Abstract
Background
Conventional wisdom suggests that out-of-pocket (OOP) expenditure reduces healthcare utilization. However, little is known about the expenditure borne in urban settings with the current development of the private health sector in sub-Saharan Africa. In an effort to update knowledge on medical expenditure, this study investigated the level and determinants of OOP among individuals reporting illness or injury in Ouagadougou, Burkina Faso and who either self-treated or received healthcare in either a private or public facility.
Methods
A cross-sectional study was conducted with a representative sample of 1017 households (5638 individuals) between August and November 2011. Descriptive statistics and multivariate techniques including generalized estimating equations were used to analyze the data.
Results
Among the surveyed sample, 29.6 % (n = 1666) persons reported a sickness or injury. Public providers were the single most important providers of care (36.3 %), whereas private and informal providers (i.e.: self-treatment, traditional healers) accounted for 29.8 and 34.0 %, respectively. Almost universally (96 %), households paid directly for care OOP. The average expenditure per episode of illness was 8404XOF (17.4USD) (median 3750XOF (7.8USD). The total expenditure was higher for those receiving care in private facilities compared to public ones [14,613.3XOF (30.3USD) vs. 8544.1XOF (17.7USD); p < 0.001], and the insured patients’ bill almost tripled uninsured (p < 0.001). Finally, medication was the most expensive component of expenditure in both public and private facilities with a mean of 8022.1XOF (16.7USD) and 12,270.5 (25.5USD), respectively.
Conclusion
OOP was the principal payment mechanism of households. A significant difference in OOP was found between public and private provider users. Considering the importance of private healthcare in Burkina Faso, regulatory oversight is necessary. Furthermore, an extensive protection policy to shield households from catastrophic health expenditure is required.
Similar content being viewed by others
Background
Out-of-pocket (OOP) expenditure on healthcare imposes a significant burden on households facing a health crisis [1–3] and is a worldwide concern [4]. Significant OOP expenditure may lead households to a “financial catastrophe” in the absence of risk and payment pooling mechanisms or insurance.
In sub-Sahara Africa (SSA), generations of health system policy were implemented in the last three decades, prompted by a quest to balance improved health for populations and concern about financial equity in access to healthcare [5]. The Bamako Initiative approach was launched in 1987 to boost the primary care policy in African setting. This policy placed emphasis on cost recovery, community participation in facilities management, and sustainable essential drug-supply policy [6, 7]. Besides, other initiatives were tried such as community-based health insurance, a risk pooling scheme to render more affordable medical costs [8] or the pay-for-performance (or results-based financing) approach that targets both quantity and quality of healthcare delivery [9, 10]. All were implemented in the context of emerging private sector of care delivery. This sector is evidenced to contribute to healthcare delivery and to boost competition leading to quality improvement [11–13].
Similar to other countries in SSA, both private and public sectors coexist in Burkina Faso, shifting therefore from the long-standing free-of-charge policy in healthcare delivery to the user charge policy [14]. The rapid development of private sector in low and middle income countries (LMIC) resulted in diversified healthcare sources and options for consumers [15]. Meanwhile, healthcare costs incurred by patients rose [16], particularly for patients treated in the private sector [17]. However, private health sector is not efficiently regulated and monitoring policies are inoperative [18, 19]. The challenges to effective regulation derive from varied constraints: poor enforcement of health regulations, insufficient institutional capacity, lack of competition in the market, weak professional associations, or prevailing dual practice [20].
In Burkina Faso, the private health sector expanded rapidly and reinforced the traditional public health system, especially following the market liberalization (in 1991). With growth estimated at 104 % between 1997 and 2007, and at 28.5 % from 2007 to 2011 [21–23], a rise of the number of medical contacts was observed (0.50: 2008, 0.63: 2010, 0.78: 2013 [24]). As elsewhere, the private health sector in Burkina Faso is inclined towards curative care delivery [25]. This private sector consists of two distinct components with different philosophy: private-for-profit (PFP) and private-not-for-profit (PNFP). The first is defined as benefit-focused, while PNFP providers are philanthropic-oriented medical institutions (Faith-based and non-governmental organizations). Because of a longstanding partnership with government, PNFP providers receive support from the State in the form of trained personnel; and deliver similar services as in government facilities, including immunization and other public health programs associated with positive externalities [25].
