Abstract
Background
Hyperglycemia in pregnancy (HIP) is suggested to be a risk factor for elevated blood pressure (BP) in offspring. However, the empirical evidence was mixed. Thus, this systematic review and meta-analysis was conducted to synthesize current evidence assessing the association between HIP and BP in offspring.
Methods
We searched PubMed, MEDLINE, and Embase to identify articles published from inception until 9 February 2021. A random-effects meta-analysis was performed to calculate a pooled effect size and 95% confidence interval (CI). Furthermore, the effects were evaluated separately while grouping by the offspring’s sex, region, economic level, published year, insulin treatment status, and BP measurement. Each article was independently reviewed for quality.
Results
Of 3385 citations identified, 23 studies involving 88695 offspring were included. The study found that the offspring of women with HIP had an increased level of both systolic blood pressure (SBP; mean difference 1.90, 95% CI 1.09 to 2.70 mmHg, P < 0.001) and diastolic blood pressure (DBP; mean difference 0.87 mmHg, 95% CI 0.11 to 1.17 mmHg, P = 0.02) compared with those whose mothers with normal blood glucose during pregnancy. According to subgroup analyses, gestational diabetes mellitus (GDM) appeared to have varied impacts on offspring BP by sex of offspring, region and economic level of family, published year, maternal insulin treatment status, and BP measurement.
Conclusion
Current evidence showed that HIP was associated with an elevated BP in offspring. Prenatal interventions targated on reducing HIP might be beneficial for controlling for offspring BP.
Similar content being viewed by others
Introduction
Hyperglycemia in pregnancy (HIP) is a kind of hyperglycemia first detected at any time during pregnancy. It can be categorized into two subtypes: one is diabetes mellitus in pregnancy (DIP), including type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM); another is gestational diabetes mellitus (GDM), encompassing pre-existing and developed diabetes during pregnancy [1, 2]. HIP is a prevalent medical complication during gestation [3]. According to the survey conducted by the International Diabetes Federation, over 21.1 million (16.7%) live births to women had HIP worldwide in 2021, with 80.3% of GDM among identified HIP [4]. Meanwhile, the prevalence of GDM varies worldwide, ranging from 6.6% in Japan and Nepal to 45.3% in the United Arab Emirates, and it is expected to rise in most countries [5,6,7,8,9,10].
A growing body of epidemiologic evidence suggested that HIP was associated with a cluster of long- and short-term adverse maternal outcomes, including preeclampsia, gestational hypertension, and T2DM [11, 12]. Apart from its direct risks to mothers, HIP has also been found to be associated with adverse fetal and neonatal outcomes, such as neonatal metabolic disturbances, fetal macrosomia, stillbirth, and other complications [13, 14]. Studies have shown that the absolute risk of these short-term neonatal consequences in family with GDM mothers ranged from 1.8% for shoulder dystocia to 16.6% for neonatal adiposity [15]. Although HIP may disappear after pregnancy [16], its harm to the next generation could be long-lasting. For instance, a population-based study with 40 years of follow-up found that the offspring of diabetic mothers had a 29% higher rate of early-onset cardiovascular disease [17]. A longitudinal study revealed positive associations between maternal glucose levels and child adiposity [18].
Abundant research indicates that women with HIP provide a fetal environment that may enhance offspring susceptibility to various chronic diseases and contribute to the progression of complex chronic diseases in offspring[19, 20]. Among these diseases, high blood pressure (BP), defined as an increase in arterial systolic and/or diastolic blood pressure at rest, is one of the major chronic diseases threatening human health. The positive association between maternal GDM and offspring BP has been repetitively indicated in recent years and has attracted increasing attention from researchers [6, 17, 18, 21]. Such association has been confirmed by a meta-analysis published in 2012. Aceti, et al. This study demonstrated the association between maternal diabetes and offspring systolic BP from thirteen cohort studies by comparing BP of offspring born to diabetic mothers with that of controls, independent of the obesity [22].
Despite the previously established evidence, it is still necessary to update the original article considering a surge in literature after 2012 [22]. In addition, neither the methodological quality nor the clinical outcomes have been systematically and thoroughly summarized, and the overall evidence remains inconclusive. Therefore, the correlation between HIP and offspring BP should be further synthesized based on an updated analysis. A systematic review and meta-analysis was conducted in the present study to assess the potential association of maternal hyperglycemia and BP in the offspring. If possible, the potential factors moderating the correlation between HIP and offspring BP were also explored.
Methods
This systematic review and meta-analysis was undertaken following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [23] and Meta-analyses Of Observational Studies in Epidemiology (MOOSE) guidelines [24]. The review protocol was preregistered in PROSPERO (CRD 42021236328).
