Abstract
Background
International studies on occupational risks in public hospitals are infrequent and only few researchers have focused on psychosocial stress in Moroccan Health Care Workers (HCWs). The aim of this study was to present and analyze Moroccan HCWs occupational risk perception. Across nine public hospitals from three Moroccan regions (northern, central and southern), a 49 item French questionnaire with 4 occupational risks subscales, was distributed to 4746 HCWs. This questionnaire was based on the Job Content Questionnaire. Psychosocial job demand, job decision latitude and social support scores analysis were used to isolate high strain jobs. Occupational risks and high strain perception correlation were analyzed by univariate and multivariate logistic regression.
Results
2863 HCWs (60 %) answered the questionnaire (54 % women; mean age 40 years; mean work seniority 11 years; 24 % physicians; 45 % nurses). 44 % of Moroccan HCWs were at high strain. High strain was strongly associated with two occupational categories: midwives (2.33 OR; CI 1.41–3.85), full-time employment (1.65 OR; CI 1.24–2.19), hypnotics and sedatives use (1.41 OR; CI 1.11–1.79), analgesics use (1.37 OR; CI 1.13–1.66).
Conclusion
Moroccan HCWs, physicians included, perceive their job as high strain. Moroccan HCWs use of hypnotics, sedatives and analgesics is high. Risk prevention plan implementation is highly recommended.
Similar content being viewed by others
Background
The workplace is an important contributor to a multitude of illnesses and is a determinant of the individual’s well-being. Among numerous risks found in the workplace, one entity has emerged lately to be a major public health concern and a challenge to the occupational health research field: the psychosocial risks (PSR). Psychosocial risks appear to be at the center of the intricate architecture of the work conditions.
Previous studies support the influence of negative organizational climate on nurses’ health [1], as well as the interactions between the physical and psychosocial risks factors that can generate musculoskeletal disorders [2]. The impact of occupational safety climate in hospitals confirms the link between PSR and workers’ health [3, 4]. In Europe, according to the working conditions surveys, the influence of PSR factors in the workplace was the second major change in working environments [5]. The European Agency for Safety and Health at Work (EU-OSHA), in its report on emerging risks [6] indicated that there is a strong correlation between variables considered for inclusion in the Occupational Safety Health composite score. An imbalance between the number of industrial accidents and the number of occupational illnesses has also been noted: even if the first is decreasing, the latter is increasing [7]. In France, indicators defined by experts permit to demonstrate that workplace PSR factors often contribute to the occurrence of health problems: cardiovascular diseases, mental health disorders or musculoskeletal disorders [8].
As the workforce in the European Union (EU) is ageing and the work intensity is constantly increasing, questions on steps to be taken to keep the workforce active have arisen, bringing out the need for a well-designed employment policy [9]. The fact that over 40 million people in the EU are suffering of consequences of work-related stress, which translates in over 20 billion € of health and absenteeism costs [10], goes to underline the economic and social importance of addressing the issue of work-related psychosocial risks.
The European Commission’s (EC) guidelines on work-related stress itemized the steps to be taken. The first step was identifying the risk, with its sources and consequences, by the means of monitoring “job content, working conditions, terms of employment, social relations at work, health, well-being and productivity” [11]. One of the important methods of detecting work-related stress, therefore PSR, is using a risk-perception evaluation, since the individual’s subjective experience will be the generator of symptoms and diseases: from transient increase in heart rate and blood pressure to developing cardiovascular diseases, and from minor indicators of anxiety or depression to clinical developments of mental health problems. EC has identified the significant proportion of employees who acknowledge the impact work has on their health, in its Improving quality and productivity at work. Community strategy 2007–2012 on health and safety at work: “35 % of workers on average feel that their job puts their health at risk” [12].
Currently, international studies on occupational risks in the public hospitals are infrequent, as are researchers concentrating on psychosocial stress in Moroccan HCWs [13–16], many focusing on ethnic groups living in other countries or on patients with different conditions. The 2008 study of Laraqui et al. [17] was one of the very few suggesting the need for occupational stress evaluation in Moroccan HCWs, based on findings of high stress prevalence, and the necessity for working conditions improvement.
