Abstract
Background
Both type 2 diabetes mellitus (T2DM) and frailty are strongly associated with congestive heart failure (CHF). Individuals with T2DM and CHF have a high frailty burden. The association of frailty with HF, all-cause, and cardiovascular mortality in patients with T2DM has not been thoroughly explored.
Methods
This study included 2894 adults with T2DM from the National Health and Nutrition Examination Survey (NHANES) database over ten cycles (1999–2018) and followed up for all-cause and cardiovascular mortality through 31 December 2019. The frailty index (FI) was calculated using a 46-item deficit model to assess frailty status. Weighted multivariable logistic regression was performed to explore the relationship between frailty and CHF in patients with T2DM. Weighted restricted cubic splines were used to evaluate the non-linear relationship between FI and outcome. All-cause mortality and cardiovascular mortality association with FI was assessed using the Kaplan–Meier curve and COX proportional hazards regression accounting for sampling weights. Subgroup and sensitivity analyses were performed to evaluate the robustness of the results.
Results
After the adjustment of essential confounders, a higher frailty index in T2DM was associated with increased odds of CHF (odds ratio [OR] for per 1-SD increase, 2.02, 95% confidence interval [CI] 1.67–2.45; P < 0.0001). The presence of frailty T2DM (OR, 3.60; 95% CI 2.34–5.54; P < 0.0001) was associated with a significant increase in the prevalence of CHF compared to non-frailty T2DM in a fully adjusted model. During the median follow-up of 6.75 years, per 1-SD increase in FI was associated with a 41% higher risk of all-cause mortality and a 30% higher risk of cardiovascular mortality after being adjusted for all confounders. Similar results were observed when sensitivity analyses were performed. There was also a non-linear relationship between FI and all-cause mortality. In a weighted multivariate COX proportional model adjusted for full confounders, frailty T2DM increased all-cause (HR, 1.86; 95% CI 1.55–2.24; P < 0.0001) and cardiovascular (HR 1.66; 95% CI 1.18–2.33; P = 0.003) mortality and compared to non-frailty T2DM. The positive association of frailty index and all-cause mortality was only in participants without CHF. The positive association of frailty index and cardiovascular mortality was only in non-anti-diabetic drug users.
Conclusions
Frailty index in T2DM was positively associated with CHF in linear fashions. The Frailty index was positively correlated with all-cause and cardiovascular death in patients with T2DM. Frailty T2DM was positively associated with CHF, all-cause mortality, and cardiovascular mortality compared to non-frailty T2DM. Promoting frailty measurement and management in T2DM may be beneficial to reduce the burden of CHF and mortality.
Similar content being viewed by others
Introduction
Type 2 diabetes (DM) is a temporary metabolic disease characterized by insulin resistance and β-cell dysfunction [1] that affects multiple organ systems, including the cardiovascular [2]. According to previous studies, heart failure may be the first cardiovascular manifestation of many T2DM patients, even without other cardiovascular diseases [3]. Besides, T2DM patients with heart failure have a worse prognosis [4]. The prevalence of HF in individuals with T2DM has up to 22% and will continue to rise [3]. This increase is mainly due to the increasing global prevalence of T2DM and an aging population [5, 6], making this co-morbid state more worrisome. Therefore, it is urgent to identify high-risk groups of heart failure in diabetic people for secondary prevention.
Frailty has attracted much attention in the field of diabetes in recent years. Firstly, the burden of frailty in T2DM patients is high due to their accelerated aging process [7, 8]. Secondly, frailty increases the adverse outcome of T2DM [9,10,11]. Recent studies have shown that despite optimal managing five cardiovascular risk factors, the risk of T2DM with heart failure was still high [12]. Understanding the independent effect of frailty on HF in patients with T2DM could help identify high-risk patients early and reduce mortality in the context of novel therapies.
Although the current definition of frailty is still inconsistent, Rockwood et al. [13] developed the FI model, which includes chronic diseases, psychosocial factors, cognitive deficits, and other signs and symptoms of old age, is the most commonly used model to assess frailty. The ratio of the accumulated acquired deficits to all potential deficits in the model calculates the frailty index [13]. The higher the deficit count, the frailer the person is. A standard FI-created procedure has shown repeatable properties and helped understand frailty-related health characteristics in older adults [14]. Another study demonstrated that FI was a prognostic survivorship factor in younger individuals and was confirmed to be validated by examining its distribution and associations with age and sex [15].
A previous study has demonstrated the excess risk of HF associated with FI in a nationally representative population [16]. A recent study confirmed higher frailty burdens were independently associated with a higher risk of cardiovascular diseases in patients with prediabetes and DM [17]. Still, the association of frailty index with congestive heart failure, all-cause, and cardiovascular mortality in diabetic patients throughout the U.S. population has not been thoroughly studied. The study was designed to explore the association of frailty with heart failure and death in diabetic patients in a large, nationally representative population.
