Abstract
Background
Sulawesi in Indonesia has a unique geographical profile with assumed separation from Sundaland. Studies of Helicobacter pylori in this region are rare due to the region’s rural location and lack of endoscopy equipment. Indirect methods are, therefore, the most appropriate for measuring H. pylori infection in these areas; with the disposable gastric brush test, we can obtain gastric juice as well as small gastric tissue samples for H. pylori culture. We investigated the prevalence of H. pylori infection and evaluated human migration patterns in the remote areas of North Sulawesi.
Methods
We recruited a total of 251 consecutive adult volunteers and 131 elementary school children. H. pylori infection was determined by urine antibody test. A gastric brush test was used to culture H. pylori. We used next-generation and polymerase chain reaction based sequencing to determine virulence factors and multi-locus sequence typing (MLST).
Results
The overall H. pylori prevalence was only 14.3% for adults and 3.8% for children, and 13.6% and 16.7% in Minahasanese and Mongondownese participants, respectively. We isolated a single H. pylori strain, termed -Manado-1. Manado-1 was East Asian type cagA (ABD type), vacA s1c-m1b, iceA1 positive/iceA2 negative, jhp0562-positive/-(1,3) galT-negative, oipA ‘on’, and dupA-negative. Phylogenetic analyses showed the strain to be hspMaori type, a major type observed in native Taiwanese and Maori tribes.
Conclusions
Our data support that very low H. pylori infection prevalence in Indonesia. Identification of hspMaori type H. pylori in North Sulawesi may support the hypothesis that North Sulawesi people migrated from north.
Similar content being viewed by others
Background
Southeast Asia is a culturally-diverse region enriched by multiple ethnicities and indigenous communities [1]. Indonesia, a developing country at the southeastern tip of mainland Asia and Oceania, is an archipelago of more than 13,600 islands; it has more than 1,000 ethnic and sub-ethnic groups delineated by the Wallace Line, a faunal boundary that separates Asian and Australian ecozones and organisms. Indonesia has more than 730 indigenous languages, most of them belonging to the geographically dispersed Austronesian language family [2]. The age-standardized incidence rate of gastric cancer in Indonesia is reportedly 2.8/100,000, relatively low among Asian countries (International Agency for Research on Cancer; GLOBOCAN2012, http://globocan.iarc.fr/).
More than half of the world’s population is infected with Helicobacter pylori, a Gram-negative bacterium etiologically associated with peptic ulcer disease, gastric adenocarcinoma, and primary gastric B-cell lymphoma [3]. Unlike several Southeast Asian countries with high H. pylori infection prevalence such as Thailand and the Philippines (54.1 to 76.1% and 60%, respectively) [4],[5], several studies have reported low prevalence in Indonesia [6]-[13]. However these studies primarily investigated Javanese populations, the major ethnic group in Indonesia.
North Sulawesi is an Indonesian province in the northernmost part of Sulawesi Island with Manado as its capital city of; it is composed of 15 districts, with Minahasanese being the predominant tribe. There are currently no detailed data about H. pylori infection prevalence in minor ethnic groups in North Sulawesi. This is partly due to a lack of endoscopy systems in remote areas of North Sulawesi. Although invasive, endoscopy gives more information and allows culture of H. pylori. We believe that indirect (non-invasive) methods such as the rapid urine test are the best choice for measuring H. pylori infection in these areas. Another test option is the disposable gastric brush, which can obtain gastric juice and small gastric tissues for H. pylori culture. This study therefore investigated the prevalence of H. pylori infection in the remote areas of North Sulawesi using rapid urine and gastric brush tests.
H. pylori strains from different geographical areas exhibit clear phylogeographic features and H. pylori population genetics studies can provide information about the migration of human populations [14]-[17]. Importantly, North Sulawesi has a unique geographical profile: although the central and western sections of the Indonesian archipelago were connected by dry land to the Asian mainland (Sundaland), Papua (New Guinea) was linked with Australia into a single continent (Sahul) about 60,000 years ago (60 ka). Sulawesi and the Philippines (except for Palawan) are assumed to be zoogeographically separated from Sundaland, a hypothesis supported by distribution patterns of mammals and birds [18]. Several authors believe that the ancestors of the North Sulawesi peoples came from the north because the traditions, manners, customs, and languages of the Minahasanese and Mongondownese people belong to the Philippine language group [19].