The objectives of the present study were to assess psychosocial risk perception among Moroccan HCWs using a validated questionnaire and to analyse occupational risk factors’ impact in Moroccan public hospitals. Attention was given to different aspects which influence the occurrence of “high strain” situations: ergonomics, working conditions, and to the use of analgesic, hypnotic and sedative medication. The main goal was to develop a model for high strain perception that could be used for crafting and implementing a specific prevention plan.
Methods
Sample
The study was a cross-sectional multicenter investigation, conducted in Moroccan public hospitals of the three Moroccan regions: northern, central and southern. The northern region included towns above the line which joined the cities of Sidi-Kacem and Taza; the northern region hospitals were those of Kenitra, Oujda and Larache. The southern region included municipalities below the line which joined the cities of Safi and Beni Mellal; the southern region hospitals were those of Agadir and Marrakech. The central region (between the two described lines) or the Casablanca region covered hospitals of Baouafi, Sekkat, Settat and Khouribga. All public hospitals’ staff was targeted. Our research obtained the approval of the Nantes Regional Ethics Committee (Comité de Protection des Personnes Ouest IV) on December 7th, 2010, for research on “Work Organisation Cancer and Health” (No. DC 2010-1199). The Moroccan Public Health Ministry’s and the Moroccan Occupational Health Ethic Committee (Ref. no 312-10, Casablanca) authorization were obtained before beginning the investigation.
Material
The occupational risks questionnaire was distributed. It had 49 questions grouped in four subscales. The first 30 items on work and psychosocial relations (decision latitude, psychological demand and social support—sum of supervisor and coworker support) were extracted from Karasek’s Job Demand Questionnaire (JCQ) [18]. The next items stemmed from a validated French questionnaire [19, 20]: eight items targeted workplace ergonomics and three items addressed workplace environment risks. The last 8 items focused on passive smoking, alcoholism and medication use (hypnotics, sedatives and analgesics) and were taken from the “Adults Health Barometer” of the French National Institute of Prevention and Health Education.
Procedure
The questionnaire was distributed and collected upon completion by Moroccan occupational medicine students. They informed the staff on the questionnaire’s purpose, items and anonymity. All 4746 employees from the nine public hospitals were considered eligible. All the employees and the Health and Safety Committee was informed of the study and approved it.
Data analysis
Moroccan occupational medicine students gathered the data. They used an Excel mask designed by the Medical Evaluation and Therapeutic Education Office of the Medical Information and Public Health Evaluation Department of Nantes University Hospital. Data was analyzed with ASS/STAT 8.2 and SPSS 13.0. Missing answers questionnaires were excluded from the analysis. Descriptive analysis of data was made: answer percentage for qualitative variables, mean and standard deviation for quantitative variables. Job Decision Latitude (JDL), Psychological Job Demand (PJD) and Social Support (SoSu) scores were calculated according to Karasek et al. [18] and Niedhammer and al. [21]. Threshold values for high PJD, low JDL and a low SoSu were respectively set to 24, 72 and 22 [21]. High strain occupations had PJD score over 24 and JDL score under 72. A SoSu score below 22 denoted social isolation. The DETA (French version of CAGE questionnaire for alcoholism screening) score could not be calculated due to the lack of answers to those items.
Bivariate analysis was performed with Chi squared test for categorical variables (e.g.: between medication use and drug consumption), with Student’s t test for between groups comparison of metric variables and with Pearson’s correlation coefficient for comparison of metric variables. Factors influencing the scores were determined by one-way ANOVA and by MANOVA for occupational categories adjustment. Step-by-step logistic regression was used for identifying factors connected to high PJD associated with low JDL.