As in other LMICs [26], in Burkina Faso, OOP is the principal healthcare payment scheme [26]. Although approximately 12.5 % of the state budget is allotted to health, fewer than 2 % of people are insured [27] and the health system still greatly depends on external funding (36.2 % in 2010 [28]). Despite the context of emergence and development of private sector in urban areas, scanty evidence exists on the level, distribution, and determinants of OOP expenditure in those areas. Yet, most studies have investigated rural settings [29–32], while urban areas have become home to numerous therapeutic systems from varied ownership and this expansion will continue [33]. This study sought to address those gaps in Ouagadougou by investigating: (a) the level of OOP expenditure on healthcare, (b) the distribution of OOP based on its primary components and on the ownership of healthcare facilities, and (c) the proximate determinants of OOP.
Methods
Study design and setting
A cross-sectional survey was conducted in the 30 administrative sectors (ASs) of Ouagadougou, the capital city of Burkina Faso from August to November in 2011. Ouagadougou is home to approximately 2 million inhabitants and has the lowest poverty level in the country (28.3 % versus national average of 46.7 %) [29]. It has an extensive number of both public and private health facilities (10 % of the public health facilities and 60.3 % of the private health facilities of Burkina Faso) [34, 35].
Sample size and sampling procedure
The population for this study came from a doctoral dissertation project entitled “Health-Care-Seeking Patterns in the Emerging Private Sector in Burkina Faso.” Because of the absence of a households list, the simplified general method for cluster-sample surveys in developing countries [36] was implemented. To strengthen the statistical power and maximize the representativeness, the selection of the clusters (streets) used the cardinal point system (South, North, West, and East in random order) applied in each of the 30 ASs. A two-stage clustered sampling was implemented based on the city map to randomly select (without replacement) the streets in the individual AS (primary sampling unit). From each selected street, starting from the first entry point (South of the AS), a skipped interval was applied to map out the households to be surveyed (secondary sampling unit). The number of households per AS was defined according to a probability-proportional-to-size (PPS). The sampling procedure is exhaustively detailed elsewhere [37]. The number of households was obtained from the Burkina Faso National Institute of Statistics and Demographics (NISD). Based on studies of its kind [38–42], 1600 households were retained for the main project. For the purposes of this study, only households residing for 6 months (at least), in which at least one member had experienced any morbid event in the 30 days prior to the survey (n = 1025) were considered.
Data collection procedures
Data were collected through an interviewer-based questionnaire. The survey adhered to the Demographic and Health Surveys (DHS) strategy which represents a standard in the field. Oral consent was sought from the household head on behalf of interviewees. In each household, the head and spouse (if any) were met separately for a face-to-face interview. In the case of a discrepancy, the household wife’s information was retained, assuming she is more aware of illnesses occurring in the household. Information on members who felt sick or were injured was recorded according to the “three-stage decision scheme” to portray health status and healthcare used [43]. First, it was asked whether any morbid event happened in the preceding 30 days. If any, then information was collected on the action taken, and finally, the type and name of provider sought, and the expenditure incurred. Six trained data collectors were assigned a fixed number of AS for this field survey. Supervision was insured by the principal investigator (PI) (BI). Each household head received a symbolic participation gift (battery-powered flashing pen) afterwards but did not have any prior knowledge of the gift to avoid undue influence.
Data collection instrument and quality control
A structured questionnaire inspired by those developed and used in Burkina Faso’s DHS was employed. The questionnaire was content-validated, forward into French and backward translated, and finally pilot-tested with 32 households. The questionnaire included three sections. The first section covered sociodemographic variables: gender, age, occupation, education, filiation, marital status, and insurance coverage. The second covered information about the therapeutic action and type of provider consulted. The last module included the itemized financial cost of treatment.
As certain respondents used nicknames to designate facilities, further details were sought to match the designated provider with the Ministry of Health Department of the Private Sector master list. Onsite verifications were performed to obtain complementary information on facilities not officially listed (unlicensed or recently registered). For quality control, the PI re-interviewed 2 % of households with a short version of the questionnaire and scrutinized each questionnaire before data were entered into the Census and Survey Processing package (CSPro), version 4.0.
Definition of variables
The dependent variable was expenditure recorded in West African CFA francs (XOF) (US$1 = 481.5XOF [44]). Explanatory variables consisted of gender, health insurance, the relationship with the household head, and age. Three other variables were specific to adults: education, marital status, and occupation. Regarding providers, the formal provider is the one providing western-based care. This included public facilities [primary healthcare centre (PHC), district hospital (DH), and teaching hospital (TH)] and formal private facilities (PFP and PNFP). Informal sources included self-treatment, traditional healers, and marabouts.
