Abstract
Background
Diabetes mellitus (DM) causes excess risk of fracture at varied sites. Whereas, the difference between the roles of types 1 DM (T1DM) and 2 DM (T2DM) diabetes in the risk of fractures remains limited and inconclusive. We, therefore, conducted a meta-analysis to assess the differences for the associations of T1DM and T2DM with the risk of fractures.
Methods
We systematically searched PubMed, Embase, and the Cochrane library for eligible studies until May 2021. The odds ratios (ORs) with 95% confidence intervals (CIs) were used to calculate the pooled effect estimates for the associations of T1DM and T2DM with the risk of fractures using the random-effects model. An indirect comparison results for the ratio of OR (ROR) with 95% CI were also applied to assess the difference between T1DM and T2DM with the risk of fractures.
Results
Twenty-two cohort studies involving a total of 6,484,851 individuals were selected for meta-analysis. We noted that T1DM was associated with an increased risk of all fractures (OR: 1.72; 95% CI 1.36–2.19; P < 0.001), and fractures at the hip (OR: 4.01; 95% CI 2.90–5.54; P < 0.001), upper arm (OR: 2.20; 95% CI 1.61–3.00; P < 0.001), ankle (OR: 1.97; 95% CI 1.24–3.14; P = 0.004), and vertebrae (OR: 2.18; 95% CI 1.85–2.57; P < 0.001). Moreover, T2DM induced excess risk to all fractures (OR: 1.19; 95% CI 1.09–1.31; P < 0.001), including fractures at the hip (OR: 1.25; 95% CI 1.15–1.35; P < 0.001), upper arm (OR: 1.42; 95% CI 1.20–1.67; P < 0.001), and ankle (OR: 1.15; 95% CI 1.01–1.31; P = 0.029). Furthermore, we noted that T1DM versus T2DM was associated with greater risk to all fractures (ROR: 1.45; 95% CI 1.12–1.87; P = 0.005), including fractures at the hip (ROR: 3.21; 95% CI 2.30–4.48; P < 0.001), upper arm (ROR: 1.55; 95% CI 1.09–2.20; P = 0.015), and ankle (ROR: 1.71; 95% CI 1.06–2.78; P = 0.029).
Conclusions
This study found that T1DM caused an excess risk to all fractures, including fractures at the hip, upper arm, and ankle than T2DM. Further studies should therefore be conducted to directly compare the differences between T1DM and T2DM with the risk of fractures at various sites.
Similar content being viewed by others
Background
The prevalence of diabetes has increased from 4.7–8.5% worldwide, directly resulting in approximately 1.6 million deaths in 2016 [1]. The inadequate control of diabetes affects the patient’s quality of life through diabetes-specific symptoms and microvascular complications [2, 3]. Diabetes and its complications are also considered a global burden, therefore, reducing the disease burden of diabetes is an important goal of medical care societies and health policymakers [4, 5]. Patients with diabetes are susceptible to excess risk of cardiovascular disease, neuropathy, nephropathy, retinopathy, and mortality [6]. Moreover, the rapidly increasing diabetes prevalence was also parallel with an increase in osteoporotic fractures [7].
Numerous studies have found a positive association of diabetes with the risk of fractures [8,9,10,11,12,13,14], and the potential reason for the association between diabetes and fractures included increased frequency of falling, cortical porosity, microvascular disease, and high levels of advanced glycation end-products [15,16,17]. The National Osteoporosis Foundation guidelines, therefore, suggested that screening for osteoporosis should be conducted for general women aged ≥ 65 years and men aged ≥ 70 years to prevent the morbidity and mortality related to fractures [18]. However, the strength of the association of type 1 diabetes mellitus (T1DM) and type 2 DM (T2DM) with the risk of fractures remains controversial. We, therefore, conducted a systematic review and meta-analysis of cohort studies to assess the differences between the associations of T1DM and T2DM with the risk of fracture at various sites. Moreover, whether study design and gender affected this difference was also evaluated.