Results
Descriptive data
Two thousand eight hundred and sixty-three HCWs (60 %) answered the questionnaire. 54 % of the HCWs were women. Mean age was 40.4 ± 10.2 years. Mean work seniority was 11.3 ± 9.9 years. 97 % of HCWs had a permanent employment contract and 79 % worked full-time. The participation rate varied among the different hospitals, with leading scores from Larache (northern Morocco) and Sekkat (Casablanca) hospitals (94 and 91 %) and lowest score (38 %) from Marrakech hospital (southern Morocco). The participation rate was higher in the administration departments (67 %) and lower in surgery and ancillary departments (57 %). The ancillary staff had the highest participation rate (74 %), followed by the custodial staff and the administrative staff (73 and 70 %). The technical staff (27 %), the psychologists (33 %) and the nursing aides (37 %) had the lowest participation in the study (Table 1).
Internal consistency of the study was determined for each subscale; Cronbach’s alpha coefficients were 0.596 for JDL, 0.383 PJD, 0.764 for SoSu, 0.737 for workplace ergonomics, 0.45 for environmental risks and 0.516 for medication use. SoSu and PJD scores were weakly correlated (r = −0.025, NS). JDL and PJD scores were correlated (r = 0.110, p < 0.01), as well as JDL and SoSu scores (r = 0.248; p < 0.01).
Psychosocial risks
JDL, PJD and SoSu scores were diverse among occupational categories (p < 0.001) (Table 2).
JDL, PJD and SoSu were independent of gender. JDL and SoSu decreased as the age of respondents increased (JDL correlation coefficient = −0.078, p < 0.01; SoSu correlation coefficient = −0.075, p < 0.01), situation persistent after adjustment for occupational category. The same JDL and SoSu pattern was found related to work seniority, but after adjustment for occupational category the situation persisted only for JDL. PJD was independent of age and seniority. JDL and PJD were independent of respondents’ employment type and contract. Temporary employees had higher social support (p < 0.001). Full-time employees scored lower in JDL and SoSu (p < 0.001), but higher in PJD (p < 0.001).
Other risks: use of hypnotics or sedatives, use of analgesics, working conditions
20 % of respondents reported taking hypnotics or sedatives on a regular basis (more than once during the week preceding the investigation), with an equal proportion of men and women. On average they were older (43.2 ± 9.9 years versus 40.3 ± 10.0 years, p < 0.001). 41 % of respondents reported taking analgesics regularly (more than once during the week preceding the investigation). Most of them were women (43 % women versus 39 % men, p < 0.05) and were older (41.9 ± 10.1 years versus 40.3 ± 9.9 years, p < 0.001). Hypnotics or sedatives use significantly correlated to low JDL (p < 0.001). It also correlated to high PJD (p < 0.05) and lower SoSu (p < 0.01). Use of analgesics also correlated significantly to low JDL (p < 0.05), as well as to high PJD (p < 0.001) and lower SoSu (p < 0.05). The questions regarding the alcohol intake could not be used because the survey was accidentally carried out in the month of Ramadan (when, following a religious principle, use of alcohol is prohibited).
High strain
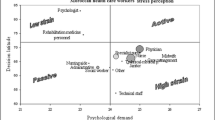
The respondents with the highest risk (high strain: occupational categories with the riskier combination of low job decision latitude, high psychological job demand and low social support) were midwives and nursing management. High strain occupations also included nurses, physicians and ancillary staff. No occupational category placed itself in the active job quadrant—high demand and high control (Fig. 1).
High strain was associated with employment contract and type, occupational category, workplace environment (noise level, lighting) and use of hypnotics and sedatives (p < 0.001) (Table 3).
Considering the risk factors in our model, stress level can be quantified by an equation: HS = a × PJD + b × JDL + c × SoSu + α (employment contract) + β (employment type) + γ (occupational category) + δ (work environment) + λ (care equipment availability), where HS = high strain, PJD = psychological job demand, JDL = job decision latitude, SoSu = social support.
