Abstract
Background
Hypertension remains a public health challenge worldwide. In the Democratic Republic of Congo, its prevalence has increased in the past three decades. Higher prevalence of poor blood pressure control and an increasing number of reported cases of complications due to hypertension have also been observed. It is well established that non-adherence to antihypertensive medication contributes to poor control of blood pressure. The aim of this study is to measure non-adherence to antihypertensive medication and to identify its predictors.
Methods
A cross-sectional study was conducted at Kinshasa Primary Health-care network facilities from October to November 2013. A total of 395 hypertensive patients were included in the study. A structured interview was used to collect data. Adherence to medication was assessed using the Morisky Medication Scale. Covariates were defined according to the framework of the World Health Organization. Logistic regression was used to identify predictors of non-adherence.
Results
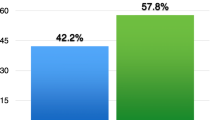
A total of 395 patients participated in this study. The prevalence of non-adherence to antihypertensive medication and blood pressure control was 54.2 % (95 % CI 47.3–61.8) and 15.6 % (95 % CI 12.1–20.0), respectively. Poor knowledge of complications of hypertension (OR = 2.4; 95 % CI 1.4–4.4), unavailability of antihypertensive drugs in the healthcare facilities (OR = 2.8; 95 % CI 1.4–5.5), lack of hypertensive patients education in the healthcare facilities (OR = 1.7; 95 % CI 1.1–2.7), prior experience of medication side effects (OR = 2.2; 95 % CI 1.4–3.3), uncontrolled blood pressure (OR = 2.0; 95 % CI 1.1–3.9), and taking non-prescribed medications (OR = 2.2; 95 % CI 1.2–3.8) were associated with non-adherence to antihypertensive medication.
Conclusion
This study identified predictors of non-adherence to antihypertensive medication. All predictors identified were modifiable. Interventional studies targeting these predictors for improving adherence are needed.
Similar content being viewed by others
Background
Hypertension (HTN) remains a public health challenge worldwide because of its high prevalence and related complications. In 2000, 26.4 % of the World’s adult population had hypertension [1]. In Sub-Saharan Africa (SSA), the prevalence of HTN varied from 6 to 48 % [2]. In the Democratic Republic of Congo (DRC), the prevalence of HTN has been increasing for the past three decades. In 1987, the prevalence was 14.2 % in urban and 9.9 % in rural areas [3] and almost doubled in 2005 to reach 26.7 % [4].
In SSA, the control of HTN is low. For example, in West African countries this control is low, less than 10 % except for Nigeria where it is approximately 30 % [5]. In the DRC, the Vitaraa study conducted in Southern Kivu found that 86.4 % of hypertensive patients were uncontrolled [6]. Uncontrolled HTN is one of the main cardiovascular risk factors (CVRF) [7] and based on the World Health Organization (WHO) estimates, at least 50 % of cardiovascular diseases (CVD) and 75 % of strokes are consequences of high blood pressure [8]. In the DRC, HTN-related complications including stroke, chronic kidney disease (CKD) are increasingly reported [9–11].
Non-adherence to antihypertensive medication (NAM) is one of the main factors contributing to uncontrolled HTN [12]. In fact, benefits of antihypertensive medication to decrease cardiovascular complications have been established. However, inadequate adherence to antihypertensive therapy or NAM has been linked to the development of cardiovascular complications. The NAM is described as a widespread problem in an insidious chronic condition like HTN [13] and studies have shown that populations of African descent with HTN were less adherent to medication compared with Caucasians. The overall prevalence of medication adherence in this population was lower for any definition used [14]. NAM is also associated with cardiovascular mortality risk. A cohort study conducted in Brazil reported that the risk of mortality from CVD was three times higher in patients discontinuing HTN medication compared with those who regularly took their medication [15]. Thus, given the situation described previously for the DRC, we believe that it is essential to identify and gain a better understanding of the factors associated with NAM in our settings with the overreaching goal to inform strategies for improving patient adherence to medication. Therefore, using the WHO framework that describes five dimensions of factors that may affect adherence to therapy and the Morisky Medication Scale, a validated self-reported medication scale, this study aims to measure non-adherence to antihypertensive medication and to identify its predictors.
Methods
Design
From October 2013 to November 2013, a cross-sectional study was carried out at Kinshasa Primary Health-care (KPHC) network facilities. This network consists of 51 facilities that allows for follow-up of patients with NCDs like hypertension and diabetes, living in Kinshasa [16].
