Abstract
Aims
To evaluate the prevalence of diabetic retinopathy (DR) in Brazilian adults with diabetes mellitus via a systematic review with meta-analysis.
Methods
A systematic review using PubMed, EMBASE, and Lilacs was conducted, searching for studies published up to February 2022. Random effect meta-analysis was performed to estimate the DR prevalence.
Results
We included 72 studies (n = 29,527 individuals). Among individuals with diabetes in Brazil, DR prevalence was 36.28% (95% CI 32.66–39.97, I2 98%). Diabetic retinopathy prevalence was highest in patients with longer duration of diabetes and in patients from Southern Brazil.
Conclusion
This review shows a similar prevalence of DR as compared to other low- and middle-income countries. However, the high heterogeneity observed—expected in systematic reviews of prevalence—raises concerns about the interpretation of these results, suggesting the need for multicenter studies with representative samples and standardized methodology.
Similar content being viewed by others
Introduction
Diabetes mellitus is a metabolic disease that may lead to chronic microvascular and macrovascular complications [1]. Diabetic retinopathy (DR)—the most common complication of diabetes mellitus—is one of the leading causes of preventable blindness in the adult population [2]. Vision impairment and blindness due to diabetes may be irreversible if timely treatment is not provided, affecting the individual’s functional capabilities and self-care [3]. Moreover, DR is considered a risk factor for other diabetes complications [4].
The International Diabetes Federation estimates that 537 million adults live with diabetes in 2021 [5]. In Brazil, a systematic review estimated a 6.9% prevalence of diabetes in the population based on studies published after 2010 [6]. With an aging population, coupled with growing rates of diabetes, a higher burden of DR and demand for eye care and treatment are expected [2]. The international literature on DR epidemiology has several population studies, such as the WESDR [7], UKPDS [8], DCCT [9], and ETDRS [10], and a recent systematic review by Teo et al. has concluded that—amongst individuals with diabetes—the global prevalence of DR is estimated at 22.27% [2]. However, factors such as varying levels of surveillance, different socio-economic factors, and health systems organization can prompt differences in estimated DR prevalence among countries [11,12,13,14].
Brazil is a large upper-middle-income country that hosts the world’s sixth largest population of individuals with diabetes [15]; it is also the country with the largest free public health care system [16], on which around 75% of its population relies [17]. National data on the prevalence of DR are lacking, but regional studies indicate a prevalence ranging from 7.6 to 44.4% of individuals with diabetes, with great regional and methodological variations in each survey [18,19,20,21,22,23].
The diagnosis of DR comprises the detection of ophthalmological lesions in ophthalmoscopy or color fundus photographs that are considering in classifying DR. The classification defines the prognosis and the need for treatment. More advanced degrees of DR have a worse prognosis. DR is classified as proliferative and non-proliferative, being divided into mild, moderate and severe; macular edema may or may not be present [24].
Because DR is a major public health issue, demanding thoughtful resource allocation, and since blindness is preventable with timely treatment, planning from health authorities is crucial. Since no national strategies or standardized workflows for DR screening and management in the Brazilian public health system currently exist [25], estimating the prevalence of DR and its regional variations is a crucial step for designing such policies and for an effective resource and workforce allocation. This study aims to assess the prevalence of DR in Brazil; additionally, this study aims to evaluate other aspects of DR epidemiology, such as geographic differences and risk factors.
Methods
This report describes a systematic review and meta-analysis of studies describing the DR prevalence in individuals with diabetes in Brazil. All procedures herein described were conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses and Meta-analyses Of Observational Studies in Epidemiology guidelines [26]. The protocol for this review was registered and publicly available at PROSPERO (CRD42022362777).
Search strategy
Three databases (PubMed, LILACS, and EMBASE) were systematically searched using terms related to diabetes, retinopathy, and prevalence. Papers written in English, Portuguese, or Spanish were retrieved, from inception to February 2022. The detailed search strategy can be consulted in Additional file 1: Table S1.
Eligibility criteria
Articles meeting the following criteria were included: (1) designed as cross-sectional, cohort, or case–control studies, (2) conducted in Brazil, (3) describing the frequency of adults with DR among those with type 1 diabetes or type 2 diabetes. Studies including pregnant women, patients with diabetes other than type 1 or type 2 diabetes mellitus, or conducted outside Brazil were excluded.
Study selection
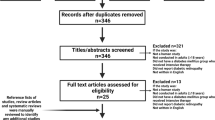
A.N.G. and M.A.R. independently reviewed titles and abstracts considering eligibility criteria. Once the initial screening was completed, full-texts were reviewed by both researchers. Discrepancies in all steps were resolved by consensus. Figure 1 shows a PRISMA diagram depicting the study selection process.
Data extraction
Two reviewers (G.L. and M.A.R.) independently extracted relevant data from the included studies using a standardized form and following a predetermined protocol. Extracted data included: title, first author, year of publication, language, study objective, study design, year of data collection, municipality and federative unit studied, sample size, gender, type of diabetes, duration of diabetes, skin color, mean age, frequency of DR, frequency by type of DR, classification of DR used, and diagnostic method of DR.
Risk of bias assessment
Risk of Bias (RoB) was assessed in duplicate by L.P.S. and T.A.C., using a tool developed by Hoy et al. [27] for RoB estimation in prevalence studies. The tool comprises 10 items, classified as low or high risk of bias and a summary item that stratifies studies in low, moderate, or high risk of bias. Disagreements were resolved by discussion, with involvement of a third author when necessary. RoB plots were generated using the ‘robvis’ package for R (version 0.3.0) [28].
Statistical analysis
Overall and subgroup prevalence estimates, with corresponding 95% confidence intervals, were estimated based on reported frequencies of DR in individuals with diabetes within the included studies. Pooled estimates were obtained by a random-effects inverse variance approach with arcsine transformation, assuming heterogeneity between studies due to the epidemiological nature of primary literature [29]. Confidence intervals for individual studies were estimated using the Clopper-Pearson approach. Percentage of total variability due to between-study heterogeneity was estimated by I2 statistic. Subgroup analyses were also performed to determine whether the following variables affected prevalence estimates: geographic region (South, Southeast, Midwest, North, and Northeast), diabetes duration (shorter than 10 and longer than 10 years), type of diabetes, year of the study (before or after 2000). All analyses were performed using the ‘meta’ package (version 6.0) for R (version 4.2.1). To reduce heterogeneity, potential factors that should affect it were explored, including studies that were carried out in ophthalmology services for the diagnosis of DR.
Results
The search retrieved 1400 articles from October 1950 to February 2022, of which 103 were duplicates and were excluded. In total, 975 articles were removed based on title and abstracts; 322 full-text articles were assessed for eligibility, of which 72 met all inclusion criteria. Figure 1 shows the flowchart of study selection.