Research design and methods
Study population
The National Health and Nutrition Examination Survey (NHANES) is an ongoing, cross-sectional, and nationally representative health survey. The NHANES was designed to assess the nutritional and health status of non-institutional civilians of the U.S. older than two months, conducted by the National Center for Health Statistics (NCHS) of the U.S. Centers for Disease Control and Prevention (CDC). And sampling methods and data collection details had been provided on the NHANES website (http://www.cdc.gov/nchs/nhanes (Accessed on 2 February 2023)].
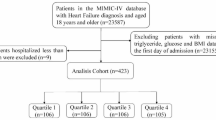
The current study enrolled patients with T2DM in ten data cycles in NHANES from 1999 to 2018. As is shown in Fig. 1, participants without complete medical records or enough information (≥ 80% out of 46 items) for the calculation of FI were excluded. Finally, 2894 participants with National Death Index (NDI) mortality data to conduct the study.
Definition of T2DM and CHF
Diabetes was defined as a self-reported diabetes diagnosis, use of diabetes medications or insulin, HbA1c ≥ 6.5%, fasting plasma glucose level ≥ 7.0 mmol/L, or random blood glucose (mmol/l) ≥ 11.1 mmol/L, 2-h OGTT blood glucose (mmol) ≥ 11.1 [18]. The definition of CHF was from the MCQ's positive answer: "Has a doctor or other health professional ever told you/sp that you/s/he had congestive heart failure?”.
Frailty index
The 49-item FI used in previous studies covered different systems, including cognition, dependence, depression, comorbidities, hospital utilization and general health, anthropometry, and laboratory data [19], constructed according to standardized procedures published before [14]. Since our participants were strictly composed of T2DM, we excluded self-reported DM, glycohemoglobin, and self-reported CHF; finally, a 46-item frailty index was made. The final FI value ranges between 0 and 1; higher scores are presented with higher frailty. We also categorized our sample into two groups: non-frail and frail, and the cut-off FI value was 0.21 [20]. All items of FI are shown in (Additional file 1: Tables S1, S2).
Covariates
Age, sex, race, education, smoking status, alcohol consumption, and medical history were self-reported. Race was categorized into Mexican American, non-Hispanic Black, non-Hispanic White, other Hispanic, and other Races; Smoking status was classified into three groups (no, former, and now). According to the self-reported average number of alcoholic drinks consumed daily, T2DM adults were classified as having no alcohol consumption, low to moderate alcohol consumption, or heavy alcohol consumption. A history of ASCVD was defined as coronary heart disease, angina, heart attack, and stroke. Hypertension was defined by those who had a self-reported history of hypertension, those who were taking anti-hypertensive medications, and those who were either having average systolic blood pressure (SBP) over 140 or/and average diastolic blood pressure (DBP) over 90 mmHg [21]. Hypertension can be diagnosed if one of these three criteria is met. Height and weight were collected at the mobile examination center (MEC), and BMI was calculated by the formula: body weight (kg)/ the square of height (m2). Obesity was defined as a BMI over 30 kg/m2. Laboratory methods for measurements of fasting total cholesterol (TC), high-density lipoprotein (HDL) cholesterol, fasting triglyceride (TG), fasting plasma glucose, albumin, and eGFR were reported in detail on the official NHANES website [http://www.cdc.gov/nchs/nhanes (Accessed on 2 February 2023)].
Outcome
The outcome of this study was all-cause and cardiovascular death. Mortality data were ascertained by linkage to the National Death Index (NDI) through 31 December 2019. Cardiovascular mortality in this study was defined as death due to heart diseases (ICD codes I00–I09, I11, I13, I20–I51) and stroke (ICD codes I60–I69) according to the International Statistical Classification of Diseases, 10th Revision [22].