Study population
Inclusion criteria
We included in the study hypertensive patients >18 years who have been under antihypertensive drugs for at least a month.
Exclusion criteria
Hypertensive pregnant women were excluded.
Sampling
Only 25, out of 51 facilities, scheduled patients’ visits during the survey were therefore selected. All patients present in the facility and who met the inclusion criteria were enrolled. The sample size was computed using the following formula \(n \ge \frac{{Z_{\alpha }^{2} \cdot p \cdot q}}{{d^{2} }}\) where the p represents the proportion of non-adherence to antihypertensive medication (we assumed that p = 50 % because the proportion of NAM in the DRC is unknown), q (1 − p), z value of the standard normal distribution corresponding to a significance level of alpha of 0.05 (1.96) and d the precision degree that we assumed to 5 % too. The minimal size computed was 384 patients. A total of 408 patients present in the health facilities were selected but only 395 (96.8 %) were eligible and enrolled. The study protocol was approved by the institutional review boards of the Kinshasa School of Public Health, Bureau Diocésain des Oeuvres Médicales de Kinshasa, and Service Médical Armée du Salut and conducted in accordance with the Helsinki Declaration II. All study participants provided written informed consent.
Data collection and study variables
Patients were surveyed using a structured questionnaire, either in French or translated in Lingala, the local language. Five surveyors had been trained over 3 days and the interview instrument was pretested prior to its use. Covariates were defined according to the WHO framework. This framework was used because actually, no model of medication adherence for HTN has been published. The Health Beliefs Model has been used in several studies but it does not include all the dimensions of the NAM factors like those described by the WHO framework [17]. The variables collected entailed social and economic characteristics of patients (gender, age, marital status, religious affiliation, education, employment); conditions-related variables (duration of HTN, control of blood pressure, experience of physical symptoms due to HTN, co-morbidity); therapy-related variables (duration of antihypertensive medication treatment, number of pills taken daily, experience of medication side effects, use of non-prescribed medication, treatment adherence); patients-related variables (knowledge of HTN risk factors and complications, knowledge of treatment benefit, perception of hypertension gravity and hypertension-related complications gravity, beliefs on BP medications importance, status acceptation); healthcare team and system-related variables (patient–provider relationship, patient education, perception of treatment cost, geographical accessibility, availability of antihypertensive drugs).
Co-morbidity has been defined in this study as HTN associated with diabetes mellitus (DM) or organ damage targets (heart disease, strokes, or CKD). Patients were interviewed if identified by a health professional as having one of these conditions.
Only the blood pressure measured by healthcare providers on the day of the survey and recorded in the patient medical file was considered. Three hundred ninety (390) out of three hundred ninety five (395) had the values of blood pressure recorded in their medical file (98.7 %). Uncontrolled HTN was defined, for a patient without co-morbidity, as a patient with a SBP ≥140 mmHg and a DBP ≥90 mmHg. For a patient with co-morbidity, uncontrolled HTN was defined as a patient with SBP ≥130 mmHg and for DBP ≥80 mmHg [18].
The self-reported medication adherence was measured using the Morisky Scale, which is a validated scale with a good internal consistency. Its Cronbach’s alpha has been reported to be of 0.90 in studies of inner-city patients with hypertension [19, 20]. Patients responded, “yes” or “no” to the four questions and have been categorized into three groups, namely high, medium and low adherence, as summarized in Table 1 [19]. Thereafter, adherence was dichotomized in order to facilitate statistical analysis. The low and medium adherence was merged and classified as non-adherent and patients with high adherence were classified as adherent, like previously used by Patel [21].
Statistical analysis
All analyses were performed using Statistical Package for Social Sciences (SPSS) version 21.0. (SPSS, Inc., Chicago, IL, USA). Descriptive statistics were used to summarize the study population characteristics. Continuous variables were reported using mean with standard deviation. Means for age of non-adherent and adherent patients were compared using Student’s t test. Categorical variables were reported as a frequency and percentage and groups were compared using χ2 test. The logistic regression helped to identify independent predictors of non-adherence. All variables associated with non-adherence to antihypertensive medication in the bivariate analysis were included in the final model. Odds ratio (OR) with a corresponding 95 % confidence interval was reported to quantify the strength of association. Significance was set at p-value of less than 0.05.
Results
Patients’ socioeconomic and clinical characteristics
Tables 2 and 3 summarize socio-economic and clinical characteristics of the patients. A total of 395 patients were assessed. The mean age of participants was 63.3 ± 9.6 years and nearly 76 % were female; almost half were married (45.6 %) and Catholic Christians (48.9 %); 40.5 % completed at least secondary school and 63.5 % were unemployed.