Table 1 shows the characteristics of the included studies by diagnostic criteria and method of assessment.
A meta-analysis was conducted; Fig. 2 shows prevalence rates. The prevalence rate of DR (pooled estimate) was 36.28% (95% CI 32.66–39.97, I2 98%).
We could not assess the prevalence of DR by gender because such variable was unspecified in most studies.
Trend analyses showed an increase in the prevalence of DR in patients with longer duration of diabetes [20.73% (95% CI 11.63–31.64 I2 98%) in less than 10 years of diabetes, and 37.73% (95% CI 30.80–44.93 I2 96%) in longer than 10 years] (Additional file 2: Fig. S1) and in patients with type 2 diabetes mellitus [26.84% (95% CI 16.43–38.74, I2 98%) in type 1 diabetes mellitus and 35.69% (95% CI 30.16–41.41, I2 98%) in type 2 diabetes mellitus] (Additional file 3: Fig. S2).
In the assessment of prevalence of DR according to the year of publication of the study, no difference in the prevalence of DR [36.06% (95% CI 31.59–40.65, I2 98%) was observed in articles published after 2000 and 37.84% (95% CI 22.90–54.07, I2 96%) in those published before 2000] (Additional file 4: Fig. S3).
The analysis of prevalence rates by diagnostic method showed a prevalence of 38.15% (95% CI 33.08–43.36, I2 98%) in patients diagnosed by indirect ophthalmoscopy, and 31.11% (95% CI 19.55–44.00, I2 98%) by color fundus photography (CFP, Additional file 5: Fig. S4).
We explored potential factors that would affect the heterogeneity of the analyses, including studies that were carried out in ophthalmology services for the diagnosis of DR. Table 2 shows prevalence rates of DR and their 95% CI by Brazilian regions and adjustment to studies that were not performed in ophthalmology services. The data in this table show that the prevalence of DR was higher in the Southern region. No significant change of the heterogeneity was observed when we did this type of new analyses.
Quality of studies
Figure 3 summarizes data regarding quality of studies. A total of 18 studies (25%) had an intermediate risk of bias, and the rest of the studies had a high risk of bias. Additional file 6: Fig. S5 shows the risk of bias assessment for each study. Most studies were based on cross-sectional design (59 studies, 82%). The most used design was convenience sampling (68 studies, 94%). Most studies were developed only in or including data from Southeastern and Southern Brazil (30 studies, 48.4% and 24 studies, 33.3%, respectively). In 23 studies (31.9%), the main objective was to evaluate the prevalence of DR.
Discussion
Our study provides comprehensive and up-to-date evaluations of the current DR prevalence in Brazil with the largest meta-analysis to date.
This study included 72 studies carried out in Brazil and found a 36.26% prevalence of DR. It also found a higher prevalence in patients with long-term disease, type 2 diabetes, and residents of the Southern region.
According to the IDF 2021 atlas [15], 15.7 million people live with diabetes in Brazil, being the sixth country with the highest number of people with diabetes. Teló et al.—in a systematic review with meta-analysis of Brazilian observational studies from 1980 to 2015—included 50 studies and showed an increasing prevalence of diabetes in recent decades, showing that the prevalence of diabetes in Brazil can reach 6.9% of the population in studies published after 2010 [6]. Data obtained from the National Survey of Health (2014 to 2015) showed the following prevalence of diabetes according to different criteria: 6.6% (95% CI 5.9–7.2) [glycated hemoglobin (HbA1c) ≥ 6.5% (47.5 mmol/mol)]; 8.4% (95% CI 7.6–9.1) [HbA1c ≥ 6.5% (47.5 mmol/mol) or use of antidiabetic drugs]; 9.4% (95% CI 8.6–10.1) [HbA1c ≥ 6.5% (47.5 mmol/mol) or history of diabetes]; and 7.5% (95% CI 6.7–to 8.2) [history of diabetes] [95]. Extrapolating the prevalence of DR found in our review, 5.7 million people would be living with DR in Brazil. Comparing our outcomes with other systematic reviews that evaluated the prevalence of DR, our study showed a higher prevalence than China (18.45%) [96], Africa (30.2–31.6%) [97], and Europe (25.7%) [98]. In India, a systematic review performed with 8,866 diabetic patients found a 16.1% prevalence of RD [11, 98]; in Pakistan, a systematic review estimated the prevalence of DR at 28.2%, ranging from 10.6 to 91.34% [12]; in the USA, a study carried out from 2005 to 2008 with 1495 diabetic patients showed a 47% prevalence of DR [13]; in Indonesia, a 2017 study showed a DR prevalence of 43.1% in patients with type 2 diabetes mellitus [14]. Different study methodologies applied in primary studies retrieved in these different meta-analyses are important to determine these high different figures among countries.
Regarding the predictors evaluated in trend analysis, the duration of diabetes increases the prevalence of DR. Duration of diabetes is an established risk factor for the development of DR and other microvascular complications in patients with diabetes [99,100,101]. The same trend was described in another systematic review [14].
The study showed a higher prevalence of DR in type 2 diabetes mellitus patients, but the literature shows that prevalence is higher in type 1 diabetes mellitus [7]. One of the possibilities is that the studies on patients with type 1 diabetes mellitus have been carried out with a short duration of disease. Moreover, since type 2 diabetes mellitus is more prevalent than type 1 diabetes mellitus, a higher number of people with type 2 diabetes mellitus are possibly being studied as compared to those with type 1 diabetes mellitus, unbalancing the final outcomes.
This meta-analysis showed that the prevalence of DR in the Southern region is higher than in the Northern region. This can be explained because disease burden components have different distributions between the North and the South in Brazil, due to economic and social disparities between regions. As a country with continental territory, racial and cultural miscegenation, Brazil experiences great social and economic problems, including socioeconomic inequality. The Federation Unit with the lowest poverty rate in 2021 was Santa Catarina (10.16%) in the South and the one with the highest proportion of poor people was Maranhão with 57.90% in the Northeast. Segmenting the country into 146 spatial strata, the one with the greatest poverty in 2021 is the Coast and Baixada Maranhense with 72.59%, while the lowest is in the municipality of Florianópolis in South with 5.7% [102]. It is theorized that patients living in the Northern region do not live long enough to develop microvascular complications of diabetes [103] and, as aforementioned, the duration of the disease is one of the markers that increase the risk of developing DR. Another difference may be because in the Northern region access to public health is more limited [104].
The gold standard method for screening for DR is CFPs [105]. In this review, eight (11%) studies used CFPs as a diagnostic method and 53 (73.6%) used ophthalmoscopy. Ophthalmoscopy and color fundus photographs are both valid strategies for DR screening. Each method has advantages and potential limitations that include cost, expertise of the examiners, and equipment. The main advantages of ophthalmoscopy are its easy handling and superior performance in cases of poor patient collaboration, on the other hand, it is not sensitive enough to detect minor signs of DR and depends on the presence of a trained operator [106]. In turn, CFPs has the advantage of providing a permanent record of retinopathy, which can be used later to document retinopathy progression and allows for a more detailed grading of retinopathy. Notably, CFPs are expensive [107].