Data analysis
Only expenditure related to acute health experience was analysed to better portray the unplanned characteristic of the financial burden. Therefore, chronic diseases, planned surgeries, and hospitalized cases were excluded. The market price of medicine was considered for any home treatment. Descriptive analysis was conducted and analysis of variance (ANOVA) or t test (as appropriate) fitted to assess how significant the difference in mean expenditure was. The median expenditure is also presented for its robustness. Because of positively skewed expenditure data, the log of expenditure was computed to better approximate a normal distribution for inference. A p value of less than 0.05 was considered significant.
Generalized estimating equations (GEE) was implemented to account for the household level clustered pattern of the data. More than one person in a household could incur expenditure and health-seeking decision within household is probably correlated. This approach is recommended for correlated data [45]. On the other hand, behaviour and expenditures in different households are probably independent. All the statistical analyses were performed using STATA, version 12.1 (Stata Corp., College Station, TX, USA) and SPSS, version 21 (SPSS inc., IL: Chicago, USA).
Ethical considerations
Ethical clearance was granted from the Burkina Faso National Research Ethics Committee upon an examination and an oral presentation of the proposal (#2011-11-82). Additional permission was obtained from the Ouagadougou city council. Prior to each interview, respondents were clearly informed of the voluntary nature of their participation and could decline their consent at any time. Data collected was anonymized at all levels of the study.
Results
Characteristics of the study population
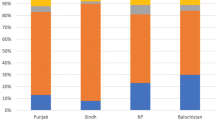
The survey covered 1025 households of which 8 were discarded for incomplete information. The final sample included 5633 persons, of whom 1666 (29.6 %) reported a morbid event. These 1666 persons constituted the analytical sample of interest (Fig. 1). Among them, 940 (56.5 %) were women, and 1126 (67.6 %) were aged 15 years or older. More than half of sample (n = 918, 55.1 %) were sons-daughters or grandsons-daughters. Among the sick adults (≥15 years), 808 (72.1 %) completed at least primary education and only 158 (14.1 %) held a formal job. Sixty-five (3.9 %) of the participants had a health insurance plan. Table 1 indicates that among the persons who reported a sickness, 1100 persons (66.0 %) had sought care from a formal health provider (public or private). In terms of morbidity patterns, malaria diagnosed at a health facility and presumptive malaria was the cause for illness for 1087 (65.3 %) persons. The other 579 (34.7 %) respondents who were sick reported a wide range of pathologies, including injuries and other infectious medical conditions (data not shown). Finally, the logistic regression test of the likelihood of reporting sickness showed that households with fewer sick members report more morbid events: 1–2 persons (OR: 2.43, 95 % CI: 1.88; 3.14), 2–3 persons (OR: 1.29, 95 % CI: 1.12; 1.48) (data not shown).
Health care expenditure by main characteristics and type of providers sought
To adhere to unplanned characteristic of the financial burden, 24 participants were excluded because they either consulted for a chronic disease, or were hospitalized, or had a planned surgery. Table 2 details health expenditure by main characteristics and type of providers. The mean total expenditure was 8404XOF (17.4USD) but age and insurance coverage significantly affect expenditures. Sick adults (≥15 year) spent 40 % more than children [9301.4XOF (19.3USD) vs. 6602.3XOF (13.7USD); p < 0.0001]. Insured persons spent almost three times as high as that of uninsured persons [22,537.4XOF (46.8USD) vs. 7824.1XOF (16.2USD); p < 0.001], but gender did not significantly affect spending (p = 0.156).
Table 3 details the mean total expenditure by type of provider. Of the 1573 persons who reported their expenditures, those treated at TH incurred the highest mean expenditure [mean: 29,270.8XOF (60.8USD), median: 19,900XOF (41.3USD)], followed by those treated in doctor-led PFP facilities [mean: 26,937.2XOF (55.9USD), median: 18,800XOF (39.0USD)]. Persons treated at doctor-led PNFP incurred expenditure that are about half those of persons treated in doctor-led PFP [mean: 13,044.5XOF (27.1USD), median: 6200XOF (12.9USD)]. Furthermore, persons who received care at PNFP led by a nurse had the lowest expenditure among those who received care in the formal system [mean: 5952.1XOF (12.3USD), median: 4100XOF (8.5USD)]. Participants who commenced the treatment at home (649 out of 785) reported an additional mean cost of 1910.4XOF (3.9USD) [median: 700XOF (1.5USD)], and most of them, (587 persons, 90.4 %) reported a malaria case. Overall, those who received care from other sources (i.e., priest, home visits) had 14 % lower expenditure than the sample mean [mean: 7188.8XOF (14.9USD), median: 6000XOF (12.5USD)] and self-medication appeared to be the least expensive option [mean: 2458.7XOF (5.1USD), median: 1000XOF (2.1USD)].