Search strategy and study selection
Two researchers (XZ and YW) independently conducted a literature search in PubMed, MEDLINE, and Embase by utilizing search terms including gestational diabetes (gestational diabetes or GDM or pregnancy glycemic index or Pregnancy-Induced Diabetes), blood pressure (blood pressure or hypertension), and children (children or adolescents or offspring) from inception until 9 February 2021. In addition, reference lists of included papers and related systematic reviews were further gone through to identify eligible sources. No language or geographic restrictions were applied. It was limited to human studies that excluded twins. The detailed search strategies are listed in Text S1, Additional file 1.
The inclusion criteria were: (i) cohort study design; (ii) studies that explored the effects of HIP on offspring SBP and DBP. The exclusion criteria were: (i) papers without full text; (ii) animal studies, randomized-controlled trials, cross-sectional studies, non-in vitro studies, or non-original studies (i.e., reviews, case reports, and protocols); (iii) studies with incomplete or insufficient data; (iv) multiple publications of the same research. When the same cohort was recruited in several studies, the one with the most comprehensive results or the largest sample size was consistently selected.
After removing duplicates from different electronic databases, two researchers (XZ and YW) independently screened the titles and abstracts of retrieved records, followed by a full-text review. Researchers resolved disagreements through discussion until they reached a consensus.
Data extraction
The following data were extracted from each of the included studies: (i) Study characteristics: first author, published year, study setting, and study design; (ii) Maternal diabetes type, definition, screening method, and treatment; (iii) Child BP measurement and the outcomes of offspring, which were classified by study location, World Health Organization (WHO) region [25], World Bank (WB) income region [26], sex, BP measurement, and insulin treatment. It is worth mentioning that the data from some retrieved studies were derived from a previous review [22]. Two reviewers (XZ, YW) independently extracted data from the included articles. Another reviewer (XY) further discussed the discrepancies until a consensus was achieved.
Quality assessment
NIH Quality Assessment Tool for Observational Cohort and Cross-sectional Studies (National Heart, Lung, and Blood Institute) was utilized to evaluate the methodological quality of the included studies [6]. The assessment is based on 14 criteria focusing on the key concepts of internal validity, with a total score of 14 points. Based on the overall quality points, included studies were categorized into low- (≤ five points), medium- (six to nine points), and high-quality groups (≥ ten points). Researchers resolved disagreements through discussion.
Data synthesis and analysis
Two researchers (YZ and YW) analyzed the association between HIP and offspring BP using Review Manager (RevMan) 5.3. Specifically, HIP was identified by WHO standardized diagnostic criteria [27], that is, classified as following (i) or (ii): (i) DIP: an elevated fasting plasma glucose (≥ 7.0 mmol/l), or a 2-h plasma glucose ≥ 11.1 mmol/l following a 75 g oral glucose load, or a random plasma glucose ≥ 11.1 mmol/l in the presence of diabetes symptoms; (ii) GDM: fasting plasma glucose 5.1–6.9 mmol/l, a 1 h plasma glucose ≥ 10.0 mmol/l following a 75 g oral glucose load, or a 2 h plasma glucose 8.5–11.0 mmol/l following a 75 g oral glucose load. The SBP and DBP were analyzed separately to assess the offspring’s BP levels. Since the outcome indexes (SBP and DBP) of this study were continuous variables, the mean difference (MD) between the offspring of diabetic mothers versus their controls and 95% confidence interval (CI) of MD were used to estimate the association.
The heterogeneity among studies was evaluated using Cochran’s Q test and the I2 statistic, defining a statistically significant heterogeneity as P-value < 0.05 or I2 ≥ 50%. A fixed-effect model was performed on the condition that no statistically significant heterogeneity was presented; otherwise, the random-effects model was utilized to offer more conservative estimations. Thus, all studies were analyzed with a random-effects model in this study to determine the estimated effect [28]. The pooled difference was weighed by the inverse of its variance to take the cross-studies variance into account [29].
Meanwhile, meta-regression and subgroup analyses were performed to analyze potential sources of heterogeneity. Subgroup analyses were carried out based on sex, WHO region, the WB income region, published year, insulin treatment, and BP measurement. To investigate a proximate time trend, the studies were divided roughly and equally into two groups based on the number of publications, using 2010 as the cut-off year. BP measurement data were divided according to manual or digital methods. A funnel plot was generated, of which symmetry suggested no evidence of publication bias. To evaluate the stability of the main analysis, a sensitivity analysis was carried out by sequential removal of each study from the analysis. It is deemed that statistical significance at a P-value < 0.05, and all P-values were two-tailed. The pooled results were all presented in the forest plot where the significant difference exists when the 95% CI of studies overlap with the y-axis [30].