Statistical analysis
We use complex sample weighted analysis of the fasting weights in the whole study according to NHANES analysis guidelines. T-test or Mann–Whitney U test (two groups of independent samples) were used to compare the continuous variables. Continuous variables are present as means (standard error). Categorical variables were expressed as numbers or percentages and compared by Pearson’s Chi-square test. Significant missing covariates were treated by missForest imputations when logistics and COX regression were ongoing to minimize the removal of samples. The logistic regression model was used to evaluate associations between FI and HF. The Cox regression models were constructed to assess the association of FI with all-cause and cardiovascular mortality. Two models were used in logistic and Cox regression analyses: model 1 was adjusted for age (continuous), gender, and race, and model 2 was adjusted for age (continuous), gender, race, education, smoking status, and alcohol consumption. Model 3 for logistic regression was adjusted for age (continuous), gender, race, education, smoking status, alcohol consumption, Obesity, systolic blood pressure, anti-diabetic drugs, HDL cholesterol, albumin, fasting plasma glucose, and eGFR. Model 3 for Cox regression was adjusted for age (continuous), gender, race, education, smoking status, alcohol consumption, Obesity, systolic blood pressure, anti-diabetic drugs, HDL cholesterol, albumin, fasting plasma glucose, eGFR, and CHF. Using a Cox proportional hazard model, the restricted cubic spline (RCS) further explored the relationship between FI and the outcome. The Kaplan–Meier method was used to analyze the survival probability data, and the log-rank test was used to compare the differences between each group. A fully adjusted multivariate regression model based on the interaction of FI with stratified covariates was used to conduct a subgroup analysis to assess whether the relationship between CHF and FI was affected by age (categories), sex, Obesity, and anti-diabetic drugs. When conducting a subgroup to determine the relationship between mortality and FI, we considered CHF in addition to the original four subgroups. Sensitivity analysis was conducted to determine the robustness by excluding participants whose follow-ups were less than one year or with an abnormal frailty index of Z score over ± 3. P < 0.05 was considered statistically significant. All statistical analyses were performed using R software (version 4.2).
Results
Baseline characteristics
The 2894 NHANES participants in T2DM with enough frailty index calculated information represented 19,493,702 non-institutionalized residents of the United States. Among the participants with T2DM [65.43 (0.30) years old; 49.23% males], the prevalence of CHF was 9.86%. Individuals with CHF were more likely to be older, had no alcohol consumption, and tended to have lower fasting total cholesterol, HDL cholesterol, albumin, and eGFR (Table 1). Patients with CHF were significantly associated with a higher percentage of Obesity, hypertension, ASCVD, anti-diabetic drug use, and frailty burden. At last, CHF patients had a higher frailty index (0.29 vs. 0.20, P < 0.0001), and weighted frailty prevalence was 40.40%.
The relationship of frailty index with CHF
We used weighted logistic regression to estimate the relationship of FI with CHF (Table 2). A crude analysis showed that an increase in FI was associated with a higher prevalence of CHF (OR = 2.10 1-SD, 95% CI 1.79–2.47, P < 0.0001). After adjusting for age (continuous), gender, race, education, smoking status, alcohol consumption, Obesity, systolic blood pressure, anti-diabetic drugs, HDL cholesterol, albumin, fasting plasma glucose, and eGFR, the association was still solid (OR = 2.02 1-SD, 95% CI 1.67–2.45, P < 0.0001). A weighted multivariate logistic regression was also conducted to examine the prevalence of CHF in T2DM participants with frailty. The presence of frailty T2DM (OR, 3.60; 95% CI 2.34–5.54; P < 0.0001) was associated with a significant increase in the prevalence of CHF compared to non-frailty T2DM in a fully adjusted model. As shown in Fig. 2, a restricted cubic spline was used to indicate the positive correlation of FI with CHF (P for nonlinearity = 0.0836). The overall population was stratified by age (categories), sex, Obesity, and anti-diabetic drugs, and subgroup analyses were conducted. We did not observe any significant interaction in both FI and frailty subgroup analysis (all P for interaction > 0.05, Fig. 3). The correlation was generally robust in sensitivity analysis when excluding participants with abnormal frailty index (Additional file 1: Table S3).
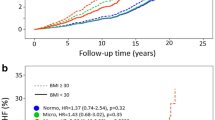
The relationship of the frailty index with all-cause and cardiovascular mortality
In this retrospective cohort, we observed an association of the frailty index with all-cause and cardiovascular mortality risk. Kaplan–Meier curves are shown in Fig. 4 to illustrate the survival probability according to non-frailty and frailty. Compared with the non-frailty group, individuals with frailty had the worst survival (36.34% at 20 years, log-rank test: P < 0.0001). The pattern was generally similar for cardiovascular mortality (log-rank test: P < 0.0001). Analysis of continuous FI showed that a 1-SD increase in FI was associated with a 44% higher risk of all-cause mortality without adjusting for confounders. The all-cause mortality risk persisted after adjusting for all confounders (HR = 1.41 1-SD, 95% CI 1.29–1.55, P < 0.0001). Similarly, a 1-SD increase in FI was associated with a 43% higher risk of cardiovascular mortality without adjusted and a 30% risk with fully adjusted for all confounders. Survival analysis was also conducted to examine the all-cause mortality and cardiovascular mortality between frailty T2DM and non-frailty T2DM. In a weighted multivariate COX proportional model adjusted for age (continuous), gender, race, education, smoking status, alcohol consumption, Obesity, systolic blood pressure, anti-diabetic drugs, HDL cholesterol, albumin, fasting plasma glucose, eGFR, and CHF, frailty T2DM increased all-cause (HR, 1.86; 95% CI 1.55–2.24; P < 0.0001) and cardiovascular (HR 1.66; 95% CI 1.18–2.33; P = 0.03) mortality and compared to non-frailty T2DM (Tables 3 and 4).
