Abstract
Osteoarthritis (OA) is one of the most frequent musculoskeletal diseases characterized by degeneration of articular cartilage, subchondral bone remodeling, and synovial membrane inflammation, which is a leading cause of global disability, morbidity, and decreased quality of life. Interpreting the potential mechanisms of OA pathogenesis is essential for developing novel prevention and disease-modifying therapeutic interventions. Gut microbiota is responsible for a series of metabolic, immunological, and structural and neurological functions, potentially elucidating the heterogeneity of OA phenotypes and individual features. In this narrative review, we summarized research evidence supporting the hypothesis of a “gut-joint axis” and the interaction between gut microbiota and the OA-relevant factors, including age, gender, genetics, metabolism, central nervous system, and joint injury, elucidating the underlying mechanisms of this intricate interaction. In the context, we also speculated the promising manipulation of gut microbiota in OA management, such as exercise and fecal microbiota transplantation (FMT), highlighting the clinical values of gut microbiota. Additionally, future research directions, such as more convincing studies by the interventions of gut microbiota, the gene regulation of host contributing to or attributed to the specific phenotypes of gut microbiota related to OA, and the relevance of distinct cell subgroups to gut microbiota, are expected. Moreover, gut microbiota is also the potential biomarker related to inflammation and gut dysbiosis that is able to predict OA progression and monitor the efficacy of therapeutic intervention.
Similar content being viewed by others
Introduction
Osteoarthritis (OA) is one of the most frequent musculoskeletal diseases characterized by degeneration of articular cartilage, subchondral bone remodeling, synovial membrane inflammation causing pain, morning stiffness, swelling, limited range of joint motion, and poor physical function, which is a leading cause of global disability, morbidity, and decreased quality of life [1]. With aging and increasing obesity population, the prevalence of osteoarthritis is rising, particularly since the mid-twentieth century, impacting 303 million individuals globally in 2017 and resulting in unsustainable clinical, humanistic, and economic burdens composed of medical care costs, lost wages, and depressed economic productivity [2,3,4].
OA is now recognized as a collection of multiple subgroups, each with specific pathophysiological and clinical features dependent on the risk factors involved, such as metabolic syndrome-associated osteoarthritis, post-traumatic osteoarthritis, and aging-associated osteoarthritis [5,6,7]. These risk factors independently or intricately contribute to a complex interaction between mechanical, biochemical, and cellular factors, leading to the pathogenesis of OA. Identifying phenotypes of patients may help to detect the disease at its early stage and could be used to guide clinical decision making and allow more effective and specific therapeutic interventions targeted toward individuals. As a result, it is meaningful to identify an underlying but important individual feature, gut microbiota, to better understand the heterogeneity of OA phenotypes.
Gut microbiota, defined as a collection of gut microbe populations, is responsible for a series of metabolic, immunological, structural, and neurological functions, such as maintenance of metabolic homeostasis, development and maturation of immune system, resistance to infections, and production of neurotransmitters [8]. The most representative bacterial phyla in gut microenvironment are Firmicutes and Bacteroidetes, followed by Verrucomicrobia, Actinobacteria, Fusobacteria, Proteobacteria, and Cyanobacteria [9]. Due to its incredible involvements, microbial dysbiosis, defined as an adverse alteration in the diversity, structure, or function of gut microbiota, contributes to diverse pathological states and diseases. Gut microbiota is involved in the initiation and progression of inflammation-driven diseases, and microbial dysbiosis has been emerged as a hidden risk factor inducing the production of proinflammatory cytokines and bacterial metabolites, which may boost the pathophysiological mechanisms of OA [10]. OA risk factors, such as aging, diet, and obesity, are shown to perturbate gut microbiota, while limited evidence supports the involvement of gut microbiota upon the mechanisms of these risk factors.
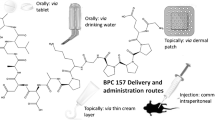
In this review, we summarized the evidence supporting the hypothesis of “gut-joint” axis and the interactions between gut microbiota and OA-relevant factors and assessed the potentials of microbiota-targeted therapies in OA management (Table 1, Fig. 1). Based on the current understanding of the crosstalk between gut microbiota and these factors, gut microbiota could be considered as an indispensable element that provides a unifying mechanism to explain the involvement of these individual-level risk factors in OA.