Some studies were carried out in ophthalmology services for the diagnosis of DR, which may represent a selection bias, considering that reference services will likely have a higher rate of patients with complications. Therefore, we performed an analysis excluding the studies conducted in ophthalmology services as shown in Table 2, resulting in a decrease in the prevalence of DR.
Our study has some limitations, the most important being the high heterogeneity. Migliavaca et al. show that prevalence studies have high heterogeneity [108]. The available smaller studies conducted in Brazil are often limited in scope and may uncover confounding or conflicting results due to their small sample size. The heterogeneous nature of studies (e.g., patient selection criteria, diabetes type, setting), disparity between study methods (color fundus photography vs. ophthalmoscopy), and possible differences between urban and rural settings, with variations on the following items: access to healthcare and eating habits [109, 110] may contribute to conflicting reports of prevalence and incidence, making a direct comparison of studies difficult. Most studies did not report visual acuity or the prevalence of maculopathy or proliferative DR, both considered vision-threatening DR. Although the significance of functional outcomes, most epidemiological studies do not address them. Rates of blindness are variable among countries (high-income vs. low- to middle-income countries) depending on the existence of screening programs, specialized workforce, and possibility of timely treatment [111]. Such limitations highlight the need for consistent data capture in Brazil.
Conclusion
This study shows a high heterogeneity that is expected in systematic reviews estimating prevalence rates. It is necessary to develop multicenter studies with representative samples and standardized methodology. Screening programs are effective for the identification of early DR, and epidemiological studies are essential for their success, as they collect data that allows identification of the magnitude of the problem, as well as regional differences. Further research is needed to collect such data in Brazil, with the use of standardized criteria and consistent terminology, and the inclusion of samples that are representative of the communities from which they are drawn. Robust longitudinal collection of patient data will be essential to allow identification of the true extent of diagnosed retinal complications of diabetes, in turn providing healthcare planners with essential information to aid future decision-making.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article and in the Additional files.
Abbreviations
- DR:
-
Diabetic retinopathy
- RoB:
-
Risk of Bias
- HbA1c:
-
Glycated hemoglobin
- CFP:
-
Color fundus photography
References
American Diabetes Association Professional Practice Committee, Draznin B, Aroda VR, Bakris G, Benson G, Brown FM, Freeman R, Green J, Huang E, Isaacs D, Kahan S, Leon J, Lyons SK, Peters AL, Prahalad P, Reusch JEB, Young-Hyman D. 12. Retinopathy, neuropathy, and foot care: standards of medical care in diabetes-2022, Diabetes Care. 2022. 45:S185–S194. https://doi.org/10.2337/dc22-S012.
Teo ZL, Tham Y-C, Yu M, Chee ML, Rim TH, Cheung N, Bikbov MM, Wang YX, Tang Y, Lu Y, Wong IY, Ting DSW, Tan GSW, Jonas JB, Sabanayagam C, Wong TY, Cheng C-Y. Global prevalence of diabetic retinopathy and projection of burden through 2045: systematic review and meta-analysis. Ophthalmology. 2021;128:1580–91. https://doi.org/10.1016/j.ophtha.2021.04.027.
Ben ÂJ, de Souza CF, Locatelli F, Rosses APO, Szortika A, de Araujo AL, de Carvalho G, Lavinsky D, Neyeloff JL, Neumann CR. Health-related quality of life associated with diabetic retinopathy in patients at a public primary care service in southern Brazil. Arch Endocrinol Metab. 2020. https://doi.org/10.20945/2359-3997000000223.
Melo LGN, Morales PH, Drummond KRG, Santos DC, Pizarro MH, Barros BSV, Mattos TCL, Pinheiro AA, Mallmann F, Leal FSL, Muniz LH, Malerbi FK, Gomes MB. Diabetic retinopathy may indicate an increased risk of cardiovascular disease in patients with type 1 diabetes—a nested case-control study in Brazil. Front Endocrinol. 2019;10:689. https://doi.org/10.3389/fendo.2019.00689.
Magliano DJ, Boyko EJ. IDF Diabetes Atlas 10th edition scientific committee, IDF DIABETES ATLAS, International Diabetes Federation, Brussels, 2022. https://www.ncbi.nlm.nih.gov/pubmed/35914061.
Telo GH, Cureau FV, de Souza MS, Andrade TS, Copês F, Schaan BD. Prevalence of diabetes in Brazil over time: a systematic review with meta-analysis. Diabetol Metab Syndr. 2016;8:65. https://doi.org/10.1186/s13098-016-0181-1.
Klein R. The Wisconsin Epidemiologic Study of diabetic retinopathy. Arch Ophthalmol. 1984;102:527. https://doi.org/10.1001/archopht.1984.01040030405011.
Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group, Lancet. 352 (1998) 837–853.
Diabetes Control and Complications Trial Research Group, Nathan DM, Genuth S, Lachin J, Cleary P, Crofford O, Davis M, Rand L, Siebert C. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus, N Engl J Med. 1993; 329: 977–986. https://doi.org/10.1056/NEJM199309303291401.
Preliminary report on effects of photocoagulation therapy. The Diabetic Retinopathy Study Research Group. Am J Ophthalmol. 1976; 81: 383–396. https://doi.org/10.1016/0002-9394(76)90292-0.
Brar AS, Sahoo J, Behera UC, Jonas JB, Sivaprasad S, Das T. Prevalence of diabetic retinopathy in urban and rural India: a systematic review and meta-analysis. Indian J Ophthalmol. 2022;70:1945–55. https://doi.org/10.4103/ijo.IJO_2206_21.
Mumtaz SN, Fahim MF, Arslan M, Shaikh SA, Kazi U, Memon MS. Prevalence of diabetic retinopathy in Pakistan; a systematic review. Pak J Med Sci Q. 2018;34:493–500. https://doi.org/10.12669/pjms.342.13819.
Zhang X, Saaddine JB, Chou C-F, Cotch MF, Cheng YJ, Geiss LS, Gregg EW, Albright AL, Klein BEK, Klein R. Prevalence of diabetic retinopathy in the United States, 2005–2008. JAMA. 2010;304:649–56. https://doi.org/10.1001/jama.2010.1111.
Sasongko MB, Widyaputri F, Agni AN, Wardhana FS, Kotha S, Gupta P, Widayanti TW, Haryanto S, Widyaningrum R, Wong TY, Kawasaki R, Wang JJ. Prevalence of diabetic retinopathy and blindness in Indonesian adults with type 2 diabetes. Am J Ophthalmol. 2017;181:79–87. https://doi.org/10.1016/j.ajo.2017.06.019.