As shown in Fig. 5, restricted cubic splines were used to indicate the positive correlation of FI with all-cause and cardiovascular mortality. The relationship between FI and all-cause mortality was non-linear (P for nonlinearity = 0.0063). However, a non-linear relationship was not observed between FI and cardiovascular mortality (P for nonlinearity = 0.2022).
The overall population was stratified by age (categories), sex, Obesity, anti-diabetic drugs, and CHF, and subgroup analyses were conducted (Figs. 6 and 7). When the frailty index was treated as continuous, we did not observe any significant interaction in the all-cause mortality subgroup analysis except for the subgroups of CHF (P for interaction = 0.023). A significant interaction was identified between frailty index and anti-diabetic drug use for the cardiovascular mortality subgroup analysis. The inverse association between frailty index and cardiovascular mortality appeared only in non-anti-diabetic drug users (HR = 1.62 1-SD; 95% CI 1.23–2.13, P for interaction = 0.002). When the frailty index was categorized into non-frailty and frailty groups, we did not observe any significant interaction in the all-cause and cardiovascular mortality subgroup analysis (all P for interaction > 0.05).
The correlations were generally robust in sensitivity analysis when excluded participants whose follow-ups were less than one year or with abnormal frailty index (Additional file 1: Tables S2–S6).
Discussion
This study explored the association of frailty index with heart failure, all-cause, and cardiovascular mortality in a representative sample of T2DM in the United States. Data collected from ten cycles of NHANES from 1999 to 2018 showed an association between frailty index and heart failure in patients with T2DM. The presence of frailty T2DM was associated with a significant increase in the prevalence of CHF compared to non-frailty T2DM. During the median follow-up of 6.75 years, increased FI was positively associated with all-cause and cardiovascular mortality. Along with the 1-SD increase in FI, the risk of all-cause mortality showed a 41% increase. In the meantime, the increase in cardiovascular mortality risk was 30%. Compared to non-frailty. Frailty T2DM was associated with a significant increase in the risk of all-cause and cardiovascular death compared to non-frailty T2DM. The positive association of frailty index and all-cause mortality was only in participants with CHF, and cardiovascular mortality was only in non-anti-diabetic users when FI was continuous.
The Fried phenotype and the Rockwood index are classic models for assessing frailty status [13, 23]. The Fried phenotype assesses the impairment of physiological reserves in 5 areas of body function: unintentional weight loss, loss of endurance, frailty, slowness of movement, and low levels of physical activity. Frailty refers to people with more than two of the above factors [23]. Rockwood FI assesses frailty as an accumulation of health deficits in multiple domains. It can be evaluated using clinical and health status data on signs and symptoms, comorbidities, laboratory data, activities of daily living, and patient-reported symptoms. Its construction model is flexible and evolving [13]. Many studies have assessed their similarities and differences, but there is still no complete agreement [20, 24,25,26,27]. Some studies prove that the vulnerability index can define the risk of adverse outcomes more precisely than phenotypes [28,29,30,31]. Several extensive studies and clinical trials in diabetic populations have also assessed frailty using the cumulative frailty index of health defects32,33,34. Thus, we ultimately chose to evaluate frailty in diabetes patients by cumulatively computing a frailty index for multiple domain health deficits.
Our study indicated that FI is associated with an increased prevalence of heart failure in T2DM. It is consistent with a recent post hoc analysis of prospective trials in which higher baseline frailty was significantly associated with a higher risk of HF in adults with T2DM [17]. The retrospective study by Chen et al. showed that frailty was associated with an increased prevalence of CHF, and subgroup analysis showed elevated FI in HF patients with T2DM. Still, no further studies were conducted [16].
Our findings confirm the positive association of frailty with all-cause mortality and cardiovascular death in patients with diabetes. Consistent with previous studies, one study showed a positive association of frailty with all-cause mortality in middle-aged and older diabetic patients [35, 36]. Also, in two prospective cohorts, frailty has been confirmed to be associated with the progression of elevated risks of all-cause mortality in individuals with prediabetes and diabetes [37]. Our study also found that frailty was associated with cardiovascular mortality in patients with T2DM in this large, nationally representative population.
