Abstract
Background
Hypoglycemia is a barrier to optimal glucose control in the treatment of both type 1 (T1DM) and type 2 diabetes mellitus (T2DM). Blood glucose monitoring is essential in diabetes management. Inappropriate glucose management is associated with high mortality and morbidity. FreeStyle Libre® (FSL) is a continuous glucose monitoring (CGM) system that provides effective, safe, and convenient glucose monitoring, without routine finger pricking. This study aims to estimate the incremental cost-effectiveness ratio (ICER) of the FSL system in comparison to conventional Self-monitoring of blood glucose (SMBG) in T1DM and T2DM patients that require intensive insulin therapy.
Methods
A decision-tree model was developed to compare the cost-effectiveness ratio between FSL and conventional SMBG from the perspective of the Brazilian Public Healthcare System (SUS). The model captures the cumulative rates of acute complications such as severe hypoglicemia and diabetic ketoacidosis, per-event costs, and quality-adjusted life-years (QALYs) gained over a 1-year time horizon in adult and pediatric patients (≥ 4 years old) with T1DM or T2DM. Inputs from the Brazilian health databases, clinical trials, and real-world data were used in the study.
Results
The results demonstrated that, regarding solely severe hypoglicemia and diabetic ketoacidosis events, T1DM have a QALY difference of 0.276, a cost difference of R$ 7.255, and an ICER of R$ 26,267.69 per QALY gained for CGM with FSL, when compared to conventional SMBG. T2DM results demonstrated equally a QALY difference of 0.184, a cost difference of R$ 7290, and an ICER of R$ 39,692.67 per QALY gained, in favour of CGM with FSL.
Conclusion
Our findings demonstrated that FSL is cost-effective in T1DM and T2DM for acute diabetic complications, from a SUS perspective. CGM with FSL can promote safe, convenient, and cost-effective glucose monitoring, therefore contributing to the improvement of the incidence of complications and quality of life.
Similar content being viewed by others
Background
Hypoglycemia is a major side effect of some glucose-lowering therapies, in particular, insulin and the insulin secretagogues [1]. The risk of hypoglycemia is a barrier to the optimal glucose control in the treatment of both type 1 (T1DM) and type 2 diabetes mellitus (T2DM), especially in the context of insulin therapy [2]. In the past years, self-monitoring of blood glucose (SMBG) was the main resource to monitor blood glucose. Nonetheless, SMBG is associated with psychological, economic, and social burdens [3, 4]. The monitoring routine is probably the main reason for that, as it requires several finger punctures per day. The frequent and painful SMBG routine might negatively impact the patient’s quality of life and treatment adherence. Although blood glucose monitoring is essential in diabetes mellitus (DM) management, several patients struggle to follow national recommendations (three or four times a day) [5]. SMBG adherence rate may vary between 13.0 and 79.9% in T2DM individuals from low- and middle-income countries [6]. Without the appropriate glucose management, T1DM and T2DM patients may suffer acute and chronic complications, such as hypoglycemia, diabetic ketoacidosis, cardiovascular, ocular, renal, and neurological impairments. Optimized glycemic control is fundamental to minimizing DM mortality and morbidity [7].
FreeStyle Libre (FSL) is a continuous flash glucose monitoring system that provides effective, safe, and convenient glucose monitoring, without routine finger pricking [8,9,10]. FSL comprises a small, round, disposable, and water-resistant dwelling sensor applied to the back of the arm and changed at 14-day intervals. FSL records interstitial glucose levels every 15 min, which are fed into an app which plots an Ambulatory Glucose Profile, trends of glucose increase or decrease, and other glucose control metrics such as Time in Range, Glucose Variability, Hipoglycemic Episodes, Estimated HbA1c, etc. The sensor does not require daily calibration and can be used by both T1DM and T2DM [11,12,13,14,15].
Currently, Canada and the United Kingdom reimburse FSL for some conditions. The Canadian Agency for Drugs and Technologies in Health (CADTH) recommends FSL reimbursement for T1DM and T2DM patients requiring multiple daily insulins injections and experiencing recurrent hypoglycemia, despite frequent SMBG and efforts to optimize insulin management [16]. The British National Institute of Health and Care Excellence (NICE) recommends reimbursement of FSL for young and adult T1DM patients and for patients with T2DM who use intensive insulin therapy and experience recurrent or severe hypoglycemia [17,18,19].