Relationship between the gut microbiota and osteoarthritis development. OA-relevant factors are involved in OA either directly, or via the modulation of gut microbiota. Several disease-modifying therapeutic approaches can relieve OA symptoms directly, or via altering the composition of gut microbiota to influence OA progression indirectly. OA, osteoarthritis
Hypothesis of “gut-joint” axis in OA
The “gut-joint” axis is established on the possibility of the crosstalk between joint and gut. It is well accepted that gut microbiota have been shown to produce a wide range of molecules, including enzymes, short-chain fatty acids (SCFAs), and metabolites. As a result, these bacterially produced proinflammatory metabolites, such as lipopolysaccharide (LPS), make their way from the “leaky gut” to the systemic circulation and induce systematic inflammation. Due to the elevation of LPS levels in association with obesity and metabolic syndrome which are the highly relevant risks to OA, it is easy to speculate the microbiota involvement in OA at least, by LPS-induced low-grade inflammation, metabolic endotoxemia, macrophage activation, and joint damage. Indeed, Huang et al. found that increased levels of lipopolysaccharide (LPS) and LPS-binding protein (LBP) were associated with knee osteophyte severity and abundance of activated macrophages in the synovium [22]. Also, monitoring of circulating LPS concentrations could provide a new means to diagnose and treat specific phenotypes of OA [23]. Furthermore, a recent interesting study performed by Christopher et al. identified a microbial DNA signature, for the first time, in human and mouse cartilage, the alternation of which is associated with the development and progression of human OA [24]. These findings suggest a potential involvement of microbiota by direct inoculation or the transportation of immune cells, while it is still a puzzle the detailed role of this specific bacterial DNA in cartilage tissue in OA pathogenesis.
The interactions between gut microbiota and OA-relevant factors
Accumulating evidence reveals that gut microbiota could be re-sharped by some OA-relevant factors, such as aging, gender, diet, and obesity, parallelly boosting the systematic inflammation, suggesting the possibility of the microbe involvement in OA, while limited convincing studies have validated this speculation by the interventions on gut microbiota. Still, the knowledge of the interactions between the OA-relevant factors and gut microbiota adds a novel layer of our understanding of the complexity of OA pathogenesis and also provides a new perspective on OA investigation.
Age
Aging has been shown to be associated with an increased incidence of osteoarthritis [25]. Previous studies have illuminated several potential mechanisms by which the aging-associated changes in articular tissues promote the progression of OA, such as pervasive aging-relevant chronic low-grade inflammation (also known as “inflammaging”), cellular senescence, mitochondrial dysfunction and oxidative stress, dysfunctional energy metabolism, and alternated mechanical properties extracellular matrix attributed to the accumulation of advanced glycation end products (AGEs) [26, 27].
In recent years, researchers are becoming increasingly interested in elucidating aging-related differences in the gut microbiota among elderly adults and young individuals to improve the understanding of aging-related mechanisms and discover novel therapies. Aging-related alterations in gut physiology, such as degenerative changes in enteric nervous system, gastric hypochlorhydria, drug perturbation, and motility disorders, have significant impacts on the diversity, composition, and functional features of gut microbiota [28]. The aging-related changes of gut microbiota were characterized by reduced diversity, decreased abundance of dominant species, increased abundance of subdominant species, and a swift of increased proteolytic and decreased saccharolytic bacteria [29,30,31]. For instance, Biagi et al. observed that the structure of the gut microbiota of centenarians differs significantly from that of non-centenarian adults, characterized by an enrichment in Proteobacteria, a phylum including many potentially pathogenic bacteria. Furthermore, these alterations in centenarians are associated with increased levels of proinflammatory markers, suggesting the potential role of gut microbiota in this pervasive systematic inflammation [32]. Given that aging is a persistent factor, the aging-associated differences in gut microbiota and relevant inflammatory status may be an important determinant of onset and progression of OA, while the intervention of aging-relevant microbiota is still needed to validate the involvement of gut microbiota in aging-relevant OA phenotypes.