The connection between the severity of frailty and mortality risk in T2DM was inconclusive. A non-linear relationship between FI and all-cause mortality in patients with T2DM was observed in the RCS, not cardiovascular mortality. According to our study, the median of FI for all-cause and cardiovascular mortality was 0.186. Our study provides a reference for the median FI of T2DM in the community. Still, it should be interpreted cautiously because the proportion of T2DM patients excluded due to insufficient FI data is not low, and it is likely to have selection bias. Our study determined the FI cut-off value of 0.21 in the diabetic population was useful and provided a reliable basis for identifying and managing frail patients with T2DM. Moreover, we also found that KM survival curves were distinguished significantly by grouping with a cut-off of 0.21. The stability of this cut-off value was further verified.
In the subgroup analysis for all-cause mortality with FI, the association between frailty index and all-cause mortality appeared only in participants without a CHF history. This suggests that the risk of all-cause death from diabetes with frailty and other complications or comorbidities may not necessarily be lower than that of heart failure. And the severity of heart failure may mask the effect of frailty on all-cause death. It also suggests that it may be beneficial to study the potential benefits of heart failure treatment for debilitating type 2 diabetes. In the subgroup analysis for cardiovascular mortality with FI, the association between frailty index and cardiovascular mortality appeared only in non-anti-diabetic drug users. This suggests that using hypoglycemic drugs may mitigate the link between frailty and cardiovascular death in patients with type 2 diabetes through blood sugar control, prevention of cardiac complications, or other possible disease-regulating effects. Moreover, specific new hypoglycemic drugs have also shown the effect of resisting weak cardiovascular damage and have good safety [38]. More research is needed to confirm this exciting association.
The mechanism of frailty associated with heart failure and mortality in T2DM remains unclear. The pathophysiological mechanisms of frailty and heart failure are intertwined, including upregulation of pro-inflammatory states, metabolic impairment, and insulin resistance [39]. Increased risk of incident heart failure and death is associated with insulin resistance in people with newly diagnosed type 2 diabetes [40]. Frailty was considered a significant factor in increasing the risk for hypoglycemia [41]. A recent randomized controlled trial confirmed severe hypoglycemia was independently associated with a greater risk of incident HF [42]. Another recent study indicated that severe hypoglycemia was associated with increased risks of hospitalization for HF among adults with diabetes regardless of coexistent CVDs [43]. These findings suggest that hypoglycemia may be an intermediary in T2DM between frailty and heart failure. More interestingly, a previous study showed that incremental frailty was associated with increased hyperglycemia rather than hypoglycemia in older adults with T2DM who are on insulin therapy. HR was increased with severe hyperglycemia [44]. Frailty was also associated with cognitive impairment. Cognitive impairment was a decisive prognostic factor identifying people with diabetes at high risk of mortality [45]. Both Frailty and hypoglycemia increased functional decline, leading to a gradient effect on mortality in individuals with diabetes [46]. Moreover, frailty may also reduce the protective effect of certain anti-diabetic drugs, such as metformin, on adverse outcomes [47]. Therefore, further mechanism exploration is urgently needed.
The study provides new insights into CHF and death associated with frailty in people with T2DM. First, the study showed a need for frailty assessment in patients with T2DM in America. It is well-known that frailty is a geriatric syndrome. The previous clinical guidelines and consensus report advocate that frailty assessment is an essential component of diabetes management for older patients [48, 49]. However, our findings suggested the need for frailty assessment was not only for older patients but also for individuals under 65 years to prevent CHF and death. Second, for patients with T2DM without heart failure, future explorations should also actively identify or manage flimsy to reduce the risk of all-cause death. Third, to study the potential protective mechanism of different hypoglycemic drugs on the effects of T2DM weakness on cardiovascular death and prescribing appropriate personalized hypoglycemic prescriptions may be a vital management link in the study of T2DM-frailty. Furthermore, due to the predictive value and the dynamic nature of frailty [9, 10, 17, 50, 51], multifactorial interventions will be needed to reverse frailty or delay the further progression of diabetes, including optimal nutrition with protein intake, combining aerobic, weight-bearing, and resistance training [52]. Relevant clinical trials are also needed to explore appropriate treatment strategies to guide treatment decisions.
Our study also has some limitations. First, we could not infer causality attributable to the observational study design. Our findings need further prospective studies with large samples to confirm. Second, we only considered FI at baseline and did not have data on dynamic changes in FI, which may lead to bias. In addition, although we considered as many covariates as possible, some confounding factors still have not been adjusted.
Conclusion
In this nationally representative sample of US adults, the frailty index in T2DM was positively associated with the presence of CHF in non-linear fashions. The Frailty index was positively correlated with all-cause and cardiovascular death in patients with T2DM. Frailty T2DM was positively associated with CHF, all-cause mortality, and cardiovascular mortality compared to non-frailty T2DM. Moreover, the strength of the association between FI and mortality differed within the study population. Promoting frailty measurement and management in T2DM may be beneficial to reduce the burden of CHF and mortality.