To date, FSL is the only continuous flash glucose monitoring device approved in Brazil. It is indicated for people older than 4 years of age with DM, being a substitute for SMBG. Although Brazilian hypoglycemia rates are one of the highest in the world [7], FSL is far from universal availability in the Brazilian Public Healthcare System (SUS). Results from the Hypoglycemia Assessment Tool (HAT) study found that 91.7% of T1DM and 61.8% of T2DM Brazilian patients had at least one hypoglycemic event during the 4 weeks after the start of the follow-up study. These rates were higher than those reported in the global HAT study (83.0% for T1DM and 46.5% for T2DM) and in the Latin-American studies (87.4% in T1DM and 43.8% in T2DM) [7]. The high incidence rates of hypoglycemia in Brazil reinforce the importance of optimizing glucose monitoring and patient access to new, safe and innovative glucose-monitoring technologies.
Given this context, the present study aims to estimate the incremental cost-effectiveness ratio (ICER) of the FSL system in comparison to SMBG in T1DM and T2DM patients that require intensive insulin therapy.
Methods
Overall characteristics of the economic model
An economic model was developed in Microsoft Excel comparing FSL with SMBG—the currently standard of care available in SUS. A decision-tree model was developed from a SUS perspective. Inputs from the Brazilian Health Databases, clinical trials, and real-world data were used in the study. The model captures the cumulative rates of acute clinical events (hypoglycemia and diabetic ketoacidosis), per-event costs, and quality-adjusted life-years (QALYs) gained over a 1-year time horizon in adult and pediatric patients (≥ 4 years old) diagnosed with T1DM or T2DM currently treated with intensive insulin therapy.
The present analysis was carried out from the SUS perspective, evaluating the direct medical costs related to the treatment of patients, such as devices and supplies and hospital care. This 1-year time horizon was chosen considering the 6-month follow-up period of the pivotal studies and the outcomes under analysis. Due to the time horizon adopted, no discount rate was applied according to the Brazilian Ministry of Health guideline for health economic studies [20].
Two identical decision trees were developed, one for each type of DM, in which patients using FSL or SMBG may experience hypoglycemia or be hospitalized for ketoacidosis or have no events (Fig. 1).
In the analysis we assumed that the average decrease in 24-h hypoglycemia event rates would be constant when evaluated during longer time horizons. Therefore, the relative decrease in the yearly hypoglycemia event rate was applied only once. We also assumed that hypoglycemia and ketoacidosis event rates were constant over the time horizon, and that the results of pivotal studies conducted in patients aged 18 or more years were extensible to younger patients (4–17 years old).
Results are presented as ICER and net monetary benefit (NMB), weighted by the proportion of T1DM and T2DM insulin users in Brazil. ICER is calculated by dividing the difference in total costs by the difference in measures of health outcome (QALY) [21]. NMB is calculated as the benefit of a therapy expressed in monetary terms net of all costs [22]. The effect of uncertainty on ICER was accessed through deterministic and probabilistic sensitivity analyses (PSA). Deterministic sensitivity analyses (DSA) were carried out to assess the impact of model inputs and assumptions on the results, by varying the parameters one at a time to the lower or upper boundary values. Those values were obtained using a 95% confidence interval variation or, if it was unavailable, a 20% variation. PSA evaluated the impact of uncertainty by simultaneously varying cost, utility, and treatment effect parameters as random values within the interval between the lower and upper boundaries of the variables on the results. Parameters varied in DSA and PSA are shown in Tables 1, 2, 3, 4 and 5. All analyses were run with 1000 individuals for 1000 iterations.
Model inputs
Use of self-monitoring of blood glucose
The Brazilian Ministry of Health T1DM guidelines recommends SMBG three or four times a day (mean 3.5; lower bound 3; upper bound 4) [23]. Although SMBG is recommended for T2DM patients using insulin, there is no recommended number of measurements per day [5]. For this study, we assume the same recommendations for T1DM and T2DM.
The use of SMBG in patients using FSL may occur when symptoms do not match flash glucose monitoring system readings. As such the number of daily SMBG with FSL for T1DM was assumed to be 0.5 according to the study by Bolinder et al. [24] (lower bound 0.37, upper bound 0.63) and for T2DM was assumed to be 0.3 according to the study by Haak et al. [25] (lower bound 0.12, upper bound 0.48).