Approximately half of the patients suffered from HTN for less than 5 years. The mean systolic blood pressure was 148.6 ± 22.1 and 87.8 ± 14.3 mmHg for the diastolic blood pressure. The control of HTN was present in 15.6 % (95 % CI 12.1–20.0 %) patients. Almost two-thirds of the patients (64.6 %) experienced physical symptoms due to HTN. Dizziness was the most common physical symptom reported. Co-morbidities were present in 53.9 % of participants, of which DM was the most common (52.4 %).
More than half of the participants had less than 5 years of antihypertensive treatment duration. On average, the patients took 1.7 ± 1.2 pills daily. Approximately half of the patients (55.9 %) experienced medication side effects, 20.5 % declared taking non-prescribed medications. Around one in three patients reported to have forgotten to take blood pressure medicine (31.9 %) and to have skipped taking drugs when they felt well (31.4 %). Using the Morisky Scale, we found that over half of participants (54.2 %) were non-adherent to their medication.
Patients’ knowledge, beliefs and perception
Table 4 summarizes the study of the population knowledge, beliefs and perception about HTN and its treatment. Poor knowledge of the risk factors related to lifestyle was observed. Stress/anxiety was the most frequent risk factors mentioned (67.6 %) and stroke was the most common complication mentioned (37.2 %). The control of blood pressure was the most common mentioned benefit of antihypertensive treatment (55.4 %), the majority of patients believed in the importance of blood pressure medication in controlling BP (86.3 %) and accepted their hypertensive status (85.6 %). Also, the majority of the patients in this study thought it possible to adhere to treatment (92.4 %).
Health team and health system variables
Table 5 summarizes the health team and system variables and shows that almost all patients declared that their relationship with care providers was very good or good (94.7 %). More than half of the patients reported that their health facility provided hypertensive patients with education (65.1 %); 86.3 % declared they payed for treatment. Three-quarters of the patients thought that the cost of the treatment was inexpensive (73.3 %). The majority of the patients reported that antihypertensive drugs were available in the healthcare facility when they needed them (87.1 %). The healthcare facilities were for the most part accessible geographically (74.2 %).
Predictors of non-adherence to antihypertensive treatment
Table 6 summarizes the predictors of NAM after logistic regression. Poor knowledge about complications of hypertension (OR = 2.4; 95 % CI 1.4–4.4); unavailability of antihypertensive drugs in the healthcare facilities (OR = 2.8; 95 % CI 1.4–5.5), lack of hypertensive patients education in the healthcare facilities (OR = 1.7; 95 % CI 1.1–2.7), prior experience of medication side effects (OR = 2.2; 95 % CI 1.4–3.3), uncontrolled blood pressure (OR = 2.0; 95 % CI 1.1–3.9) and taking of non-prescribed medications (OR = 2.2; 95 % CI 1.2–3.8) were independently associated with NAM in this study.
Discussion
This study aimed to measure NAM and to identify its predictors. This study found a high prevalence of NAM and a poor control of blood pressure. Patients, therapy and health system factors were the predictors of NAM.
The prevalence of non-adherence to antihypertensive medication was high and consistent with previous findings [14, 22, 23]. However, this prevalence could have been underestimated because of two factors: age of the patients and level of the facilities surveyed. The mean age of patients in this study was 63.3 ± 9.6 years whereas a previous study conducted in the DRC reported a mean age of 54.3 ± 9.2 years among patients admitted to hospital for HTN-related complications [11]. Previous studies reported that, compared with older patients, younger patients were more likely to be non-adherent [24, 25]. Then, we posed a question on the follow-up of the younger hypertensive patients. Probably, younger hypertensive patients in Kinshasa are underdiagnosed. The Vitaraa Study conducted in Southern Kivu province of the DRC reported that more than half of the hypertensive patients were unaware of their status [6]. Given that older patients usually have several health concerns, the probability of HTN being diagnosed incidentally is high. Secondly, this study was carried out in primary healthcare facilities that use essential or generic drugs, which were inexpensive. The cost of drugs is described as a factor of non-adherence; it has been minimized in this study. Also, some non-adherent patients may have developed complications necessitating hospital admission at secondary and tertiary facilities. Overall, we believe that if this study was carried out at secondary and tertiary levels, the proportion of non-adherence would have been higher.
