Abstract
Background
First-degree relatives (FDRs) of people with rheumatoid arthritis (RA) have a fourfold increased risk of developing RA. The Symptoms in Persons At Risk of Rheumatoid Arthritis (SPARRA) questionnaire was developed to document symptoms in persons at risk of RA. The aims of this study were (1) to describe symptoms in a cohort of FDRs of patients with RA overall and stratified by seropositivity and elevated CRP and (2) to determine if patient characteristics were associated with symptoms suggestive of RA.
Methods
A cross-sectional study of FDRs of patients with RA, in the PREVeNT-RA study, who completed a study questionnaire, provided a blood sample measured for rheumatoid factor, anti-CCP and CRP and completed the SPARRA questionnaire. Moderate/severe symptoms and symmetrical, small and large joint pain were identified and described. Symptoms associated with both seropositivity and elevated CRP were considered suggestive of RA. Logistic regression was used to determine if symptoms suggestive of RA were associated with patient characteristics.
Results
Eight hundred seventy participants provided all data, 43 (5%) were seropositive and 122 (14%) had elevated CRP. The most frequently reported symptoms were sleep disturbances (20.3%) and joint pain (17.9%). Symmetrical and small joint pain were 11.3% and 12.8% higher, respectively, in those who were seropositive and 11.5% and 10.7% higher in those with elevated CRP. In the logistic regression model, seropositivity, older age and feeling depressed were associated with increased odds of small and symmetrical joint pain.
Conclusions
This is the first time the SPARRA questionnaire has been applied in FDRs of patients with RA and has demonstrated that the presence of symmetrical and small joint pain in this group may be useful in identifying people at higher risk of developing RA.
Similar content being viewed by others
Background
It is known that early treatment of RA improves long-term outcomes and reduces the risk of joint damage [1]. Studies have shown that patients with RA may have circulating autoantibodies 5 or more years prior to developing the disease [2]. Recent studies have also investigated whether treatment prior to a clinical diagnosis of RA can actually prevent disease onset. Results from the PRAIRI (prevention of clinically manifest RA by B cell directed therapy in the earliest phase of disease) study has shown that a single infusion of rituximab in patients who were seropositive (positive for rheumatoid factor (RF) or anti-citrullinated protein antibodies (ACPA)) but without clinical synovitis can delay onset of arthritis, though not prevent it [3]. Further studies are ongoing in patients deemed at high risk of developing RA, usually based on the presence of autoantibodies [4]. Identifying people who are at higher risk of developing RA is not straightforward however, as the aetiology of RA is incompletely understood and involves the accumulation of both genetic and environmental factors [5].
A preclinical phase, where patients experience symptoms prior to the development of overt clinical synovitis, has been described [6]. The EULAR study group for risk factors for RA indicated the importance of identifying symptoms that are associated with subsequent development of RA [6]. Few studies have tried to elucidate this complex of symptoms; however, a qualitative study in 2017 of symptoms in newly diagnosed patients with RA and patients with arthralgia identified themes of joint pain, joint swelling and redness, joint stiffness, weakness and loss of motor control, fatigue, sleeping difficulties and depressive symptoms and pattern of symptoms and onset [7]. Often prediction models predicting RA include symptoms such as swollen and tender joints and morning stiffness [8, 9].
Given the genetic predisposition to RA, [5] first-degree relatives (FDRs) of people with RA are a group at higher risk of developing the disease, with a 2–4 times higher risk compared to the general population [10]. This group may therefore offer an opportunity to study the development of RA in the pre-clinical phase. A study of FDRs of patients with RA in North American native (NAN) population found that FDRs reported more joint symptoms than white controls [11]. However, the prevalence of rheumatic disease in the NAN population is one of the highest in the world [12] thus may not be representative of other groups. Therefore, in this study, we aimed to (1) describe symptoms in a cohort of FDRs of patients with RA overall, then stratified by seropositivity and elevated CRP, and (2) determine any patient characteristics associated with symptoms suggestive of RA.