Hypoglycemia events
To consider the potential effect of FSL in the occurrence of severe hypoglycemia, we applied the changes from baseline events of glucose levels < 2.5 mmol/L (45 mg/dL) within 24 h for FSL from the pivotal studies to the incidence of severe hypoglycemia captured in the HAT study with Brazilian T1DM and T2DM patients [7]. Accordingly, the same approach was undertaken to events of glucose levels < 3.9 mmol/L (70 mg/dL) within 24 h, in which the differences observed from baseline with FSL in the pivotal studies were applied to the incidence of non-severe hypoglycemia events captured in the HAT study [7] (Table 2). This approach was also used by other authors [26], and is consistent with the relationship between the occurrence of biochemical hypoglycemia and the occurrence of severe hypoglycemia [27]. Beck et al. [29] found that the risk of severe hypoglycemia in a 3-month period was higher when there was at least one identified biochemical hypoglycemia event (< 70.0 mg/dL or < 5.4 mg/dL) in the Diabetes Control and Complications Trial (DCCT) data set [27].
The HAT study was an observational study developed to explore the hypoglycemia incidence and awareness among insulin treated patients in Brazil. It included 321 T1DM and 293 T2DM, with median time of insulin use of 14.0 and 6.0 years, respectively. The study captured the incidence of severe and non-severe hypoglycemia, the frequency of nocturnal events, and that of hospitalization-requiring events [7].
Ketoacidosis
The effect of FSL in the incidence of hospitalizations due to ketoacidosis was evaluated in a French study. Roussel et al. [28] used a nationwide database of reimbursement claims to estimate ketoacidosis rates (ICD-10 codes E10.1) in the year before the initiation of FSL and in the first year of the device use. The yearly ketoacidosis rates were reduced by 52% and by 47% after FSL initiation for T1DM and T2DM, respectively [28] (Table 3).
Utility
Baseline utilities for T1DM and T2DM were extracted from the study by Bahia et al. [29] and considered equal at baseline. This multicenter study evaluated the quality of life and calculated the utility values associated with hypoglycemia in patients with T1DM treated in the SUS [29]. The disutility for severe and non-severe hypoglycemia events were used for glucose level < 2.5 mmol/L (45 mg/dL) events and glucose level < 3.9 mmol/L (70 mg/dL) events, respectively. A regression equation proposed by Laurisden et al. [30] was used to adjust the disutility of hypoglycemic events, lowering the utility as frequency increases (Table 4).
Matza et al. [31] estimated the utility related to FSL use in comparison to SMBG. They interviewed 209 individuals from Edinburgh and London (United Kingdom) using the time trade-off method. The difference of 0.030 between the utilities given to both health states, FSL and SMBG, was applied to the model as the utility associated with FSL use for both T1DM and T2DM [31] (Table 4).
Costs
The costs associated with SMBG included the provision of a glucometer (one-off cost), disposable lancets, and reagent strips. The costs of these resources were extracted from the SUS public health price panel (BPS—Banco de Preços em Saúde), by calculating the weighted average public purchases carried out for the period of competence from January to December 2022. The costs of FSL comprised one reader (1st purchase, one-off cost), and the sensors, replaced at 14-day periods.
The median cost of hospitalization for ketoacidosis was derived from the SUS Hospitalization Information System (SIH/SUS). Public data was extracted from SUS Department of Informatics (DATASUS—Departamento de Informática do Sistema Único de Saúde) for the period of competence from January to December 2022, using ketoacidosis ICD-10 codes (E10.1; E13.1 or E14.1) and the reimbursement claims codes from SUS Procedures, Medicines, Orthotics, Prostheses and Special Materials Management System (SIGTAP) for treatment of metabolic disorders (03.03.03.004-6); or treatment of diabetes mellitus (03.03.03.003-8); or pediatric intensive care unit (ICU) level I (day cost; 08.02.01.014-8); or pediatric ICU level II (day cost, 08.02.01.015-6); or pediatric ICU level III (day cost; 08.02.01.007-5); or adult ICU level I (day cost, 08.02.01.010-5); or adult ICU level II (day cost, 08.02.01.008-3); or adult ICU level III (day cost, 08.02.01.009-1) (Table 5). The higher the level of the ICU, the higher the medical resources used and the higher the costs.