This study also reported a poor control of blood pressure. These findings corroborate previous studies carried out in African populations, where the proportion of blood pressure control was very low, less than 10 % [5]. This poor control may be explained partly by the presence of patients with co-morbidity at primary-level care facilities. Co-morbidity has been defined in this study as HTN associated with diabetes or organ damage targets. Hypertensive patients associated with these diseases are categorized as high cardiovascular risk and this category of patients cannot be followed at the primary-level care facilities [18]. The low proportion of blood pressure control reported in this study could explain the prevalence of HTN-related complications reported at secondary and tertiary levels care in the DRC.
This study reports poor knowledge about risk factors related to HTN. This has also been described by a previous study carried out in Pakistan [26]. Furthermore, stress is the main factor, as corroborated by a study carried out in Zimbabwe where 70.6 % of patients mentioned stress as a cause of hypertension [27]. However, risk factors related to lifestyle such as obesity, tobacco use and excessive alcohol consumption were not often mentioned. In this study, stroke has been the most mentioned as a complication of HTN in contrast with a study conducted in Pakistan, where the heart complication was the most mentioned (30.6 %) [24]. This difference may be explained by the fact that stroke has been described as a major CVD present in the black population [18].
Social and economic factors (education level, sex, age, employment) are described by the WHO as the NAM factors [14]. In this study none of these factors have been associated with NAM. We provided some explanations above on age and employment, the latter has not been associated with NAM, probably because the majority of patients declared that antihypertensive drugs were inexpensive.
Hypertension is considered as a condition without symptom, the experience of physical symptoms due to HTN influences treatment adherence significantly, patients who do not feel unwell may be less adherent. In a qualitative study carried out in Bandundu (a province of the DRC), hypertensive patients reported that they took medication only when they experienced perceived symptoms of HTN [28]. In this study, no association was found between patients experiencing physical symptoms and treatment adherence. This result is consistent with a previous study which did not find this association [29].
Patient education is described as a catalyst for lifestyle change and treatment adherence [27]. This association with treatment adherence has previously been reported [30]. Patient education improves the patient’s understanding of diseases, lifestyle change and medication. In this study, patients who admitted to benefitting from education and who had a good knowledge of hypertension and its complications respectively were twice more likely to be treatment adherent.
Also, this study found that patients who took non-prescribed medication were twice more likely to be non-adherent to treatment than other patients. We surmise that probably these patients use complementary and alternative medicine (CAM) which is defined as a “group of diverse medical and healthcare systems, practices, and products that are not presently considered to be part of conventional medicine” [31]. Previous studies reported an association between the use of CAM and treatment adherence and blood pressure control [32–35]. It is also reported that the experience of side effects is among the main predictors of CAM use. In this study, patients experiencing side effects were more non-adherent than their strong hypothesis of the use of CAM. Unfortunately, the use of CAM was not measured in this study, future studies may be carried out to assess the use of CAM in hypertensive patients in Kinshasa.
Unavailability of antihypertensive medication in healthcare facilities is a barrier to health care and is described as a factor of medication non-adherence. Patients who reported the availability of antihypertensive medication in healthcare facilities were about twice more likely to be adherent. These findings are consistent with that previously reported by Ghozzi in Tunis [36].
We acknowledge some limitations in this study. A potential selection bias may have been introduced in this study relating to the level of care facilities surveyed. Also, information bias was possible—firstly by using the self-reported questionnaire for measuring medication adherence and secondly by reporting the blood pressure measured by non standardized methods. However, these overall findings corroborate those found in previous studies. We think that the results of this study may be generalized to hypertensive patients living in Kinshasa.
Conclusion
This is the first study in the DRC with a large sample to measure the antihypertensive non-adherence and to identify related predictors. These findings show that all predictors identified were modifiable by strengthening the capacity of healthcare providers by communication with patients. Antihypertensive medication should be made available in healthcare facilities.
Abbreviations
- BP:
-
blood pressure
- CAM:
-
complementary and alternative medicine
- CKD:
-
chronic kidney disease
- CVD:
-
cardiovascular diseases
- CVRF:
-
cardiovascular risk factors
- DM:
-
diabetes mellitus
- DRC:
-
Democratic Republic of Congo
- HTN:
-
hypertension
- KPHC:
-
Kinshasa Primary Health-care
- NAM:
-
non-adherence to antihypertensive medication
- NCDs:
-
non communicable diseases
- OR:
-
odds ratio
- SSA:
-
Sub-Saharan Africa
- WHO:
-
World Health Organization
References
Kearney MP, Whelton M, Reynolds K, Muntner P, Whelton KP, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–23.