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, Stein C, Basit A, Chan JCN, Mbanya JC, Pavkov ME, Ramachandaran A, Wild SH, James S, Herman WH, Zhang P, Bommer C, Kuo S, Boyko EJ, Magliano DJ. IDF Diabetes Atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183: 109119. https://doi.org/10.1016/j.diabres.2021.109119.
Queiroz MS, de Carvalho JX, Bortoto SF, de Matos MR, das Graças Dias Cavalcante C, Andrade EAS, Correa-Giannella ML, Malerbi FK. Diabetic retinopathy screening in urban primary care setting with a handheld smartphone-based retinal camera. Acta Diabetol. 2020;57:1493–9.
Fernandes AG, Ferraz AN, Brant R, Malerbi FK. Diabetic retinopathy screening and treatment through the Brazilian National Health Insurance. Sci Rep. 2022;12:13941. https://doi.org/10.1038/s41598-022-18054-6.
de Souza EV, de Souza NV, Rodrigues MdLV. Retinopatia diabética em pacientes de um programa de atendimento multidisciplinar do Hospital das Clínicas de Ribeirão Preto—USP. Arq Bras Oftalmol. 2004;67(3):433–6. https://doi.org/10.1590/S0004-27492004000300012.
Escarião PHG, de Arantes TEF, Filho NCF, de Deus Urtiga R, Florêncio TLT, de Andrade Lima Arcoverde AL. Epidemiologia e diferenças regionais da retinopatia diabética em Pernambuco, Brasil. Arq Bras Oftalmol. 2008. https://doi.org/10.1590/s0004-27492008000200008.
Melo LGN, Morales PH, Drummond KRG, Santos DC, Pizarro MH, Barros BSV, Mattos TCL, Pinheiro AA, Mallmann F, Leal FSL, Malerbi FK, Gomes MB. Current epidemiology of diabetic retinopathy in patients with type 1 diabetes: a national multicenter study in Brazil. BMC Public Health. 2018;18:989. https://doi.org/10.1186/s12889-018-5859-x.
de Souza GF, Figueira RM, Alkmim MB, de Sousa LAP, Bonisson L, Ribeiro ALP, Vasconcelos-Santos DV. Teleophthalmology screening for diabetic retinopathy in Brazil: applicability and economic assessment. Telemed J E Health. 2020;26:341–6. https://doi.org/10.1089/tmj.2018.0241.
Schellini SA, de Carvalho GM, Rendeiro FS, Padovani CR, Hirai FE. Prevalence of diabetes and diabetic retinopathy in a Brazilian population. Ophthalmic Epidemiol. 2014;21:33–8. https://doi.org/10.3109/09286586.2013.868004.
Reggi Junior SS, Morales PHA, Ferreira SRG. Existe concordância no acometimento renal e retiniano da microangiopatia diabética? Arq Bras Endocrinol Metabol. 2001;45:452–9. https://doi.org/10.1590/S0004-27302001000500008.
Wilkinson CP, Ferris FL, Klein RE, Lee PP, Agardh CD, Davis M, Dills D, Kampik A, Pararajasegaram R, Verdaguer JT. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology. 2003;110(9):1677–82. https://doi.org/10.1016/S0161-6420(03)00475-5.
Malerbi FK, Melo GB. Feasibility of screening for diabetic retinopathy using artificial intelligence, Brazil. Bull World Health Organ. 2022;100:643–7. https://doi.org/10.2471/BLT.22.288580.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021. https://doi.org/10.1136/bmj.n71.
Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, Baker P, Smith E, Buchbinder R. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65:934–9. https://doi.org/10.1016/j.jclinepi.2011.11.014.
McGuinness L. robvis: A package to quickly visualise risk-of-bias assessment results, Github, n.d. https://github.com/mcguinlu/robvis. Accessed 18 Nov 2022.
Barker TH, Migliavaca CB, Stein C, Colpani V, Falavigna M, Aromataris E, Munn Z. Conducting proportional meta-analysis in different types of systematic reviews: a guide for synthesisers of evidence. BMC Med Res Methodol. 2021;21:189. https://doi.org/10.1186/s12874-021-01381-z.
Alvarenga LS, Martins EN, Grottone GT, Morales PHA, Paranhos A Jr, de Freitas D, Scarpi MJ. Usefulness of corneal esthesiometry for screening diabetic retinopathy. Rev Saude Publica. 2003;37:609–15. https://doi.org/10.1590/s0034-89102003000500010.
de Andrade AJM, de Andrade AJM, Höfling-Lima AL, Yu MCZ, Godoy P, Gompertz OF, de Souza Bonfim S, de Andrade FEM. Estudo da micobiota em conjuntiva sadia de diabéticos, residentes na área urbana da cidade de São Paulo—Brasil. Arq Bras Oftalmol. 2006;69:75–83. https://doi.org/10.1590/s0004-27492006000100015.
de Assis CS, Diniz TG, Alcântara JOS, Brito VPAdS, do Nascimento RAF, Nunes MKDS, Silva AS, de Queiroga Evangelista IW, Viturino MGM, de Lima RLFC, Persuhn DC. Metabolic impact of the VDR rs1544410 in diabetic retinopathy. PLoS ONE. 2022;17: e0263346. https://doi.org/10.1371/journal.pone.0263346.
Cardoso CRL, Leite NC, Muxfeldt ES, Salles GF. Thresholds of ambulatory blood pressure associated with chronic complications in type 2 diabetes. Am J Hypertens. 2012;25:82–8. https://doi.org/10.1038/ajh.2011.168.
Cardoso CRL, Leite NC, Dib E, Salles GF. Predictors of development and progression of retinopathy in patients with type 2 diabetes: importance of blood pressure parameters. Sci Rep. 2017;7:4867. https://doi.org/10.1038/s41598-017-05159-6.
Cardoso CRL, Leite NC, Salles GF. Differential effects of treatment targets on risks of adverse outcomes according to diabetes duration, age and complications: Can these characteristics be used to individualize diabetes treatment? The Rio de Janeiro type 2 diabetes cohort. J Diabetes Complications. 2022;36: 108124. https://doi.org/10.1016/j.jdiacomp.2021.108124.
Chacon DdA, de Araújo Chacon D, da Silva Magalhães Chaves AD, Duarte RA, de Amorim Garcia CA, da Cunha Medeiros A. Achados da fundoscopia e alterações do pé diabético em pacientes do Hospital Universitário Onofre Lopes/UFRN. Acta Cir Bras. 2005;20:3–7. https://doi.org/10.1590/s0102-86502005000700002.
