on the sex of the fetus [57]. While the current study did not have adequate statistical power to conduct analyses separately for male and female offspring (see Additional file 1), this background evidence suggests that an investigation of whether offspring sex moderates the relationship between NVP severity and ASD symptomatology is an important priority for future research.
A strength of the study design was the availability of standardized and widely used assessments of symptomatology on a large cohort of children with ASD that were assessed in a single geographic location (Perth, Western Australia), thus limiting bias in data collection methods. However, we note two important limitations of the study design. First, the scale used to measure NVP was developed for the purpose of this study and has not undergone broader validation. The most widely used prospective scale—the Pregnancy-Unique Quantification of Emesis and nausea (PUQE) [58]—asks women about NVP symptoms in the immediately preceding 12-h period. Given the retrospective nature of the current study, the PUQE was not considered a reliable measure of NVP, and the scale used in the current study incorporated broader NVP categories asking about daily NVP experiences (compared to hourly experiences in the PUQE). However, a major limitation of this scale is the lack of information on the timing and duration of NVP experienced by the mothers. While it is estimated that 91% of women experience NVP prior to 20 weeks’ gestation [59], there is considerable variability in the onset (and therefore duration) of symptoms. This information was not recorded in the current study, which limits the conclusions that can be drawn from the dataset. Furthermore, while the current study identified significant linear trends across NVP categories of increasing frequency and different symptomatology (nausea vs vomiting), it remains unclear whether these represent a true gradient of NVP severity. However, we note that treatment studies for NVP often differentiate between nausea and vomiting in defining NVP symptoms of increasing severity [60], and epidemiological studies have identified differential relationships between these categories and a number of pregnancy [61] and offspring [62, 63] outcomes.
A second limitation is that the obstetric information, including information on NVP, was collected via retrospective maternal report, which may be subject to a recall bias [64]. While the maternal experience of hyperemesis gravidarum is routinely noted in medical records, the full spectrum of NVP symptomatology is not prospectively recorded, which makes it challenging to determine the accuracy of maternal recall in this study. An average of 8 years had passed since the experience of NVP in the current maternal sample. While there is evidence that mothers have moderate levels of accuracy in recalling severe obstetric events (e.g., hyperemesis gravidarium) across this time period [65], there is less evidence of the validity of recall of the broader spectrum of NVP symptoms. Previous studies have also reported that a child’s health status can bias maternal recall [66], such that mothers of children with greater health or developmental difficulties may be less accurate in recalling obstetric events. While there is no evidence for this phenomenon in the ASD population, the possibility that mothers of children with more severe ASD symptoms inaccurately recalled more severe NVP symptoms than they actually experienced remains an important consideration in the interpretation of the current findings.
Conclusion
The current study identified a positive association between increasing frequency and severity of maternal NVP and ASD severity in offspring. Based on current understanding of the biological mechanisms underpinning NVP, the findings from the current study provide further evidence that exposure to an atypical prenatal hormone environment may affect neurodevelopment and contribute to the ASD phenotype. Given this is the first such finding, replication of this effect in a separate cohort is a priority before any further conclusions can be made. Furthermore, the current study only examined NVP in pregnancies that produced an offspring who received an ASD diagnosis. Future studies can extend this work through a “within family” study design that compares the maternal experience of NVP between pregnancies from the same mother that resulted in a child with ASD and a sibling without ASD.
Abbreviations
- ASD:
-
Autism spectrum disorder
- CCC-2:
-
Children’s Communication Checklist–2nd edition
- GCC:
-
Global Communication Composite
- H. pylori :
-
Helicobacter pylori
- hCG:
-
Human chorionic gonadotropin
- NVP:
-
Nausea and vomiting during pregnancy
- SRS:
-
Social Responsiveness Scale
References
Jeste SS, Geschwind DH. Disentangling the heterogeneity of autism spectrum disorder through genetic findings. Nat Rev Neurol. 2014;10:74–81.