Methods
Data sources, search strategy, and selection criteria
The Meta-analysis Of Observational Studies in Epidemiology protocol was used to conduct and report this systematic review and meta-analysis [19]. On the basis of this protocol, cohort studies that investigated the role of T1DM or T2DM with the risk of fractures were eligible in our study. The databases of PubMed, Embase, and the Cochrane library were searched for eligible studies from their inception up to May 2021. The following terms were used as medical subject headings or text words: (“diabetes” OR “diabetes mellitus” OR “glucose” OR “glycated hemoglobin”) AND (“fractures, spontaneous” OR “osteoporotic fractures” OR “fractures, compression” OR “fracture”). The reference lists of potentially relevant articles were also manually reviewed for additional new eligible studies.
The literature search and study selection were conducted independently by 2 reviewers, and face-to-face discussions were used to settle disagreements until a consensus was reached. A study was included if they fulfilled the following inclusion criteria: (1) Study design: prospective or retrospective cohort studies; (2) Participants: general population; (3) Exposure and control: T1DM, T2DM, and non-DM population; (4) Outcome: all fracture, or fractures at hip, distal forearm, upper arm, ankle, and vertebrae; and (5) all the studies should have reported the effect estimates for the role of T1DM or T2DM with the risk of fractures. This study did not contain any human or life participants, therefore, ethics approval and informed consent were not applicable.
Data collection and quality assessment
Information from included studies contained the first author or study group’s name, publication year, region, study design, sample size and number of DM, mean age, male proportion, smoking proportion, body mass index (BMI), DM type, follow-up duration, adjusted factors, and reported effect estimates. The quality of the individual studies were also assessed using the Newcastle–Ottawa Scale (NOS), which is widely used for assessing the quality of observational studies in a meta-analysis. The scoring system for each study ranged from 0–9 [20]. Studies having between 7 and 9 stars were regarded as high-quality. Data extraction and quality assessment were also independently performed by 2 reviewers, and any inconsistency was resolved and adjudicated by an additional reviewer during reading of the full-text of studies.
Statistical analysis
The role of T1DM and T2DM in the risk of fractures was calculated based on the effect estimates (relative risk, hazard ratio, or odds ratio [OR]) using the 95% confidence intervals (CIs) in individual studies. The pooled OR was also calculated using the random-effects models, which considered the underlying variations across included studies [21, 22]. Then, the OR ratio (ROR) with a 95% CI was estimated on the basis of specific ORs, and 95% CIs were taken for T1DM and T2DM studies having risk of fractures [23]. Heterogeneity for each investigated outcome was also assessed using the I2 and Q statistic, and significant heterogeneity was defined as I2 > 50.0% or P < 0.10 [24, 25]. Subgroup analyses for the differences of T1DM and T2DM with the risk of fractures were also assessed on the basis of the study design, and gender. Similarly, publication bias was evaluated as well using qualitative and quantitative methods, including funnel plots, Egger, and Begg tests [26, 27]. The 2-sided inspection level for pooled results was adopted, and statistical significance was set at P < 0.05. Also, all the analyses in our study were performed using the STATA (version 10.0; STATA Corporation, College Station, TX, USA) software.
Results
Literature search
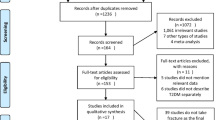
A total of 9873 articles were identified from initial electronic searches, and 5621 articles were retained after duplicate articles were removed. A total of 5527 articles were further removed because these studies reported irrelevant topics. The remaining 94 studies were then retrieved for further full-text evaluations. Of these 94 remaining studies, 72 of them were excluded because they were intervention studies (n = 34); not cohort designs (n = 23); and did not differentiate DM types (n = 15). Reviewing the references of relevant articles found additional 14 potentially included studies, including all studies contained in electronic searches. Finally, 22 cohort studies were selected for the final meta-analysis [28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49] (Fig. 1).
Study characteristics
Of the 22 included studies, 14 studies were prospective cohort studies, whereas the remaining 8 studies were retrospective cohort studies. The characteristics of identified studies and individuals are shown in Table 1. A total of 6,484,851 individuals and 766,610 patients with DM were identified from the 22 studies. Nine studies reported the role of T1DM with the risk of fractures, and 20 studies reported the role of T2DM with the risk of fractures. The follow-up duration ranged from 1.3 to 20.0 years. Also, 9 studies contained only females. Similarly, study quality assessment using the NOS-scoring method showed that 3 studies had 9 stars, 7 studies had 8 stars, 8 studies had 7 stars, and the remaining 4 studies had 6 stars.
