Abstract
Background
This study aimed to evaluate, longitudinally, the outcome of periodontal regenerative therapy using a deproteinized bovine bone mineral (DBBM) in combination with a collagen barrier (CB) for the treatment of intrabony defects.
Results
Patients with chronic periodontitis who have completed initial periodontal therapy participated in this study. They had at least one 2- or 3-wall intrabony periodontal defect of ≥3 mm in depth. During surgery, defects were filled with DBBM and covered with CB. Ten patients completed 2.5-year reevaluation. At baseline, mean clinical attachment level (CAL) of the treated site was 8.0 mm and mean probing depth (PD) was 7.5 mm. Mean depth of intrabony component was 4.6 mm. Mean gains in CAL at 6 months and 2.5 years were 2.8 ± 1.0 and 1.4 ± 1.5 mm, respectively, both showing a significant improvement from baseline. CAL gains at 1 and 2.5 years were significantly reduced from that at 6 months. A significant improvement in PD was also noted: mean reductions in PD at 6 months and 2.5 years were 4.0 ± 0.8 and 3.2 ± 0.8 mm, respectively.
Conclusions
The combination therapy using DBBM and CB yielded statistically significant effects such as CAL gain and PD reduction, up to 2.5 years in the treatment of intrabony defects. However, the trend for decrease in CAL gain over time calls for the need for careful maintenance care.
Similar content being viewed by others
Background
Periodontitis is an inflammatory disease of tooth supporting tissues induced by plaque biofilm [1] and also considered as a dysbiotic disease with an adverse effect on systemic health [2]. In the treatment of periodontitis, initial periodontal therapy consisting of plaque control and scaling and root planing is the fundamental non-surgical treatment. In cases of moderate to advanced periodontitis, surgical interventions are often necessary.
Guided tissue regeneration (GTR) is defined as ‘a surgical procedure with the goal of achieving new bone, cementum, and periodontal ligament attachment to a periodontally diseased tooth, using barrier devices or membranes to provide space maintenance, epithelial exclusion, and wound stabilization’ [3]. GTR has been successfully used for the regeneration of periodontal tissues for more than three decades [4]. For the treatment of intrabony defects (periodontal defect within the bone surrounded by one, two or three bony walls or combination of thereof), especially those with uncontained configuration (1 or 2 wall) or ≥3-mm width, combination GTR therapy is recommended [5]. Various bone graft materials can be used with barrier membranes [6, 7]. GTR using a deproteinized bovine bone mineral (DBBM) combined with a collagen barrier (CB) membrane has been reported to yield more gains in clinical attachment level (CAL) than flap operation alone [8, 9]. Furthermore, the combination therapy demonstrated a significantly more periodontal regeneration than each individual component [10, 11]. Although these GTR therapies yielded clinically favourable results, a substantial degree of variability in the outcome has been reported with a marked center effect [6, 12, 13], and longitudinal data are still limited. Furthermore, according to the practice guideline by the Japanese Society of Periodontology, the evidence for added benefit of the combination GTR therapies is not yet sufficient [14].
Previously, we conducted a series of prospective multicenter studies of the GTR using a DBBM (Bio-Oss®, Geistlich Pharma AG, Switzerland) and a non-cross-linked CB (Bio-Gide®, Geistlich) in the treatment of intrabony defect, and reported that the combined use of the DBBM and CB yielded a significant gain in CAL and reduction in probing depth (PD) at 6 months following surgery [15, 16]. We hypothesized that the favourable clinical outcome can be sustained for longer period of time, following this combination therapy.
This study aimed to assess 2.5-year clinical outcome of periodontal regenerative therapy using DBBM in combination with CB in the treatment of intrabony defects in patients with chronic periodontitis.