Itemized health expenditure by facility ownership
Table 4 presents expenditure by item stratified by type of provider. Among the 398 participants who recalled the amount of expenditure by item, the single most expensive expenditure item was drug [mean: 10,256.8 (21.3USD)], median [7500 (15.5 USD)]. Laboratory/imagery appeared to come close second for the amount spent [mean: 8965.1XOF (18.6USD), median: 5333.5XOF (11.1USD)].
A comparison by providers suggests that patients in private facilities paid about 50 % more for their drugs than those in public facilities [mean: 12,270.5 XOF (25.5USD) vs. 8022.1 XOF (16.7 USD), p < 0.001]. Similarly, patients in private facilities paid about 100 % more for consultation fees than those in public facilities [mean: 2328.8 (4.8 USD), median: 1000 (2.1) vs. 844.1 (1.7 USD), 300 (0.6 USD), p < 0.001]. Consultation fees covered a wide range, from 100XOF (0.2USD) (in PHC), to 20,000XOF (41.5USD) (specialists). In both private and public providers, in average, adults spent about 69 % more than children [mean: 16,609.7XOF (34.5USD) vs. 9837.9XOF (20.4USD), p < 0.001; not shown].
Finally, those who visited public or private facilities, spent less for a malaria case treatment than for any other category of illness (means: 5671.7XOF [11.8USD] vs. 14,302.2XOF [29.7USD], p < 0.001).
Proximate determinants of OOP expenditure
The multivariate results (Table 5) indicate that age, gender, and relationship with the household head were not significant predictors of health expenditure. Households with fewer sick members (≤3) tended to spend more (model 1). Insured persons spent 56 % (model 1) and 51 % (model 2) more than uninsured. Furthermore, patients seeking care in private facilities spent 48 % more than those in public facilities (Model 1) (95 % CI = 0.27; 0.69, p < 0.001). When using participants who treated themselves as reference, those who attended public facilities spent 97 % more (95 % CI = 0.67; 1.27, p < 0.001) and those who attended private 141 % more (95 % CI = 1.11; 1.71, p < 0.001) (Model 2). Finally, malaria patients experienced less of a financial burden compared to the rest of medical conditions (p < 0.001).
Discussion
Three crucial results were found. First, residents of Ouagadougou received care from a variety of providers. Second, while the mean OOP expenditure was 8404XOF [17.4USD], persons who visited private providers paid, on average 50 % more than those treated in the public sector. Likewise, insured patients appeared to incur even higher expenditure. Finally, medication was the single most expensive component of the OOP expenditure.
The mean OOP in this study represent 27 % of the minimum legal monthly wage of 30,684XOF [63.7USD]. In addition, a single morbid episode treated by PFP doctor costs 115.40 % of the monthly per capita expenditure of Ouagadougou residents [46]. In other words, PFPs are beyond the reach of modest families in Ouagadougou. Similar results have been found elsewhere. In a single study in Vietnam, Thuan et al. [47] indicated that annual health expenditure amounted to 247.3 Vietnamese Dong (VND) in formal private facilities compared to 59.9 VND in a public reference hospital. In one recent study on malaria care seeking for children under 5 years old in Uganda, Orem and al [48]. observed that, medicine cost (2.3USD) less than consultation (3.3USD) and hospitalization (7.6USD). The private providers were the preferred option, although, the odds of incurring OOP were 13.4 times higher than the odds for a child who went to a public facility. The literature suggests that possible reasons of higher expenditures in private facilities include the fact that certain patients trust private providers more [49], appreciate their interpersonal quality [50], and perceived improved quality of services [51]. Certain authors have suggested that patients tend to patronize private providers for moderate or acute health conditions [50, 51]. In an early research in Ouagadougou, Beogo et al. [37] suggested that the utilization of the PFP health facilities was predicted by enabling factors that include insurance coverage, high education level, and holding a good job. An extensive insurance plan might help reduce families’ exposure to OOP, which might ultimately lead to catastrophic health expenditure and impoverishment.
Surprisingly and interestingly, insured patients paid high financial toll. Two hypotheses were set: (1) the behaviour of practitioners and (2) the type of provider that insured patients favoured might explain this fact. First, in Ouagadougou, insured persons are among the wealthiest and most hold private insurance plans which are 80–100 % refund-based. Indeed, medical bill inflation correlation with insurance is a well-known phenomena [52]. However, little is known on difference in prescription in literature. It could be argued that practitioners behave discriminatorily with insured patients. Since it is assumed that they will be refunded, costly diagnostic tests, treatments, and/or brand medicines are prescribed, even though generic medicines are available. The third party will help pay the higher bill. Such a supplier-side induction behavior could be majored by the demand-side one, aggrandizing therefore the bill. The second argument is based merely on the high burden incurred by PFP. Apart from the user charge that are the highest in the market—also evidenced in this study—insured patients are prompt to patronize PFP [53, 54], known to bill comparatively higher [17]. The present study finding on health insurance is relevant and important as the central government develops a national insurance. It provides insight and encourages policy makers to be mindful.