The median cost of hospitalization due severe hypoglycemia was derived from SIH/SUS using hypoglycemia ICD-10 codes (E16.0; E16.1; or E16.2) and SIGTAP claim codes. In the HAT study, 5.2% of T1DM and 3.3% of T2DM patients reported hospitalization due to hypoglycemia. These figures were used to weight the cost of severe hypoglycemia [7] (Table 5). The widely accepted definition of severe hypoglycemia in the guidelines refers to episodes of hypoglycemia that require assistance from another person [5, 34]. In this sense and considering that this action does not imply costs from the SUS perspective, only hospitalization costs were considered in the analysis. This assumption lead to an underestimation of the incidence of sever hypoglycemia events that often do not reach the hospital We also assumed that non-severe hypoglycemia events incurred with zero cost to the SUS.
Results
Over a 1-year horizon, treatment with FSL combined with sporadic SMBG presented a positive outlook for T1DM and T2DM, compared with SMBG alone. The T1DM scenario showed a QALY difference of 0.276, a R$ 7.255 cost difference, and an ICER of R$ 26,267.69 per QALY gained. In comparison, the T2DM results demonstrated a QALY difference of 0.184, a R$ 7290 cost difference, and an ICER of R$ 39,692.67 per QALY gained. The complete results are available in Table 6.
As for DSA, basal event-rates of severe hypoglycemia per patient-years, disutility of severe daytime hypoglycemic events and events of glucose < 2.5 mmol/L (45 mg/dL) within 24h per patient-years with FreeStyle Libre were the most sensitive parameters to impact results in both T1DM (Figs. 2, 3) and T2DM populations (Figs. 4, 5).
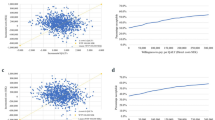
In 1000 simulations PSA-wise analysis, 64.4% and 58% of the points resulting from T1DM and T2DM, respectively, remain above the willingness-to-pay threshold line of R$ 40,000/QALY in the scatter plot. However, 35.6% of the points from the T1DM and 42% from T2DM analyses remain below thew willingness-to-pay threshold line (Figs. 6, 7).
The cost-effectiveness acceptability curves for T1DM and T2DM are presented in Figs. 8 and 9.
Discussion
Hypoglycemia affects glycemic control and safety during insulin treatment of both T1DM and T2DM populations [7]. Hypoglycemia is associated with increased morbidity and mortality [7, 39]. Its manifestations within different glucose ranges vary from asymptomatic to severe symptoms of neurological and cardiovascular dysfunction, such as dizziness, confusion, weakness, anxiety, fear, disrupted sleep, cardiac arrythmias and ischemia, convulsions, cognitive disorders, coma and even death [7, 39]. Hypoglycemia has a significant burden on healthcare resources, due to the direct costs of its treatment and the indirect costs of lost productivity, in addition to a great impact on the quality of life of patients and their families [1]. Lamounier et al. [7] estimated that hypoglycemic episodes represented an yearly cost to SUS of R$709 per T1DM patient [range R$0–R$12,364 (mean direct costs: R$640; mean indirect costs: R$69)] and of R$396 per T2DM patient [range R$0–R$10,431 (mean direct costs: R$390; mean indirect costs: R$6)]. Hospitalizations was the main cost driver [7, 40].
Even though pharmacotherapeutic advances have increased in recent years, a significant proportion of patients are still unable to control their blood glucose levels within the recommended limits [39]. Current monitoring based on SMBG has significant limitations, especially regarding low patient adherence to the recommendations established by national and international scientific societies [39].
The FreeStyle Libre system enables patients to measure their glucose levels in the interstitial fluid without routinely pricking their fingers. Also, it reduces the number of steps required to monitor glucose levels, compared to the traditional SMBG approach. This new technology is associated with several outcome benefits. A meta-analysis conducted by Gordon et al. [41] demonstrated a mean HbA1c reduction in T1DM patients of 4.5 mmol/mol (2.6%) [95% CI 3.3–5.6 mmol/mol (2.5–2.7%)] [41]. Dicembrini et al. [42] also reported that FSL is related to an improvement in quality of life and a lower incidence of hypoglycemic events in T2DM patients.