Methods
Study setting
This was a cross-sectional study using data from the PRe-clinical EValuation of Novel Targets in RA (PREVeNT-RA) study, a cohort study of FDRs of patients with established RA in the UK. To be included in the cohort, individuals needed to be an FDR (parent, sibling or half-sibling, offspring) of a proband with a diagnosis of RA (from a rheumatologist) and aged 30 years or over. Individuals were excluded if they had a previous diagnosis of RA or any other inflammatory arthritis.
Study procedures
Individuals who were eligible for inclusion and consented to take part in the PREVeNT-RA study completed a baseline questionnaire and were provided with a blood collection kit. The baseline questionnaire collected information on demographics, medical history, female reproductive history, lifestyle characteristics, health status measured using the EQ-5D-3L health questionnaire [13] and disability measured using the Health Assessment Questionnaire (HAQ) [14]. The blood collection kit enabled a blood sample to be taken in primary care, or at a local rheumatology clinic, and returned to the study coordinating centre. Individuals who consented to completing further questionnaires were sent the Symptoms in Persons At Risk of Rheumatoid Arthritis (SPARRA) questionnaire (described below) [15] to complete and return to the study coordinating centre. To be included in this analysis, individuals needed to have completed a baseline questionnaire, provided a blood sample and completed the SPARRA questionnaire.
Blood samples
Blood samples collected prior to SPARRA completion were used to measure rheumatoid factor (RF) (latex test), anti-cyclic citrullinated peptide (anti-CCP) (Viapath CCP – Immunocap) and C-reactive protein (CRP) (Cormay hsCRP assay). Individuals were considered seropositive if RF was ≥ 20 U/ml and/or anti-CCP was ≥ 7 U/ml. Individuals were considered to have high CRP if CRP was ≥ 5 mg/L.
Cohort characteristics
The following characteristics were determined from the baseline questionnaire: age, gender, smoking status (never smoker, former smoker or current smoker), average alcohol units per week and body mass index (BMI) calculated from self-reported height and weight. Individuals were considered to have depression if they indicated they were moderately or extremely anxious or depressed in the EQ-5D. Education status was categorised by age of leaving education (less than 16 years, 16–17 years, 18–20 years and 21 and over). Socioeconomic status was measured using index of multiple deprivation (IMD) quintile [16]. For females, only the following characteristics were determined: ever being pregnant, ever breastfed a child, ever taken oral contraception and ever taken hormone replacement therapy (HRT).
SPARRA questionnaire
The SPARRA questionnaire (Additional file 1) collects self-reported information on the duration, severity and impact of joint symptoms: pain, swelling, stiffness, burning sensations, tingling sensations and changes in skin colour; other symptoms: muscle cramps, weakness, fatigue, emotional distress, concentration difficulties and sleep problems; and severity of pain in specific locations in the body [15]. For the purposes of analysis, each symptom was categorised as being severe if severity was reported as either moderate or severe. Patterns of joint pain or swelling indicative of RA were also identified: symmetrical joint pain was identified if moderate or severe pain was indicated in any joint on both sides of the body. Small joint pain was identified if moderate or severe pain was indicated in the fingers, wrist or toes. Large joint pain was identified if moderate or severe pain was indicated in the elbow, shoulder, hip, knee or ankle.
Analysis
Seropositivity was considered an indicator of ‘higher risk’ of future RA based on previous literature [2] as was elevated CRP given it is a broad marker of inflammation. Cohort characteristics, overall and stratified by seropositivity and elevated CRP, were tabulated. A priori, symmetrical and small joint pain or swelling were considered in keeping with a possible pre-RA phenotype, and a two-sample test of proportions was used to identify the proportion, with 95% confidence interval (CI), of individuals with these features overall and stratified by seropositivity and elevated CRP. The same test was used to identify associations between any other severe symptoms within SPARRA and seropositivity or elevated CRP. Where significant associations were identified, they were considered suggestive of RA.