All fracture
The studies assessing the role of T1DM and T2DM in the risk of all fractures were reported in studies 4 and 12 studies, respectively (Fig. 2). We noted that both T1DM (OR: 1.72; 95%CI 1.36–2.19; P < 0.001) and T2DM (OR: 1.19; 95% CI 1.09–1.31; P < 0.001) were associated with an increased risk of all fractures. Moreover, there was a significant heterogeneity in the role of T1DM (I2 = 97.8%; P < 0.001) and T2DM (I2 = 94.3%; P < 0.001). We also noted from the selected studies that the risk of all fractures in T1DM patients was significantly higher than in T2DM patients (ROR: 1.45; 95% CI 1.12–1.87; P = 0.005; Table 2). Similarly, subgroup analyses found that excess risk of fractures in T1DM patients existed during pooled prospective cohort studies (ROR: 1.21; 95%CI 1.00–1.46; P = 0.050), retrospective cohort studies (ROR: 1.56; 95%CI 1.09–2.24; P = 0.015), or studies that reported both male and female (ROR: 1.99; 95%CI 1.40–2.83; P < 0.001) (Table 3). Also, no significant publication bias to all fractures was observed (P-value for Egger: 0.075; P-value for Begg: 0.535; Additional file 1).
Hip fracture
The studies that reported the role of T1DM and T2DM in hip fracture risk were studies 9 and 19, respectively (Fig. 3). The summarized results indicated that T1DM (OR: 4.01; 95%CI 2.90–5.54; P < 0.001) and T2DM (OR: 1.25; 95%CI 1.15–1.35; P < 0.001) were associated with an increased risk of hip fracture. Also, there was a significant heterogeneity in the reports for the role of T1DM (I2 = 95.2%; P < 0.001) and T2DM (I2 = 86.7%; P < 0.001) in these fractures. Patients with T1DM were associated with excessive risk of hip fracture than those with T2DM (ROR: 3.21; 95%CI 2.30–4.48; P < 0.001; Table 2). Also, subgroup analyses found that a significant difference between T1DM and T2DM was associated with the risk of hip fracture in all subgroups (Table 3). In contrast, the Begg test did not find any significant publication bias for hip fracture (P = 0.856), while the Egger-test found significant publication bias (P < 0.001) (Additional file 1).
Distal forearm fracture
The studies that reported the role of T1DM and T2DM in distal forearm fracture risk were studies 2 and 9, respectively (Fig. 4). We noted that T1DM (OR: 1.39; 95%CI 0.70–2.77; P = 0.344) and T2DM (OR: 0.94; 95%CI 0.82–1.07; P = 0.348) were not associated with the risk of distal forearm fracture. However, there was significant heterogeneity in the role of T1DM (I2 = 86.7%; P = 0.001) and T2DM (I2 = 58.8%; P = 0.007) in this fracture. Also, the risk of distal forearm fracture in relation to T1DM and T2DM was not statistically significant (ROR: 1.48; 95%CI 0.73–2.98; P = 0.274; Table 2). Similarly, no significant publication bias to distal forearm fractures was observed (P-value for Egger: 0.358; P-value for Begg: 0.584; Additional file 1).
Upper arm fracture
The studies that reported the role of T1DM and T2DM in upper arm fracture risk were studies 2 and 7, respectively (Fig. 5). A summary of the results indicated that T1DM (OR: 2.20; 95%CI 1.61–3.00; P < 0.001) and T2DM (OR: 1.42; 95%CI 1.20–1.67; P < 0.001) were associated with an increased risk of upper arm fracture. Significant heterogeneity was also observed for the role of T1DM (I2 = 72.6%; P = 0.026) and T2DM (I2 = 81.2%; P < 0.001). From the results, T1DM patients showed an excessive risk of upper arm fracture than T2DM patients (ROR: 1.55; 95%CI 1.09–2.20; P = 0.015; Table 2). However, there was no significant publication bias to upper arm fracture (P-value for Egger: 0.117; P-value for Begg: 0.837; Additional file 1).