Result
Study selection
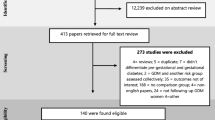
As outlined in Fig. 1, our initial literature search identified a total of 3385 records. After the removal of duplicates, 2362 records were screened by title and abstract, leaving 50 potentially eligible records for full-text review. Finally, the search yielded 23 studies for data extraction (Fig. 1 and Table S1 in Additional file 1).
Study characteristics
All included studies in this systematic review and meta-analysis were cohort studies [18, 21, 31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51], of which 20 [18, 21, 32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47, 49, 51] were described as prospective cohorts and 3 [31, 48, 50] were retrospective studies. Complete data on offspring SBP were available from 20 studies [18, 21, 31,32,33,34,35,36,37,38,39, 41,42,43,44, 46,47,48, 50, 51] and on DBP from 18 studies [18, 21, 31,32,33,34,35,36,37,38,39, 41, 42, 44, 46,47,48, 50]. In addition, one of the included studies [36] had two cohorts and the other one [42] included three. Apart from the data on GDM and offspring BP, authors provided separate data for T1DM in five original studies [39, 41, 44, 46, 50] and T2DM in one study [32], respectively. The regions included were the European Region (EUR; n = 9, 39.1%), Eastern Mediterranean Region (EMR; n = 1, 4.3%), Region of the Americas (AMR; n = 7, 30.4%), South-East Asia Region (SEAR; n = 3, 13.0%) and Western Pacific Region (WPR; n = 3, 13.0%). 17 studies were conducted on high-income countries (HICs) which accounted for the majority of participants (73.9%). Three (13.0%) studies [18, 33, 36] were conducted in upper-middle-income countries (UMICs), and the remaining three (7.4%) studies [32, 37, 38] were in lower-middle-income countries (LMICs). A description of all studies’ characteristics was provided in Table 1.
Methodological quality and risk of bias for the included studies
In addition to the uneven distribution of studies across socioeconomic contexts and regions, the use of varying methodological approaches also may have contributed to the risk of bias. For example, studies reporting the “exposure assess before to outcome measurement”, “different levels of the exposure of interest”, “repeated exposure assessment”, and “ blinding of outcome assessors” were considered potentially to have a high risk of bias. Five (21.7%) studies [18, 21, 38, 39, 46] reported blinding of outcome assessment. 10 (43.5%) studies [18, 31, 32, 42, 43, 45, 48,49,50,51] reported the exposure assessed prior to outcome measurement. Eight (34.8%) studies [21, 36, 38, 40, 42, 45, 46, 51] reported different levels of the exposure of interest and 12 (52.2%) studies [18, 21, 31, 35, 36, 38, 40, 42, 43, 45,46,47] reported the repeated exposure assessment. The quality assessment of included studies is shown in Table S2, Additional file 1.
Offspring blood pressure
A summary of the meta-analysis results from the included studies is presented in figures below. In these diagrams, results regarding the offspring BP of the mothers with HIP are presented. Furthermore, where the adequate data was available in primary studies, the diagnosed subtypes of HIP were analyzed respectively.
Offspring of mothers with HIP
Overall, 20 studies [18, 21, 31,32,33,34,35,36,37,38,39, 41,42,43,44, 46,47,48, 50, 51] provided data on SBP in offspring of mothers with HIP, and 18 [18, 21, 31,32,33,34,35,36,37,38,39, 41, 42, 44, 46,47,48, 50] on DBP. It can be seen from forest diagrams that both SBP and DBP were significantly higher in offspring of mothers with HIP than those in their controls (SBP: 2.07 mmHg, 95% CI [1.19, 2.95], P < 0.001; Fig. 2a. DBP: 2.41 mmHg, 95% CI [0.88, 3.94], P < 0.001; Fig. 2b).
Offspring of T1DM
In total, five studies [39, 41, 44, 46, 50] reported data on BP in children born to T1DM. There was no difference in either SBP or DBP between offspring of women with T1DM and controls (SBP: 0.25 mmHg, 95% CI [− 2.55, 3.04], P = 0.86; Fig. 3a. DBP: 0.10 mmHg, 95% CI [− 1.03, 1.23], P = 0.86; Fig. 3b).
Offspring of women with GDM
There were 15 studies [18, 21, 31, 33, 34, 36,37,38,39, 43, 44, 47, 48, 50, 51] that reported data on SBP and 13 [18, 21, 31, 33, 34, 36,37,38,39, 44, 47, 48, 50] on DBP under the exposure of maternal gestational diabetes. Both SBP and DBP in Offspring of women with GDM were higher than those in controls (SBP: 1.90 mmHg, 95% Cl [1.09, 2.70], P < 0.001; Fig. 4a. DBP: 0.87 mmHg, 95% Cl [0.11, 1.63], P = 0.02; Fig. 4b).