Chen-Ku CH, Gonzalez-Galvez G, Vásquez M, Fuente G, Nakazone MA, Silva AI, de Sa Pereira MH. vascular complications in patients with type 2 diabetes: prevalence and comorbidities in 6 countries of Latin America (a cohort of the discover study program). Endocr Pract. 2019;25(10):994–1002. https://doi.org/10.4158/EP-2018-0473.
Dantas da Costa e Silva ME, Polina ER, Crispim D, Sbruzzi RC, Lavinsky D, Mallmann F, Martinelli NC, Canani LH, Dos Santos KG. Plasma levels of miR-29b and miR-200b in type 2 diabetic retinopathy. J Cell Mol Med. 2019;23:1280–7. https://doi.org/10.1111/jcmm.14030.
Costa LA, Canani LH, Lisbôa HRK, Tres GS, Gross JL. Aggregation of features of the metabolic syndrome is associated with increased prevalence of chronic complications in Type 2 diabetes. Diabet Med. 2004;21:252–5. https://doi.org/10.1111/j.1464-5491.2004.01124.x.
DePaula AL, Stival A, Halpern A, Vencio S. Thirty-day morbidity and mortality of the laparoscopic ileal interposition associated with sleeve gastrectomy for the treatment of type 2 diabetic patients with BMI <35: an analysis of 454 consecutive patients. World J Surg. 2011;35:102–8. https://doi.org/10.1007/s00268-010-0799-3.
Dieter C, Lemos NE, de Faria Corrêa NR, Pellenz FM, Canani LH, Crispim D, Bauer AC. The A allele of the rs759853 single nucleotide polymorphism in the AKR1B1 gene confers risk for diabetic kidney disease in patients with type 2 diabetes from a Brazilian population. Arch Endocrinol Metab. 2022. https://doi.org/10.20945/2359-3997000000432.
Esteves JF, Kramer CK, de Azevedo MJ, Stolz AP, Roggia MF, Larangeira A, Miozzo SA, Rosa C, Lambert JH, Pecis M, Rodrigues TC, Canani LHS. Prevalence of diabetic retinopathy in patients with type 1 diabetes mellitus. Rev Assoc Med Bras. 2009;55:268–73. https://doi.org/10.1590/s0104-42302009000300017.
Felício JS, Pacheco JT, Ferreira SR, Plavnik F, Moisés V, Junior OK, Ribeiro AB, Zanella MT. Impaired reduction of nocturnal systolic blood pressure and severity of diabetic retinopathy. Exp Clin Cardiol. 2007;12:157–60.
Fernandez MLMP, Moura CAA, Jorge PT. Estudo de prevalência de retinopatia diabética no ambulatório da Universidade Federal de Uberlândia / Prevalence study of diabetic retinopathy in the ambulatory of Universidade Federal de Uberlandia. Arq Bras Endocrinol Metabol. 1998;42:368–73.
Foss MC, Paccola GMGF, de Souza NV, Iazigi N. Estudo analítico de uma amostra populacional de diabéticos tipo II da regiäo de Ribeirão Preto (SP) / Analytic study in a population sample of diabetic patients type II from Ribeiräo Preto area (São Paulo). AMB Rev Assoc Med Bras. 1989;35:179–83.
Galvão FM, Silva YP, de Resende MIL, Barbosa FR, Martins TA, Carneiro LB. Prevalência e fatores de risco para retinopatia diabética em pacientes diabéticos atendidos por demanda espontânea: um estudo transversal. Rev Bras Oftalmol. 2021. https://doi.org/10.37039/1982.8551.20210006.
Gomes MB, Calliari LE, Conte D, Correa CL, Drummond KRG, Mallmann F, Pinheiro AA, Muniz LH, Leal FSL, Morales PH, Negrato CA. Diabetes-related chronic complications in Brazilian adolescents with type 1 diabetes. A multicenter cross-sectional study. Diabetes Res Clin Pract. 2021;177: 108895. https://doi.org/10.1016/j.diabres.2021.108895.
Gomes MB, Lucchetti MR, Gazzola H, Dimetz T, Gonçalves MF, Neves R, Matos H. Microalbuminuria and associated clinical features among Brazilians with insulin dependent diabetes mellitus. Diabetes Res Clin Pract. 1997;35:143–7. https://doi.org/10.1016/s0168-8227(97)01368-5.
Gomes MB, Giannella-Neto D, Faria M, Tambascia M, Fonseca RM, Rea R, Macedo G, Modesto-Filho J, Schmid H, Bittencourt AV, Cavalcanti S, Rassi N, Pedrosa H, Dib SA. Estimating cardiovascular risk in patients with type 2 diabetes: a national multicenter study in Brazil. Diabetol Metab Syndr. 2009;1:22. https://doi.org/10.1186/1758-5996-1-22.
Greca LF, Pinto LC, Rados DR, Canani LH, Gross JL. Clinical features of patients with type 2 diabetes mellitus and hepatitis C infection. Braz J Med Biol Res. 2012;45:284–90. https://doi.org/10.1590/s0100-879x2012007500013.
Gross JL, Stein AC, Beck MO, Fuchs SC, Silveiro SP, de-Azevedo MJ, Friedman R. Risk factors for development of proteinuria by type II (non-insulin dependent) diabetic patients. Braz J Med Biol Res. 1993;26:1269–78.
Guedes MF, Portes AJF, de Souza Couto Junior A, dos Santos Nunes J, Oliveira RCC. Prevalência da retinopatia diabética em unidade do Programa de Saúde da Família. Rev Bras Oftalmol. 2009;68:90–5. https://doi.org/10.1590/s0034-72802009000200005.
Hirata CL, Fang T, Casella AMB, Eliezer M, Abujarnra S. Prevalência de retinopatia em uma população de diabéticos. Arq Bras Oftalmol. 1986;49:31–3.
Hissa MN, D’Almeida JAC, Cremasco F, de Bruin VMS. Event related P300 potential in NIDDM patients without cognitive impairment and its relationship with previous hypoglycemic episodes. Neuro Endocrinol Lett. 2002;23:226–30.
Hokazono K, Belizário FS, Portugal V, Messias-Reason I, Nisihara R. Mannose binding lectin and pentraxin 3 in patients with diabetic retinopathy. Arch Med Res. 2018;49:123–9. https://doi.org/10.1016/j.arcmed.2018.06.003.
Jost BS, Hilgemberg É, Rodrigues EB, Daniotti AF, Bonamigo EL. Prevalência de retinopatia diabética na população portadora de diabetes mellitus tipo 2 do município de Luzerna—SC. Arq Bras Oftalmol. 2010;73:259–65. https://doi.org/10.1590/s0004-27492010000300010.
Junior SSR, Morales PHA, Ferreira SRG. Existe concordância no acometimento renal e retiniano da microangiopatia diabética? Arq Bras Endocrinol Metabol. 2001;45:452–9. https://doi.org/10.1590/s0004-27302001000500008.