We previously showed that H. pylori could be divided into seven major populations (hpAfrica1, hpAfrica2, hpNEAfrica, hpEurope, hpAsia2, hpEastAsia, and hpSahul) based on multi locus sequence typing (MLST) using sequences of seven housekeeping genes (atpA, efp, mutY, ppa, trpC, ureI, and yphC) [14],[15],[20]. hpEastAsia is divided into three subpopulations: hspMaori in native Taiwanese, Polynesian, and Melanesian people. Our recent analyses showed that hspMaori populations migrated from Taiwan through the Pacific around 5,000 years ago [20]. However, the study did not include H. pylori strains from Sulawesi or several islands in eastern Indonesia. It is important to clarify this migration model to support our hypothesis that Indonesia could be a junction of human migration and that waves of human migration occurred more than twice in this region. Therefore, a second purpose of this study was to use H. pylori as a tool to evaluate human migration patterns.
Results
Study population and H. pylori infection rate in North Sulawesi
We performed three surveys in North Sulawesi province from April 30 to May 1, 2011, January 30 to February 3, 2012, and July 23-24, 2012. Consecutive adult volunteers were enrolled in each survey. In total, 251 volunteers (146 women and 105 men; mean age, 46.2°19.5 years old; range, 14-88 years) were included and provided urine samples. The study consisted of 147 Minahasanese subjects, 90 Mongondownese, six Javanese, three Gorontalonese, one Makassarese, one Ternatenese, one Sangirese, one Balinese, and one Bataknese subject. A map of the collection area is shown in Figure 1. We also obtained urine samples from 131 elementary school children (71 girls and boys; mean age 8.47°1.64 years; range, 6-12 years) in Wori during the July 23-24, 2012 survey.
The population of 251 adult volunteers consisted of 57 subjects aged -29 years, 34 subjects aged 30-39 years, 60 subjects aged 40-49 years, 37 subjects aged 50-59 years, and 63 aged -60 years old. The H. pylori prevalence by age group was 14.0% (8/57), 11.7% (4/34), 15.0% (9/60), 16.2% (6/37), and 14.3% (9/63) respectively, with an overall H. pylori based on urine testing of 14.3% (36/251) (Figure 2). There was no statistically significant relationship between H. pylori prevalence and age or sex (P=0.84 and P=0.69). Only five elementary school children (3.8%) were positive for H. pylori, a rate significantly lower than the adult population (P=0.02).
To confirm the urine test accuracy, 50 subjects were randomly selected among the 251 adult volunteers for H. pylori seropositivity serum testing. Three (6.0%) patient serum samples were positive for H. pylori antibodies, identical to the urine test findings (100% sensitivity, specificity, and accuracy based on serum H. pylori antibody test as a gold standard).
H. pylori infection rates according to ethnicity
Among 147 Minahasanese subjects, 20 (13.6%) were positive for H. pylori. Fifteen of 90 (16.7%) Mongondownese were positive for H. pylori infection (P=0.59 compared with Minahasanese). One of six (16.6%) Javanese study subjects was positive for H. pylori. In contrast, none of the Gorontalo, Makassarese, Ternatenese, Sangirese, Balinese, or Bataknese study subjects tested positive for H. pylori infection.
Identification of a North Sulawesi H. pylori genotype
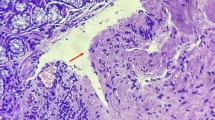
Among 36 patients infected with H. pylori, 6 agreed to undergo gastric brush tests. We successfully cultured H. pylori from one patient; we termed the strain Manado-1.
Virulence factor analysis using PCR/PCR-based sequencing showed that the strain was East Asian type cagA (ABD type), vacA s1c-m1b, iceA1 positive/iceA2 negative, jhp0562-positive/-(1,3) galT-negative, oipA ‘on’ and dupA-negative. A Genbank database BLAST search of full-length Manado-1 cagA sequences showed greatest nucleotide similarity with strains PHL2 (GU173854.1) and PHL10 (GU173856.1) from the Philippines, with homologies of 97.7% and 97.6%, respectively.
Manado-1 population type
We constructed a phylogenetic tree using MLST sequence data from Manado-1 and 1,231 PubMLST strains. Manado-1 clustered with hspMaori strains (Figure 3). Branch colors represent H. pylori populations previously determined using STRUCTURE Bayesian clustering software [16].