Methods
Study design and participants
This study presents a subset of patients who were treated at Tokyo Dental College Chiba Hospital, Chiba, Japan as part of a multicenter study [16]. The original study was conducted as a prospective non comparative 6-month study, performed at five centers; four private practices specialized in periodontics in Tokyo, Japan, and one dental school clinic. The participants were recruited from patients with chronic periodontitis [17] from April 2013 to February 2014. This study was performed in accordance with the Helsinki Declaration, and the protocol was approved by the ethics committee of Tokyo Dental College (No.431). Written informed consent was obtained from all participants.
Inclusion and exclusion criteria
Inclusion criteria consisted of having at least one 2- or 3-wall intrabony defect ≥3 mm in depth in interproximal area of teeth, interproximal sites with probing depth (PD) ≥6 mm, keratinized gingiva ≥2 mm, and good level of oral hygiene [mean plaque index (PlI) ≤1] [18]. Participants must have completed initial periodontal therapy consisting of plaque control and consecutive sessions of quadrant scaling and root planing within 3 months.
Systemic exclusion criteria were the presence of uncontrolled systemic diseases, smokers, allergy to collagen, concurrent or previous bisphosphonate, high dose corticosteroid or other drug therapy, current pregnancy or lactation and general contraindications for dental and/or surgical treatment. Those under 20 years old or with furcation involvements at target teeth are also excluded.
Clinical examination
The following parameters were recorded by trained, calibrated examiners at baseline: after recording of gingival index (GI) [19] and PlI, PD and gingival recession (GR) were recorded in 0.5 mm increments using a pressure-sensitive periodontal probe (Gram Probe #2, YDM, Higashi Matsuyama, Japan). CAL was calculated as the sum of PD and GR. Bleeding on probing (BOP) was recorded as the presence or absence of bleeding following measurement of PD. Tooth mobility (TM) [20] was also recorded. Reevaluations were performed at 6 months, 1 and 2.5 years after surgery.
Radiographic assessment
Semi-standardized radiographs were taken with the long cone paralleling technique using film holders (CID-3, Hanshin Technical Laboratory, Nishinomiya, Japan) with customized occlusal stents.
Surgical procedures
The surgical intervention was implemented as described previously [16]. Briefly, following local infiltration anaesthesia, defects were accessed using the modified papilla preservation technique [21] or the simplified papilla preservation flap [22]. After removal of granulation tissue, scaling and root planning was performed. No root surface conditioning was used. Then the defects were filled with DBBM (Geistlich Bio-Oss®, 0.25–1 mm, Geistlich Pharma AG, Wolhusen, Switzerland), which had been pre-soaked in sterile saline. A porcine-derived non-cross-linked CB membrane (Geistlich Bio-Gide®, Geistlich Pharma AG) was then placed to cover the bone graft material and defect margin. No sutures were used to stabilize the CB. The flaps were then replaced to obtain full closure and sutured by modified vertical mattress and interrupted sutures using e-PTFE sutures (Gore-Tex® Suture CV-6, W.L. Gore and Associates, Flagstaff, AZ, USA). No periodontal dressing was used.
Intrasurgical measurements
The following parameters were assessed after debridement of the area: (1) distance from the cemento-enamel junction (CEJ) to the bottom of the defect (CEJ-BD); (2) distance from the CEJ to the most coronal extension of the interdental bone crest (CEJ-BC). These measurements were performed at the deepest interdental point of the defect and recorded in 0.5 mm increments. The intrabony component of the defect (INTRA) was calculated as INTRA = (CEJ-BD) − (CEJ-BC).
Postsurgical care
The patients received antimicrobial agents (typically cefdinir 300 mg/d, for 4 days). Standard analgesic was given as needed. Patients were instructed to rinse twice daily with an antimicrobial mouth rinse (Listerine® Fresh Mint, Johnson & Johnson, Tokyo, Japan) and to use the following oral hygiene procedures in the treated area for the first 4 postoperative weeks. The patients were asked to start gentle wiping of the operated dento-gingival area with an ultra-soft toothbrush from the third postoperative day. No interdental cleaning in the treated area was allowed during the first 4 weeks.