Gore AC, Martien KM, Gagnidze K, Pfaff D. Implications of prenatal steroid perturbations for neurodevelopment, behavior, and autism. Endocr Rev. 2015;35:961–91.
Baron-Cohen S, Auyeung B, Norgaard-Pederson B, Hougaard DM, Abdallah MW, Melgaard L. Elevated fetal steroidogenic activity in autism. Mol Psychiatry. 2015;20:369–76.
Whitehouse A, Mattes E, Maybery M, Dissanayake C, Sawyer M, Jones R. Perinatal testosterone exposure and autistic-like traits in the general population: a longitudinal pregnancy-cohort study. J Neurodev Disord. 2012;4:25.
Auyeung B, Baron-Cohen S, Ashwin E, Knickmeyer R, Taylor K, Hackett G. Fetal testosterone and autistic traits. Br J Psychol. 2009;100:1–22.
Knickmeyer R, Baron-Cohen S, Raggatt P, Taylor K. Foetal testosterone, social relationships, and restricted interests in children. J Child Psychol Psyc. 2005;46:198–210.
Whitehouse AJO, Mattes E, Maybery MT, Sawyer MG, Jacoby P, Keelan JA. Sex-specific associations between umbilical cord blood testosterone levels and language delay in early childhood. J Child Psychol Psyc. 2012;53:726–34.
Hollier LP, Mattes E, Maybery MT, Keelan JA, Hickey M, Whitehouse AJO. The association between perinatal testosterone concentration and early vocabulary development: a prospective cohort study. Biol Psychol. 2013;92:212–5.
Kung KTF, Constantinescu M, Browne WV, Noorderhaven RM, Hines M. No relationship between early postnatal testosterone concentrations and autistic traits in 18 to 30-month-old children. Mol Autism. 2016;7:15.
Lyall K, Pauls DL, Santangelo S, Spiegelman D, Ascherio A. Maternal early life factors associated with hormone levels and the risk of having a child with an autism spectrum disorder in the nurses’ health study II. J Autism Dev Disord. 2010;41:618–27.
Krakowiak P, Walker CK, Bremer AA, Baker AS, Ozonoff S, Hansen RL. Maternal metabolic conditions and risk for autism and other neurodevelopmental disorders. Pediatrics. 2012;129:e1121–e8.
Hvidtjorn D, Grove J, Schendel D, Schieve LA, Svaerke C, Ernst E, et al. Risk of autism spectrum disorders in children born after assisted conception: a population-based follow-up study. J Epidemiol Community H. 2011;65:497–502.
Pepper GV, Craig Roberts S. Rates of nausea and vomiting in pregnancy and dietary characteristics across populations. Proc Biol Sci. 2006;273:2675–9.
Bustos M, Venkataramanan R, Caritis S. Nausea and vomiting of pregnancy—what’s new? Auton Neurosci. 2017;202:62–72.
Corey LA, Berg K, Solaas MH, Nance WE. The epidemiology of pregnancy complications and outcome in a Norwegian twin population. Obstet Gynaecol. 1992;80:989–94.
Vikanes AV, Skjaerven R, Grjibovski AM, Gunnes N, Vangen S, Magnus P. Recurrence of hyperemesis gravidarum across generations: population based cohort study. Brit Med J. 2010;340:c2050.
Niemeijer MN, Grooten IJ, Vos N, Bais JM, van der Post JA, Mol BW, et al. Diagnostic markers for hyperemesis gravidarum: a systematic review and metaanalysis. Am J Obstet. 2014;211:e151–15.
Mullin P, Bray A, Schoenberg-Paik F. Prenatal exposure to hyperemesis gravidarum linked to increased risk of psychological and behavioral disorders in adulthood. J Dev Orig Dis. 2011;2:200–4.
Mullin P, Bray A, Vu V. No increased risk of psychological/behavioral disorders in siblings of women with hyperemesis gravidarum unless their mother had HG. J Dev Orig Dis. 2012;3:375–9.