Optimized glycemic control is fundamental to minimizing morbidity. Poor glycemic control in diabetes is associated with serious complications such as sight-threatening retinopathy and renal failure. The most expensive aspect of treating severe hypoglycemia is hospital admission and inpatient care [1]. Oyagüez et al. [39] developed a model to estimate the annual savings with FSL compared with SMBG in the Spanish health system. The results indicate that FSL utilization would reduce 43.1% of the total annual cost per patient. Reduction of severe hypoglycemia was the main contributing parameter for the estimated cost savings [39]. Cost savings were equally observed in the United Kingdom; an annual saving of £234.28 per T1DM patient was reported with FSL use [26]. These data must probably have been of paramount importance to the recent recommendation from the United Kingdom National Health System of continuous glucose monitoring for all T1DM patients [43].
Our analysis was conducted from a SUS perspective. For T1DM patients, it is estimated an ICER of R$ 26,267.69 per QALY. For the T2DM scenario, the ICER was estimated at R$
39,692.67 per QALY. In 2022, the National Committee for Technology Implementation in the Public Health System (CONITEC) established an ICER threshold for reimbursement decisions [44]. The guideline defines that the standard value for most diseases should not overpass one Gross Domestic Product per capita/QALY (R$ 40,000.00/QALY). In other scenarios involving ultrarare diseases or advanced technologies, ICER value can overtake up to three times the reference value [44]. Therefore, both T1DM (R$ 26,267.69) and T2DM (R$ 39,692.67) ICER values would be under the threshold defined by CONITEC.
The impact of uncertainty on ICER was assessed using DSA and PSA. The DSA results were presented in the form of a “tornado chart”, with parameters ordered based on to the extent of the uncertainty variation [45]. The analysis revealed that the ICER was primarily influenced by two key variables: the basal events of severe hypoglycemia per patient-year and disutility of severe nocturnal hypoglycemic event. While both parameters exhibited a larger degree of uncertainty in comparison to the others, it is noteworthy that these critical variables were derived from national epidemiological studies, thereby enhancing the robustness of the dataset. Furthermore, the variation of parameters related to ketoacidosis were not among the most influential in the ICER (data not shown in the manuscript).
Implementation particularities for FSL may exist. Two elements seem to be operational in this regard: one is the sensor reader, a one-off cost item. However, many users do not buy the FSL reader today. The company has developed a mobile application (LibreView®) that enables users to read the sensor through cell phones with “Near Field Communication” (NFC) capacity. The NFC technology enables communication between two electronic devices, allowing such features as identification of documents, contactless payment, and scanning FSL sensors. Although NFC is a relatively recent set of communication in mobile phones, there are nowadays more than two billion NFC-enabled devices worldwide. In the long run, NFC technology is expected to be available in most cell phone devices [46]. Therefore, this one-off, significant cost may not be necessary for several patients, which might bring a reduction in the overall cost. The other element is the sensor itself, which must be replaced at 14-day periods. This may bring forth concerns about the system-related annual cost. Nonetheless, the reduction in hypoglycemic episodes and in the need for SMBG supplies with FSL use results in lesser consumption of healthcare resources [25]. Therefore, the overall cost of FSL system might translate into a better control of the disease and a reduction in the consumption of other supplies.
There are some limitations to our model. The first one is related to the ketoacidosis rate, which was based on the French data and may not reflect the Brazilian incidence. The second is related to the time horizon of the analysis, which was of 1 year, despite DM being a chronic disease. We chose to estimate the cost-effectiveness of glucose monitoring with FSL over a 1-year time horizon based on the results of FSL clinical trials in T1DM and T2DM groups. The third limitation is associated with subgroup analyses: results obtained from adult participants were extended to children and adolescents. Therefore, the data might not entirely reflect the other subgroup scenarios.
Conclusions
The current study pioneers the development of an economic model to estimate the implementation of FSL for T1DM and T2DM patients from the SUS perspective. The results demonstrated that ICER values for T1DM and T2DM patients are under the threshold defined by the Brazilian Committee for Technology Implementation in 2022. FSL's innovative technology can promote safe, convenient, and cost-effective glucose monitoring and therefore contributing to the improvement of the incidence of complications and quality of life for the millions of people living with diabetes in Brazil, with many thousands of children and adolescents among them.
Availability of data and materials
Not applicable.