Ankle fracture
The studies that reported the role of T1DM and T2DM in ankle fracture risk were reported in studies 1 and 3, respectively (Fig. 6). We noted that T1DM (OR: 1.97; 95%CI 1.24–3.14; P = 0.004) and T2DM (OR: 1.15; 95%CI 1.01–1.31; P = 0.029) was associated with an increased risk of ankle fracture. However, no significant heterogeneity was observed across included studies for the role of T1DM (I2 = 29.3%; P = 0.234) and T2DM (I2 = 0.0%; P = 0.886). Patients with T1DM were also associated with an increased risk of ankle fracture than those with T2DM (ROR: 1.71; 95%CI 1.06–2.78; P = 0.029; Table 2). Similarly, no significant publication bias to ankle fracture was observed (P-value for Egger: 0.109; P-value for Begg: 0.060; Additional file 1).
Vertebrae fracture
The studies that reported the role of T1DM and T2DM in vertebrae fracture risk were studies 1 and 8, respectively (Fig. 7). We noted that T1DM was associated with an increased risk of vertebrae fracture (OR: 2.18; 95%CI 1.85–2.57; P < 0.001), whereas no significant association of T2DM in vertebrae fracture risk (OR: 1.45; 95%CI 0.82–2.56; P = 0.200) was observed. Also, no significant heterogeneity for the role of T2DM (I2 = 98.5%; P < 0.001) was reported. Furthermore, the association between the risk of vertebrae fracture in T1DM and T2DM patients, respectively, was notstatistically significant (ROR: 1.50; 95%CI 0.83–2.72; P = 0.177; Table 2). Also, no significant publication bias existed in relation to vertebrae fracture (P-value for Egger: 0.267; P-value for Begg: 1.000; Additional file 1).
Discussion
This study compared the strengths of T1DM and T2DM roles in relation to the risk of fractures. A total of 6,484,851 individuals and 766,610 patients with DM from 22 cohort studies were identified in this comprehensive quantitative meta-analysis. This study found that T1DM was associated with an increased risk of all fractures, including fractures at the hip, upper arm, ankle, and vertebrae, whereas T2DM caused excess risk of all fractures, including fractures at the hip, upper arm, and ankle. Moreover, patients with T1DM were associated with an increased risk of all fractures, hip, upper arm, and ankle fractures than those with T2DM. Furthermore, significant differences in the risk of all fractures between patients having T1DM and T2DM were mainly observed in the subgroups of prospective cohort studies, retrospective cohort studies, or studies that reported both males and females. Finally, the risk of hip fracture in T1DM patients was significantly higher than in T2DM in all predefined subgroups.
A prior meta-analysis conducted by Vestergaard et al. found that T1DM and T2DM patients were associated with an increased risk of hip fracture. An increase in the relative risk of patients with T1DM was also observed to be significantly higher than those with T2DM. Moreover, bone mineral density was increased in patients with T2DM but decreased in patients with T1DM [50]. Janghorbani et al. conducted a meta-analysis based on 2 case-controls and 14 cohort studies and found similar conclusions. Previous studies have indicated that T2DM was weakly associated with fractures at other sites [51]. However, these studies focused on the risk of hip fracture between T1DM and T2DM patients, but did not compare the strength of T1DM and T2DM with the risk of fracture at various sites. Therefore, this study was conducted to update the knowledge about discrepancies in fracture risk between T1DM and T2DM patients.
From this study, it was also found both T1DM and T2DM patients was associated with an increased risk of fractures at most sites. Moreover, the risk of all fractures, including fractures at the hip, upper arm, and ankle in T1DM patients was significantly higher than in T2DM patients. This observation proposes a potential role of T1DM in skeletal fragility, including deficits in bone mineral density, bone geometry, bone microarchitecture, and biomechanical properties [52,53,54]. Furthermore, the role of T2DM in the risk of fracture is proposed to be because of lower levels of bone turnover markers with reduced bone formation [55, 56]. Additionally, patients with T1DM were associated with an increased risk of all fractures, hip, upper arm, and ankle fractures than those with T2DM. The potential reason for this observation is proposed to be that T2DM patients presented higher body weight and BMI than those with T1DM patients, while the fracture in T2DM patients was due to sustained higher traumatic load and soft-tissue energy absorption in obese patients [50]. Finally, the changes in body mineral density in T1DM and T2DM patients differed, which caused the observed varying fracture risk [51].
Subgroup analyses found significant differences that existed between T1DM and T2DM patients, resulting in the risk of all fractures, including hip fracture in most of the subgroups. The risk of all fractures between T1DM and T2DM patients were not also observed in the studies that focused on males and females. This observation is because of (1) the all-fracture risk between T1DM and T2DM that was balanced by fracture at other sites. Therefore, T1DM and T2DM did not affect the risk of distal forearm; (2) the imbalance characteristics between T1DM and T2DM patients, which affected the risk of fractures; and (3) the adjusted factors between T1DM and T2DM that differed, thereby affecting the risk of fracture.