Fejzo MS, Magtira A, Schoenberg FP, Macgibbon K, Mullin P. Neurodevelopmental delay in children exposed in utero to hyperemesis gravidarum. Eur J Obstet Gynecol Reprod. 2015;189:79–84.
Windham GC, Lyall K, Anderson M, Kharrazi M. Autism spectrum disorder risk in relation to maternal mid-pregnancy serum hormone and protein markers from prenatal screening in California. J Autism Dev Disord. 2016;46:478–88.
Andersen SL, Laurberg P, Wu CS, Olsen J. Attention deficit hyperactivity disorder and autism spectrum disorder in children born to mothers with thyroid dysfunction: a Danish nationwide cohort study. Brit J Obstet Gynaecol. 2014;121:1365–74.
Brown AS, Surcel HM, Kinkka-Yli-Alomaki S, Cheslack-Postava K, Bao A, Sourander A. Maternal thyroid autoantibody and elevated risk of autism in a national birth cohort. Biol Psychiatry. 2015;57:86–92.
Chen SW, Zhong XS, Jiang LN, Zheng XY, Xiong YQ, Ma SJ, et al. Maternal autoimmune diseases and the risk of autism spectrum disorders in offspring: a systematic review and meta-analysis. Behav Brain Res. 2016;296:61–9.
Lagiou P, Tamimi R, Mucci LA, Trichopoulos D, Adami H-O, Hsieh C-C. Nausea and vomiting in pregnancy in relation to prolactin, estrogens, and progesterone: a prospective study. Obstet Gynecol. 2003;101(4):639–44.
Taylor LJ, Maybery M, Wray J, Ravine D, Hunt A, Whitehouse AJO. Do the nature of communication impairments in autism spectrum disorders relate to the broader autism phenotype in parents? J Autism Dev Disord. 2013;43:2984–9.
Whitehouse AJO, Cooper MN, Bebbington K, Alvares G, Lin A, Wray J, et al. Evidence of a reduction over time in the behavioral severity of autistic disorder diagnoses. Autism Res. 2017;10:179–87.
Dobbins TA, Sullivan EA, Roberts CL, Simpson JM. Australian national birthweight percentiles by sex and gestational age, 1998–2007. Med J Aust. 2012;197:291–4.
Constantino JN, Gruber C. The Social Responsiveness Scale. Los Angeles: Western Psychological Services; 2005.
Bishop DVM. The Children’s Communication Checklist (2nd Ed.). London: Psychological Corporation; 2003.
Halladay AK, Bishop S, Constantino JN, Daniels AM, Koenig K, Palmer K, et al. Sex and gender differences in autism spectrum disorder: summarizing evidence gaps and identifying emerging areas of priority. Molecular Autism. 2015;6(1):36.
Colodro-Conde L, Jern P, Johansson A, Sánchez-Romera JF, Lind PA, Painter JN, et al. Nausea and vomiting during pregnancy is highly heritable. Behav Genet. 2016;46(4):481–91.
Corey LA, Berg K, Solaas MH, Nance WE. The epidemiology of pregnancy complications and outcome in a Norwegian twin population. Obstet Gynecol. 1992;80(6):989–94.
Rubenstein E, Chawla D. Broader autism phenotype in parents of children with autism: a systematic review of percentage estimates. J Child Family Stud. 2018;27(6):1705–20.
Frigo P, Lang C, Reisenberger K, Kolbl H, Hirschl AM. Hyperemesis gravidarum associated with Helicobacter pylori seropositivity. Obstet Gynaecol. 1998;91:615–7.
Bagis T, Gumurdulu Y, Kayaselcuk F, Yilmaz ES, Killicadag E, Tarim E. Endoscopy in hyperemesis gravidarum and Helicobacter pylori infection. Int J Gynaecol Obstet. 2002;79:105–9.