Subgroup analysis
Subgroup analyses of offspring of mothers with HIP were performed according to sex, the WHO region, economic level, published year, insulin treatment, and BP measurement. The detailed analyzed data for the offspring BP subgroups are listed in Table 2.
SBP and DBP of offspring of women with HIP in both males and females were higher than those in control groups (Male SBP: 2.12 mmHg, 95% CI [0.43, 3.81]; P = 0.01; Male DBP: 1.76 mmHg, 95% CI [0.89, 2.63]; P < 0.001. Female SBP: 2.99 mmHg, 95% CI [1.59, 4.38]; P < 0.001; Female DBP: 1.71 mmHg, 95% CI [0.44, 2.99], P = 0.008).
With regard to the subgroup analyses of offspring of mothers with HIP based on the WHO region, SBP of Offspring of women with gestational diabetes mellitus (OGDM) among AMR, SEAR, and WPR were all significantly higher than that of their counterparts in other regions (AMR: 2.08 mmHg, 95% CI [0.97, 3.19], P < 0.001; SEAR: 2.74 mmHg, 95% CI [0.39, 5.09], P = 0.02; WPR: 2.57 mmHg, 95% CI [1.74, 3.39], P < 0.001), while such difference did not exist between SBP of cases and controls in EUR (− 2.21 mmHg, 95% CI [− 6.31, 1.88]; P = 0.29). As for DBP, no difference was found between offspring of women with HIP and their controls in all EUR, AMR, SEAR, and WPR (EUR: − 1.22 mmHg, 95% CI [− 5.21, 2.76], P = 0.55; AMR: 0.51 mmHg, 95% CI [− 1.10, 2.11], P = 0.54; SEAR: 1.21 mmHg, I [− 0.42, 2.84], P = 0.15; WPR: 1.27 mmHg, 95% CI [− 0.12, 2.66], P = 0.07).
In the subgroup analyses of offspring of women with HIP based on income, this study found that SBP was higher than that in controls in HICs, UMICs, and LMICs. (HICs: 1.44 mmHg 95% CI [0.32, 2.55]; P = 0.01; UMICs: 2.79 mmHg, 95% CI [1.90, 3.68], P < 0.001; LMICs: 2.74 mmHg, 95% CI [0.39, 5.09]; P = 0.02). However, there was no significant difference between DBP of offspring of women with HIP and that in controls in all HICs, UMICs, LMICs (HICs: 0.70 mmHg 95%CI [− 0.52, 1.91]; P = 0.26. UMICs: 0.21 mmHg, 95% CI [− 2.45, 2.86]; P = 0.88; LMICs: 1.21 mmHg, 95% CI [− 0.42, 2.84]; P = 0.15).
For the analyses based on published year, our study found that only estimated BP in maternal HIP group published after 2011 was significantly higher than that in controls (SBP: 2.07 mmHg, 95% CI 1.35, 2.80], P < 0.001; DBP: 0.88 mmHg, 95% CI [0.17, 1.59], P = 0.02) whereas results showed no difference of BP in studies before 2010 (SBP: 1.58 mmHg, 95% CI [− 0.40, 3.56], P = 0.12. DBP: 0.68 mmHg, 95% CI [− 1.10, 2.47], P = 0.97).
While grouping by insulin treatment status, SBP in insulin-treated group and BP in insulin-untreated group were both higher than those in controls (SBP insulin-treated: 2.04 mmHg, 95% CI [0.44, 3.65], P = 0.01; SBP insulin-untreated: 1.35 mmHg, 95% CI [0.65, 2.06], P < 0.001; DBP insulin-untreated: 1.74 mmHg, 95% CI [0.45, 3.03], P = 0.008). By contrast, there was no significant difference between DBP in the insulin-treated group and that in controls (0.03 mmHg, 95% CI [− 1.26, 1.32], P = 0.97).
For the subgroup analysis of offspring of women with HIP based on BP measurement, BP assessed by digital and manual BP measurement was both higher than in controls (SBP Digital measurement: 2.45 mmHg, 95% CI [1.59, 3.32], P < 0.001; SBP manual measurement: 2.30 mmHg, 95% CI [1.21, 3.39], P < 0.001; DBP digital measurement: 1.71 mmHg, 95% CI [0.92, 2.50], P < 0.001; DBP manual measurement: 1.03 mmHg, 95% CI [0.01, 2.05], P = 0.05).
Publication bias of the included studies
Funnel plots were visually inspected to assess the potential publication bias.