The limitations of this study should be acknowledged. First, this study contained both prospective and retrospective cohort studies, and the selection or recall biases is proposed to be biases on the risk of fracture. Second, the difference between T1DM and T2DM associated with the risk of fractures at varied sites was based on indirect comparison evidence, and various adjusted factors resulted in the risk of fractures. Third, the role of T1DM in the risk of fracture was reported in a smaller number of included studies, and the power to detect potential differences affected the comparison results. Fourth, subgroup analyses were conducted based on study design and gender, but the differences based on other characteristics were not conducted. Fifth, the severity of DM was not addressed, which is proposed to play an important role in subsequent fracture risk. Finally, inherent limitations for meta-analysis of published articles, including inevitable publication bias and the restricted detailed analyses also posed a limitation to this study.
Conclusions
This study found that T1DM and T2DM induced excess risk of fractures at most sites. Moreover, T1DM patients were associated with an increased risk of all fractures, including fractures at the hip, upper arm, and ankle than T2DM patients. Further, large-scale prospective studies should thus be conducted to directly compare the differences between T1DM and T2DM patients with their risk of fracture at various sites.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- DM:
-
Diabetes mellitus
- T1DM:
-
Type 1 diabetes mellitus
- T2DM:
-
Type 2 diabetes mellitus
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- ROR:
-
Ratio of odds ratio
- NOF:
-
National Osteoporosis Foundation
- BMI:
-
Ody mass index
- NOS:
-
Newcastle–Ottawa Scale
References
World Health Organization-Diabetes; 2019. https://www.who.int/health-topics/diabetes.
Laiteerapong N, Karter AJ, Liu JY, Moffet HH, Sudore R, Schillinger D, John PM, Huang ES. Correlates of quality of life in older adults with diabetes: the diabetes & aging study. Diabetes Care. 2011;34:1749–53.
American Diabetes Association Standards of medical care in diabetes, vol. 40; 2017.
Ogurtsova K, da Rocha Fernandes JD, Huang Y, Linnenkamp U, Guariguata L, Cho NH, Cavan D, Shaw JE, Makaroff LE. IDF Diabetes Atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract. 2017;128:40–50.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 44 million participants. Lancet. 2016;387:1513–30.
Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–53.
Reginster JY, Burlet N. Osteoporosis: a still increasing prevalence. Bone. 2006;38:S4-9.
Koromani F, Oei L, Shevroja E, Trajanoska K, Schoufour J, Muka T, Franco OH, Ikram MA, Zillikens MC, Uitterlinden AG, et al. Vertebral fractures in individuals with type 2 diabetes: more than skeletal complications alone. Diabetes Care. 2020;43:137–44.
Wang H, Ba Y, Xing Q, Du JL. Diabetes mellitus and the risk of fractures at specific sites: a meta-analysis. BMJ Open. 2019;9:e024067.
Thong EP, Herath M, Weber DR, Ranasinha S, Ebeling PR, Milat F, Teede H. Fracture risk in young and middle-aged adults with type 1 diabetes mellitus: A systematic review and meta-analysis. Clin Endocrinol (Oxf). 2018;89:314–23.
Ni Y, Fan D. Diabetes mellitus is a risk factor for low bone mass-related fractures: a meta-analysis of cohort studies. Medicine (Baltimore). 2017;96:e8811.
Dytfeld J, Michalak M. Type 2 diabetes and risk of low-energy fractures in postmenopausal women: meta-analysis of observational studies. Aging Clin Exp Res. 2017;29:301–9.
Fan Y, Wei F, Lang Y, Liu Y. Diabetes mellitus and risk of hip fractures: a meta-analysis. Osteoporos Int. 2016;27:219–28.
Shah VN, Shah CS, Snell-Bergeon JK. Type 1 diabetes and risk of fracture: meta-analysis and review of the literature. Diabet Med. 2015;32:1134–42.
Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology. 2010;21:658–68.
Brownlee M. The pathobiology of diabetic complications: a unifying mechanism. Diabetes. 2005;54:1615–25.