Berker B, Soylemez F, Cengiz SD, Kose SK. Serologic assay of Helicobacter pylori infection. Is it useful in hyperemesis gravidarum. J Reprod Med. 2003;48:809–12.
Sandven I, Abdelnoor M, Britt-Ingjerd N, Melby KK. Helicobacter pylori infection and hyperemesis gravidarum: a systematic review and meta-analysis of case–control studies. Acta Obstet Gynecol Scand. 2009;88:1190–200.
Rossi G, Romagnoli S, Lauretti L, Pancotto L, Taccini E, Rappuoli R, et al. Helicobacter pylori infection negatively influences pregnancy outcome in a mouse model. Helicobacter. 2004;9:152–7.
Eslick GD, Yan P, Xia HH-X, Murray H, Spurrett B, Talley NJ. Foetal intrauterine growth restrictions with Helicobacter pylori infection. Aliment Pharmacol Ther. 2002;16:1677–82.
Cetin I, Alvino G. Intrauterine growth restriction: implications for placental metabolism and transport. A review. Placenta. 2009;30(Supplement):77–82.
Ponzetto A, Cardaropoli S, Piccoli E, Rolfo A, Gennero L, Kanduc D. Pre-eclampsia is associated with Helicobacter pylori seropositivity in Italy. J Hypertens. 2006;24:2445–9.
UstUn Y, Engin-UstUn Y, Ozkaplan E, Otlu B, SaitTekerekoGlu M. Association of Helicobacter pylori infection with systemic inflammation in preeclampsia. J Matern Fetal Med. 2012;23:311–4.
Cardaropoli S, Rolfo A, Piazzese A, Ponzetto A, Todros T. Helicobacter pylori’s virulence and infection persistence define pre-eclampsia complicated by fetal growth retardation. World J Gastroenterol. 2011;17:5156–65.
Wilson KT, Crabtree JE. Immunology of Helicobacter pylori: insights into the failure of the immune response and perspectives on vaccine studies. Gastroenterology. 2007;133:288–308.
Deverman BE, Patterson PH. Cytokines and CNS development. Neuron. 2009;64:61–78.
Parker-Athill EC, Tan J. Maternal immune activation and autism spectrum disorder: interleukin-6 signaling as a key mechanistic pathway. Neurosignals. 2011;18:113–28.
Braunschweig D, Krakowiak P, Duncanson P, Boyce R, Hansen RL, Ashwood P, et al. Autism-specific maternal autoantibodies recognize critical proteins in developing brain. Translat Psychiatry. 2013;3:e277.
Jiang HY, Xu LL, Shao L, Xia RM, Yu ZH, Ling ZX, et al. Maternal infection during pregnancy and risk of autism spectrum disorders: a systematic review and meta-analysis. Brain Behav Immun. 2016;133:288–308.
Eusebi LH, Zagari RM, Bazzoli F. Epidemiology of Helicobacter pylori infection. Helicobacter. 2014;19:1–5.
Källén B. Hyperemesis during pregnancy and delivery outcome: a registry study. Eur J Obstet Gynecol Reprod. 1987;26:291–302.
Askling J, Erlandsson G, Kajser M, Akre O. Sickness in pregnancy and sex of child. Lancet. 1999;354:2053.
Vandraas KF, Vikanes AV, Stoer NC, Vangen S, Magnus P, Grjibovski AM. Is hyperemesis gravidarum associated with placental weight and the placental weight-to-birth weight ratio? A population-based Norwegian cohort study. Placenta. 2013;34:990–4.
Barjaktarovic M, Korevaar TIM, Jaddoe VWV, de Rijke YB, Visser TJ, Peeters RP, et al. Human chorionic gonadotropin (hCG) concentrations during the late first trimester are associated with fetal growth in a fetal sex-specific manner. Eur J Epidemiol. 2017;32:135–44.
Sundrani DP, Roy SS, Jadhav AT, Joshi SR. Sex-specific differences and developmental programming for diseases in later life. Reprod Fertil Dev. 2017;29:2085–99.