In Burkina Faso, the government owns an extensive network of PHCs—the first line of health facilities—which are the pillar of primary care delivery. They are easily accessible geographically, state-subsidized, and offer an integrated service that includes preventive care (vaccination, infant check-up, etc.), basic curative care, and generic drug dispensation at a nominal price. In addition, primary healthcare facilities are mainly staffed by nurses or midwives whose salaries are lower than those of doctors. The cost to the State to operate public facilities is therefore lower than that of the private sector, translating into lower expenditure for patients.
The study ranked healthcare providers according to the expenditure incurred by patients receiving care therein. PFP facilities are the most expensive, followed by PNFP, and public providers, excluding tertiary hospitals. The PNFP and public providers are probably more affordable for patients because of their organizational structure: patients are treated by nurses (1st line) who manage common conditions and refer only complex cases to doctors (2nd line) or specialist (3rd line). On the contrary, in the private sector, in doctor-led PFP especially, doctor sees all patients and the cost structure leans toward price maximization.
The propensity to self-treat raises the issue of financial access, perceived severity of the disease, or resilience to malaria. Geographical access is unlikely be an obstacle in Ouagadougou, where the mean radius to any facility is the lowest in the country (1.7 vs. 6.4 km). Such a high proportion might be strongly associated with seasonality [55].
In the current study, medication was the single most expensive element of the household healthcare bill. Similar results have been found in Burkina and elsewhere. The NISD [46] reported that medications accounted for 75.6 % of the health expenditure by households in 2003. In Chad, medication took up 64.5 % of the total patient bill for medical visits in the capital city [56]. That item accounted for 58–70 % of the total treatment costs per person in urban Nigeria [57]. Nguyen [17] clearly outlined the weight of medications in private medical bills in one Vietnamese study: patients in the private sector were likely to be prescribed 4.1 drug items on average, or 3.8 drug items in a tertiary institution, with more injections. In Tajikistan, Tediosi et al. [58] observed that 76.7 % of visits lead to a medicine prescription. In one ecological study in low income countries, medicine was the largest component of OOP expenditure for outpatient services in both public and private facilities (57 and 45 %; [59]).
Two points have emerged from the sociodemographic determinants of expenditure from the present study. First is the parallel upward trend between age and the amount paid for care received. This pattern concurs with the results of Steinhardt et al. [60], except that in the present study, the correlation is irrespective of the provider type. Besides, it appeared that the fewer the number of persons in a household, the greater the likelihood of reporting a disease. This result might be explained either by the recall bias or selection bias, because substantial differences exist in reported illness or injury and the actual illness experienced [61], due to family wealth [62], even for child healthcare [63]. The recall period of 30 days was used as suggested by Heijink et al. [64]. But 30 days might be too long since a sizeable proportion of interviewees is illiterate (41.6 %), and might not be able to record their expenditure. This might explain why a number of persons could not recall item costs in the total bill. Secondly, expenditure was not relates to quality, severity of illness, and other services variables. Finally, the study targeted direct costs and did not address indirect cost such as loss of income. In particular, information on queuing and waiting time was not collected. That could be longer in public facilities, meaning that while direct costs were lower for care received there, the indirect cost (time lost not only for the sick person but also for the caregiver if any) might be higher.
Conclusion
The present study provides a snapshot of medical expenditure and its determinants in a SSA urban setting with a diverse provision of care. The present study emphasizes the high level of OOP expenditure for patients since Burkina Faso applies a cost recovery policy and the country does not have an extensive insurance plan. A significant difference on expenditure was observed by ownership of the facilities with care at private providers causing the highest expenditures. Furthermore, medication represented the largest share of the medical expenditure across providers. Finally, this paper highlights the importance of the private sector as a key player in the health system. Further, findings from this paper could inform policy in the ongoing national healthcare insurance debate in Burkina Faso and elsewhere. The national insurance plan in Burkina Faso is currently at the design stage, and if implemented, may help improve healthcare access by covering expenditure incurred in both public and private facilities and by protecting financially vulnerable households.