Shanbhogue VV, Hansen S, Frost M, Brixen K, Hermann AP. Bone disease in diabetes: another manifestation of microvascular disease? Lancet Diabetes Endocrinol. 2017;5:827–38.
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, Lindsay R. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25:2359–81.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–12.
Wells G, Shea B and O'Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2014. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
Ades AE, Lu G, Higgins JP. The interpretation of random-effects meta-analysis in decision models. Med Decis Making. 2005;25:646–54.
Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ. 2003;326:219.
Deeks JJ, Higgins JP, Altman DG. Analysing data and undertaking meta‐analyses. In: Cochrane handbook for systematic reviews of interventions: cochrane book series. edn.; 2008: 243–96.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–101.
Forsén L, Meyer HE, Midthjell K, Edna TH. Diabetes mellitus and the incidence of hip fracture: results from the Nord-Trøndelag Health Survey. Diabetologia. 1999;42:920–5.
Nicodemus KK, Folsom AR. Type 1 and type 2 diabetes and incident hip fractures in postmenopausal women. Diabetes Care. 2001;24:1192–7.
Ivers RQ, Cumming RG, Mitchell P, Peduto AJ. Diabetes and risk of fracture: The Blue Mountains Eye Study. Diabetes Care. 2001;24:1198–203.
Schwartz AV, Sellmeyer DE, Ensrud KE, Cauley JA, Tabor HK, Schreiner PJ, Jamal SA, Black DM, Cummings SR. Older women with diabetes have an increased risk of fracture: a prospective study. J Clin Endocrinol Metab. 2001;86:32–8.
Ottenbacher KJ, Ostir GV, Peek MK, Goodwin JS, Markides KS. Diabetes mellitus as a risk factor for hip fracture in mexican american older adults. J Gerontol A Biol Sci Med Sci. 2002;57:M648–53.
Miao J, Brismar K, Nyrén O, Ugarph-Morawski A, Ye W. Elevated hip fracture risk in type 1 diabetic patients: a population-based cohort study in Sweden. Diabetes Care. 2005;28:2850–5.
Dobnig H, Piswanger-Sölkner JC, Roth M, Obermayer-Pietsch B, Tiran A, Strele A, Maier E, Maritschnegg P, Sieberer C, Fahrleitner-Pammer A. Type 2 diabetes mellitus in nursing home patients: effects on bone turnover, bone mass, and fracture risk. J Clin Endocrinol Metab. 2006;91:3355–63.
Janghorbani M, Feskanich D, Willett WC, Hu F. Prospective study of diabetes and risk of hip fracture: the Nurses’ Health Study. Diabetes Care. 2006;29:1573–8.
Ahmed LA, Joakimsen RM, Berntsen GK, Fønnebø V, Schirmer H. Diabetes mellitus and the risk of non-vertebral fractures: the Tromsø study. Osteoporos Int. 2006;17:495–500.
Bonds DE, Larson JC, Schwartz AV, Strotmeyer ES, Robbins J, Rodriguez BL, Johnson KC, Margolis KL. Risk of fracture in women with type 2 diabetes: the Women’s Health Initiative Observational Study. J Clin Endocrinol Metab. 2006;91:3404–10.
Melton LJ 3rd, Leibson CL, Achenbach SJ, Therneau TM, Khosla S. Fracture risk in type 2 diabetes: update of a population-based study. J Bone Miner Res. 2008;23:1334–42.
Strotmeyer ES, Kamineni A, Cauley JA, Robbins JA, Fried LF, Siscovick DS, Harris TB, Newman AB. Potential explanatory factors for higher incident hip fracture risk in older diabetic adults. Curr Gerontol Geriatr Res. 2011;2011:979270.
Jung JK, Kim HJ, Lee HK, Kim SS, Shin CS, Kim JT. Fracture incidence and risk of osteoporosis in female type 2 diabetic patients in Korea. Diabetes Metab J. 2012;36:144–50.
Oei L, Zillikens MC, Dehghan A, Buitendijk GH, Castaño-Betancourt MC, Estrada K, Stolk L, Oei EH, van Meurs JB, Janssen JA, et al. High bone mineral density and fracture risk in type 2 diabetes as skeletal complications of inadequate glucose control: the Rotterdam Study. Diabetes Care. 2013;36:1619–28.