The sutures were removed after 14 days. Professional supragingival tooth cleaning was performed at weeks 1, 2 and 4. Thereafter, all patients were placed on the maintenance programs.
Maintenance care
Following completion of the original 6-month study, the patients were assigned to maintenance or supportive periodontal therapy based on individual needs. They were asked to come in at 3-month intervals as appropriate. At these appointments, the patients’ oral hygiene status and periodontal conditions were evaluated and the oral hygiene procedures were reinforced as necessary. Scaling and professional tooth cleaning were performed as needed.
Statistical analysis
At each visit, data were recorded in a case report form. After proofed for entry errors, the data were compiled by creating a computerized file. The primary outcome variable was the change in CAL. In the calculations, measurements at the same deepest point of the selected defect were included. CAL gain and PD reduction were also summarized as percentage changes from baseline values.
Repeated measures analysis of variance with Tukey–Kramer multiple comparisons test or Friedman test with Dunn’s multiple comparisons test was used to analyze changes in quantitative data over time. Comparisons for BOP data were made by Fisher’s exact test. Correlation between variables was analyzed by Spearman rank correlation. A software package (InStat version 3.10 for Windows, GraphPad Software, La Jolla, CA, USA) was used. A p value of less than 0.05 was considered statistically significant.
Results
Study participants and baseline clinical parameters
Out of 19 Japanese patients at Tokyo Dental College who have completed the original 6-month study [16], 10 patients (mean age 55.5 years old, 5 women and 5 men) were available for the follow-up 2.5 years post-treatment. The reasons for drop-outs were patient no-shows and appointment cancellations for transferring to a different dental clinic or for unknown reasons. Demographic information and clinical parameters at baseline are presented in Table 1.
Each participant contributed one defect site. Treated teeth comprised 3 (30% of treated sites) incisors (2 maxillary, 1 mandibular), 1 (10%) canine (maxillary), 3 (30%) premolars (2 maxillary, 1 mandibular) and 3 (30%) molars (3 mandibular). The mean width of keratinized tissue was 4.9 mm. The mean value for INTRA was 4.6 mm.
Change in clinical parameters
All participants had received systemic antimicrobial agents, analgesics and mouth rinse as instructed. The postoperative healing was generally uneventful. Throughout the study, none of the participants underwent any adverse event.
At 6 months after surgery, a significant improvement in CAL from baseline was observed (p < 0.001) (Fig. 1a). A significant improvement from baseline was also observed at 1 year (p < 0.01) and at 2.5 years (p < 0.05). The CAL values at 1 and 2.5 years were significantly greater than that at 6 months (p < 0.01). The mean gains in CAL (primary outcome variable) at 6 months and 2.5 years were 2.8 ± 1.0 mm (range: 1.0 mm to 4.0 mm) and 1.4 ± 1.5 mm (range: −1 mm to 4.0 mm), respectively. Percentages of CAL gains at 6 months and 2.5 years were 35.5 and 17.0%, respectively.
Change in CAL. a Mean CAL values at each evaluation period. Data shown as mean ± SD (n = 10). *P < 0.05, **P < 0.01, ***P < 0.001, compared to baseline, †† P < 0.01, compared to 6 months, by ANOVA with Tukey–Kramer multiple comparisons test. b Distribution of individual CAL change from baseline at 2.5 years. Dotted line indicates the mean value. CAL clinical attachment level
Distribution of CAL change values at 2.5 years is shown in Fig. 1b. Seven participants showed CAL gains and three showed CAL losses or no change.
As for the secondary outcome variables, a significant improvement in PD was noted at 6 months, 1 and 2.5 years (Fig. 2a). No significant differences in PD values were observed between 6 months, 1 and 2.5 years. The mean reductions in PD at 6 months and 2.5 years were 4.0 ± 0.8 and 3.2 ± 0.8, respectively. Percentages of PD reductions at 6 months and 2.5 years were 53.0 and 42.3%, respectively. There was a gradual increase in GR from baseline to 1 year after surgery (Fig. 2b). A significant difference from baseline in GR values was observed at 1 and 2.5 years (p < 0.01). However, no significant difference between 1 and 2.5 years was noted. Compared to 6 months, contribution of GR to the reduction in PD was greater at 2.5 years (Fig. 3).