Clifton VL. Review: sex and the human placenta: mediating differential strategies of fetal growth and survival. Placenta. 2010;31:S33–S9.
Hsiao EY, Patterson PH. Placental regulation of maternal-fetal interactions and brain development. Dev Neurobiol. 2012;72:1317–26.
Koren G, Boskovic R, Hard M, Maltepe C, Navioz Y, Einarson A. Motherisk—PUQE (pregnancy-unique quantification of emesis and nausea) scoring system for nausea and vomiting of pregnancy. Am J Obstet Gynecol. 2002;186(5, Supplement 2):S228–S31.
Gadsby R, Barnie-Adshead AM, Jagger C. A prospective study of nausea and vomiting during pregnancy. Br J Gen Pract. 1993;43(371):245–8.
McParlin C, O’Donnell A, Robson SC, et al. Treatments for hyperemesis gravidarum and nausea and vomiting in pregnancy: a systematic review. JAMA. 2016;316(13):1392–401.
Chortatos A, Haugen M, Iversen PO, Vikanes Å, Eberhard-Gran M, Bjelland EK, et al. Pregnancy complications and birth outcomes among women experiencing nausea only or nausea and vomiting during pregnancy in the Norwegian mother and child cohort study. BMC Pregnancy Childb. 2015;15(1):138.
Chan RL, Olshan AF, Savitz DA, Herring AH, Daniels JL, Peterson HB, et al. Severity and duration of nausea and vomiting symptoms in pregnancy and spontaneous abortion. Hum Reprod. 2010;25(11):2907–12.
Hinkle SN, Mumford SL, Grantz KL, et al. Association of nausea and vomiting during pregnancy with pregnancy loss: a secondary analysis of a randomized clinical trial. JAMA Intern Med. 2016;176(11):1621–7.
Koren G, Maltepe C, Navioz Y, Wolpin J. Recall bias of the symptoms of nausea and vomiting of pregnancy. Am J Obstet Gynecol. 2004;190:485–8.
Sou SC, Chen WJ, Hsieh W, Jeng S. Severe obstetric complications and birth characteristics in preterm or term delivery were accurately recalled by mothers. J Clin Epidemiol. 2006;59(4):429–35.
McCormick MC, Brooks-Gunn J. Concurrent child health status and maternal recall of events in infancy. Pediatrics. 1999;104(Supplement 6):1176–81.
Funding
This research program is supported by the Angela Wright Bennett Foundation. Andrew Whitehouse is supported by a NHMRC Senior Research Fellowship (#1077966). The funders had no influence over the design of the study, nor data collection, analysis, and interpretation.
Availability of data and materials
The datasets used during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
AJOW, GA, KV, and MM conceived the study design. All authors were involved in data collection. MM conducted the data analysis, and all authors were involved in the data interpretation. AJOW wrote the initial draft of the manuscript, and all authors provided critical feedback that contributed to the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval for the WAABR was granted by the Human Ethics Committee at Princess Margaret Hospital for Children in Perth, Western Australia. The primary caregiver provided informed consent to be a part of the study.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Power analyses for a one-way ANOVA of the results. Table S1. Power analyses for a one-way ANOVA of the five-level NVP variable. Table S2. Means (SD, n) for the total and subscale scores of the SRS as a function of maternal nausea and vomiting during pregnancy and child sex. Higher scores equates to greater levels of impairment. Table S3. Means (SD, n) for the General Communication Composite and subscale standard scores of the CCC-2 as a function of maternal nausea and vomiting during pregnancy and child sex. Lower scores equate to greater levels of impairment. (DOCX 46 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Whitehouse, A.J.O., Alvares, G.A., Cleary, D. et al. Symptom severity in autism spectrum disorder is related to the frequency and severity of nausea and vomiting during pregnancy: a retrospective case-control study. Molecular Autism 9, 37 (2018). https://doi.org/10.1186/s13229-018-0223-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13229-018-0223-7