Subsequently, characteristics associated with the development of RA from previous literature (age, sex, smoking status, alcohol consumption, BMI, education level, IMD quintile, depression, elevated CRP and antibody positivity) [17] were modelled in univariate and multivariate logistic regression models to determine if they were associated with each of the SPARRA items suggestive of RA identified in the first analysis. As there are some female specific characteristics known to be associated with RA development [17], further analyses were conducted in females only with the following additional characteristics included: pregnancy, breastfeeding, taking HRT and taking oral contraceptives. Symptoms not identified as suggestive of RA were modelled in univariate and multivariate (i.e. all symptoms together) logistic regression models to determine if they were associated with the items suggestive of RA.
Results
As of July 2018, 3114 people had consented to take part in PREVeNT-RA and 2917 had completed the baseline questionnaire. Of those, 713 had not provided a blood sample, 70 had not been sent a SPARRA questionnaire, 317 had not had their blood sample analysed and 947 had not returned the SPARRA questionnaire resulting in 870 people who were eligible for this analysis (Fig. 1). Those eligible for this study were similar in terms of age and gender to those who were not eligible, because either they did not return the SPARRA questionnaire or had returned the SPARRA questionnaire but had not had their blood sample analysed (data not shown).
The mean age of the cohort was 51.8 years (SD 12.1) and 76.6% (n = 666) were female. A small proportion were current smokers (6.4%, n = 56), and the majority of the cohort were Caucasian (97.8%, n = 851). Nearly one fifth reported depression (19.4%, n = 169), and the most frequently reported co-morbidity was hypertension (15.4%, n = 134). Half of the cohort were in the two least deprived IMD quintiles (IMD quintile 4: 24.4%, n = 212, IMD quintile 5: 25.3%, n = 220) (Table 1).
In this cohort, 5% (n = 43) were seropositive, primarily RF positive (Additional file 2, Table 1) and 14% (n = 122) had elevated CRP. Those who were seropositive were older, had a higher proportion with Asian ethnicity and with diabetes. Those with elevated CRP had a higher BMI, fewer years of education, were more likely to have smoked and more likely to have hypertension and diabetes (Table 1).
Symptoms
The most frequently reported symptoms were sleep disturbances (20.3%), joint pain (17.9%), fatigue (16.7%) and distress (16.1%). When stratified by seropositivity, the proportion reporting muscle cramps was significantly higher in those who were seropositive (seronegative: n = 84, 10.3% vs seropositive: n = 10, 23.8%) (Table 2 and Fig. 2A). When stratified by elevated CRP, those with elevated CRP had significantly more joint stiffness (normal CRP: n = 44, 6% vs elevated CRP: n = 25, 20.7%), concentration difficulties (normal CRP: n = 51, 6.9% vs elevated CRP n = 16, 13.2%) and sleep disturbances (normal CRP: n = 137, 18.5% vs elevated CRP: n = 38, 31.4%) (Table 2 and Fig. 2B).
Patterns of joint symptoms
The most frequently identified pattern of joint pain was large joint pain (31%, n = 270). One fifth of the cohort reported small joint pain (22.8%, n = 198) and 17.1% (n = 149) reported symmetrical joint pain. When stratified by seropositivity, a higher proportion of those who were seropositive had small joint pain (seronegative: n = 183, 22.1% vs seropositive: n = 15, 34.9%) and symmetrical joint pain (seronegative: n = 137, 16.6% vs seropositive: n = 12, 27.9%)), though these differences were not statistically significant (Table 2 and Fig. 2C). When stratified by elevated CRP, a significantly higher proportion of those with elevated CRP had symmetrical (normal CRP: n = 116, 15.5% vs elevated CRP: n = 33, 27.0%), small joint (normal CRP: n = 159, 21.3% vs elevated CRP: n = 39, 32.0%) and large joint pain (normal CRP: n = 222, 29.7% vs elevated CRP: n = 48, 39.3%) (Table 2 and Fig. 2D). Only a small number of participants reported joint swelling (n = 52); almost all were seronegative (n = 51) and had normal CRP (n = 44) (Table 2). Therefore, further analysis of joint swelling including stratifying by size and symmetry of joints involved was not possible.