It is observable that the distribution of studies was generally consistent across funnel plots of maternal HIP and GDM as outcomes. Visually, all four funnel plots had an overall symmetrical presentation, representing little effect from publication bias. We could not use a funnel plot to assess the bias because fewer than 10 studies of offspring of mothers with T1DM were reported (Fig. 5).
Discussion
This systematic review and meta-analysis aimed to assess the potential risk of hypertension in the offspring of HIP. In general, there was an increased danger of higher DBP and SBP in offspring born to mothers with general HIP and GDM.
Compared with the article of Aceti et al. we have synthesized current studies in more comprehensive ways. Up-to-date evidence was added to the previous ten studies [31, 33, 34, 37, 39, 44, 47, 48, 50, 51] included in the meta-analysis of Aceti et al. we have the rest three studies [35, 41, 46] because they mismatched our inclusion criteria [53].
The results of our study reflect the recent global health status considering the ongoing social changes and research advances better. Furthermore, our research has broadly explored the subgroup analyses which suggested that the linkage between offspring BP and maternal HIP may vary depending on the sex of offspring, BP measurement, insulin treatment status, income, region, and the published year of articles.
More specifically, SBP and DBP appeared to have more substantial and persistent effects on female offspring. Despite the protective effect of endogenous estrogen on BP regulation [54], recent data has cast doubt on the actual protective function for females. We recently found that women have higher BP than men among individuals born prematurely [55]. In line with this evidence, intracardiac studies have also shown that young women with characteristics associated with metabolic syndrome have the highest risk of acute myocardial infarction [56]. It may be because the major estrogen distribution changes throughout puberty together with the menstrual cycle may also affect BP [57]. Therefore, based on mixed pictures of empirical studies, the results of gender differences here should also be carefully used.
As for economic status, it is commonly believed that higher income or socio-economic status might lead to a healthier lifestyle. Aligning with this common sense, mothers with higher socio-economic status have been demonstrated to be at a lower risk of GDM [58]. However, in our research, there were no varied patterns of influence from GDM on offspring DBP and SBP across HICs, UMICs, and LMICs. For one, it could be explained that many low-income countries are currently experiencing demographic and epidemiological transitions as well as lifestyle changes.
Related to this, the BP seemed to be consistently influenced by maternal GDM across regions. Our study defined the region of mothers by their ethnicity, that is, the maternal region of birth. Therefore, the possible biological variances among women from various ethnicities were allowed for inspection in our research. In contrast to our result, previous research suggested maternal diabetes affected child health outcomes differently in Australia and Caucasians [59]. We suspect that there are two reasons for such inconsistency. One is that there are only small pieces of literature included in the regional subgroup [39, 44], and the other lies in the few samples in the experimental and control group in the literature. Therefore, future research still warrants uncovering this mechanism [58].
An interesting phenomenon from our result is that the effect of HIP on offspring’s DBP varied by maternal use of insulin medication. However, another study found no meaningful differences in long-term childhood growth among the offspring of women with GDM treated with insulin compared to nutritional therapy groups [58]. We were constrained from yielding a definitive conclusion due to the unspecified BP measures [60, 61] in several studies and the limitation of sample size. These effects can also explain our finding: there was no significant difference in DBP in the pre-2010 studies, whereas post-2011 studies did. While looking into post-2011 studies, there were larger sample sizes, and mix-methods of BP measurements were more frequently used, including manual sphygmomanometers and automated devices [36, 62]. Furthermore, according to the quality assessment, the methods were of potential risks of bias. As a result, when the analysis was limited to high-quality studies with minimal heterogeneity [63], treatment status and published no longer influenced the relationship between maternal HIP and offspring BP. Therefore, more examinations with high quality should be carried out in the future to distinguish confounds from real effects.
Strengths and limitations
Our study was more comprehensive than previous studies. Compared with the meta-analysis published by Aceti et al. in 2012, which elucidated the association between maternal diabetes and offspring BP [22], we have updated the original article based on existing eligible research. In addition, more meaningful subgroup analyses of OGDM were perform according to the WHO region, economic level, published year, insulin treatment, and BP measurement.
The present study had several limitations. Firstly, owing to a lack of previous data on T1DM, most of the above conclusions are of limited applicability for those mother-child dyads until more empirical studies are conducted. Secondly, the lifestyle variables, such as diet, physical activities, and sleep patterns were lacking in original studies. Therefore, the behavioral factors during the generational transmission of such adverse health conditions remain unclear. Lastly, we failed to demonstrate the age distribution of children in relation to the BP outcomes, which may have been able to trace the dynamic developmental trajectory of offspring in the meta-analysis.