Phylogenetic tree based on the seven housekeeping genes of H. pylori . Sequence data sets of the seven housekeeping genes of 1,126 strains with different genotypes were obtained from the pubMLST database (62 from hpAsia2, 493 from hpEurope, 76 from hpNEAfrica, 50 from hpSahul, 28 from hpAfrica2, 279 from hpEastAsia, and 138 from hpAfrica1). The 1,126 reference strains from GenBank, Manado-1, and Taiwan-47 strains are included. Neighbor-joining trees were constructed in MEGA v.5.05 using Kimura-2 parameters. The scale bar indicates genetic distance.
We sequenced Manado-1 and a strain isolated from a native Taiwanese participant (Taiwan-47) using the next-generation sequencer. We used next-generation sequencing data to construct 39 and 34 Manado-1 and Taiwan-47 contig sequences, respectively (average sequencing coverage and %GC of 2,455x and 38.9% and 721x and 38.7%, respectively), and extracted protein-coding sequences from the contigs. We then integrated this data with sequence data obtained from GenBank to construct a phylogenetic tree based on the concatenated sequences of 644 orthologous genes shared by all analyzed strains.
Manado-1 and Taiwan-47 formed a phylogenetic tree sub-branch with Malaysian and some Okinawa strains, which reflects phylogeographic differences from typical East Asian strains (Figure 4).
Nucleotide sequences
Nucleotide sequence data for strains Manado-1 and Taiwan-47 are available under DDBJ accession numbers AB985740 to AB985753 for MLST, and JRAC00000001-38 and JQNY00000001-58 for the genome data using the next generation sequencer.
Discussion
We observed extremely low H. pylori prevalence in North Sulawesi, Indonesia using RAPIRUN, a rapid immunochromatography method for detection of anti-H. pylori IgG in urine; this result is consistent with our previous report of very low prevalence among Javanese [6]-[12],[21]. We recently confirmed the high accuracy of RAPIRUN using five different methods to test H. pylori status (culture, rapid urease test, histology, immunohistochemistry, and RAPIRUN) in Surabaya, on Java island in Indonesia [21]. In this study, we also found identical results from urine and serum samples.
Contrary to typical age-related H. pylori prevalence patterns in developing countries, where H. pylori infections occur earlier in life and with higher frequency [22], we found that only 3.8% of participants with a mean age 8.47 years were infected. Even taking into account the possibility of negative rapid urine test results in children based on reports of lower antibody titers than true positive results [23], the prevalence of H. pylori in children in North Sulawesi was very low. The transmission routes of H. pylori are still not entirely understood, but human-to-human spread through oral-oral or fecal-oral routes are considered the most plausible infection routes [22]. In developing countries, H. pylori is mainly transmitted feco-orally, in contrast to gastro-oral transmission in developed countries [24]. The degrees of crowding and contact between family members during are important variables. For example, Malaty et al. reported a 23% H. pylori prevalence in children of infected mothers, whereas only a 5% prevalence was observed in children of uninfected mothers [25]. Further studies are necessary to clarify the role of familial clustering in typical age-related prevalence patterns of H. pylori infection in North Sulawesi.
Javanese form the predominant ethnic group in Surabaya and have a close genetic relationship and common ancestral history with Melayu populations in Malaysia [26], which also have low H. pylori infection rates [1], suggesting that host genetic factors might contribute to reduced H. pylori infection susceptibility. However, the Javanese ethnic origins differ from those of Minahasanese, so it is unclear why the H. pylori prevalence was very low in both ethnic populations.
Although H. pylori was isolated from only one subject in North Sulawesi, it was interesting that the strain was hspMaori, a subpopulation of the East Asian type often isolated from native Taiwanese and Maori tribes as well as some individuals from the Philippines [20]. The Philippines and Sulawesi are neighboring regions assumed to be zoogeographically separated from Sundaland. Therefore, our data support the hypothesis that the Philippines hspMaori type was not only spread directly to the Pacific islands, but also to Sulawesi. Previously, the hpSahul populations were believed to pass through the Pleistocene landmass known as Sundaland (i.e., the Malay peninsula, Sumatra, Java, Borneo, and Bali) 23,000 to 32,000 years ago [20]. Much later, migration of Javanese ancestors through this region likely replaced the indigenous peoples; therefore, hpSahul remained isolated in New Guinea and Australia.