As expected, baseline values for PlI, GI, and TM were relatively low, because the participants have already received initial periodontal therapy. A further, significant reduction in GI from baseline was found at 1 and 2.5 years (Table 2). No significant differences in PlI and TM were found during the observation periods. As for BOP, a significant difference from baseline was noted at 2.5 years (Table 3).
Relationship between baseline variables and CAL gain or PD reduction at 2.5 years
No significant correlation was found between CAL gain at 2.5 years and baseline variables (Table 4). PD reduction at 2.5 years was significantly positively correlated with baseline PD and INTRA, indicating that the deeper the initial PD or INTRA, the greater tends to be PD reduction after surgery.
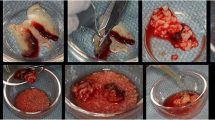
A representative case is shown in Fig. 4.
A representative treatment case. 42-year-old woman. a Before surgery (baseline), in the mesial aspect of the maxillary right canine; PD 6.0 mm, CAL 7.0 mm (top). In the radiograph, vertical bone defect is observed (bottom). b During surgery, careful scaling and root planing was performed after removal of granulation tissue (top). Then the defect was filled with DBBM (middle) and covered with CB (bottom). c Postoperative views at 6 months, d 1 year, e 2.5 years; PD 2.0 mm, CAL 3.0 mm (top). In the radiograph, an improvement in the initial bone defect area can be observed (bottom)
Discussion
In the present study, we evaluated longitudinally the clinical outcome of periodontal regenerative therapy using DBBM in combination with CB in the treatment of intrabony defects in Japanese patients with chronic periodontitis. The combination therapy yielded statistically significant gains in CAL and reductions in PD at 2.5 years, when compared with the preoperative values. However, the trend for decrease in CAL gain over time was noted. These results should be interpreted with caution in terms of their clinical relevance.
A meta-analysis study has indicated that combination regenerative therapies performed better than the single therapies, although the additional benefits were small [23]. In the present study, significant PD reductions from baseline were sustained up to 2.5 years, and no significant difference in PD was observed between 6 months and 2.5 years. As for the CAL gain, the mean value was 1.4 ± 1.5 mm at 2.5 years after the combination therapy. The value was significantly smaller than that obtained at 6 months (2.8 ± 1.0 mm). Moreover, the CAL gain at 2.5 years is smaller than the values in the previous studies of combination regenerative therapies with longer observation periods. In a case-series of 15 patients, Stavropoulos and Karring [24] showed the mean CAL gain of 4.1 ± 1.3 mm at 5Y after the GTR therapy using the DBBM in combination with PLA/PGA bioabsorbable membrane. In their randomized clinical trial [25], the mean CAL gain of 2.3 ± 2.1 mm was noted in 10 patients at 6Y after the same combination therapy. In a randomized controlled study, Sculean et al. [26] demonstrated the CAL gain of 3.7 ± 1.1 mm in 10 patients at 5 years after the same combination therapy as the present study. The mean CAL gain in the present study was also smaller than the values observed in our previous studies of different regenerative therapies. In our 5-year clinical evaluation of GTR using a non-resorbable membrane only [27], the mean CAL gain was 3.6 mm, and another study using the enamel matrix derivative (EMD) showed the value of 3.4 mm at 2 years [28]. Even among studies using the same materials, it is difficult to directly compare clinical results because of the differences in the skill of surgeons, incision and flap designs and baseline CAL or PD values of the participants. For example, the baseline mean PD in the study by Sculean et al. [26] was 9.1 mm whereas the value for our study was 7.5 mm. It has been reported that a greater gain in CAL can be expected after regenerative therapy, in patients with greater initial values in PD and CAL [29, 30], although no significant correlation was found between the CAL gains at 2.5 years and baseline PD or CAL values in the present participants.