Kramer CK, Leitão CB, Canani LH, Gross JL. Afternoon blood pressure increase: a blood pressure pattern associated with microvascular complications in type 2 diabetes mellitus. Am J Hypertens. 2011;24:64–9. https://doi.org/10.1038/ajh.2010.202.
Kramer CK, Leitão CB, Canani LH, Ricardo ED, Pinto LC, Valiatti FB, Gross JL. Late afternoon blood pressure increase is associated with diabetic retinopathy in normotensive type 2 diabetes mellitus patients. Diabetes Res Clin Pract. 2009;84:e12–4. https://doi.org/10.1016/j.diabres.2008.12.016.
Kramer CK, Leitão CB, Azevedo MJ, Valiatti FB, Rodrigues TC, Canani LH, Gross JL. Diabetic retinopathy is associated with early autonomic dysfunction assessed by exercise-related heart rate changes. Braz J Med Biol Res. 2008;41:1110–5. https://doi.org/10.1590/s0100-879x2008001200011.
Lima CGMG, Franco LJ, Dal Fabbro AL, Martinez EZ, Veira-Filho JPB, Ventura AACM, Prevelato L, Cruz AAV. Diabetic retinopathy among Brazilian Xavante Indians. Diabetol Metab Syndr. 2018;10:46. https://doi.org/10.1186/s13098-018-0348-z.
Lima CF, Morais IH, Suckow K, Nisihara R, Skare T. Nailfold capillaroscopy and microvascular involvement in Diabetes Mellitus. Sci Med. 2021;31: e39679. https://doi.org/10.15448/1980-6108.2021.1.39679.
Korn Malerbi F, Lelis Dal Fabbro A, Botelho Vieira Filho JP, Franco LJ. The feasibility of smartphone based retinal photography for diabetic retinopathy screening among Brazilian Xavante Indians. Diabetes Res Clin Pract. 2020;168: 108380. https://doi.org/10.1016/j.diabres.2020.108380.
Malerbi FK, Mendes G, Barboza N, Morales PH, Montargil R, Andrade RE. Diabetic macular edema screened by handheld smartphone-based retinal camera and artificial intelligence. J Med Syst. 2021;46:8. https://doi.org/10.1007/s10916-021-01795-8.
Malerbi FK, Andrade RE, Morales PH, Stuchi JA, Lencione D, de Paulo JV, Carvalho MP, Nunes FS, Rocha RM, Ferraz DA, Belfort R Jr. Diabetic retinopathy screening using artificial intelligence and handheld smartphone-based retinal camera. J Diabetes Sci Technol. 2022;16:716–23. https://doi.org/10.1177/1932296820985567.
Martins EN, Alvarenga LS, Höfling-Lima AL, Freitas D, Zorat-Yu MC, Farah ME, Mannis MJ. Aerobic bacterial conjunctival flora in diabetic patients. Cornea. 2004;23:136–42. https://doi.org/10.1097/00003226-200403000-00006.
Massaro JD, Polli CD, Silva MC, Alves CC, Passos GA, Sakamoto-Hojo ET, de Holanda Miranda WR, Cezar NJB, Rassi DM, Crispim F, Dib SA, Foss-Freitas MC, Pinheiro DG, Donadi EA. Post-transcriptional markers associated with clinical complications in Type 1 and Type 2 diabetes mellitus. Mol Cell Endocrinol. 2019;490:1–14. https://doi.org/10.1016/j.mce.2019.03.008.
Massignam ET, Dieter C, Pellenz FM, Assmann TS, Crispim D. Involvement of miR-126 rs4636297 and miR-146a rs2910164 polymorphisms in the susceptibility for diabetic retinopathy: a case–control study in a type 1 diabetes population. Acta Ophthalmol. 2021;99:e461–9. https://doi.org/10.1111/aos.14638.
da Mata AR, Álvares J, Diniz LM, da Silva MRR, dos Santos BRA, Júnior AAG, Cherchiglia ML, Andrade EIG, Godman B, de Assis Acurcio F. Quality of life of patients with diabetes mellitus types 1 and 2 from a referral health centre in Minas Gerais, Brazil. Expert Rev Clin Pharmacol. 2016;9:739–46. https://doi.org/10.1586/17512433.2016.1152180.
Mori RC, Santos-Bezerra DP, Pelaes TS, Admoni SN, Perez RV, Monteiro MB, Machado CG, Queiroz MS, Machado UF, Correa-Giannella ML. Variants in HSD11B1 gene modulate susceptibility to diabetes kidney disease and to insulin resistance in type 1 diabetes. Diabetes Metab Res Rev. 2021;37: e3352. https://doi.org/10.1002/dmrr.3352.
Mota PR, Daher EF, Silva GB, Lima JWO, Libório AB, Forti AC. Coronary artery disease associated with low-grade albuminuria in type 2 diabetes mellitus, Hong Kong. J Nephrol. 2011;13:27–32. https://doi.org/10.1016/S1561-5413(11)60004-5.
Parisi MCR, Moura Neto A, Menezes FH, Gomes MB, Teixeira RM, de Oliveira JEP, Pereira JRD, Fonseca RMC, Guedes LBA, Costa e Forti A, de Oliveira AMA, de Medeiros Nóbrega MB, Colares VNQ, Schmid H, Nienov OH, Nery M, Fernandes TD, Pedrosa HC, Schreiber de Oliveira CS, Ronsoni M, Rezende KF, Quilici MTV, Vieira AEF, de Macedo GMC, Stuchi-Perez EG, Dinhane KGI, Pace AE, de Freitas MCF, Calsolari MR, Saad MJA. Baseline characteristics and risk factors for ulcer, amputation and severe neuropathy in diabetic foot at risk: the BRAZUPA study. Diabetol Metab Syndr. 2016;8:25. https://doi.org/10.1186/s13098-016-0126-8.
Pedrosa DR, Lemos EO, Gonçalves DCA, Ranieri PSG, Pires CAA, Paiva VR. Prevalência de retinopatia diabética em pacientes atendidos pela Estratégia Saúde da Família no município de Ananindeua—PA. Rev Bras Med Fam Comunidade. 2012;8:58–63. https://doi.org/10.5712/rbmfc8(26)394.
Penido R, Nascentes L, Rocha SVM. Incidência de retinopatia diabética em uma associação de diabéticos. Rev Bras Oftalmol. 2001;60:375–8.
Piccirillo LJ, Cunha EF, Gonçalves MdFR, Clemente ELS, Neves R, Gomes MdB. Microalbuminúria em pacientes diabéticos tipo 1: prevalência e fatores associados. Arq Bras Endocrinol Metabol. 2002;46:640–7. https://doi.org/10.1590/S0004-27302002000600007.