Several implications of this review are pointed out for future research and practice. Firstly, the quality of assessment suggested superior quality may be achieved through adherence to sufficient measurement reports, multiple levels of HIP estimation, the blindness of assessors, etc. Additionally, based on the close relationship between offspring BP and maternal HIP, its pathology process is needed for the next-step research. Besides, the epigenetic pathways may contribute to our understanding of the underlying reasons by introducing more psycho-social or genetic factors into this research scope. In this way, those studies may provide new insights into the pathogeneses of human diseases and tailored prevention by following the concept of Developmental Origins of Health and Disease (DOHaD). Nevertheless, the T1DM condition did not relate to the higher BP of offspring. Although the study's amount of T1DM is relatively small, it may reveal the indirect effect of maternal insulin resistance on the offspring hypertension, a vascular complication of T1DM, is limited [64]. This finding has valuably provided evidence for the “fetal programming” hypothesis of maternal diabetes on the development of metabolic disease [22, 36, 65].
Conclusion
In summary, our review indicates that GDM may result in elevated systolic and diastolic BP in the offspring, providing evidence for fetal cardiovascular risks brought by HIP. Moreover, our study revealed that BP is more seriously impacted after 2011 or when mothers are insulin-untreated. All these factors imply that changes in epigenetic mechanisms may influence the initiation and progression of metabolic diseases that warrant future research. Crucially, we also stress the importance of medical treatment and health promotion adapted to social development.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- HIP:
-
Hyperglycemia in pregnancy
- BP:
-
Blood pressure
- CI:
-
Confidence interval
- SBP:
-
Systolic blood pressure
- MD:
-
Mean difference
- DBP:
-
Diastolic blood pressure
- GDM:
-
Gestational diabetes mellitus
- DIP:
-
Diabetes mellitus in pregnancy
- T1DM:
-
Type 1 diabetes mellitus
- T2DM:
-
Type 2 diabete mellitus
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- MOOSE:
-
Meta-analyses of observational studies in epidemiology
- WHO:
-
World Health Organization
- WB:
-
World bank
- RevMan:
-
Review manager
- EUR:
-
European region
- EMR:
-
Eastern mediterranean region
- AMR:
-
Region of the americas
- SEAR:
-
South-East Asia region
- WPR:
-
Western Pacific region
- HICs:
-
High-income countries
- UMICs:
-
Upper-middle-income countries
- LMICs:
-
Lower-middle-income countries
- OGDM:
-
Offspring of women with gestational diabetes mellitu
- DOHaD:
-
Developmental origins of health and disease
References
World Health Organization. Classification of diabetes mellitus. Geneva: World Health Organization; 2019.
World Health Organization. Diagnostic criteria and classification of hyperglycaemia first detected in pregnancy. Geneva: World Health Organization; 2013.
Toledano Y, Hadar E, Hod M. Pharmacotherapy for hyperglycemia in pregnancy—the new insulins. Diabetes Res Clin Pract. 2018;145:59–66.
International Diabetes Federation. IDF diabetes atlas. 10th ed. Brussels: International diabetes federation; 2021.
Juan J, Yang H. Prevalence prevention and lifestyle intervention of gestational diabetes mellitus in China. Int J Environ Res Public Health. 2020;17:24.
National Heart, Lung, and Blood Institute: U.S Department of Health and Human Services. Quality assessment tool for observa-tional cohort and cross-sectional studies. Available from: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. Accessed 14 May 2021
Ferrara A. Increasing prevalence of gestational diabetes mellitus: a public health perspective. Diabetes Care. 2007;30(Suppl 2):S141–6.
Shah NS, et al. Trends in gestational diabetes at first live birth by race and ethnicity in the US, 2011–2019. JAMA. 2021;326(7):660–9.
Sweeting A, et al. A clinical update on gestational diabetes mellitus. Endocr Rev. 2022;43(5):763–93. https://doi.org/10.1210/endrev/bnac003.
Yuen L, et al. Projections of the prevalence of hyperglycaemia in pregnancy in 2019 and beyond results from the international diabetes federation diabetes atlas 9th edition. Diabetes Res Clin Pract. 2019;157:107841. https://doi.org/10.1016/j.diabres.2019.107841.
Venkatesh KK, et al. Risk of adverse pregnancy outcomes among pregnant individuals with gestational diabetes by race and ethnicity in the United States, 2014–2020. JAMA. 2022;327(14):1356–67. https://doi.org/10.1001/jama.2022.3189.
Vounzoulaki E, et al. Progression to type 2 diabetes in women with a known history of gestational diabetes: systematic review and meta-analysis. BMJ. 2020;369:m1361.
Catalano PM, et al. The hyperglycemia and adverse pregnancy outcome study: associations of GDM and obesity with pregnancy outcomes. Diabetes Care. 2012;35(4):780–6.
Farrar D, et al. Hyperglycaemia and risk of adverse perinatal outcomes: systematic review and meta-analysis. BMJ. 2016;354:i4694.