Discussion
This is the first cross-sectional multicenter study to assess PSR perception and to estimate occupational stress in Moroccan public hospitals. It showed a good participation rate. We believe that hospital HCWs’ very strong desire to participate in the survey (94 % participation rate in Sekkat Casablanca and 91 % participation rate in Larache) speaks in itself about awareness and need for change in working conditions. There were not many studies on Moroccan HCWs’ PSR perception, aside of the work of Laraqui et al. [17], who first focused on national, multicenter PSR evaluation in Moroccan hospitals, and found a 21.7 % prevalence of stress. Karasek’s model of PSR assessment differentiated three work dimensions: psychological demands, decision latitude and social support. By placing the worker at the core of the working systems, it has found high international audience. Though Karasek’s JCQ was translated, tested and used in many different countries [21–24], most of the investigations included one or two occupational categories. Previous studies in healthcare focused mainly on nurses, probably because they were a more homogenous and easier to access group, as opposed to the more sensitive group of physicians. Due to its specific high workload and responsibilities, the latter group is a complex target. There are even studies who excluded physicians because of the difficulty in obtaining response [24]. As Robert Karasek has already stated in his 1998 study on psychosocial job assessment through JCQ [18], one of the problems with demanding job holders was their reluctance to participate in research projects, which resulted in underreporting and scientific substantiation weakening in the cause-effect correlation. Having that in mind and the 69 % of high-strain (low JDL, high PJD and low SoSu) HCWs in our study, a 60 % participation rate in the health care sector and a 67 % rate of responsiveness in physicians are dependable data for analysis, as the second of our investigation strengths is the size and diversity of the HCWs’ group.
Significantly more Moroccan HCWs have high strain jobs compared to French university hospital HCWs [19]. Whereas the French study found many active jobs: physician, nursing management and midwife, the Moroccan study brought to attention a crowded high-strain quadrant in the JDL-PJD diagram (Fig. 1). This included all of the above occupations, alongside nurses and even custodial staff, which were passive category in the French survey. In reverse, none of the Moroccan HCW jobs qualified as active. There might be a cultural mark involved, but the main reasons were economic and organizational: Moroccan physician and nurse staffing was insufficient, the doctors’ activity was always intense and had great time pressure, the staff was poorly paid and had low degree of job independence, many HCWs had to have a second job because of low pay, the technical equipment was often inadequate, outdated or faulty. Among the main perceived occupational risks, HCWs indicated also aggression, additional workload, musculoskeletal disorders and stress. Though physician and nurse were considered active jobs [18], there are many investigations with opposite results. Columbian nurses had high demands but also high control [25]. The 2004 French report [26] on public hospital HCWs showed great level of job autonomy in physicians, but a much lower one on nurses and nursing aides. The 2011 Italian study on risk factors in health care professionals [27] showed low JDL and SoSu scores for ancillary workers, but no significant variation in PJD, which is consistent with our findings. But differences in job demands are not unusual between countries and thus cultures. Pisanti et al. [28] brought evidence of higher pressure in Italian nurses as opposed to Dutch nurses, also consistent with the difference between PJD scores in our Moroccan nurses. But there are many elements to influence job perception and thus job satisfaction: the difficult climate of economic crisis leaves its mark on job security, even if all three scores of PJD, JDL and SoSu are high enough to place the nurse in the active jobs category [24].
High strain in nurses is also not uncommon and the reasons outlined by researchers reside as well in gender disparity: women report lower levels of decision latitude [18]. The 2008 study on Moroccan HCW’s found stress to be prevalent in female workers and in paramedics [17]. We did not find any gender influence on high-strain scores. However there are grounds for high strain in women: cultural elements, tradition, or increased workload (based on unclear competencies) forced on nurses [29]. Moroccan women have a different social status, since Moroccan traditional family structure gives them the household responsibilities, which may increase their general stress level [30]. Social status and high or low level of education can also influence understanding of any questionnaire content and purpose and may affect answer, bringing in bias [31].