Availability of data and materials
The original contributions presented in the study are included in the article/Additional files. Further inquiries can be directed to the corresponding authors.
References
Rawshani A, Rawshani A, Franzén S, Eliasson B, Svensson AM, Miftaraj M, et al. Mortality and cardiovascular disease in type 1 and type 2 diabetes. N Engl J Med. 2017;376(15):1407–18.
Ahmad E, Lim S, Lamptey R, Webb DR, Davies MJ. Type 2 diabetes. Lancet. 2022;400(10365):1803–20.
Pop-Busui R, Januzzi JL, Bruemmer D, Butalia S, Green JB, Horton WB, et al. Heart failure: an underappreciated complication of diabetes. A consensus report of the American diabetes association. Diabetes Care. 2022;45(7):1670–90.
Ferreira JP, Vasques-Nóvoa F, Ferrão D, Saraiva F, Falcão-Pires I, Neves JS, et al. Fenofibrate and heart failure outcomes in patients with type 2 diabetes: analysis from ACCORD. Diabetes Care. 2022;45(7):1584–91.
Ritchie RH, Abel ED. Basic mechanisms of diabetic heart disease. Circ Res. 2020;126(11):1501–25.
Omote K, Verbrugge FH, Borlaug BA. Heart failure with preserved ejection fraction: mechanisms and treatment strategies. Annu Rev Med. 2022;27(73):321–37.
Wu Y, Xiong T, Tan X, Chen L. Frailty and risk of microvascular complications in patients with type 2 diabetes: a population-based cohort study. BMC Med. 2022;20(1):473.
Perkisas S, Vandewoude M. Where frailty meets diabetes. Diabetes Metab Res Rev. 2016;32(Suppl 1):261–7.
Chao CT, Wang J, Chien KL, COhort of GEriatric Nephrology in NTUH (COGENT) study group. Both pre-frailty and frailty increase healthcare utilization and adverse health outcomes in patients with type 2 diabetes mellitus. Cardiovasc Diabetol. 2018;17(1):130.
Ida S, Kaneko R, Imataka K, Murata K. Relationship between frailty and mortality, hospitalization, and cardiovascular diseases in diabetes: a systematic review and meta-analysis. Cardiovasc Diabetol. 2019;18(1):81.
Ferri-Guerra J, Aparicio-Ugarriza R, Salguero D, Baskaran D, Mohammed YN, Florez H, et al. The association of frailty with hospitalizations and mortality among community dwelling older adults with diabetes. J Frailty Aging. 2020;9(2):94–100.
Rawshani A, Rawshani A, Franzén S, Sattar N, Eliasson B, Svensson AM, et al. Risk factors, mortality, and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2018;379(7):633–44.
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–95.
Searle SD, Mitnitski A, Gahbauer EA, Gill TM, Rockwood K. A standard procedure for creating a frailty index. BMC Geriatr. 2008;30(8):24.
Jiang M, Foebel AD, Kuja-Halkola R, Karlsson I, Pedersen NL, Hägg S, et al. Frailty index as a predictor of all-cause and cause-specific mortality in a Swedish population-based cohort. Aging (Albany NY). 2017;9(12):2629–46.
Chen X, Hou C, Yao L, Ma Y, Li Y, Li J, et al. The association between chronic heart failure and frailty index: a study based on the National Health and Nutrition Examination Survey from 1999 to 2018. Front Cardiovasc Med. 2022;9:1057587.
Pandey A, Khan MS, Garcia K, Simpson F, Bahnson J, Patel KV, et al. Association of baseline and longitudinal changes in frailty burden and risk of heart failure in type 2 diabetes-findings from the look AHEAD trial. J Gerontol A Biol Sci Med Sci. 2022;77(12):2489–97.
American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2020. Diabetes Care. 2020;43(1):S14-31.
Hakeem FF, Bernabé E, Sabbah W. Association between oral health and frailty among american older adults. J Am Med Dir Assoc. 2021;22(3):559-563.e2.
Blodgett J, Theou O, Kirkland S, Andreou P, Rockwood K. Frailty in NHANES: comparing the frailty index and phenotype. Arch Gerontol Geriatr. 2015;60(3):464–70.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2018;71(19):e127-248.
Li B, Chen L, Hu X, Tan T, Yang J, Bao W, et al. Association of serum uric acid with all-cause and cardiovascular mortality in diabetes. Diabetes Care. 2023;46(2):425–33.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146-156.
Malmstrom TK, Miller DK, Morley JE. A comparison of four frailty models. J Am Geriatr Soc. 2014;62(4):721–6.