Dalal S, Beunza JJ, Volmink J, Adebamowo C, Bajunirwe F, Njelekela M, et al. Non- communicable diseases in sub-Saharan Africa: what we know now. Int J Epidemiol. 2011;40:885–901.
M’Buyamba-Kabangu JR, Fagardr ST, Lijnen P, Amery A. Correlates of blood pressure in rural and urban Zaire. J Hypertens. 1987;5:371–5.
Longo MB, Ngoma VD, Nahimana D, Mupepe MD, Mbungu FS, Ekwanzala F, Beya C. Screen detection and the WHO stepwise approach to the prevalence and risk factors of arterial hypertension in Kinshasa. Eur J Cardiovasc Prev Rehabil. 2008;15:503–8.
Lwelunmor J, Airhihenbuwa CO, Cooper R, Tayo B, Plange-Rhule J, Adanu R, Ogedegbe G. Prevalence, determinants and systems-thinking approaches to optimal hypertension control in West Africa. Glob Health. 2014;10:42.
Katchunga BP, Mbuyamba KJR, Masumbuka EB, Lemogoum D, Kashongwe MZ, Degaute JP, et al. Hypertension in adult Congolese population in Southern Kivu: results of the Vitaraa Study. Presse Médicale. 2011;. doi:10.1016/jlpm2010.10.036.
Connor M, Rheeder P, Bryer A, Meredith M, Beukes M, Dubb A, et al. The South African stroke risk in general practice study. S Afr Med J. 2005;95:334–9.
World Health Organization. Reducing risks, promoting healthy life. In the World Health report 2002. Geneva: World Health Organization; 2002.
Sumaili EK, Krzesinski JM, Cohen EP, Nseka NM. Epidemiologie de la maladie rénale chronique en Republique Démocratique du Congo: revue des études transversales de Kinshasa, la capitale. Nephrol Ther. 2010;6(4):232–9.
Sumaili KE, Nseka NM, Makulo JRR, Zinga CV, Longo AL, Mukendi SK et al. Statut socioéconomique et protéinurie: résultats de campagne de dépistage des maladies des reins 2007 à Kinshasa. Ann Afr Med. 2009;2(3):170–7.
M’Buyamba KJR, Biswika RT, Thijs L, Tshimanga GM, Ngalula FM, Disashi T, et al. In-hospital mortality among black patients admitted for hypertension-related disorders in Mbuji Mayi, Congo. Am J Hypertens. 2009;22:643–8.
Matsumura K, Arima H, Tominaga M, Ohtsubo T, Sasaguri T, Fujii K, et al. Impact of antihypertensive medication adherence on blood pressure control in Hypertension: the COMFORT study. Q J Med. 2013;106:909–14.
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–97.
Sabate E. Adherence to long-term therapies: evidence for action. Geneva: World Health Organization; 2003.
Correa Leite ML, Firmo JOA, Loyola Filho AI, Lima-costa MF. Discontinuation of anti-hypertensive drugs increases 11-year cardiovascular mortality risk in community-dwelling elderly (the Bambui Cohort Study of Ageing). BMC Public Health. 2014;14:725.
Kapongo YR, Lulebo MA, Mafuta ME, Mutombo BP, Dimbelolo MJC, Bieleli IE. Assessment of health service delivery capacities, health providers’ knowledge and practices related to type 2 diabetes care in Kinshasa primary health care network facilities, Democratic Republic of Congo. BMC Health Serv Res. 2015;15:9.
Stretcher V, Rosenstock IM. The Health Belief Model. In: Glanz K, Lewis FM, Rimer BK, editors. Health behavior and health education: theory, research and practice. San Francisco: Jossey-Bass; 1997.
Lemogoum D, Seedat YK, Mabadeje AF, Mendis S, Bovet P, Onwubere B, et al. Recommendations for prevention, diagnosis and management of hypertension and cardiovascular risk factors in sub-Saharan Africa. J Hypertens. 2003;21:1993–2000.
Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74.
Shea S, Misera D, Ehrlich MA. Correlates of non adherence to hypertension treatment in an inner-city minority population. Am J Public Health. 1992;82:1607–12.
Patel RP, Taylor SD. Factors affecting medication adherence in hypertensive patient. Ann Pharmacother. 2002;36:40–5.
Lewis LM, Schoenthaler AM, Ogedegbe G. Patients factors, but not provider and health care system factors, predict medication adherence in hypertensive black men. J Clin Hypertens. 2012;14:250–5.