Another study purpose was to build a ground basis for organizational and work environment changes, to decrease occupational stress and increase job control and social support. It has already been shown that, among many consequences, high JDL and SoSu enhanced safety participation [32]. After an intervention plan would be implemented in all Moroccan public hospitals, an evaluative re-analysis of PSR would be not only necessary but of high utility [33].
Our study showed no positive correlation between age and high strain (0.99 adjusted OR, CI: 0.98–0.99), similar to results from larger and more heterogeneous groups [18], though JDL and SoSu were decreasing with age, which is similar to the French study results [20]. We must consider the risk of cardiovascular disease (CVD) that comes with age, one which is already linked to job strain [34]. In a meta-analysis of fourteen prospective cohort studies, Kivimäki et al. suggested an average of 50 % excess risk of coronary heart disease when occupational stress was present [35]. A connection between occupational stress and inflammation appears to exist, the latter triggering CVDs [36].
Since we found no explanation for temporary HCWs having higher SoSu and for senior workers having lower SoSu, there is need for further investigation. Full-time employees experienced more stress than part-time employees, which was consistent with findings from previous studies [19, 20]. There was certainly more pressure and the perceived responsibility increases in full-time contract. Longer working time enhanced work load and stress, as its imprints on scores proved: lower JDL (65.5 ± 9.6), lower SS (21.6 ± 3.9) and higher PJD (24.7 ± 3.3).
Moroccan HCWs took significantly more hypnotics and sedatives (20 %) and analgesics (40 %) than French HCWs (9 and 25 %) [20]. The use of medication was significantly associated to high strain (p < 0.001). Medication use in Moroccan HCWs proved to be much higher than other reports from hospital environments. Virtanen et al. conducted a study in 21 Finnish hospitals and found lower usage rate: 5 % for anxiolytic and hypnotic medication and 16 % for pain killers [37]. Use of sedatives and hypnotics was linked to alternative shifts, night work, stress, workload and fatigue. Analgesics use associated with musculoskeletal disorders. Alcohol intake in Moroccan HCWs could not be analyzed because of the alcohol prohibition of Ramadan month. This was not taken into account when the study was designed and led to a study limitation.
Though PJD was lower in Moroccan HCWs, it still held a high score, and when associated to low JDL it concentrated a higher percentage of high strain HCWs (44 %) than the ones reported in other studies: 16.5 % in Taiwanese HCWs [23], 25 % in European workers [38]. This raises high concern and we feel it calls for an urgent intervention. As for the different occupational categories, it must be noted that Moroccan physicians were at a higher level of strain than physicians from any other country. In our study they were not an active occupation (Fig. 1). Work overload, insufficient staffing, poor doctor-patient relationship, low hospital budget are all triggers of occupation status deterioration. All studies on perceived stress focusing on or including doctors have placed them in the high demand-high control job category. This indicates higher risk degree in Moroccan doctors for developing CVDs and mental disorders. Higher depression rates compared to general population have been reported in physicians with high work demands [39]. At the other end, Moroccan rehabilitation medicine staff was classified as having a passive job, similar to findings in other reports [39, 40], which attested a much lower degree of independence.
Limitations and future research
Our study has encountered a number of limitations. The weak points of self-reporting must be first restated. There is no solution to avoid or limit individual variation in PSR perception. The target is a personal, subjective sensation and understanding and not an objective quantification. But there is sufficient evidence that perception is at the origin of changes in well-being and of ill health, and prevention of health alterations is occupational medicine’s ultimate goal. Participants in the study have not been randomly selected. Reasons for unresponsiveness were not requested. Results may have been influenced by exclusion of subjects due to missing item answers. Karasek’s demand-control model leaves out the effort-reward balance and the patient-caregiver relationship, and there is no data on absenteeism, presenteeism and patient admission rates, factors to be taken into account in future investigation. The questionnaire version used in Morocco wasn’t perfectly identical to the one used in the French studies (see Additional file 1) [19, 20], because some workstation ergonomics items weren’t identical and therefore not mentioned. We don’t know whether job musculoskeletal injury with concomitant sedative/hypnotic and/or analgesic use preceded high strain or if high strain caused those things. However, the study provides an accurate picture of PSR in Moroccan public hospitals. It brings forward a map of stressful occupations and it points out priorities for action. Future analysis could highlight more factors to influence occupational stress and improve our mathematical formula.