In the present study, two participants showed CAL losses at 2.5 years from baseline (−1.0 and −0.5 mm), although they both had CAL gains of ≥3.0 mm at 6 months. Given the small number of participants, these negative values contributed to the relatively modest mean CAL gains observed at 2.5 years. Moreover, at 2.5 years, seven out of 10 participants showed a decrease in CAL gain values from 6 months. It is notable that the mean PD of the participants at 6 months was 3.5 mm, which is somewhat greater than the value (2.7 mm) reported in our previous study using EMD [28]. These data may indicate the need for more meticulous postoperative maintenance care in the present participants. A partial loss of the CAL gain obtained 1 year after GTR has been shown to be associated with smoking, compromised oral hygiene [31], and poor compliance with a supportive periodontal program [32, 33]. All participants were asked to follow 3-month recall, but some (including those with CAL loss) failed to comply with this, resulting in longer maintenance intervals.
It has been shown that newly formed periodontal tissues in intrabony defects can be managed for ≥10 years [34]. It is unclear whether more frequent or meticulous supportive periodontal therapy could have prevented such CAL losses in the two patients. In a previous randomized clinical trial of the combination therapy, it was reported that poor oral hygiene, frequent BOP and infrequent maintenance visits did not seem to play a critical role in the long-term stability of the CAL gain [25]. However, patient compliance and appropriate periodontal maintenance are generally considered to be important for long-term success of periodontal regenerative therapy [5]. We continue to provide careful maintenance care to the participants in the present study.
There are several limitations of this study. First, the sample size was small and the data were from one institution. Second, the study was non-random and uncontrolled. A controlled, longitudinal study with larger sample size is needed to better evaluate the long-term performance of the combination therapy. Since periodontal disease is a multifactorial disease, the use of multivariate analysis would be more appropriate to analyse data from larger sample size. Also, it is not possible to confirm that periodontal regeneration had indeed occurred to the treated site, because no histological analysis can be presented. Lastly, the surgical procedures were performed by seven periodontists with various experience levels. This may have contributed to the differences in clinical outcomes among the participants, as indicated by the high standard deviations.
Despite these limitations, the study findings add significantly to the existing literature on the clinical effectiveness of the combination regenerative therapies. The participants in the present study are currently being followed up to evaluate more longitudinal treatment outcomes.
Conclusions
The periodontal regenerative therapy using DBBM and CB produced significant clinical effects such as gain in CAL and reduction in PD, up to 2.5 years in the treatment of intrabony defects. There was a trend for decrease in CAL gain over time. Further studies are required to determine the true benefit of and appropriate case selection for this combination therapy. Such information may contribute to the optimization of the periodontal regenerative therapy.
Abbreviations
- DBBM:
-
deproteinized bovine bone mineral
- CB:
-
collagen barrier
- CAL:
-
clinical attachment level
- PD:
-
probing depth
- BOP:
-
bleeding on probing
- GI:
-
gingival index
- PlI:
-
plaque index
- TM:
-
tooth mobility
- GR:
-
gingival recession
References
Pihlstrom BL, Michalowicz BS, Johnson NW. Periodontal diseases. Lancet. 2005;366:1809–20.
Hajishengallis G. Periodontitis: from microbial immune subversion to systemic inflammation. Nat Rev Immunol. 2015;15:30–44.
American Academy of Periodontology. Glossary of Periodontal Terms. http://www.perio.org/libraries/glossary. Accessed 31 Jan 2017.
Scantlebury T, Ambruster J. The development of guided regeneration: making the impossible possible and the unpredictable predictable. J Evid Based Dent Pract. 2012;12:101–17.
Reynolds MA, Kao RT, Nares S, Camargo PM, Caton JG, Clem DS, et al. Periodontal regeneration—intrabony defects: practical applications from the AAP regeneration workshop. Clin Adv Periodontics. 2015;5:21–9.