Hothersall EJ, Livingstone SJ, Looker HC, Ahmed SF, Cleland S, Leese GP, Lindsay RS, McKnight J, Pearson D, Philip S, et al. Contemporary risk of hip fracture in type 1 and type 2 diabetes: a national registry study from Scotland. J Bone Miner Res. 2014;29:1054–60.
Martinez-Laguna D, Tebe C, Javaid MK, Nogues X, Arden NK, Cooper C, Diez-Perez A, Prieto-Alhambra D. Incident type 2 diabetes and hip fracture risk: a population-based matched cohort study. Osteoporos Int. 2015;26:827–33.
Weber DR, Haynes K, Leonard MB, Willi SM, Denburg MR. Type 1 diabetes is associated with an increased risk of fracture across the life span: a population-based cohort study using The Health Improvement Network (THIN). Diabetes Care. 2015;38:1913–20.
Majumdar SR, Leslie WD, Lix LM, Morin SN, Johansson H, Oden A, McCloskey EV, Kanis JA. Longer duration of diabetes strongly impacts fracture risk assessment: the Manitoba BMD cohort. J Clin Endocrinol Metab. 2016;101:4489–96.
Wallander M, Axelsson KF, Nilsson AG, Lundh D, Lorentzon M. Type 2 Diabetes and risk of hip fractures and non-skeletal fall injuries in the elderly: a study from the fractures and fall injuries in the elderly cohort (FRAILCO). J Bone Miner Res. 2017;32:449–60.
Holm JP, Jensen T, Hyldstrup L, Jensen JB. Fracture risk in women with type II diabetes. Results from a historical cohort with fracture follow-up. Endocrine. 2018;60:151–8.
Jensen MH, Vestergaard P. Hypoglycaemia and type 1 diabetes are associated with an increased risk of fractures. Osteoporos Int. 2019;30:1663–70.
Jiajue R, Qi X, Jiang Y, Wang Q, Wang W, Pei Y, Wang X, Huang W, Zheng X, Ning Z, et al. Incident fracture risk in type 2 diabetic postmenopausal women in Mainland China: peking vertebral fracture study. Calcif Tissue Int. 2019;105:466–75.
Vestergaard P. Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes–a meta-analysis. Osteoporos Int. 2007;18:427–44.
Janghorbani M, Van Dam RM, Willett WC, Hu FB. Systematic review of type 1 and type 2 diabetes mellitus and risk of fracture. Am J Epidemiol. 2007;166:495–505.
Hough FS, Pierroz DD, Cooper C, Ferrari SL. MECHANISMS IN ENDOCRINOLOGY: Mechanisms and evaluation of bone fragility in type 1 diabetes mellitus. Eur J Endocrinol. 2016;174:R127–38.
Roggen I, Gies I, Vanbesien J, Louis O, De Schepper J. Trabecular bone mineral density and bone geometry of the distal radius at completion of pubertal growth in childhood type 1 diabetes. Horm Res Paediatr. 2013;79:68–74.
Shanbhogue VV, Hansen S, Frost M, Jørgensen NR, Hermann AP, Henriksen JE, Brixen K. Bone geometry, volumetric density, microarchitecture, and estimated bone strength assessed by HR-pQCT in adult patients with type 1 diabetes mellitus. J Bone Miner Res. 2015;30:2188–99.
Shu A, Yin MT, Stein E, Cremers S, Dworakowski E, Ives R, Rubin MR. Bone structure and turnover in type 2 diabetes mellitus. Osteoporos Int. 2012;23:635–41.
Starup-Linde J, Eriksen SA, Lykkeboe S, Handberg A, Vestergaard P. Biochemical markers of bone turnover in diabetes patients–a meta-analysis, and a methodological study on the effects of glucose on bone markers. Osteoporos Int. 2014;25:1697–708.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
JQD and JW designed the study; JW and QZ did the literature collection; JQD, JW and QZ analysed the data; JQD and JW wrote the manuscript; QZ revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study did not contain any human participates, and the ethics approval and informed consent are not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Funnel plot.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dou, J., Wang, J. & Zhang, Q. Differences in the roles of types 1 and 2 diabetes in the susceptibility to the risk of fracture: a systematic review and meta-analysis. Diabetol Metab Syndr 13, 84 (2021). https://doi.org/10.1186/s13098-021-00687-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-021-00687-8