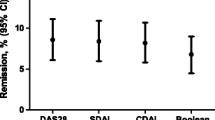
Characteristics associated with small and symmetrical joint pain
From first principles, having both symmetrical and small joint pain was considered suggestive of RA and therefore was incorporated as an alternative outcome measure to seropositivity. There were 116/870 (13.3%) people who had both symmetrical and small joint pain. For characteristics, the multivariate logistic regression model indicated that higher age (OR 1.04 (95% CI 1.02, 1.07)), feeling depressed (OR 2.77 (95% CI 1.65, 4.65)) and being antibody positive (OR 2.55 (95% CI 1.09, 5.97)) were associated with increased odds of having both symmetrical and small joint pain. Leaving education age 18–20 years, compared to leaving education age 16–17 years, was associated with reduced odds of symmetrical and small joint pain (OR 0.51 (95% CI 0.27, 0.97) (Table 3). In the model with females only, higher age (OR 1.03 (95% CI 1.01, 1.06)) and depression (OR 2.92 (95% CI 1.58, 5.39)) remained associated with increased odds of symmetrical and small joint pain. In addition, ever using HRT was associated with increased odds of symmetrical and small joint pain (OR 2.21 (95% CI 1.15, 4.23)) (Additional file 2, Table 2).
Symptoms associated with small and symmetrical joint pain
Those with small and symmetrical joint pain reported more symptoms overall. The multivariate logistic regression model indicated that joint pain, joint stiffness, joint burning, joint tingling and fatigue were all associated with increased odds of symmetrical and small joint pain (Table 4). Similar results were seen in the female only model (Additional file 2, Table 3).
Discussion
This is the first time that symptoms have been captured in a cohort of FDRs of patients with RA, using a questionnaire that that captures data related to the full spectrum of symptoms associated with the early stages of RA. We found that symmetrical and small joint pain was associated with antibody positivity and higher levels of inflammation in the blood. The study also identified associations between increasing age, depression and seropositivity and odds of having both symmetrical and small joint pain; whereas education after age 16 was associated with reduced odds of having both symmetrical and small joint pain. Other reported symptoms did not show a clear pattern helpful for identifying patients at risk of RA in a cross-sectional setting; this may be due to the broad nature of the symptoms. Symmetrical and small joint pain have also been associated with RA in previous studies [17], highlighting that the sections of the SPARRA questionnaire where symmetrical and small joint pain can be identified may be useful for identifying people at high risk of developing RA.
It was of interest that depression was strongly associated with symmetrical and small joint pain. Depression has been found to be highly prevalent in patients with RA [18]. Depression and RA have also been shown to have a bidirectional association, with the presence of pre-existing depression increasing the likelihood of developing RA, and the presence of RA increasing the likelihood of developing depression [19]. Further, in a study of patients with seropositive arthralgia, depressive mood was found to be associated with musculoskeletal symptoms but not arthritis development [20], though recent studies have found depression to be associated with subsequent RA [21, 22]. In our study, depression was highly associated with having small and symmetrical joint pain and also large joint pain (results not shown). However, depression in our study was measured relatively crudely with a single question in the EQ-5D questionnaire, and therefore, this relationship warrants further investigation in other pre-RA cohorts. Our finding that low educational attainment was associated with symmetrical and small joint pain is also in keeping with previous inflammatory arthritis literature; in the EPIC to NOAR study, Lahiri et al. identified that rates of inflammatory polyarthritis were lower in those with degree level education [16].