Polina ER, Oliveira FM, Sbruzzi RC, Crispim D, Canani LH, Santos KG. Gene polymorphism and plasma levels of miR-155 in diabetic retinopathy. Endocr Connect. 2019;8:1591–9. https://doi.org/10.1530/EC-19-0446.
Preti RC, Motta AAL, Maia OdO Jr, Morita C, Nascimento VP, Monteiro MLR, Takahashi WY. Relationship between diabetic retinopathy severity and the timespan between the endocrinopathy diagnosis and the first ophthalmic examination. Arq Bras Oftalmol. 2010;73:240–3. https://doi.org/10.1590/s0004-27492010000300006.
Rodrigues TC, Pecis M, Canani LH, Schreiner L, Kramer CK, Biavatti K, Macedo B, Esteves JF, Azevedo MJ. Caracterização de pacientes com diabetes mellitus tipo 1 do sul do Brasil: complicações crônicas e fatores associados. Rev Assoc Med Bras. 2010;56:67–73. https://doi.org/10.1590/s0104-42302010000100019.
Rodrigues KF, Pietrani NT, Sandrim VC, Vieira CMAF, Fernandes AP, Bosco AA, Gomes KB. Association of a large panel of cytokine gene polymorphisms with complications and comorbidities in type 2 diabetes patients. J Diabetes Res. 2015;2015: 605965. https://doi.org/10.1155/2015/605965.
da Rosa LCGF, Zajdenverg L, Souto DL, Dantas JR, Pinto MVR, de Salles GFdCM, Rodacki M. HbA1c variability and long-term glycemic control are linked to diabetic retinopathy and glomerular filtration rate in patients with type 1 diabetes and multiethnic background. J Diabetes Complications. 2019;33:610–5. https://doi.org/10.1016/j.jdiacomp.2019.05.022.
Rosses APO, Ben ÂJ, de Souza CF, Skortika A, de Araújo AL, de Carvalho G, Locatelli F, Neumann CR. Diagnostic performance of retinal digital photography for diabetic retinopathy screening in primary care. Fam Pract. 2017;34:546–51. https://doi.org/10.1093/fampra/cmx020.
Sampaio E, Almeida HGG, Delfino VDA. Nefropatia e retinopatia em diabéticos do tipo 1 de um programa de atendimento multiprofissional universitário. Arq Bras Endocrinol Metabol. 2007;51:410–8. https://doi.org/10.1590/S0004-27302007000300008.
Santos KG, Tschiedel B, Schneider JR, Souto KEP, Roisenberg I. Prevalence of retinopathy in Caucasian type 2 diabetic patients from the South of Brazil and relationship with clinical and metabolic factors. Braz J Med Biol Res. 2005;38:221–5. https://doi.org/10.1590/s0100-879x2005000200010.
dos Santos KG, Canani LH, Gross JL, Tschiedel B, Pires Souto KE, Roisenberg I. The -374A allele of the receptor for advanced glycation end products gene is associated with a decreased risk of ischemic heart disease in African-Brazilians with type 2 diabetes. Mol Genet Metab. 2005;85:149–56.
Scheffel RS, Kramer CK, Rados DV, Pinto LC, Crispim D, Gross JL, Canani LH. The prevalence of chronic diabetic complications and metabolic syndrome is not associated with maternal type 2 diabetes. Braz J Med Biol Res. 2008;41:1123–8. https://doi.org/10.1590/S0100-879X2008001200013.
Schmid H, Schaan B, Cecconello F, Maestri T, Neumann C. Proliferative diabetic retinopathy is related to cardiovascular autonomic neuropathy in non-insulin-dependent diabetes mellitus. Diabetes Res Clin Pract. 1995;29:163–8. https://doi.org/10.1016/0168-8227(95)01120-x.
Serfaty FM, Dantas JR, Almeida MH, Duarte JDG, Kupfer R, Campos F, Zajdenverg L, Milech A, Rodacki M, de Oliveira JEP. Implicações clínicas da persistência de anti-GAD positivo e peptídeo C detectável em pacientes com diabetes melito tipo 1 de longa duração. Arq Bras Endocrinol Metabol. 2010;54:449–54. https://doi.org/10.1590/s0004-27302010000500004.
Steck AD, de Figueiredo Esteves R, de Miranda Gonçalves JC. Prevalência de retinopatia diabética em uma população de diabéticos do HC de Franco da Rocha—SP. Arq Bras Oftalmol. 1993. https://doi.org/10.5935/0004-2749.19930035.
Sugano DM, Serra DC, Canovas R, Barros RA, Rehder JRCL. Impacto da retinopatia diabética em campanha de prevenção da cegueira, Fundação ABC. 2001.
de Syllos RWC, Sandrim VC, Lisboa HRK, Tres GS, Tanus-Santos JE. Endothelial nitric oxide synthase genotype and haplotype are not associated with diabetic retinopathy in diabetes type 2 patients. Nitric Oxide. 2006;15:417–22. https://doi.org/10.1016/j.niox.2006.02.002.
Tres GS, Lisbôa HRK, Syllos R, Canani LH, Gross JL. Prevalence and characteristics of diabetic polyneuropathy in Passo Fundo, South of Brazil. Arq Bras Endocrinol Metabol. 2007;51:987–92. https://doi.org/10.1590/s0004-27302007000600014.
Viégas M, Costa C, Lopes A, Griz L, Medeiro MA, Bandeira F. Prevalence of osteoporosis and vertebral fractures in postmenopausal women with type 2 diabetes mellitus and their relationship with duration of the disease and chronic complications. J Diabetes Complications. 2011;25:216–21. https://doi.org/10.1016/j.jdiacomp.2011.02.004.
Wobeto VPA, Rosim ET, Melo MB, Calliari LEP, Sonaati MdF. Haptoglobin polymorphism and diabetic retinopathy in Brazilian patients. Diabetes Res Clin Pract. 2007;77(3):385–8. https://doi.org/10.1016/j.diabres.2006.12.018.
Wolosker N, Rosoky RM, Muraco Neto B, Langer B. Maintenance treatment of diabetic patients, associating arterial obstructive tibio-peroneal disease. Sao Paulo Med J. 1995;113(1):701–5. https://doi.org/10.1590/S1516-31801995000100007.
de Oliveira GMM, Brant LCC, Polanczyk CA, Malta DC, Biolo A, Nascimento BR, de Souza MdFM, Lorenzo ARD, Fagundes Júnior AAdP, Schaan BD, de Castilho FM, Cesena FHY, Soares GP, Xavier Junior GF, Barreto Filho JAS, Passaglia LG, Pinto Filho MM, Machline-Carrion MJ, Bittencourt MS, Pontes Neto OM, Villela PB, Teixeira RA, Sampaio RO, Gaziano TA, Perel P, Roth GA, Ribeiro ALP. Cardiovascular statistics—Brazil 2021. Arq Bras Cardiol. 2022; 118:115–373. https://doi.org/10.36660/abc.20211012.