Ravindrarajah R, Lee DM, Pye SR, Gielen E, Boonen S, Vanderschueren D, et al. The ability of three different models of frailty to predict all-cause mortality: results from the European Male Aging Study (EMAS). Arch Gerontol Geriatr. 2013;57(3):360–8.
Cao X, Yang Z, Li X, Chen C, Hoogendijk EO, Zhang J, et al. Association of frailty with the incidence risk of cardiovascular disease and type 2 diabetes mellitus in long-term cancer survivors: a prospective cohort study. BMC Med. 2023;21(1):74.
Petermann-Rocha F, Hanlon P, Gray SR, Welsh P, Gill JMR, Foster H, et al. Comparison of two different frailty measurements and risk of hospitalisation or death from COVID-19: findings from UK Biobank. BMC Med. 2020;18(1):355.
Kulminski AM, Ukraintseva SV, Kulminskaya IV, Arbeev KG, Land K, Yashin AI. Cumulative deficits better characterize susceptibility to death in elderly people than phenotypic frailty: lessons from the Cardiovascular Health Study. J Am Geriatr Soc. 2008;56(5):898–903.
Theou O, Brothers TD, Mitnitski A, Rockwood K. Operationalization of frailty using eight commonly used scales and comparison of their ability to predict all-cause mortality. J Am Geriatr Soc. 2013;61(9):1537–51.
Li JJ, Jiang S, Zhu ML, Liu XH, Sun XH, Zhao SQ. Comparison of three frailty scales for prediction of adverse outcomes among older adults: a prospective cohort study. J Nutr Health Aging. 2021;25(4):419–24.
Oviedo-Briones M, Rodríguez-Laso Á, Carnicero JA, Gryglewska B, Sinclair AJ, Landi F, et al. The ability of eight frailty instruments to identify adverse outcomes across different settings: the FRAILTOOLS project. J Cachexia Sarcopenia Muscle. 2022;13(3):1487–501.
Simpson FR, Justice JN, Pilla SJ, Kritchevsky SB, Boyko EJ, Munshi MN, Ferris CK, Espeland MA; Look AHEAD Research Group. An examination of whether diabetes control and treatments are associated with change in frailty index across 8 years: an ancillary exploratory study from the action for health in diabetes (Look AHEAD) trial. Diabetes Care. 2023;46(3):519–25. https://doi.org/10.2337/dc22-1728
Evans JK, Usoh CO, Simpson FR, Espinoza S, Hazuda H, Pandey A, Beckner T, Espeland MA, Action for Health in Diabetes Study Group. Long-term impact of a 10-year intensive lifestyle intervention on a deficit accumulation frailty index: action for health in diabetes (Look AHEAD) trial. J Gerontol A Biol Sci Med Sci. 2023. https://doi.org/10.1093/gerona/glad088.
Pond HM, Kehler S, Seaman K, Bouchard DR, Sénéchal M. Association between physical activity & sedentary time on frailty status in males and females living with diabetes mellitus: a cross-sectional analysis. Exp Gerontol. 2022;161:111741. https://doi.org/10.1016/j.exger.2022.111741
Castro-Rodríguez M, Carnicero JA, Garcia-Garcia FJ, Walter S, Morley JE, Rodríguez-Artalejo F, et al. Frailty as a major factor in the increased risk of death and disability in older people with diabetes. J Am Med Dir Assoc. 2016;17(10):949–55.
Chode S, Malmstrom TK, Miller DK, Morley JE. Frailty, diabetes, and mortality in middle-aged African Americans. J Nutr Health Aging. 2016;20(8):854.
He D, Li J, Li Y, Zhu J, Zhou T, Xu Y, et al. Frailty is associated with the progression of prediabetes to diabetes and elevated risks of cardiovascular disease and all-cause mortality in individuals with prediabetes and diabetes: evidence from two prospective cohorts. Diabetes Res Clin Pract. 2022;194: 110145.
Kutz A, Kim DH, Wexler DJ, Liu J, Schneeweiss S, Glynn RJ, et al. Comparative cardiovascular effectiveness and safety of SGLT-2 inhibitors, GLP-1 receptor agonists, and DPP-4 inhibitors according to frailty in type 2 diabetes. Diabetes Care. 2023. https://doi.org/10.2337/dc23-0671.
Pandey A, Kitzman D, Reeves G. Frailty is intertwined with heart failure: mechanisms, prevalence, prognosis, assessment, and management. JACC Heart Fail. 2019;7(12):1001–11.
Wamil M, Coleman RL, Adler AI, McMurray JJV, Holman RR. Increased risk of incident heart failure and death is associated with insulin resistance in people with newly diagnosed type 2 diabetes: UKPDS 89. Diabetes Care. 2021;44(8):1877–84.