Conclusions
The aim of this study was to carry out a multicenter investigation focused on assessing PSR perception and occupational risk in Moroccan public hospitals. Our results show that Moroccan HCWs, physicians included, have high strain activity. There were no active occupations found after PSR analysis, which show HCW’s low level of work control. Use of hypnotics, sedatives and analgesics is at high level in Moroccan HCWs and correlates with high strain. Since sedative use is high, it would be important to know whether the analgesic use is primarily NSAIDs/Tylenol vs opioids, then this is future investigation that should be done. Further research with an enlarged study pool and a more exhaustive analysis would bring more information on PSR and HCWs’ health and would help design better occupational safety and health policy, aimed at enhancing and consolidating HCWs well-being at work.
References
Gershon RRM, Stone PW, Zeltser M, Faucett J, Macdavitt K, Chou SS. Organizational climate and nurse health outcomes in the United States: a systematic review. Ind Health. 2007;45:622–36.
Devereux JJ, Vlachonikolis IG, Buckle PW. Epidemiological study to investigate potential interaction between physical and psychosocial factors at work that may increase the risk of symptoms of musculoskeletal disorder of the neck and upper limb. Occup Environ Med. 2002;59:269–77.
Roland-Lévy C, Lemoine J, Jeoffrion C. Health and well-being at work: The hospital context. Eur Rev Appl Psychol. 2014;64:53–62. doi:10.1016/j.erap.2014.01.002.
Smith DR, Muto T, Sairenchi T, Ishikawa Y, Sayama S, Yoshida A, Townley-Jones M. Hospital safety climate, psychosocial risk factors and needlestick injuries in Japan. Ind Health. 2010;48(1):85–95.
European Foundation for the Improvement of Living and Working Conditions. Rise in psychosocial risk factors at the workplace. 2009. http://www.eurofound.europa.eu/ewco/surveyreports/FR0909019D/FR0909019D.pdf. Accessed 15 Jan 2014.
Van Stolk C, Staetsky L, Hassan E, Chong Woo K. European Agency for Safety and Health at Work (EU-OSHA). Management of psychosocial risks at work: An analysis of the findings of the European Survey of Enterprises on New and Emerging Risks (ESENER). European Risk Observatory (Report). Luxembourg: Publications Office of the European Union 2012.
European Foundation for the Improvement of Living and Working Conditions. A review of working conditions in France. 2007. http://www.eurofound.europa.eu/ewco/surveys/FR0603SR01/FR0603SR01.pdf. Accessed 15 Jan 2014.
Collège d’expertise sur le suivi statistique des risques psychosociaux au travail. Indicateurs provisoires de facteurs de risques psychosociaux au travail. 2009. http://www.college-risquespsychosociauxtravail.fr/site/medias/indicateurprovisoires.pdf. Accessed 11 July 2014.
Eurofound. Fifth European Working Conditions Survey. Luxembourg: Publications Office of the European Union 2012.
Leka S, Cox T. PRIMA-EF guidance on the European framework for psychosocial risk management: a resource for employers and worker representatives. Geneva: World Health Organization; 2008.
Commission European. Guidance on work-related stress—Spice of life or kiss of death?. Luxembourg: Office for Official Publications of the European Communities; 2002.
European Commission. Improving quality and productivity at work: Community strategy 2007–2012 on health and safety at work. Communication from the Commission to the European Parliament, the Council, the European Economic and Social Committee and the Committee of the Regions. 21 Feb 2007. http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=COM:2007:0062:FIN:EN:PD.
Goedhart G, Snijders AC, Hesselink AE, van Poppel MN, Bonsel GJ, Vrijkotte TG. Maternal depressive symptoms in relation to perinatal mortality and morbidity: results from a large multi-ethnic cohort study. Psychosom Med. 2010;72(8):769–76.