Abbreviations
- BPS:
-
SUS Public Health Price Panel (Banco de Preços em Saúde)
- CADTH:
-
The Canadian Agency for Drugs and Technologies in Health
- CONITEC:
-
Brazilian National Committee for Technology Implementation in the Public Health System
- DATASUS:
-
SUS Department of Informatics (Departamento de Informática do Sistema Único de Saúde)
- DCCT:
-
Diabetes Control and Complications Trial
- DM:
-
Diabetes Mellitus
- DSA:
-
Deterministic sensitivity analyses
- FSL:
-
FreeStyle Libre
- HAT:
-
Hypoglycemia Assessment Tool
- ICER:
-
Incremental Cost-Effectiveness Ratio
- ICU:
-
Intensive Care Unit
- NFC:
-
Near Field Communication
- NICE:
-
British National Institute of Health and Care Excellence
- NMB:
-
Net Monetary Benefit
- PSA:
-
Probabilistic Sensitivity Analyses
- QALY:
-
Quality-Adjusted Life-Years
- SIGTAP:
-
SUS Procedures, Medicines, Orthotics, Prostheses and Special Materials Management System (Sistema de Gerenciamento da Tabela de Procedimentos, Medicamentos e OPM do SUS)
- SIH/SUS:
-
SUS Hospitalization Information System (Sistema de Informação Hospital)
- SMBG:
-
Self-Monitoring of Blood Glucose
- SUS:
-
Brazilian Public Healthcare System (Sistema Único de Saúde)
- T1DM:
-
Type 1 Diabetes mellitus
- T2DM:
-
Type 2 Diabetes mellitus
- WTP:
-
Willingness-To-Pay
References
Heller SR, Frier BM, Hersløv ML, Gundgaard J, Gough SCL. Severe hypoglycaemia in adults with insulin-treated diabetes: impact on healthcare resources. Diabet Med (Internet). 2016;33(4):471–7. https://doi.org/10.1111/dme.12844.
Kunt T, Snoek FJ. Barriers to insulin initiation and intensification and how to overcome them. Int J Clin Pract (Internet). 2009;63:6–10. https://doi.org/10.1111/j.1742-1241.2009.02176.x.
Hortensius J, Kleefstra N, Houweling ST, van der Bijl JJ, Gans RO, Bilo HJ. What do professionals recommend regarding the frequency of self-monitoring of blood glucose? Neth J Med. 2012;70(6):287–91.
Knapp S, Manroa P, Doshi K. Self-monitoring of blood glucose: advice for providers and patients. Cleve Clin J Med. 2016;83(5):355–60.
da Brasil MS. Protocolo Clínico e Diretrizes Terapêuticas do Diabete Melito Tipo 2; 2020.
Mogre V, Johnson NA, Tzelepis F, Shaw JE, Paul C. A systematic review of adherence to diabetes self-care behaviours: evidence from low- and middle-income countries. J Adv Nurs. 2019;75(12):3374–89.
Lamounier RNN, Geloneze B, Leite SOO, Montenegro R, Zajdenverg L, Fernandes M, et al. Hypoglycemia incidence and awareness among insulin-treated patients with diabetes: the HAT study in Brazil. Diabetol Metab Syndr (Internet). 2018;10(1):83. https://doi.org/10.1186/s13098-018-0379-5.
FreeStyle Libre—Sistema Flash de Monitoramento de Glicose. Disponível em: <https://www.freestylelibre.com.br/index.html>. Acesso em 13 de maio de 2020. 2020.
Unger J, Kushner P, Anderson JE. Practical guidance for using the FreeStyle Libre flash continuous glucose monitoring in primary care. Postgr Med. 2020;2020:1.
Stone JY, Bailey TS. Benefits and limitations of continuous glucose monitoring in type 1 diabetes. Expert Rev Endocrinol Metab. 2020;15(1):41–9.
Palylyk-Colwell E, Ford C. Flash glucose monitoring system for diabetes. CADTH Issues Emerg Health Technol. 2016;2016:1.
Mancini G, Berioli MG, Santi E, Rogari F, Toni G, Tascini G, et al. Flash glucose monitoring: a review of the literature with a special focus on type 1 diabetes. Nutrients. 2018;10(8):1.
Chico A, Aguilera E, Ampudia-Blasco FJ, Bellido V, Cardona-Hernandez R, Escalada FJ, et al. Clinical Approach to flash glucose monitoring: an expert recommendation. BMC Endocr Disord. 2020;14(1):155–64.
Leelarathna L, Wilmot EG. Flash forward: a review of flash glucose monitoring. Diabet Med. 2018;35(4):472–82.