However, differences in H. pylori infection rates between this study and data from the Philippines was marked: H. pylori prevalence in the Philippines is a reported 60% (31/52) [5]. This difference cannot be explained by sanitary conditions alone, because food hygiene and drinking water quality in the Philippines are better than in Indonesia: approximately 50% of the Indonesian population has basic environmental sanitary conditions, especially in rural areas (UNICEF, http://www.unicef.org/). Two possibilities could explain differences in H. pylori infection rates between Minahasanese and Philippinos. First, H. pylori prevalence might be low among native Philippinos with hspMaori type. However, it does also not mean that hspMaori H. pylori is universally difficult to infect, since H. pylori prevalence in native Taiwanese is high [27]. As a former Spanish colony, current Philippino populations may have acquired H. pylori through intermarriage of various races and nationalities with indigenous ethnic groups, resulting in reduced hspMaori strains due to competition with novel strains. This theory is supported by the fact that the majority of CagA types in the Philippines are Western type [28]. Interestingly, Minahasanese populations also had extensive relations and communications with Western countries, especially the Dutch (350 years ago), but relatively few people are infected with H. pylori. Therefore, specific environmental factors including Minahasanese dietary habits, may contribute to reduced H. pylori susceptibility in North Sulawesi.
The second possibility to explain different infection rates is that migration waves from Taiwan through the Pacific that distributed hspMaori around 5,000 years ago might not involve Sulawesi island; the original introduction of the Manado-1 strain may have occurred later, which is likely considering that Manado is a coastal city. In this hypothesis, Minahasanese and Philippinos might have different ancestral origins. A larger sample size of H. pylori strains isolated from North Sulawesi is necessary to elucidate the origin of H. pylori strains in Indonesia.
Only one strain was obtained after culturing, which was one limitation of this study. The lack of frozen conditions during transportation likely contributed to the low culture rate of the gastric brush test. H. pylori recovery rates have been reported to be 25% (1 of 4) when stored for 7 days at 4°C, resulting in markedly diminished recovery [29]. In this survey we kept the specimens at 4°C from the time of collection at the rural hospital to the time they were stored at -20°C for a week at Sam Ratulangi University, Manado. The specimens were then sent to Surabaya at room temperature to be kept at -20°C for 3 days at Airlangga University Faculty of Medicine before culture. Future surveys should immediately freeze or culture the fluid that dripped from the brush.
Another limitation of this study was a lack of volunteer medication information. It is possible that we have included patients who had been administered antibiotics, histamine-2 receptor antagonists (H2-blockers), or proton pump inhibitors, which can influence H. pylori infection prevalence. However, a previous report found the prevalence of H. pylori infection in Indonesia to be quite low (10.2%) even after patients taking proton pump inhibitors were excluded from the study population [10].
Conclusions
We found extremely low H. pylori prevalence in North Sulawesi. We also discovered an hspMaori type strain in North Sulawesi, which was widespread among aboriginal Taiwanese tribes, supporting the hypothesis that North Sulawesi people came from the north, although these findings remain to be confirmed.
Methods
H. pylori infection status
H. pylori status was evaluated with a rapid urine test (RAPIRUN® H. pylori antibody, Otsuka Pharmaceutical Co., Tokyo, Japan) according to the manufacturer’s instructions. RAPIRUN has been reported to have high accuracy, with excellent sensitivity, specificity, and accuracy in Japanese (92.0%, 93.1%, and 92.3%, respectively) [30] and Vietnamese populations [31]. Immediately after collection, urine samples were tested for H. pylori antibodies. All urine samples were measured and analyzed by a skilled researcher (MM) blinded to subjects’ information.
A disposable extendable oro-gastric brush was constructed on a guide-wire with a handle (modified Baylor Gastric Brush, Tochigi Seiko, Tochigi, Japan). The brush was ~5 mm in diameter and fit within an enlarged distal sheath portion. Withdrawal of the brush into the sheath closed the brush compartment. After administration of topical oral anesthesia, the 5-mm brush assembly was swallowed. Approximately 60°Cm from the incisor teeth, the brush was extended and moved back and forth 38°Cm, three or four times. The brush was then retracted into the protective sleeve and withdrawn from the subject. The brush was placed in a dram vial containing approximately 1 mL of cysteine transport medium with 20% glycerol [32], mixed by shaking, and 100 L withdrawn for culture. Samples were kept at 4°C and stored at -20°C within a day of collection at Sam Ratulangi University, Manado. The samples were then sent for isolation of H. pylori using standard culture methods at the Institute of Tropical Disease, Airlangga University in Surabaya [33]. Culture stocks were sent to Oita University Faculty of Medicine for further analyses.