Abbreviations
- AS:
-
administrative sector
- DH:
-
district hospital
- GEE:
-
generalized estimating equations
- LMIC:
-
low and middle income countries
- OOP:
-
out-of-pocket
- PHC:
-
primary healthcare center
- PFP:
-
private for profit
- PNFP:
-
private not-for-profit
- SSA:
-
sub-Sahara Africa
- USD:
-
US dollar
- TH:
-
teaching hospital
- XOF:
-
Franc CFA (West Africa)
- ISO:
-
currency code
References
Essue BM, Kimman M, Svenstrup N, Lindevig Kjoege K, Lea Laba T, Hackett ML, Jan S. The effectiveness of interventions to reduce the household economic burden of illness and injury: a systematic review. Bull World Health Organ. 2015;93(2):102.
Atella V, Brugiavini A, Pace N. The health care system reform in China: effects on out-of-pocket expenses and saving. China Econ Rev. 2015;34:182–95.
Wang Q, Brenner S, Leppert G, Banda TH, Kalmus O, De Allegri M. Health seeking behaviour and the related household out-of-pocket expenditure for chronic non-communicable diseases in rural Malawi. Health Policy Plan. 2015;30(2):242–52.
Barros AJ, Bertoldi AD. Out-of-pocket health expenditure in a population covered by the Family Health Program in Brazil. Int J Epidemiol. 2008;37(4):758–65.
Ridde V, Robert E, Meessen B. A literature review of the disruptive effects of user fee exemption policies on health systems. BMC Public health. 2012;12(289):2–7.
Paganini A. The Bamako Initiative was not about money. Health Policy Dev J. 2004;2(1):11–3.
Lagarde M, Palmer N. The impact of user fees on health service utilization in low- and middle-income countries: how strong is the evidence? Bull World Health Organ. 2008;86(11):839–48.
Dong H, De Allegri M, Gnawali D, Souares A, Sauerborn R. Drop-out analysis of community-based health insurance membership at Nouna, Burkina Faso. Health Policy. 2009;92(2–3):174–9.
Witter S, Fretheim A, Kessy F, Lindahl A. Paying for performance to improve the delivery of health interventions in low- and middle-income countries (review). Cochrane Database Syst Rev. 2012;2:1–82.
Meessen B, Soucat A, Sekabaraga C. Performance-based financing: just a donor fad or a catalyst towards comprehensive health-care reform? Bull World Health Organ. 2011;89(2):153–6.
Duc HA, Sabin LL, Cuong LQ, Thien DD, Feeley R III. Potential collaboration with the private sector for the provision of ambulatory care in the Mekong region, Vietnam. Glob Health Action. 2012;5:1–11.
Pan J, Qin X, Li Q, Messina JP, Delamater PL. Does hospital competition improve health care delivery in China? China Econ Rev. 2015;33:179–99.
Katyal A, Singh PV, Bergkvist S, Samarth A, Rao M. Private sector participation in delivering tertiary health care: a dichotomy of access and affordability across two Indian states. Health Policy Plan. 2015;30(Suppl 1):i23–31.
Dilip TR. Utilization of inpatient care from private hospitals: trends emerging from Kerala, India. Health Policy Plan. 2010;25(5):437–46.
Berendes S, Heywood P, Oliver S, Garner P. Quality of private and public ambulatory health care in low and middle income countries: systematic review of comparative studies. PLoS Med. 2011;8(4):1–10.
Shah NM, Wang W, Bishai DM. Comparing private sector family planning services to government and NGO services in Ethiopia and Pakistan: how do social franchises compare across quality, equity and cost? Health Policy Plan. 2011;26(Suppl 1):i63–71.
Nguyen H. The principal-agent problems in health care: evidence from prescribing patterns of private providers in Vietnam. Health Policy Plan. 2011;26(Suppl 1):i53–62.
Naqvi SA, Naseer M, Kazi A, Pethani A, Naeem I, Zainab S, et al. Implementing a public-private mix model for tuberculosis treatment in urban Pakistan: lessons and experiences. Int J Tuberc Lung Dis. 2012;16(6):817–21.
Mahendradhata Y. The case for stronger regulation of private practitioners to control tuberculosis in low- and middle-income countries. BMC Res Notes. 2015;8:600.
Akhtar A. Health care regulation in low-and middle-income countries: a review of the literature. Melbourne; 2011.
MS Burkina Faso. Annuaire Statistique 2012. In: Direction générale de l’information et des statistiques sanitaires, editor. Ouagadougou; 2013.
MS Burkina Faso. La santé d’après les enquêtes statistiques nationales: Une synthèse des résultats disponibles depuis l’indépendance du Burkina Faso. In: Direction générale de l’information et des statistiques sanitaires, editor. Ouagadougou; 2010e.