A surprising finding was that the proportion of current and former smokers was lower in those who were seropositive compared to those who were seronegative. This is most likely to be due to the small number of people who were seropositive (only 5% of this cohort), though the proportion who were seropositive was similar in a Dutch FDR cohort with similar patient characteristics, where 6.6% were seropositive [23]. The subset of the PREVeNT-RA cohort used for this study had few comorbidities and may have had healthier lifestyles than the broader UK population. For example, the proportion of the cohort who were current smokers was low, and only 6.4% were current smokers, which is lower than current UK wide estimates of 15% [24]. Similarly, only 3.2% of participants self-reported diabetes, whereas the 2016 estimated prevalence in England was 8.6% [25]. Overall 52.7% had a BMI that was overweight or obese which is lower than 64% estimated to be overweight or obese in the UK in 2017 [26]. However, a high proportion (19.4%) indicated feeling moderately or severely anxious or depressed, slightly greater than the overall UK estimates of 15.7% [27]. This means the study population may not be fully representative of the general FDR population, perhaps due to non-responder bias, as to be included in this study participants needed to have completed and returned the SPARRA questionnaire.
Only a few studies to date have sought to describe symptoms in unaffected FDRs of patients with RA, mainly reporting joint symptoms. Our findings were similar those of a study of unaffected FDRs in the USA (the SERA cohort) where 23% reported inflammatory joint signs, defined as tender or swollen RA-specific joints (hands, wrists, feet and elbow) [28] which is similar to the proportion reporting small joint pain in this study (22.8%). However, in a different study of NAN FDRs, joint symptoms were more frequently reported compared to this study, with 55% reporting pain in the hands compared to 18% reporting pain in any joint in this study [11]; this may be due to differences between the populations used as NANs have higher prevalence of RA [12]. Musculoskeletal symptoms have also been described in a non-FDR population, where symptoms in consulters to UK primary care with a musculoskeletal (MSK) condition were compared to symptoms in a matched population who consulted for a non-MSK condition. It was found 42% MSK consulters reported symmetrical joint pain, so too did 37% of the matched sample [29]. For both groups, this was higher than in our study where 17% reported symmetrical joint pain. However, the patients in that study were older than in our study and likely to be more unwell as they were consulting at primary care. Studies of patients who were seropositive, but not specifically FDRs, found similar results to our study. Rakieh et al found that found tenderness in small joints to be associated with progression to inflammatory arthritis in patients who were anti-CCP positive [9]. Another small study included 10 people who were ACPA-positive or IgM RF-positive and had symmetrical small joint arthralgia; of those, 6 went onto to develop arthritis [30]. This suggests symmetrical and small joint pain may be important to identify in at-risk populations and that questionnaires such as this will have utility on screening such groups.
This was a large prospective study of unaffected FDRs of patients with RA in the PREVeNT-RA cohort, and the use of the SPARRA questionnaire allowed the collection of detailed symptom data. However, there were some limitations. It was a cross-sectional study; thus, we cannot infer any time dependent or causal relationships. Although the PREVeNT-RA study has been running for 7 years, there are currently too few cases of RA to analyse and validate the SPARRA questionnaire against the outcome of a clinical RA diagnosis. We therefore used seropositivity as proxy measures of this outcome, indicating those at ‘higher risk’ of future RA. We acknowledge, however, that not all patients with RA are seropositive nor all seropositive individuals develop RA [5], particularly those who are only RF positive [30]. Our study was also not able to recall these patients for more detailed clinical assessment, such as joint examination; therefore, there may have been undiagnosed RA or other inflammatory conditions. This could mean some characteristics identified as putting a person at high risk of RA, could be symptoms of RA that has already developed, or conversely could be due to another condition. Enhancing this questionnaire with additional clinical and imaging assessments may identify RA at a very early stage for interventions, and such future studies are planned. Finally, our response rate to the questionnaire was low, albeit within the range expected for surveys [31]. The SPARRA questionnaire is long, and some subjects fed back some difficulties in understanding all the questions. Our work however may point the way to how the questionnaire could be refined and perhaps shortened without any loss of its discriminatory power.
Conclusions
This study of FDRs of patients with RA found that symmetrical and small joint pain was associated with antibody positivity and higher levels of inflammation in the blood, which may be an indicator of people who may be at higher risk of developing RA.
Availability of data and materials
No data are available as the PREVeNT-RA study is still ongoing.