Borot S, Benhamou PY, Atlan C, Bismuth E, Bonnemaison E, Catargi B, et al. Practical implementation, education and interpretation guidelines for continuous glucose monitoring: a French position statement. Diabetes Metab. 2018;44(1):61–72.
CADTH. Flash glucose monitoring system FreeStyle Libre to monitor glycemia in patients with diabetes; 2020. p. undefined-51.
Poole R. Diagnosis and management of type 1 diabetes in adults. Practitioner. 1861;2022(266):23–6.
NICE Guidelines. Recommendations | Diabetes (type 1 and type 2) in children and young people: diagnosis and management | Guidance | NICE. NICE Guidel. 2022(June):1–68.
Martyn A. Type 2 diabetes in adults. Nurs Stand. 2006;20(30):67.
Ministério da Saúde (Brasil). Secretaria de Ciência-Tecnologia e Insumos Estratégicos. Departamento de Ciência e Teccnologia. Diretrizes metodológicas: estudos de avaliação econômica de tecnologias em saúde. 2nd ed. Brasília: Ministério da Saúde; 2014. p. 132.
York Health Economics Consortium. Incremental Cost-Effectiveness Ratio (ICER). 2023; Available from: https://yhec.co.uk/glossary/incremental-cost-effectiveness-ratio-icer/.
Shafrin J, May S, Skornicki M, Hathway J, Macaulay R, Villeneuve J, et al. Use of Net Monetary Benefit Analysis to Comprehensively Understand the Value of Innovative Treatments. Value Heal [Internet]. 2016;19(7):A731. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1098301516335689.
Brasil. Ministério da Saúde. Protocolo Clínico e Diretrizes Terapêuticas de Diabetes Melito Tipo 1. 2019; Available from: https://www.gov.br/conitec/pt-br/midias/protocolos/portaria-conjunta-pcdt-diabete-melito-1.pdf.
Bolinder J, Antuna R, Geelhoed-Duijvestijn P, Kröger J, Weitgasser R. Novel glucose-sensing technology and hypoglycaemia in type 1 diabetes: a multicentre, non-masked, randomised controlled trial. Lancet. 2016;388(10057):2254–63.
Haak T, Hanaire H, Ajjan R, Hermanns N, Riveline J-PP, Rayman G. Flash glucose-sensing technology as a replacement for blood glucose monitoring for the management of insulin-treated type 2 diabetes: a multicenter, open-label randomized controlled trial. Diabetes Ther (Internet). 2017;8(1):55–73. https://doi.org/10.1007/s13300-016-0223-6.
Hellmund R, Weitgasser R, Blissett D. Cost calculation for a flash glucose monitoring system for UK adults with type 1 diabetes mellitus receiving intensive insulin treatment. Diabetes Res Clin Pr. 2018;138:193–200.
Beck RW, Bergenstal RM, Riddlesworth TD, Kollman C. The association of biochemical hypoglycemia with the subsequent risk of a severe hypoglycemic event: analysis of the DCCT data set. Diabetes Technol Ther. 2019;21(1):1–5.
Roussel R, Guerci B, Vicaut E, Depouvourville G, Detournay B, Emery C, et al. 68-OR: dramatic drop in ketoacidosis rate after freestyle libre system initiation in type 1 and type 2 diabetes in france, especially in people with low self-monitoring of blood glucose (SMBG): a nationwide study. Diabetes. 2020;69(Supplement 1):68-OR.
Bahia L, Kupfer R, Momesso D, Cabral DAP, Tschiedel B, Puñales M, et al. Health-related quality of life and utility values associated to hypoglycemia in patients with type 1 diabetes mellitus treated in the Brazilian Public Health System: a multicenter study. Diabetol Metab Syndr. 2017;9(1):9.
Lauridsen JT, Lønborg J, Gundgaard J, Jensen HH. Diminishing marginal disutility of hypoglycaemic events: results from a time trade-off survey in five countries. Qual Life Res Int J Qual Life Asp Treat Care Rehabil. 2014;23(9):2645–50.
Matza LS, Stewart KD, Davies EW, Hellmund R, Polonsky WH, Kerr D. Health state utilities associated with glucose monitoring devices. Value Heal J Int Soc Pharmacoeconomics Outcomes Res. 2017;20(3):507–11.