MS Burkina Faso. Annuaire statistique 2011. In: Direction générale de l’information et des statistiques sanitaires, editor. Ouagdougou; 2012.
MS Burkina Faso. Bulletin d’épidémiologie et d’information sanitaire. In: Direction générale des études et des statistiques sectorielles, editor, vol. 19ème. Ouagadougou; 2014.
Howard DH, Roy K. Private care and public health: do vaccination and prenatal care rates differ between users of private versus public sector care in India? Health Serv Res. 2004;39(6):2013–26.
World bank. Out-of-pocket health expenditure. In: World bank; 2015. Accessed 06 Nov 2015. http://data.worldbank.org/indicator/SH.XPD.OOPC.ZS.
MS Burkina Faso. Comptes Nationaux de la Santé et Sous comptes Paludisme, Tuberculose et VIH/Sida. In: Direction générale de l’information et des statistiques sanitaires, editor. Ouagadougou: Ministère de la santé; 2011.
MS Burkina Faso. Comptes Nationaux de la Santé: comptes globaux et Sous comptes Paludisme, Tuberculose et VIH/Sida. In: Direction générale de l’information et des statistiques sanitaires, editor. Ouagadougou: Ministère de la santé; 2013.
Rutebemberwa E, Pariyo G, Peterson S, Tomson G, Kallander K. Utilization of public or private health care providers by febrile children after user fee removal in Uganda. Malar J. 2009;8(45):1–9.
Konde-Lule J, Gitta SN, Lindfors A, Okuonzi S, Onama VO, Forsberg BC. Private and public health care in rural areas of Uganda. BMC Int Health Hum Rights. 2010;10:29.
Meremikwu M, Okomo U, Nwachukwu C, Oyo-Ita A, Eke-Njoku J, Okebe J, et al. Antimalarial drug prescribing practice in private and public health facilities in South-east Nigeria: a descriptive study. Malar J. 2007;6:55.
Nuwaha F. Determinants of choosing public or private health care among patients with sexually transmitted infections in Uganda. Sex Transm Dis. 2006;33(7):422–7.
Matthews Z, Channon A, Neal S, Osrin D, Madise N, Stones W. Examining the ‘‘urban advantage’’ in maternal health. PLoS Med. 2010;7(9):1–7.
MS Burkina Faso. Repertoire 2010 des établissements privés de soins du Burkina. In: Direction générale de l’information et des statistiques sanitaires, editor. Ouagadougou; 2011. p. 162.
MS Burkina Faso. Document d’analyse de la cartographie de l’offre des soins de la région du Centre. Document d’analyse. In: Direction générale de l’information et des statistiques sanitaires, editor. Ouagadougou: Ministère de la santé; 2010.
Benett S, Woods T, Liyanage WM, Smith DL. A simplified general method for cluster-sample surveys of health in developing countries. World Health Stat Q. 1991;44(3):98–106.
Beogo I, Liu CY, Chou YJ, Chen CY, Huang N. Health-care-seeking patterns in the emerging private sector in Burkina Faso: a population-based study of urban adult residents in Ouagadougou. PLoS One. 2014;9(5):e97521.
Habtoma GK, Ruys P. The choice of a health care provider in Eritrea. Health Policy. 2007;80(1):202–17.
Janjua NZ, Khan MI, Usman HR, Azam I, Khalil M, Ahmad K. Pattern of health care utilization and determinants of care-seeking from GPs in 2 districts of Pakistan. SouthEast Asia J Trop Med Public Health. 2006;37(6):1242–53.
Amaghionyeodiwe LA. Determinants of the choice of health care provider in Nigeria. Health Care Manag Sci. 2007;11(3):215–27.
Tipke M, Louis VR, Ye M, De Allegri M, Beiersmann C, Sie A, et al. Access to malaria treatment in young children of rural Burkina Faso. Malar J. 2009;8:266.
Su TT, Kouyaté B, Flessa S. Catastrophic household expenditure for health care in a low income society: a study from Nouna District, Burkina Faso. Bull World Health Organ. 2006;84(1):21–7.
Ha NTH, Berman P, Larsen U. Household utilization and expenditure on private and public health services in Vietnam. Health Policy Plan. 2002;17(1):61–70.
Banque Centrale des Etats de l’Afrique de l’Ouest. Cours des devises contre Franc CFA à appliquer aux transferts. In. Dakar: BCEAO; 2011. Accessed 02 Feb 2013. http://www.bceao.int/-Cours-des-devises-contre-Franc-CFA-.html.
Hanley JA, Negassa A, Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003;157(4):364–75.