McIntyre HD, et al. Gestational diabetes mellitus. Nat Rev Dis Primers. 2019;5(1):47.
Aziz S, Munim TF, Fatima SS. Post-partum follow-up of women with gestational diabetes mellitus: effectiveness, determinants, and barriers. J Matern Fetal Neonatal Med. 2018;31(12):1607–12.
Vogt BA. Hypertension in children and adolescents: definition, pathophysiology, risk factors, and long-term sequelae. Curr Ther Res. 2001;62:283–97.
Lu J, et al. Maternal gestational diabetes is associated with offspring’s hypertension. Am J Hypertens. 2019;32(4):335–42.
Al-Biltagi M, El Razaky O, El Amrousy D. Cardiac changes in infants of diabetic mothers. World J Diabetes. 2021;12(8):1233–47.
Nielsen NM, et al. Maternal diabetes and risk of multiple sclerosis in the offspring: a danish nationwide register-based cohort study. Mult Scler. 2021;27(11):1686–94.
Tam WH, et al. In utero exposure to maternal hyperglycemia increases childhood cardiometabolic risk in offspring. Diabetes Care. 2017;40(5):679–86.
Aceti A, et al. The diabetic pregnancy and offspring blood pressure in childhood: a systematic review and meta-analysis. Diabetologia. 2012;55(11):3114–27.
Moher D, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Stroup DF, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–12.
World Health Organization. WHO regional offices. Available from: https://www.who.int/data. Accessed 19 June 2022
World Bank. World bank country and lending groups. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. Accessed 24 July 2022
World Health Organization. Diagnostic criteria and classification of hyperglycaemia first detected in pregnancy: a World Health Organization guideline. Diabetes Res Clin Pr, 2014. 103(3): 341–63
Borenstein M, et al. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1(2):97–111. https://doi.org/10.1002/jrsm.12.
Field AP, Gillett R. How to do a meta-analysis. Br J Math Stat Psychol. 2010;63(Pt 3):665–94.
Leucht S, Kissling W, Davis JM. How to read and understand and use systematic reviews and meta-analyses. Acta Psychiatr Scand. 2009;119(6):443–50.
Boney CM, et al. Metabolic syndrome in childhood: association with birth weight, maternal obesity, and gestational diabetes mellitus. Pediatrics. 2005;115(3):e290–6.
Bunt JC, Tataranni PA, Salbe AD. Intrauterine exposure to diabetes is a determinant of hemoglobin A(1)c and systolic blood pressure in pima Indian children. J Clin Endocrinol Metab. 2005;90(6):3225–9.
Buzinaro EF, et al. Overweight in adolescent offspring of women with hyperglycemia during pregnancy. Arq Bras Endocrinol Metabol. 2008;52(1):85–92.
Catalano PM, et al. Perinatal risk factors for childhood obesity and metabolic dysregulation. Am J Clin Nutr. 2009;90(5):1303–13.
Cho NH, et al. Correlations between the intrauterine metabolic environment and blood pressure in adolescent offspring of diabetic mothers. J Pediatr. 2000;136(5):587–92.
Guttier MC, et al. Repeated high blood pressure at 6 and 11 years at the pelotas 2004 birth cohort study. BMC Public Health. 2019;19(1):1260.
Krishnaveni GV, et al. Intrauterine exposure to maternal diabetes is associated with higher adiposity and insulin resistance and clustering of cardiovascular risk markers in Indian children. Diabetes Care. 2010;33(2):402–4.
Krishnaveni GV, et al. Exposure to maternal gestational diabetes is associated with higher cardiovascular responses to stress in adolescent indians. J Clin Endocrinol Metab. 2015;100(3):986–93.
Kvehaugen AS, Andersen LF, Staff AC. Anthropometry and cardiovascular risk factors in women and offspring after pregnancies complicated by preeclampsia or diabetes mellitus. Acta Obstet Gynecol Scand. 2010;89(11):1478–85.
Lindsay RS, et al. Programming of adiposity in offspring of mothers with type 1 diabetes at age 7 years. Diabetes Care. 2010;33(5):1080–5.
Manderson JG, et al. Cardiovascular and metabolic abnormalities in the offspring of diabetic pregnancy. Diabetologia. 2002;45(7):991–6.
Miranda JO, et al. Maternal diabetes mellitus as a risk factor for high blood pressure in late childhood. Hypertension. 2019;73(1):e1–7.
Perng W, et al. In utero exposure to gestational diabetes mellitus and cardiovascular risk factors in youth: a longitudinal analysis in the EPOCH cohort. Pediatr Obes. 2020;15(5):e12611.