Queiroz Godoy ACD, Velludo EV. Factors that interfere the medication compliance in hypertensive patients. Einstein. 2013;11(3):331–7.
Lee KYG, Wang HXH, Liu QLK, Cheung Y, Morisky ED, Wong CSM. Determinants of medication adherence to antihypertensive medication among a Chinese population using Morisky Adherence Scale. PLoS One. 2013;8(4):2775. doi:10.1371/journal.pone.0062775.
Burnier M. Medication adherence and persistence as the cornerstone of effective antihypertensive therapy. Am J Hypertens. 2006;19:1190–6.
Almas A, Siraj GS, Lalani S, Aziz SZ, Hameed KA. Good knowledge about hypertension is linked to better control of hypertension; a multicentre cross-sectional study in Karachi, Pakistan. BMC Res Notes. 2012;5:579.
Mungati M, Manangazira P, Takundwa L, Gombe NT, Rusakaniko S, Tshimanga M. Factors affecting diagnostics and management of hypertension in Mazowe District of Mashonaland Central Province in Zimbabwe: 2012. BMC Cardiovasc Disord. 2014;14:102.
Fina LJP, Mabuza L, Malete N, Maduna P, Ndimande VJ. Reasons for non-compliance among patients with hypertension at Vanga Hospital, Bandundu province, Democratic Republic of Congo: a qualitative study. Afr J Prim Health Care Fam Med. 2009;. doi:10.4102/phcfm.Vlil.68.
Okken VS, Niemeijer MG, Dijkstra A, Baars MW, Said S, Hoogenberg K, et al. The effect of physical, social and psychological factors on drug compliance in patients with mild hypertension. Neth Heart J. 2008;16:197–200.
Saounatsou M, Patsi O, Fasoi G, Stylianou M. The influence of the hypertensive patient’s education in compliance with their medication. Public Health Nurs. 2001;18(6):436–42.
NCCAM (National Center for Complementary and Alternative Medicine). 2015. http://nccam.nih.gov/health/whatiscam/. Accessed 13 Mar 2015
Kretchy AI, Owusu-Daaku TF, Danquah S. Locus of control and antihypertensive medication adherence in Ghana. Pan Afr Med J. 2014;17(Supp 1):13.
Okoro RN, Ngong CK. Assessment of patient’s antihypertensive medication adherence level in non-comorbid hypertension in a tertiary hospital in Nigeria. Int J Pharm Biomed Sci. 2012;3(2):47–54.
Siew-Mooi C, Vasudevan R, Zacharia Z, Paimin F. Frequency of complementary and alternative medicine usage among Malaysian hypertensive subjects. Life Sci J. 2013;10(4):2526–31.
Kretchy AI, Owusu-Daaku F, Danquah F. Patterns and determinants of the use of complementary and alternative medicine: a cross-sectional study of hypertensive patients in Ghana. BMC Complement Altern Med. 2014;14:44.
Ghozzi H, Kassis M, Hakim A, Sahnoun Z, Abderrhmen A, Abbes R, et al. Observance médicamenteuse chez un échantillon d’hypertendus dans la région de Sfax (Tunisie). Ann Cardiol Angeiol. 2010;59(3):131–7.
Authors’ contributions
LN, AL and PM designed the research, AL and PM conducted the fieldwork and analyzed data; AL, PM and EM wrote the paper; and AM, MM, PK and YC revised the manuscript. AL has the primary responsibility for the final content. All authors read and approved the final manuscript.
Acknowledgements
We acknowledge the Bureau Diocésain des Oeuvres médicales de Kinshasa (BDOM) and the Bureau Médical de l’Armée du Salut for their approval for data collection in their health care facilities. We acknowledge, too, all health care providers and patients for their participation. We are thankful to the United States Agency for International Development (USAID) for their funding for data collection. Also, we are grateful to Future Health Systems (FHS) for providing small grants to the Kinshasa School of Public Health through Africa Hub, funded by the Department for International Development (DFID) for stationery paper. These funding sources are non-commercial.
Compliance with ethical guidelines
Competing interests The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Lulebo, A.M., Mutombo, P.B., Mapatano, M.A. et al. Predictors of non-adherence to antihypertensive medication in Kinshasa, Democratic Republic of Congo: a cross-sectional study. BMC Res Notes 8, 526 (2015). https://doi.org/10.1186/s13104-015-1519-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13104-015-1519-8