Evans M, Khunti K, Mamdani M, Galbo-Jørgensen CB, Gundgaard J, Bøgelund M, et al. Health-related quality of life associated with daytime and nocturnal hypoglycaemic events: a time trade-off survey in five countries. Health Qual Life Outcomes. 2013;11:90.
Peasgood T, Brennan A, Mansell P, Elliott J, Basarir H, Kruger J. The impact of diabetes-related complications on preference-based measures of health-related quality of life in adults with type I diabetes. Med Decis Making. 2016;36(8):1020–33.
Sociedade Brasileira de Diabetes (SBD). Diretrizes Sociedade Brasileira de Diabetes 2019–2020. Available on: <https://www.diabetes.org.br/profissionais/images/banners/Diretrizes_SBD_2020_04FEV20.pdf>. 1 Mar 2023; 2020.
Banco de Preços em Saúde. Código do CATMAT: BR0389555; Compras de 2022; 2023.
Banco de Preços em Saúde. Código do CATMAT: BR0339565; Compras de 2022; 2023.
Banco de Preços em Saúde. Código do CATMAT: BR0338605; Compras de 2022; 2023.
BRASIL.Ministério da Saúde. Departamento de Informática do Sistema Único de Saúde (DATASUS); 2022.
Oyagüez I, Merino-Torres JF, Brito M, Bellido V, Cardona-Hernandez R, Gomez-Peralta F, et al. Cost analysis of the flash monitoring system (FreeStyle Libre 2) in adults with type 1 diabetes mellitus. BMJ Open Diabetes Res Care (Internet). 2020;8(1):001330. https://doi.org/10.1136/bmjdrc-2020-001330.
Lamounier R, Ermetice M, Griciunas F, Silva C. Costs of managing hypoglycaemias among insulin-treated patients with diabetes: results from the hat study in Brazil. Value Heal. 2017;20(9):PA920-A921.
Gordon I, Rutherford C, Makarounas-Kirchmann K, Kirchmann M. Meta-analysis of average change in laboratory-measured HbA1c among people with type 1 diabetes mellitus using the 14 day Flash Glucose Monitoring System. Diabetes Res Clin Pract (Internet). 2020 Jun;164:108158. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0168822720304083.
Dicembrini I, Mannucci E, Monami M, Pala L. Impact of technology on glycaemic control in type 2 diabetes: a meta-analysis of randomized trials on continuous glucose monitoring and continuous subcutaneous insulin infusion. Diabetes Obes Metab (Internet). 2019;21(12):2619–25. https://doi.org/10.1111/dom.13845.
NICE. National Institute for Health and Care Excellence. Vol. Published:, NICE guideline. Type 1 diabetes in adults: diagnosis and management; 2022.
Brasil.Ministério da Saúde. O uso de limiared de custo-efetividade nas decisões em saúde: Recomendação da Comissão Nacional de Incorporação de Tecnologias no SUS (Internet); 2022. Available from: https://www.gov.br/conitec/pt-br/midias/pdf/2022/20221106_relatorio-uso-de-limiares-de-custo-efetividade-nas-decisoes-em-saude.pdf.
York Health Economics Consortium. Deterministic Sensitivity Analysis (Internet). 2023. Available from: https://yhec.co.uk/glossary/deterministic-sensitivity-analysis/#:~:text=Deterministic sensitivity analysis (DSA) is parameter or set of parameters.
Staneley H. Near Field Communication: What is NFC & How to Use It. Available from: https://www.shopify.com/retail/near-field-communication.
Acknowledgements
The authors acknowledge the support of the Brazilian Society of Diabetes.
Funding
This study was sponsored by a research grant of the Brazilian Diabetes Society.
Author information
Authors and Affiliations
Contributions
LB, KFM, DAM were responsible for the design of the study and made critical revisions of the manuscripts. LLPL, NLC, EM were responsible for data collection, statistical analysis and drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate:
Not applicable.
Consent for publication
Not applicable.
Competing interests
LLPL, NLC and EM are employees of IQVIA. The remaining authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bahia, L., Mello, K.F., Lemos, L.L.P. et al. Cost-effectiveness of continuous glucose monitoring with FreeStyle Libre® in Brazilian insulin-treated patients with types 1 and 2 diabetes mellitus. Diabetol Metab Syndr 15, 242 (2023). https://doi.org/10.1186/s13098-023-01208-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-023-01208-5