We also randomly selected 50 subjects for anti-H. pylori antibody serum testing: serum samples were transported to the Institute of Tropical Disease at Airlangga University using the same procedure described above. H. pylori seropositivity was evaluated using a commercially available ELISA kit (Eiken Co., Ltd., Tokyo, Japan) according to the manufacturer’s instructions.
Informed consent was obtained from all participants, and the protocol was approved by the Ethics Committees of Sam Ratulangi University (Manado, Indonesia) and Oita University Faculty of Medicine (Yufu, Japan).
H. pylori isolation and genotyping
H. pylori DNA was extracted using the QIAamp DNA Mini Kit (QIAGEN, Valencia, CA) according to the manufacturer’s directions. Whole-genome sequencing was performed using 90-base paired-end reads on an Illumina HiSeq 2000 next-generation sequencer (Illumina, Inc., San Diego, CA). The nucleotide sequences of cagA, vacA, jhp0562, -(1,3) galT, oipA, iceA, and dupA genes were extracted from the data and confirmed by PCR-based sequencing as described previously [33]-[39]. Multi locus sequence typing genes; atpA, efp, mutY, ppa, trpC, ureI, and yphC were also extracted from the next-generation sequencing data and confirmed by PCR-based sequencing as described previously [34].
Phylogenetic analysis of H. pylori strains
A phylogenetic tree was constructed using MLST sequence datasets comprised of seven housekeeping genes from 1,231 strains with different genotypes obtained from the pubMLST database (http://pubmlst.org/). These sequence datasets were integrated with our North Sulawesi sequence data. A neighbor-joining tree was constructed based on the sequence alignment using MEGA v.5.05 (Kimura-2-parameter model) [40],[41]. We also sequenced Manado-1 and a strain isolated from a native Taiwanese participant (Taiwan-47) using the next-generation sequencer (HiSeq2000). HiSeq2000 output was integrated into contig sequences by CLC Genomics Workbench 7.0.4. Genomics Workbench was also used for gene prediction and translated to protein sequence using an original perl script. Protein coding genes of 47H. pylori strains whose genomes are publically available were obtained from GenBank. We defined gene groups using OrthoMCL gene clustering software and selected single-copy orthologs from each strain, resulting in a total of 644 gene groups. We aligned gene sequences using MAFFT version 7 (http://mafft.cbrc.jp/alignment/server/), concatenated the alignment using an original perl script, and used MEGA v.5.05 to construct a phylogenetic tree (Poison model, bootstrap 1,000).
Statistical analysis
Data were analyzed using SPSS, version 19 (SPSS Inc., Chicago, IL, USA). Discrete variables were tested using the chi-square test; continuous variables were tested using Mann-Whitney U and t-tests. A two-tailed P- value <0.05 was considered statistically significant.
Authors’ contributions
MM (Muhammad Miftahussurur) and YY designed the study; prepared the isolates; acquired, analyzed, and interpreted the data, and wrote the manuscript. RS carried out the sequence alignment and analysis of next generation sequencing results. JT, FK, and YK contributed to data analysis and interpretation. MM (Miyuki Matsuda) prepared isolates for analysis. SP, IST, and PNH contributed to data acquisition. All authors read and approved the final manuscript.
Abbreviations
- MLST:
-
Multi-locus sequence typing
- PCR:
-
Polymerase chain reaction
References
Lee YY, Mahendra Raj S, Graham DY:Helicobacter pylori infection - a boon or a bane: lessons from studies in a low-prevalence population. Helicobacter. 2013, 18: 338-346. 10.1111/hel.12058.
Tumonggor MK, Karafet TM, Hallmark B, Lansing JS, Sudoyo H, Hammer MF, Cox MP: The Indonesian archipelago: an ancient genetic highway linking Asia and the Pacific. J Hum Genet. 2013, 58: 165-173. 10.1038/jhg.2012.154.
Suerbaum S, Michetti P:Helicobacter pylori infection. N Engl J Med. 2002, 347: 1175-1186. 10.1056/NEJMra020542.
Sahara S, Sugimoto M, Vilaichone RK, Mahachai V, Miyajima H, Furuta T, Yamaoka Y: Role of Helicobacter pylori cagA EPIYA motif and vacA genotypes for the development of gastrointestinal diseases in Southeast Asian countries: a meta-analysis. BMC Infect Dis. 2012, 12: 223-10.1186/1471-2334-12-223.