INSD Burkina Faso. Annuaire statistique 2012. In: Institut National de la Statistique et de la Démographie, editor. Ouagadougou: Ministère de l’economie et des finances; 2013.
Thuan NT, Lofgren C, Lindholm L, Chuc NT. Choice of healthcare provider following reform in Vietnam. BMC Health Serv Res. 2008;8:162.
Nabyonga Orem J, Mugisha F, Okui AP, Musango L, Kirigia JM. Health care seeking patterns and determinants of out-of-pocket expenditure for malaria for the children under-five in Uganda. Malar J. 2013;12:175.
Ozawa S, Walker DG. Comparison of trust in public vs private health care providers in rural Cambodia. Health Policy Plan. 2011;26(Suppl 1):i20–9.
Russell S. Treatment-seeking behaviour in urban Sri Lanka: trusting the state, trusting private providers. Soc Sci Med. 2005;61:1396–407.
Ergler CR, Sakdapolrak P, Bohle HG, Kearns RA. Entitlements to health care: why is there a preference for private facilities among poorer residents of Chennai, India? Soc Sci Med. 2011;72(3):327–37.
Smith S, Newhouse JP, Freeland MS. Income, insurance, and technology: why does health spending outpace economic growth? Health Aff. 2009;28(5):1276–84.
Bryant J, Prohmmo A. Payment mechanisms and prescriptions in four Thai hospitals. Health Policy. 2005;73(2):160–71.
Perlman F, Balabanova D, McKee M. An analysis of trends and determinants of health insurance and healthcare utilisation in the Russian population between 2000 and 2004: the ‘inverse care law’ in action. BMC Health Serv Res. 2009;9:68.
Chuma JM, Thiede M, Molyneux CS. Rethinking the economic costs of malaria at the household level: evidence from applying a new analytical framework in rural Kenya. Malar J. 2006;5:76.
Gauthier B, Wane W. Bypassing health providers: the quest for better price and quality of health care in Chad. Soc Sci Med. 2011;73(4):540–9.
Ewelukwa O, Onoka C, Onwujekwe O. Viewing health expenditures, payment and coping mechanisms with an equity lens in Nigeria. BMC Health Serv Res. 2013;13:87.
Tediosi F, Aye R, Ibodova S, Thompson R, Wyss K. Access to medicines and out of pocket payments for primary care: evidence from family medicine users in rural Tajikistan. BMC Health Serv Res. 2008;8:109.
Saksena P, Xu K, Elovainio R, Perrot J. Health services utilization and out-of-pocket expenditure at public and private facilities in low-income countries. In: World Health Report, vol. 20. Geneva: World Health Organization; 2010. p. 20.
Steinhardt LC, Waters H, Rao KD, Naeem AJ, Hansen P, Peters DH. The effect of wealth status on care seeking and health expenditures in Afghanistan. Health Policy Plan. 2008;24(1):1–17.
Pokhrel S. Determinants of parental reports of children’s illnesses: empirical evidence from Nepal. Soc Sci Med. 2007;65(6):1106–17.
Rous JJ, Hotchkiss DR. Estimation of the determinants of household health care expenditures in Nepal with controls for endogenous illness and provider choice. Health Econ. 2003;12(6):431–51.
Filmer D. Fever and its treatment among the more and less poor in sub-Saharan Africa. Health Policy Plan. 2005;20(6):337–46.
Heijink R, Xu K, Saksena P, Evans D. Validity and comparability of out-of-pocket health expenditure from household surveys—a review of the literature and current survey instruments In: discussion paper, vol. 1. Geneva: World Health Organization 2011; p. 28.
Authors’ contributions
IB designed, collected data and drafted the manuscript. NH oversaw the entire process step by step and reviewed the final draft. MPG reviewed the last draft and re-edited the language. DDA rearticulated the literature review, advised on some statistical analyses, and reviewed successive drafts of the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The study is part of a Ph.D. project at International Health Program, National Yang Ming University. We thank National Yang Ming University, Taiwan International Development and Cooperation Fund and African Doctoral Dissertation Research Fellowships through African Population and Health Research Center for their contribution.
Authors’ thanks go to Mamadou Drabo at the Ministry of health, Burkina Faso for providing administrative information and to Eric Woba for his endeavor during the field data collection.
Competing interests
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Beogo, I., Huang, N., Gagnon, MP. et al. Out-of-pocket expenditure and its determinants in the context of private healthcare sector expansion in sub-Saharan Africa urban cities: evidence from household survey in Ouagadougou, Burkina Faso. BMC Res Notes 9, 34 (2016). https://doi.org/10.1186/s13104-016-1846-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13104-016-1846-4