Crone MR, Bekkema N, Wiefferink CH, Reijneveld SA. Professional identification of psychosocial problems among children from ethnic minority groups: room for improvement. J Pediatr. 2010;156(2):277–84.
Eichelsheim VI, Buist KL, Deković M, Wissink IB, Frijns T, van Lier PA, Koot HM, Meeus WH. Associations among the parent-adolescent relationship, aggression and delinquency in different ethnic groups: a replication across two Dutch samples. Soc Psychiatry Psychiatr Epidemiol. 2010;45(3):293–300.
Abourazzak FE, Allali F, Rostom S, Hmamouchi I, Ichchou L, El Mansouri L, Bennani L, Khazzani H, Abouqal R, Hajjaj-Hassouni N. Factors influencing quality of life in Moroccan postmenopausal women with osteoporotic vertebral fracture assessed by ECOS 16 questionnaire. Health Qual Life Outcomes. 2009;7:23.
Laraqui O, Laraqui S, Tripodi D, Caubet A, Verger C, Laraqui CH. Evaluation du stress chez le staff de santé au Maroc: à propos d’une étude Multicentrique. Stress assessment among health care workers in Morocco. Arch Mal Prof Environ. 2008;69:672–82.
Karasek RA, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3:322–55.
Tripodi D, Keriven-Dessomme B, Lombrail P, Bourut Lacouture M, Chabot AS, Houdebine MT, Gordeeff C, Durand Perdiel MH, Moret L, Dupas D, Cantineau A, Geraut C. Evaluation des risques professionnels perçus chez le staff du centre hospitalo-universitaire de Nantes. Arch Mal Prof Environ. 2007;68:457–73.
Tripodi D, Roedlich C, Laheux MA, Longuenesse C, Roquelaure Y, Lombrail P, Geraut C. Stress perception among employees in a French University Hospital. Occup Med (Lond). 2012;62(3):216–9.
Niedhammer I. Psychometric properties of the French version of the Karasek Job Content Questionnaire: a study of the scales of decision latitude, psychological demands, social support, and physical demands in the GAZEL cohort. Int Arch Occup Environ Health. 2002;75(3):129–44.
Araújo TM, Karasek R. Validity and reliability of the job content questionnaire in formal and informal jobs in Brazil. SJWEH. 2008;6:52–9.
Chien TW, Lai WP, Wang HY, Hsu SY, Castillo RV, Guo HR, Chen SC, Su SB. Applying the revised Chinese Job Content Questionnaire to assess psychosocial work conditions among Taiwan’s hospital workers. BMC Public Health. 2011;18(11):478.
Eum KD, Li J, Jhun HJ, Park JT, Tak SW, Karasek R, Cho SI. Psychometric properties of the Korean version of the job content questionnaire: data from health care workers. Int Arch Occup Environ Health. 2007;80(6):497–504.
GomezOrtiz V. Evaluación de estresores psicosociales en el trabajo: propiedades psicométricas del Cuestionario del contenido del trabajo (JCQ) con trabajadores colombianos. Rev Latinoam Psicol. 2011;43(2):329–42.
Le Lan R., Baubeau D. Les conditions de travail perçues par les professionnels de santé. Études et résultats. DREES. 2004;335. http://www.drees.sante.gouv.fr/IMG/pdf/er335.pdf. Accessed 20 May 2014.
Albini E, Zoni S, Parrinello G, Benedetti L, Lucchini R. An integrated model for the assessment of stress-related risk factors in health care professionals. Ind Health. 2011;49(1):15–23.
Pisanti R, van der Doef M, Maes S, Lazzari D, Bertini M. Job characteristics, organizational conditions, and distress/well-being among Italian and Dutch nurses: a cross-national comparison. Int J Nurs Stud. 2011;48(7):829–37.
Bojtor A. The importance of social and cultural factors to nursing status. Int J Nurs Pract. 2003;9(5):328–35.