Destura RV, Labio ED, Barrett LJ, Alcantara CS, Gloria VI, Daez ML, Guerrant RL: Laboratory diagnosis and susceptibility profile of Helicobacter pylori infection in the Philippines. Ann Clin Microbiol Antimicrob. 2004, 3: 25-10.1186/1476-0711-3-25.
Tokudome S, Samsuria Soeripto WD, Triningsih FX, Suzuki S, Hosono A, Triono T, Sarjadi IW, Miranti IP, Ghadimi R, Moore MA:Helicobacter pylori infection appears essential for stomach carcinogenesis: observations in Semarang, Indonesia. Cancer Sci. 2005, 96: 873-875. 10.1111/j.1349-7006.2005.00122.x.
Tokudome S, Soeripto , Triningsih FX, Ananta I, Suzuki S, Kuriki K, Akasaka S, Kosaka H, Ishikawa H, Azuma T, Moore MA: Rare Helicobacter pylori infection as a factor for the very low stomach cancer incidence in Yogyakarta, Indonesia. Cancer Lett. 2005, 219: 57-61. 10.1016/j.canlet.2004.09.043.
Zhao Y, Wang J, Tanaka T, Hosono A, Ando R, Soeripto S, Ediati Triningsih FX, Triono T, Sumoharjo S, Astuti EY, Gunawan S, Tokudome S: Association between HLA-DQ genotypes and haplotypes vs Helicobacter pylori infection in an Indonesian population. Asian Pac J Cancer Prev. 2012, 13: 1247-1251. 10.7314/APJCP.2012.13.4.1247.
Syam AF, Rani AA, Abdullah M, Manan C, Makmun D, Simadibrata M, Djojoningrat D, Sato T: Accuracy of Helicobacter pylori stool antigen for the detection of Helicobacter pylori infection in dyspeptic patients. World J Gastroenterol. 2005, 11: 386-388.
Syam AF, Abdullah M, Rani AA, Nurdjanah S, Adi P, Djumhana A, Tarigan P, Wibawa ID: Evaluation of the use of rapid urease test: pronto dry to detect H pylori in patients with dyspepsia in several cities in Indonesia. World J Gastroenterol. 2006, 12: 6216-6218.
Saragih JB, Akbar N, Syam AF, Sirait S, Himawan S, Soetjahyo E: Incidence of helicobacter pylori infection and gastric cancer: an 8-year hospital based study. Acta Med Indones. 2007, 39: 79-81.
Aulia D, Manz GO, Simadibrata M: Pepsinogen I concentration in organic dyspepsia patients at Gastroenterology Division, Department of Internal Medicine, Cipto Mangunkusumo Hospital. Acta Med Indones. 2009, 41: 107-114.
Miftahussurur M, Shiota S, Suzuki R, Matsuda M, Uchida T, Kido Y, Kawamoto F, Maimunah U, Adi P, Rezkitha Y, Nasronudin ?, Nusi I, Yamaoka Y: Identification of Helicobacter pylori infection in symptomatic patients in Surabaya, Indonesia, using five diagnostic tests. Epidemiol Infect. 2014, ?: 1-11. 10.1017/S095026881400154X. [Epub ahead of print]
Falush D, Wirth T, Linz B, Pritchard JK, Stephens M, Kidd M, Blaser MJ, Graham DY, Vacher S, Perez-Perez GI, Yamaoka Y, Mégraud F, Otto K, Reichard U, Katzowitsch E, Wang X, Achtman M, Suerbaum S: Traces of human migrations in Helicobacter pylori populations. Science. 2003, 299: 1582-1585. 10.1126/science.1080857.
Linz B, Balloux F, Moodley Y, Manica A, Liu H, Roumagnac P, Falush D, Stamer C, Prugnolle F, van der Merwe SW, Yamaoka Y, Graham DY, Perez-Trallero E, Wadstrom T, Suerbaum S, Achtman M: An African origin for the intimate association between humans and Helicobacter pylori. Nature. 2007, 445: 915-918. 10.1038/nature05562.
Yamaoka Y:Helicobacter pylori typing as a tool for tracking human migration. Clin Microbiol Infect. 2009, 15: 829-834. 10.1111/j.1469-0691.2009.02967.x.