Abdelhafiz AH, McNicholas E, Sinclair AJ. Hypoglycemia, frailty and dementia in older people with diabetes: reciprocal relations and clinical implications. J Diabetes Complications. 2016;30(8):1548–54.
Echouffo-Tcheugui JB, Kaze AD, Fonarow GC, Dagogo-Jack S. Severe hypoglycemia and incident heart failure among adults with type 2 diabetes. J Clin Endocrinol Metab. 2022;107(3):e955–62.
Lee YB, Bae YJ, Kim H, Park J, Kwon SY, Park SH, et al. Severe hypoglycemia and risk of hospitalization for heart failure in adults with diabetes treated with oral medications with or without insulin: a population-based study. Diabetes Res Clin Pract. 2022;192: 110083.
Fung E, Lui LT, Huang L, Cheng KF, Lau GH, Chung YT, et al. Characterising frailty, metrics of continuous glucose monitoring, and mortality hazards in older adults with type 2 diabetes on insulin therapy (HARE): a prospective, observational cohort study. Lancet Healthy Longev. 2021;2(11): e724.
Thein FS, Li Y, Nyunt MSZ, Gao Q, Wee SL, Ng TP. Physical frailty and cognitive impairment is associated with diabetes and adversely impact functional status and mortality. Postgrad Med. 2018;130(6):561–7.
Li CL, Chang HY, Shyu YIL. The excess mortality risk of diabetes associated with functional decline in older adults: results from a 7-year follow-up of a nationwide cohort in Taiwan. BMC Public Health. 2011;23(11):953.
Liu P, Pan Y, Song Y, Zhou Y, Zhang W, Li X, et al. Association of metformin exposure with low risks of frailty and adverse outcomes in patients with diabetes. Eur J Med Res. 2023;28(1):65.
Dunning T, Sinclair A, Colagiuri S. New IDF guideline for managing type 2 diabetes in older people. Diabetes Res Clin Pract. 2014;103(3):538–40.
Davies MJ, Aroda VR, Collins BS, Gabbay RA, Green J, Maruthur NM, et al. Management of hyperglycemia in type 2 diabetes, 2022. A consensus report by the American diabetes association (ADA) and the European association for the study of diabetes (EASD). Diabetes Care. 2022;45(11):2753–86.
Ting MJM, Hyde Z, Flicker L, Almeida OP, Golledge J, Hankey GJ, et al. Associations between diabetes, body mass index and frailty: the Western Australian health in men study. Maturitas. 2022;161:58–64.
Espeland MA, Justice JN, Bahnson J, Evans JK, Munshi M, Hayden KM, et al. Eight-year changes in multimorbidity and frailty in adults with type 2 diabetes mellitus: associations with cognitive and physical function and mortality. J Gerontol A Biol Sci Med Sci. 2022;77(8):1691–8.
American Diabetes Association Professional Practice Committee. 13. Older adults: standards of medical care in diabetes-2022. Diabetes Care. 2022;45(1):S195-207.
Acknowledgements
This study is based on the National Health and Nutrition Examination Survey (NHANES). We would like to thank the NHANES research staff and every participant for their valuable time and efforts devoted to the NHANES project.
Funding
None.
Author information
Authors and Affiliations
Contributions
YNQ collected and analyzed the data and wrote the original manuscript. XPZ contributed to the manuscript revision. Both authors approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The studies involving human participants were reviewed and approved by the National Center for Health Statistics (NCHS) Research Ethics Review Board (ERB). The patients/participants provided written informed consent to participate in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Variables in the 46-item frailty index and their respective scorings. Table S2. Logistic regression analysis of the 1-SD FI and frailty after excluding participants with abnormal FI data. (N = 2873). Table S3. Risk of all-cause mortality among diabetes patients according to 1-SD FI and frailty after excluding participants who died within 1 years of follow-up (N = 2834). Table S4. Risk of cardiovascular mortality among diabetes patients according to 1-SD FI and frailty after excluding participants who died within 1 years of follow-up (N = 2834). Table S5. Risk of all-cause mortality among diabetes patients according to 1-SD FI and frailty after excluding participants with abnormal FI data (N = 2873). Table S6. Risk of cardiovascular mortality among diabetes patients according to 1-SD FI and frailty after excluding participants with abnormal FI data (N = 2873).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Qin, YN., Zheng, XP. Association of frailty index with congestive heart failure, all-cause and cardiovascular mortality among individuals with type 2 diabetes: a study from National Health and Nutrition Examination Surveys (NHANES), 1999–2018. Diabetol Metab Syndr 15, 210 (2023). https://doi.org/10.1186/s13098-023-01165-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-023-01165-z