Chahraoui K, Bioy C, Gilles F, Laurent A, Valache B, Quenot JP. Vécu psychologique des soignants en réanimation: une étude exploratrice et qualitative. Ann Fr Anesth Reanim. 2001;30:342–8.
Hökerberg YH, Aguiar OB, Reichenheim M, Faerstein E, Valente JG, Fonseca Mde J, Passos SR. Dimensional structure of the demand control support questionnaire: a Brazilian context. Int Arch Occup Environ Health. 2010;83(4):407–16.
Turner N, Stride CB, Carter AJ, McCaughey D, Carroll AE. Job demands-control-support model and employee safety performance. Accid Anal Prev. 2012;45:811–7.
Bourbonnais R, Brisson C, Vézina M. Long-term effects of an intervention on psychosocial work factors among healthcare professionals in a hospital setting. Occup Environ Med. 2011;68(7):479–86.
Belkic KL, Landsbergis PA, Schnall PL, Baker D. Is job strain a major source of cardiovascular disease risk? Scand J Work Environ Health. 2004;30(2):85–128.
Kivimäki M, Virtanen M, Elovainio M, Kouvonen A, Väänänen A, Vahtera J. Work stress in the etiology of coronary heart disease–a meta-analysis. Scand J Work Environ Health. 2006;32(6):431–42.
Poantă L, Crăciun A, Dumitraşcu DL. Professional stress and inflammatory markers in physicians. Rom J Intern Med. 2010;48(1):57–63.
Virtanen M, Vahtera J, Batty GD, Tuisku K, Oksanen T, Elovainio M, Ahola K, Pentti J, Salo P, Vartti AM, Kivimäki M. Health risk behaviors and morbidity among hospital staff–comparison across hospital ward medical specialties in a study of 21 Finnish hospitals. Scand J Work Environ Health. 2012;38(3):228–37.
Niedhammer I, Sultan-Taïeb H, Chastang JF, Vermeylen G, Parent-Thirion A. Exposure to psychosocial work factors in 31 European countries. Occup Med (Lond). 2012;62(3):196–202.
Wang LJ, Chen CK, Hsu SC, Lee SY, Wang CS, Yeh WY. Active job, healthy job? Occupational stress and depression among hospital physicians in Taiwan. Ind Health. 2011;49(2):173–84.
Campo MA, Weiser S, Koenig KL. Job strain in physical therapists. Phys Ther. 2009;89(9):946–56.
Authors’ contributions
DT draw the design, implemented the project in France and then in Morocco. He contributed to the methods, the questionnaire creation, he contributed to discussion and manuscript revision; he mentored DIG in research internship in the Department of Occupational Medicine and Occupational Hazards, University Hospital of Nantes and mentored the Moroccan occupational medicine students studying for a university degree in occupational medicine. DIG contributed to methods, to data analysis, interpretation and discussion, wrote and revised the manuscript. CJ and BG contributed to data analysis and interpretation. CJ commented on drafts of the manuscript and revised it critically. BKD advised on and contributed to data analysis and interpretation; PL, LM and YR contributed to the creation and validation of the French version of the Questionnaire. AC, CV, CG have supported the study and commented on drafts of the manuscript. CEHL supported the study, mentored the Moroccan occupational medicine students and commented on drafts of the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The authors acknowledge the participation and help of the Moroccan occupational medicine students. DIG’s contribution to the study is part of research carried out within the framework of POSDRU/CPP107/DMI1.5/S/76851 project, co-financed by the European Social Fund through the Sectoral Operational Programme Human Resources Development 2007–2013.
Compliance with ethical guidelines
Competing interests The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional files
Additional file 1.
French version of the questionnaire
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Giurgiu, D.I., Jeoffrion, C., Grasset, B. et al. Psychosocial and occupational risk perception among health care workers: a Moroccan multicenter study. BMC Res Notes 8, 408 (2015). https://doi.org/10.1186/s13104-015-1326-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13104-015-1326-2