Yamaoka Y: Mechanisms of disease: Helicobacter pylori virulence factors. Nat Rev Gastroenterol Hepatol. 2010, 7: 629-641.
Perger R: Did the genus Parandrocephalus Heller, 1916 (Coleoptera, Cerambycidae, Callichromatini) cross the Wallace line? The taxonomic status of Parandrocephalus blairi Bentanachs & Vives 2009 and a new subgenus of Hexamitodera Heller, 1896, with notes on convergent evolution and secondary sexual characters. Zookeys. 2013, 293: 77-89. 10.3897/zookeys.293.5133.
Wigboldus JS: A History of the Minahasa c. 1615-1680. Archipel. 1987, 34: 63-101. 10.3406/arch.1987.2374.
Moodley Y, Linz B, Yamaoka Y, Windsor HM, Breurec S, Wu JY, Maady A, Bernhöft S, Thiberge JM, Phuanukoonnon S, Jobb G, Siba P, Graham DY, Marshall BJ, Achtman M: The peopling of the Pacific from a bacterial perspective. Science. 2009, 323: 527-530. 10.1126/science.1166083.
Dabiri H, Bolfion M, Mirsalehian A, Rezadehbashi M, Jafari F, Shokrzadeh L, Sahebekhtiari N, Zojaji H, Yamaoka Y, Mirsattari D, Zali MR: Analysis of Helicobacter pylori genotypes in Afghani and Iranian isolates. Pol J Microbiol. 2010, 59: 61-66.
Goh KL, Chan WK, Shiota S, Yamaoka Y: Epidemiology of Helicobacter pylori infection and public health implications. Helicobacter. 2011, 16 (Suppl 1): 1-9. 10.1111/j.1523-5378.2011.00874.x.
Okuda M, Kamiya S, Booka M, Kikuchi S, Osaki T, Hiwatani T, Maekawa K, Fukuda Y: Diagnostic accuracy of urine-based kits for detection of Helicobacter pylori antibody in children. Pediatr Int. 2013, 55: 337-341. 10.1111/ped.12057.
Blaser MJ:Helicobacter pylori and gastric diseases. BMJ. 1998, 316: 1507-1510. 10.1136/bmj.316.7143.1507.
Malaty HM, Kumagai T, Tanaka E, Ota H, Kiyosawa K, Graham DY, Katsuyama T: Evidence from a nine-year birth cohort study in Japan of transmission pathways of Helicobacter pylori infection. J Clin Microbiol. 2000, 38: 1971-1973.
Hatin WI, Nur-Shafawati AR, Zahri MK, Xu S, Jin L, Tan SG, Rizman-Idid M, Zilfalil BA, Consortium HP-AS: Population genetic structure of peninsular Malaysia Malay sub-ethnic groups. PLoS One. 2011, 6: e18312-10.1371/journal.pone.0018312.
Chen HL, Chen MJ, Shih SC, Wang HY, Lin IT, Bair MJ: Socioeconomic status, personal habits, and prevalence of Helicobacter pylori infection in the inhabitants of Lanyu. J Formos Med Assoc. 2014, 113: 278-283. 10.1016/j.jfma.2013.11.013.
Cortes MC, Yamakawa A, Casingal CR, Fajardo LS, Juan ML, De Guzman BB, Bondoc EM, Mahachai V, Yamazaki Y, Yoshida M, Kutsumi H, Natividad FF, Azuma T: Diversity of the cagA gene of Helicobacter pylori strains from patients with gastroduodenal diseases in the Philippines. FEMS Immunol Med Microbiol. 2010, 60: 90-97. 10.1111/j.1574-695X.2010.00722.x.
Graham DY, Kudo M, Reddy R, Opekun AR: Practical rapid, minimally invasive, reliable nonendoscopic method to obtain Helicobacter pylori for culture. Helicobacter. 2005, 10: 1-3. 10.1111/j.1523-5378.2005.00285.x.
Graham DY, Reddy S: Rapid detection of anti-Helicobacter pylori IgG in urine using immunochromatography. Aliment Pharmacol Ther. 2001, 15: 699-702. 10.1046/j.1365-2036.2001.00968.x.
Nguyen LT, Uchida T, Tsukamoto Y, Trinh TD, Ta L, Ho DQ, Matsuhisa T, Uchida M, Takayama A, Hijiya N, Okimoto T, Kodama M, Murakami K, Fujioka T, Moriyama M: Evaluation of rapid urine test for the detection of Helicobacter pylori infection in the Vietnamese population. Dig Dis Sci. 2010, 55: 89-93. 10.1007/s10620-009-0720-9.