Pirkola J, et al. Maternal type 1 and gestational diabetes: postnatal differences in insulin secretion in offspring at preschool age. Pediatr Diabetes. 2008;9(6):583–9.
Pribylova H, Dvorakova L. Long-term prognosis of infants of diabetic mothers. relationship between metabolic disorders in newborns and adult offspring. Acta Diabetol. 1996;33(1):30–4.
Rijpert M, et al. Cardiovascular and metabolic outcome in 6–8 year old offspring of women with type 1 diabetes with near-optimal glycaemic control during pregnancy. Early Hum Dev. 2011;87(1):49–54.
Tam WH, et al. Glucose intolerance and cardiometabolic risk in children exposed to maternal gestational diabetes mellitus in utero. Pediatrics. 2008;122(6):1229–34.
Tsadok MA, et al. Obesity and blood pressure in 17-year-old offspring of mothers with gestational diabetes: insights from the jerusalem perinatal study. Exp Diabetes Res. 2011;2011:906154.
Vohr BR, McGarvey ST, Coll CG. Effects of maternal gestational diabetes and adiposity on neonatal adiposity and blood pressure. Diabetes Care. 1995;18(4):467–75.
West NA, et al. Cardiovascular risk factors in children exposed to maternal diabetes in utero. Diabetologia. 2011;54(3):504–7.
Wright CS, et al. Intrauterine exposure to gestational diabetes, child adiposity, and blood pressure. Am J Hypertens. 2009;22(2):215–20.
Carpenter MW, Coustan DR. Criteria for screening tests for gestational diabetes. Am J Obstet Gynecol. 1982;144(7):768–73.
Horvath K, et al. Effects of treatment in women with gestational diabetes mellitus: systematic review and meta-analysis. BMJ. 2010;340:c1395.
Dubey RK, et al. Sex hormones and hypertension. Cardiovasc Res. 2002;53(3):688–708.
Parkinson JRC et al. Preterm birth and adult blood pressure: a meta-analysis. Available from: https://www.neonatalsociety.ac.uk/2011/11/10/preterm-birth-and-adult-blood-pressure-a-meta-analysis/. Accessed 10 Jan 2022
Mente A, et al. Metabolic syndrome and risk of acute myocardial infarction a case-control study of 26,903 subjects from 52 countries. J Am Coll Cardiol. 2010;55(21):2390–8.
Dunne FP, et al. Changes in blood pressure during the normal menstrual cycle. Clin Sci. 1991;81(4):515–8.
Feghali M, et al. Treatment of gestational diabetes mellitus and offspring early childhood growth. J Clin Endocrinol Metab. 2021;106(4):e1849–58.
Cynthia P, Timothy S, Isabelle E. What is the impact of diabetes for Australian aboriginal women when pregnant? Diabetes Res Clin Pract. 2011;93(1):e29–32.
Yu C, et al. Exposure to maternal diabetes induces endothelial dysfunction and hypertension in adult male rat offspring. Microvasc Res. 2021;133:104076.
Graves JW, Althaf MM. Utility of ambulatory blood pressure monitoring in children and adolescents. Pediatr Nephrol. 2006;21(11):1640–52.
Lee H, et al. Early manifestation of cardiovascular disease risk factors in offspring of mothers with previous history of gestational diabetes mellitus. Diabetes Res Clin Pract. 2007;78(2):238–45.
Falkner B. Maternal and gestational influences on childhood blood pressure. Pediatr Nephrol. 2020;35(8):1409–18.
Donaghue KC, et al. Microvascular and macrovascular complications associated with diabetes in children and adolescents. Pediatr Diabetes. 2009;10(Suppl 12):195–203.
Pathirana MM, et al. Cardiovascular risk factors in offspring exposed to gestational diabetes mellitus in utero: systematic review and meta-analysis. J Dev Orig Health Dis. 2020;11(6):599–616.
Acknowledgements
We are thankful for the support of all the investigators and participants. Additionally, we would like to thank MengYa Fan, for her valuable help at filtering the data and article writing.
Funding
This work was supported by the construction of multi-dimensional risk identification strategies for prevention and control of childhood hypertension (72104211).
Author information
Authors and Affiliations
Contributions
PS designed the study. XZ and YW managed and analyzed the data. XZ and YW prepared the first draft. PS, WX, DJ, JZ, XY, SW, and SL revised the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
We declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Text S1 Comprehensive search strategy. Table S1 The process of literature review and data extraction. Table S2 The quality assessment of included studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, X., Wang, Y., Xiao, W. et al. Hyperglycaemia in pregnancy and offspring blood pressure: a systematic review and meta-analysis. Diabetol Metab Syndr 15, 10 (2023). https://doi.org/10.1186/s13098-023-00978-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-023-00978-2