Song P, Yu J, Chan KY, Theodoratou E, Rudan I. Prevalence, risk factors and burden of diabetic retinopathy in China: a systematic review and meta-analysis. J Glob Health. 2018. https://doi.org/10.7189/jogh.08.010803.
Burgess PI, MacCormick IJC, Harding SP, Bastawrous A, Beare NAV, Garner P. Epidemiology of diabetic retinopathy and maculopathy in Africa: a systematic review. Diabet Med. 2013;30:399–412. https://doi.org/10.1111/j.1464-5491.2012.03756.x.
Li JQ, Welchowski T, Schmid M, Letow J, Wolpers C, Pascual-Camps I, Holz FG, Finger RP. Prevalence, incidence and future projection of diabetic eye disease in Europe: a systematic review and meta-analysis. Eur J Epidemiol. 2020;35:11–23. https://doi.org/10.1007/s10654-019-00560-z.
Zoungas S, Woodward M, Li Q, Cooper ME, Hamet P, Harrap S, Heller S, Marre M, Patel A, Poulter N, Williams B, Chalmers J. ADVANCE Collaborative group, Impact of age, age at diagnosis and duration of diabetes on the risk of macrovascular and microvascular complications and death in type 2 diabetes. Diabetologia. 2014;57:2465–74. https://doi.org/10.1007/s00125-014-3369-7.
Liu DP, Molyneaux L, Chua E, Wang YZ, Wu CR, Jing H, Hu LN, Liu YJ, Xu ZR, Yue DK. Retinopathy in a Chinese population with type 2 diabetes: factors affecting the presence of this complication at diagnosis of diabetes. Diabetes Res Clin Pract. 2002;56:125–31. https://doi.org/10.1016/s0168-8227(01)00349-7.
Voigt M, Schmidt S, Lehmann T, Köhler B, Kloos C, Voigt UA, Meller D, Wolf G, Müller UA, Müller N. Prevalence and progression rate of diabetic retinopathy in type 2 diabetes patients in correlation with the duration of diabetes. Exp Clin Endocrinol Diabetes. 2018;126:570–6. https://doi.org/10.1055/s-0043-120570.
M. Neri, Mapa da Nova Pobreza. FGV Social. 2022. https://cps.fgv.br/MapaNovaPobreza Accessed 30 Jan 2023.
Costa AF, Flor LS, Campos MR, de Oliveira AF, Costa MdFdS, da Silva RS, Lobato LCdP, Schramm JMdA. Carga do diabetes mellitus tipo 2 no Brasil. Cad Saúde Pública. 2017. https://doi.org/10.1590/0102-311X00197915.
Dantas MNP, de Souza DLB, de Souza AMG, Aiquoc KM, de Souza TA, Barbosa IR. Fatores associados ao acesso precário aos serviços de saúde no Brasil. Rev Bras Epidemiol. 2020. https://doi.org/10.1590/1980-549720210004.
Photocoagulation for diabetic macular edema: early treatment diabetic retinopathy study report no. 4. The Early Treatment Diabetic Retinopathy Study Research Group. Int Ophthalmol Clin. 1987;27: 265–272. https://doi.org/10.1097/00004397-198702740-00006.
Kinyoun JL, Martin DC, Fujimoto WY, Leonetti DL. Ophthalmoscopy versus fundus photographs for detecting and grading diabetic retinopathy. Invest Ophthalmol Vis Sci. 1992;33:1888–93.
Moss SE, Klein R, Kessler SD, Richie KA. Comparison between ophthalmoscopy and fundus photography in determining severity of diabetic retinopathy. Ophthalmology. 1985;92:62–7. https://doi.org/10.1016/s0161-6420(85)34082-4.
Borges Migliavaca C, Stein C, Colpani V, Barker TH, Munn Z, Falavigna M. How are systematic reviews of prevalence conducted? A methodological study. BMC Med Res Methodol. 2020. https://doi.org/10.1186/s12874-020-00975-3.
Costa DVdP, Lopes MS, Mendonça RdD, Malta DC, de Freitas PP, Lopes ACS. Diferenças no consumo alimentar nas áreas urbanas e rurais do Brasil: Pesquisa Nacional de Saúde. Ciênc Saúde Coletiva. 2021;26:3805–13. https://doi.org/10.1590/1413-81232021269.2.26752019.
Arruda NM, Maia AG, Alves LC. Desigualdade no acesso à saúde entre as áreas urbanas e rurais do Brasil: uma decomposição de fatores entre 1998 a 2008. Cad Saude Publica. 2018. https://doi.org/10.1590/0102-311x00213816.
Vujosevic S, Aldington SJ, Silva P, Hernández C, Scanlon P, Peto T, Simó R. Screening for diabetic retinopathy: new perspectives and challenges. Lancet Diabetes Endocrinol. 2020;8:337–47. https://doi.org/10.1016/S2213-8587(19)30411-5.
Acknowledgements
Not applicable.
Funding
This work was supported by Research Incentive Fund (FIPE) of the Hospital de Clínicas de Porto Alegre and Graduate Program in Medical Sciences: Endocrinology from the Federal University of Rio Grande do Sul, Medical School. This study was partially funded by the Coordination for the Improvement of Higher Education Personnel—Brasil (CAPES)—Finance Code 001, National Council for Scientific and Technological Development (CNPq), Institute for Assessment of Technology in Health (IATS), and Foundation for Research Support of the state of Rio Grande do Sul.
Author information
Authors and Affiliations
Contributions
TAC: Conceptualization, methodology, data curation; MAR: Conceptualization, methodology, data curation, writing—original draft. LAL; ANG; LPS: Methodology, data curation. FKM; GBM; BDS: Conceptualization, supervision, writing—reviewing and editing. MAR, is the guarantor of this work and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors have reviewed the final version of the manuscript and agree with the publication of the results presented.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Table S1. Literature search strategy used.
Additional file 2.
Figure S1. Forest plot representing diabetic retinopathy prevalence rates by duration of diabetes.
Additional file 3.
Figure S2. Forest plot representing diabetic retinopathy prevalence rates by diabetes type.
Additional file 4.
Figure S3. Forest plot representing diabetic retinopathy prevalence rates by study publication year.
Additional file 5.
Figure S4. Forest plot representing diabetic retinopathy prevalence rates by diagnostic method.
Additional file 6.
Figure S5. Risk of bias assessment in the included studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chagas, T.A., dos Reis, M.A., Leivas, G. et al. Prevalence of diabetic retinopathy in Brazil: a systematic review with meta-analysis. Diabetol Metab Syndr 15, 34 (2023). https://doi.org/10.1186/s13098-023-01003-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-023-01003-2