Han SW, Flamm R, Hachem CY, Kim HY, Clarridge JE, Evans DG, Beyer J, Drnec J, Graham DY: Transport and storage of Helicobacter pylori from gastric mucosal biopsies and clinical isolates. Eur J Clin Microbiol Infect Dis. 1995, 14: 349-352. 10.1007/BF02116531.
Yamaoka Y, Kodama T, Kita M, Imanishi J, Kashima K, Graham DY: Relationship of vacA genotypes of Helicobacter pylori to cagA status, cytotoxin production, and clinical outcome. Helicobacter. 1998, 3: 241-253. 10.1046/j.1523-5378.1998.08056.x.
Matsunari O, Shiota S, Suzuki R, Watada M, Kinjo N, Murakami K, Fujioka T, Kinjo F, Yamaoka Y: Association between Helicobacter pylori virulence factors and gastroduodenal diseases in Okinawa, Japan. J Clin Microbiol. 2012, 50: 876-883. 10.1128/JCM.05562-11.
Takahashi A, Shiota S, Matsunari O, Watada M, Suzuki R, Nakachi S, Kinjo N, Kinjo F, Yamaoka Y: Intact long-type dupA as a marker for gastroduodenal diseases in Okinawan subpopulation, Japan. Helicobacter. 2013, 18: 66-72. 10.1111/j.1523-5378.2012.00994.x.
Atherton JC, Cao P, Peek RM, Tummuru MK, Blaser MJ, Cover TL: Mosaicism in vacuolating cytotoxin alleles of Helicobacter pylori. Association of specific vacA types with cytotoxin production and peptic ulceration. J Biol Chem. 1995, 270: 17771-17777. 10.1074/jbc.270.30.17771.
Yamaoka Y, Kodama T, Gutierrez O, Kim JG, Kashima K, Graham DY: Relationship between Helicobacter pylori iceA, cagA, and vacA status and clinical outcome: studies in four different countries. J Clin Microbiol. 1999, 37: 2274-2279.
Yamaoka Y, El-Zimaity HM, Gutierrez O, Figura N, Kim JG, Kodama T, Kashima K, Graham DY, Kim JK: Relationship between the cagA 3? repeat region of Helicobacter pylori, gastric histology, and susceptibility to low pH. Gastroenterology. 1999, 117: 342-349. 10.1053/gast.1999.0029900342.
Yamaoka Y, Kikuchi S, el-Zimaity HM, Gutierrez O, Osato MS, Graham DY: Importance of Helicobacter pylori oipA in clinical presentation, gastric inflammation, and mucosal interleukin 8 production. Gastroenterology. 2002, 123: 414-424. 10.1053/gast.2002.34781.
Kumar S, Nei M, Dudley J, Tamura K: MEGA: a biologist-centric software for evolutionary analysis of DNA and protein sequences. Brief Bioinform. 2008, 9: 299-306. 10.1093/bib/bbn017.
Tamura K, Dudley J, Nei M, Kumar S: MEGA4: Molecular Evolutionary Genetics Analysis (MEGA) software version 4.0. Mol Biol Evol. 2007, 24: 1596-1599. 10.1093/molbev/msm092.
Acknowledgements
This report is based on work supported in part by grants from the National Institutes of Health (DK62813) (YY) and Grants-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology (MEXT) of Japan (22390085, 22659087, 24406015, 24659200, 25293104 and 26640114) (YY). This work was also supported by the Japan Society for the Promotion of Science (JSPS) Institutional Program for Young Researcher Overseas Visits (YY) and the Strategic Funds for the Promotion of Science and Technology from Japan Science and Technology Agency (JST) (YY) as well as MEXT KAKENHI (221S0002) (YY). MM (Muhammad Miftahussurur) is a PhD student supported by The Japanese Government (Monbukagakusho: MEXT) Scholarship Program for 2012.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Miftahussurur, M., Tuda, J., Suzuki, R. et al. Extremely low Helicobacter pylori prevalence in North Sulawesi, Indonesia and identification of a Maori-tribe type strain: a cross sectional study. Gut Pathog 6, 42 (2014). https://doi.org/10.1186/s13099-014-0042-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13099-014-0042-0