Declarations
Change history
19 October 2021
A Correction to this paper has been published: https://doi.org/10.1186/s13075-021-02645-1
References
Smolen JS, Landewé R, Bijlsma J, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Ann Rheum Dis. 2017;76:960–77.
Rantapää-Dahlqvist S, de Jong BAW, Berglin E, et al. Antibodies against cyclic citrullinated peptide and IgA rheumatoid factor predict the development of rheumatoid arthritis. Arthritis Rheum. 2003;48:2741–9.
Gerlag DM, Safy M, Maijer KI, et al. Effects of B-cell directed therapy on the preclinical stage of rheumatoid arthritis: The PRAIRI study. Ann Rheum Dis. 2019;78:179–85.
Van Steenbergen HW, Da Silva JAP, Huizinga TWJ, et al. Preventing progression from arthralgia to arthritis: targeting the right patients. Nat. Rev. Rheumatol. 2018;14:32–41.
Smolen JS, Aletaha D, Barton A, et al. Primer arthritis rheumatoid. Nat Publ Gr. 2018;4:1–23.
Gerlag DM, Raza K, Van Baarsen LGM, et al. EULAR recommendations for terminology and research in individuals at risk of rheumatoid arthritis: report from the Study Group for Risk Factors for Rheumatoid Arthritis. Ann Rheum Dis. 2012;71:638–41.
Jutley GS, Latif ZP, Raza K. Symptoms in individuals at risk of rheumatoid arthritis. Best Pract Res Clin Rheumatol. 2017;31:59–70.
Van De Stadt LA, Witte BI, Bos WH, et al. A prediction rule for the development of arthritis in seropositive arthralgia patients. Ann Rheum Dis. 2013;72:1920–6.
Rakieh C, L Nam J, Hunt L, et al. Predicting the development of clinical arthritis in anti-CCP positive individuals with non-specific musculoskeletal symptoms: a prospective observational cohort study. Ann Rheum Dis. 2015;74:1659–66.
Frisell T, Saevarsdottir S, Askling J. Family history of rheumatoid arthritis: an old concept with new developments. Nat Rev Rheumatol. 2016;12:335–43.
Smolik I, Robinson DB, Bernstein CN, et al. First-degree relatives of patients with rheumatoid arthritis exhibit high prevalence of joint symptoms. J Rheumatol. 2013;40:818–24.
Peschken CA, Esdaile JM. Rheumatic diseases in North America’s indigenous peoples. Semin Arthritis Rheum. 1999;28:368–91.
EuroQol - a new facility for the measurement of health-related quality of life. Health Policy (New York). 1990;16(3):199–208.
Fries JF, Spitz P, Kraines RG, et al. Measurement of patient outcome in arthritis. Arthritis Rheum. 1980;23:137–45.
van Beers-Tas MH, ter Wee MM, van Tuyl LH, et al. Initial validation and results of the Symptoms in Persons At Risk of Rheumatoid Arthritis (SPARRA) questionnaire: a EULAR project. RMD Open. 2018;4:e000641.
Smith T, Noble M, Noble S, Wright G, McLennan D, Plunkett E. The English indices of deprivation 2015: technical report. London: Department for Communities and Local Government; 2015.
Lahiri M, Luben RN, Morgan C, et al. Using lifestyle factors to identify individuals at higher risk of inflammatory polyarthritis (results from the European Prospective Investigation of Cancer-Norfolk and the Norfolk Arthritis Register-the EPIC-2-NOAR Study). Ann Rheum Dis. 2014;73:219–26.
Matcham F, Rayner L, Steer S, et al. The prevalence of depression in rheumatoid arthritis: a systematic review and meta-analysis. Rheumatology (Oxford). 2013;52:2136–48.
Lu MC, Guo HR, Lin MC, et al. Bidirectional associations between rheumatoid arthritis and depression: a nationwide longitudinal study. Sci Rep. 2016;6:1–7.