Aichelmann-Reidy ME, Reynolds MA. Predictability of clinical outcomes following regenerative therapy in intrabony defects. J Periodontol. 2008;79:387–93.
Nygaard-Østby P, Bakke V, Nesdal O, Susin C, Wikesjö UME. Periodontal healing following reconstructive surgery: effect of guided tissue regeneration using a bioresorbable barrier device when combined with autogenous bone grafting. A randomized-controlled trial 10-year follow-up. J Clin Periodontol. 2010;37:366–73.
Camargo PM, Levkovic V, Weinlaender M, Nedic M, Vasilic N, Wolinsky LE, et al. A controlled re-entry study on the effectiveness of bovine porous bone mineral used in combination with a collagen membrane of porcine origin in the treatment of intrabony defects in humans. J Clin Periodontol. 2000;27:889–96.
Sculean A, Berakdar M, Chiantella GC, Donos N, Arweiler NB, Brecx M. Healing of intrabony defects following treatment with a bovine-derived xenograft and collagen membrane. A controlled clinical study. J Clin Periodontol. 2003;30:73–80.
Camelo M, Nevins ML, Lynch SE, Schenk RK, Simion M, Nevins M. Periodontal regeneration with an autogenous bone-Bio-Oss composite graft and a Bio-Gide membrane. Int J Periodontics Restorative Dent. 2001;21:109–19.
Nevins ML, Camelo M, Lynch SE, Schenk RK, Nevins M. Evaluation of periodontal regeneration following grafting intrabony defects with bio-oss collagen: a human histologic report. Int J Periodontics Restorative Dent. 2003;23:9–17.
Rösing CK, Aass AM, Mavropoulos A, Gjermo P. Clinical and radiographic effects of enamel matrix derivative in the treatment of intrabony periodontal defects: a 12-month longitudinal placebo-controlled clinical trial in adult periodontitis patients. J Periodontol. 2005;76:129–33.
Heden G, Wennström JL. Five-year follow-up of regenerative periodontal therapy with enamel matrix derivative at sites with angular bone defects. J Periodontol. 2006;77:295–301.
Japanese Society of Periodontology. JSP clinical practice guideline of the regenerative therapy for patients with periodontal disease; 2012. www.perio.jp/publication/upload_file/guideline_regenerative_medicine.pdf).
Ohazama A, Kitamura H, Suzuki M, Yamada S, Hasegawa K. The clinical evaluation of periodontal surgery with porous bone graft material (Bio-Oss®) and collagen membrane (Bio-Gide®). J Jpn Soc Periodontol. 1999;41:153–65. www.jstage.jst.go.jp/article/perio1968/41/2/41_2_153/_article).
Irokawa D, Okubo N, Nikaido M, Shimizu H, Konobu N, Matsui T, et al. Periodontal regenerative therapy of intrabony defects using deproteinized bovine bone mineral in combination with collagen barrier membrane: a multicenter prospective case-series study. Int J Periodontics Restorative Dent. doi:10.11607/prd.2888.
Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol. 1999;4:1–6.
Silness J, Löe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand. 1964;22:121–35.
Löe H. The gingival index, the plaque index and the retention index systems. J Periodontol. 1967;38:610–6.
Miller SC. Textbook of periodontia. Philadelphia: Blakiston; 1950.
Cortellini P, Pini Prato G, Tonetti MS. The modified papilla preservation technique. A new surgical approach for interproximal regenerative procedures. J Periodontol. 1995;66:261–6.
Cortellini P, Pini Prato G, Tonetti MS. The simplified papilla preservation flap. A novel surgical approach for the management of soft tissues in regenerative procedures. Int J Periodontics Restorative Dent. 1999;19:589–99.
Tu Y-K, Needleman I, Chambrone L, Lu H-K, Faggion CM. A bayesian network meta-analysis on comparisons of enamel matrix derivatives, guided tissue regeneration and their combination therapies. J Clin Periodontol. 2012;39:303–14.