Holla JFM, Van Beers-Tas MH, Van De Stadt LA, et al. Depressive mood and low social support are not associated with arthritis development in patients with seropositive arthralgia, although they predict increased musculoskeletal symptoms. RMD Open. 2018;4(1):e000653.
Sparks JA, Malspeis S, Hahn J, et al. Depression and subsequent risk for incident rheumatoid arthritis among women. Arthritis Care Res (Hoboken). 2021;73:78–89.
Vallerand IA, Lewinson RT, Frolkis AD, et al. Depression as a risk factor for the development of rheumatoid arthritis: a population-based cohort study. RMD Open. 2018;4:670.
Maijer KI, Gerlag DM, Tak PP. Prevalence of anti-citrullinated protein antibodies and IgM rheumatoid factor in first-degree relatives of Dutch rheumatoid arthritis patients. Arthritis Rheumatol. 2015;67:3324–6.
Windsor-Shellard B. Adult smoking habits in the UK. London: Office for National Statistics; 2017. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandlifeexpectancies/bulletins/adultsmokinghabitsingreatbritain/2017. Accessed 25 Feb 2020.
Public Health England. Diabetes Prevalence Model 2016. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/612306/Diabetesprevalencemodelbriefing.pdf.
Statistics on Obesity, Physical Activity and Diet in England, 2019. Part 3: Adult overweight and obesity - NHS Digital. https://digital.nhs.uk/data-and-information/publications/statistical/statistics-on-obesity-physical-activity-and-diet/statistics-on-obesity-physical-activity-and-diet-england-2019/part-3-adult-obesity. Accessed 27 Feb 2020.
McManus S, Bebbington P, Jenkins RBT. Mental health and wellbeing in England: Adult Psychiatric Morbidity Survey 2014; 2016.
Sparks JA, Chang SC, Deane KD, et al. Associations of smoking and age with inflammatory joint signs among unaffected first-degree relatives of rheumatoid arthritis patients: results from studies of the etiology of rheumatoid arthritis. Arthritis Rheumatol. 2016;68:1828–38.
Hider SL, Muller S, Helliwell T, et al. Symptoms associated with inflammatory arthritis are common in the primary care population: results from the joint symptoms survey. Rheumatology. 2019;58:2009–14.
Bos WH, Wolbink GJ, Boers M, et al. Arthritis development in patients with arthralgia is strongly associated with anti-citrullinated protein antibody status: a prospective cohort study. Ann Rheum Dis. 2010;69:490–4.
Garcia I, Portugal C, Chu L-H, et al. Response rates of three modes of survey administration and survey preferences of rheumatoid arthritis patients. Arthritis Care Res (Hoboken). 2014;66:364–70.
Acknowledgements
We would like to thank the PREVeNT-RA participants and principal investigators as follows: Dr Michael Batley - Maidstone and Tunbridge Wells NHS Trust, Dr Marwan Bukhari - Royal Lancaster Infirmary, Lancaster, Dr James Burns - Antrim Area Hospital, Northern Ireland, Dr Lucy Coates - Tameside General Hospital, Manchester, Dr Andrew Cope – Guy’s Hospital, London, Dr Emily Deeney - Queen Elizabeth Hospital, Gateshead, Dr Karen Douglas - Russells Hall Hospital, Dudley, Dr Paul Emery- Leeds Teaching Hospital, Dr Andrew Filer - Birmingham Queen Elizabeth hospital, Dr Charlotte Filer - Stepping Hill Hospital, Stockport, Dr James Galloway - Kings College hospital, London, Dr Phillip Gardiner - Altnagelvin Hospital (Western Health and Social Care Trust), Northern Ireland, Dr John Isaacs - Freeman Hospital, Newcastle, Dr Rachel Jeffrey - Northampton General Hospital, Dr Sophia Khan - Heart of England NHS foundation Trust, Solihull, Dr Suzanne Lane - Ipswich Hospital, Suffolk, Dr Sara Littlejohns - North Devon District Hospital, Barnstable, Dr Kirsten Mackay - Torbay Hospital, Torquay, Dr Nicola Maiden – Craigavon Area Hospital, Portadown, Dr Tarnya Marshall - Norfolk and Norwich University Hospital, Norfolk, Dr Sophia Naz – Fairfield General Hospital, Bury, Dr Sophia Naz - North Manchester General Hospital, Manchester, Dr Terence O'Neill - Salford Royal Hospital, Salford, Dr Ira Pande - Queens Medical Centre, Nottingham, Dr Yusef Patel - Hull Royal Infirmary, Hull, Dr Anandita Paul - Bolton NHS Foundation Trust, Dr John Pauling - Royal National Mineral Hospital for Rheumatic Diseases, Bath, Dr Adrian Peall – The County Hospital, Hereford, Dr Suzannah Pegler - Great Western Hospital, Swindon, Dr Helen Prady - Warrington and Halton Teaching Hospitals NHS Foundation Trust, Warrington, Dr Karim Raza - Birmingham City Hospital, Birmingham, Dr Lindsay Robertson - Derriford Hospital, Plymouth, Dr Richard Smith - Salisbury District Hospital, Wiltshire, Dr Peter Taylor - Oxford University Hospitals NHS Foundation Trust, Oxford, Dr Julia Taylor - Poole Hospital, Dorset, Jessica Thrush - Worcestershire Acute Hospitals NHS Trust, Redditch Dr Lisa Trembath - Royal Cornwall Hospital, Truro, Professor David Walsh - Sherwood Forest Hospitals NHS Foundation Trust, Nottinghamshire, Dr Pippa Watson – Manchester University NHS Foundation Trust, Manchester, Professor Simon Bowman - Milton Keynes University Hospital NHS Foundation Trust, Milton Keynes, Helena Cox - Burton Hospitals (Queens Hospital) & Royal Derby Hospital, Dr Emily Deeney – Gateshead Health NHS Foundation Trust, Gateshead, Dr Sam Hider - Haywood Hospital, Stoke, Dr Cath Lawson - Harrogate District Hospital, Harrogate, Dr Paul McCabe - Trafford General Hospital, Manchester, Dr Constantino Pitzalis – Mile End Hospital, London, Dr Lee-Suan The - Royal Blackburn Hospital, Blackburn, Dr Louise Warburton - Shropshire Community Health NHS Trust, Shrewsbury.
Ethical approval and consent to participate
The NRES Committee North West - Greater Manchester West approved this cohort study (Ref: 12/NW/0867).
Funding
This research was funded by the NIHR Biomedical Research Centre and supported by the Centre for Epidemiology Versus Arthritis (grant number: 21755). Professor Bruce is a National Institute for Health Research (NIHR) Senior Investigator and is funded by the NIHR Manchester Biomedical Research Centre. Professor Raza is supported by the NIHR Birmingham Biomedical Research Centre.
Author information
Authors and Affiliations
Contributions
INB conceived the idea. INB, REC, JS, and JHH designed the study. MH and REC analysed the data. All authors interpreted the data. REC drafted the manuscript. All authors revised the manuscript for intellectual content, approved the final draft and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: the Acknowledgement section was updated.
Supplementary Information
Additional file 1:.
Symptoms in Persons At Risk of Rheumatoid Arthritis (SPARRA) Questionnaire
Additional file 2:
Table 1 Specific details of seropositivty. Table 2 Characteristics and associations with symmetrical and small joint pain in females only. Table 3: Symptoms and associations with symmetrical and small joint pain in females only (N=631)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Costello, R.E., Humphreys, J.H., Sergeant, J.C. et al. Symptoms in first-degree relatives of patients with rheumatoid arthritis: evaluation of cross-sectional data from the symptoms in persons at risk of rheumatoid arthritis (SPARRA) questionnaire in the PRe-clinical EValuation of Novel Targets in RA (PREVeNT-RA) Cohort. Arthritis Res Ther 23, 210 (2021). https://doi.org/10.1186/s13075-021-02593-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13075-021-02593-w