Stavropoulos A, Karring T. Five-year results of guided tissue regeneration in combination with deproteinized bovine bone (Bio-Oss) in the treatment of intrabony periodontal defects: a case series report. Clin Oral Invest. 2005;12:271–7.
Stavropoulos A, Karring T. Guided tissue regeneration combined with a deproteinized bovine bone mineral (Bio-Oss®) in the treatment of intrabony periodontal defects: 6-year results from a randomized-controlled clinical trial. J Clin Periodontol. 2010;37:200–10.
Sculean A, Schwarz F, Chiantella GC, Donos N, Arweiler NB, Brecx M, et al. Five-year results of a prospective, randomized, controlled study evaluating treatment of intra-bony defects with a natural bone mineral and GTR. J Clin Periodontol. 2007;34:72–7.
Takahashi J, Saito A, Nakagawa T, Oshima M, Yamanouchi K, Yamada S. Long-term clinical evaluation of class II furcation and vertical osseous defects treated by guided tissue regeneration using non-resorbable membranes. J Jpn Soc Periodontol. 1998;40:119–25. https://www.jstage.jst.go.jp/article/perio1968/40/1/40_1_119/_article/-char/ja/.
Fujinami K, Hayakawa H, Ota K, Ida A, Nikaido M, Makiishi T, et al. Two-year follow-up of treatment of intrabony periodontal defect with enamel matrix derivative. Bull Tokyo Dent Coll. 2011;52:215–21.
Cortellini P, Pini Prato G, Tonetti MS. Periodontal regeneration of human intrabony defects. I. Clinical measures. J Periodontol. 1993;64:254–60.
Saito A, Nanbu Y, Nagahata T, Yamada S. Treatment of intrabony periodontal defects with enamel matrix derivative in private practice: a long-term retrospective study. Bull Tokyo Dent Coll. 2008;49:89–96.
Cortellini P, Tonetti MS. Long-term tooth survival following regenerative treatment of intrabony defects. J Periodontol. 2004;75:672–8.
Cortellini P, Pini-Prato G, Tonetti M. Periodontal regeneration of human infrabony defects (V). Effect of oral hygiene on long-term stability. J Clin Periodontol. 1994;21:606–10.
Weigel C, Brägger U, Hämmerle CH, Mombelli A, Lang NP. Maintenance of new attachment 1 and 4 years following guided tissue regeneration (GTR). J Clin Periodontol. 1995;22:661–9.
Kao RT, Nares S, Reynolds MA. Periodontal regeneration—intrabony defects: a systematic review from the AAP regeneration workshop. J Periodontol. 2015;86(Suppl. 2):S77–104.
Authors’ contributions
DI and AS contributed to planning the study protocol, the analysis, interpretation of the data and drafting of the manuscript. TT, KN, HG and ME contributed to the data collection. HS contributed to data analysis. MN, AS and ST contributed to study conception. All authors read and approved the final manuscript.
Acknowledgements
The authors are grateful to the dental hygienists at Tokyo Dental College Chiba Hospital for their patient care.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
All data and further information about “Method” section are available via the corresponding author (atsaito@tdc.ac.jp).
Consent to publish
Written informed consent for publication was obtained from all participants. All authors agreed to final submission.
Ethics approval and consent to participate
This study was performed in accordance with the Helsinki Declaration, and the protocol was approved by the ethics committee of Tokyo Dental College (No.431). Written informed consent for study participation was obtained from all participants.
Funding
Bio-Oss® and Bio-Gide® were provided by Geistlich Pharma AG (Wolhusen, Switzerland). This study was supported in part by a research grant from Geistlich Pharma AG. The funder has no direct involvement with the scientific aspects of the study. The authors alone are responsible for the content and writing of the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Irokawa, D., Takeuchi, T., Noda, K. et al. Clinical outcome of periodontal regenerative therapy using collagen membrane and deproteinized bovine bone mineral: a 2.5-year follow-up study. BMC Res Notes 10, 102 (2017). https://doi.org/10.1186/s13104-017-2426-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13104-017-2426-y