Gender
It is a striking observation that females are at greater risk for developing knee, hip, and hand OA compared to males and tend to be more severe [33]. The underlying mechanisms behind the increased incidence of OA with sex difference remains to be unclear, while this higher prevalence of OA observed in women at the time of menopause has been attributed to the hypothesis that hormonal factors, such as estrogens, play a role in the development of OA, for instance, estrogens increase the sensitivity to inflammatory stimuli and responses in female [34]. Moreover, some possible conjectures also have been proposed for explaining the discrepancy of gender-dependent influence in OA, such as sex differences in gut microbiota composition [35].
Comparing the gut microbiota composition of 341 female with 348 male mice, Elin et al. showed a decreased relative abundance of Porphyromonaceae and Rikenella and a higher abundance of Ruminococcus, Coprococcus, and Dorea in male mice, while a higher presence of Allobaculum, Anaeroplasma, and Lactobacillaceae and Veilonellaceae in female mice, demonstrating that sex differences exist in microbiota composition [36]. A recent clinical study was conducted in a subgroup of 75 patients (39 men and 36 women), who had similar dietary background and matched by age, to analyze differences in fecal samples intestinal microbiota composition by 16S DNA sequencing, observing that women had a higher abundance of Bacteroides and Bilophila compared to men while men present higher abundance of Veillonella and Methanobrevibacter [37].
The different composition of gut microbiota between males and females may be mediated by sex hormones. Although no study has validated that these gender-relevant difference of gut microbiota contributes to the higher OA prevalence of female individuals, Li et al. built the link between sex steroid, bone loss, and gut microbiota. Their study showed that sex steroid deficiency led to the increase of gut permeability and sex steroid deficiency-induced bone loss is gut microbiota-dependent [38]. Given that subchondral bone loss is a phenotype of OA, this evidence gives a clue that gut microbiota might be involved in OA subchondral bone loss and the gender divergence in gut microbiota might have an indispensable role in the definition of gender differences in the prevalence of OA.
Genetics
Genetic factor is responsible for 60% of hand and hip OA and 40% of knee OA [39]. An increasing number of susceptibility loci, such as insulin-like growth factor 1 gene (IGF1), growth differentiation factor 5 gene (GDF5), and vitamin D receptor gene (VDR), are proven to contribute to genetic predisposition of OA onset [40, 41].
Solovieva et al. found that VDR gene polymorphisms play a role in the etiology of symmetrical hand OA in Finnish population [42]. Moreover, the effect of VDR polymorphisms on the risk of OA may be modified by daily calcium intake. Interestingly, the influence of VDR gene variation on gut microbiota was also demonstrated in a genome-wide association analysis (GWAS) study performed by Wang et al. [43]. Still, no evidence supports the role of genetic susceptibility of VDR gene in the interaction between host and gut microbiota on OA onset and progression while we believe that this critical gene in bone and joint health may contribute to the individual difference of OA patients by the involvement in host-gut interaction. In the context, elucidating the association between gut microbiota and genetic factors is an important contribution to our comprehension of how these manipulations of the bacteria or its metabolites affect bone and cartilage growth in individual levels.
Diet
Several dietary factors have been reported to be involved in the pathophysiology of OA, such as polyunsaturated fatty acids, antioxidants, and amino acids [44, 45]. Baker et al. found a positive connection between the n-6 polyunsaturated fatty acid (PUFA), arachidonic acid (AA), and synovitis but an inverse relation between total plasma n-3 PUFA, docosahexaenoic acid (DHA), and patellofemoral cartilage loss, suggesting that systemic levels of n-3 and n-6 PUFAs which are manipulated by diet may be associated with articular-cartilage composition and structural damage [46]. Previous studies have showed that the intake of dietary antioxidants such as vitamin C, D, and K, involved in regulating collagen formation, bone metabolism, and cartilage mineralization, may prevent the progression of OA [44]. Although the effects of dietary supplements on OA prevention are controversial, it is no doubt that these nutrients are indispensable and at least benefit metabolic health. In this context, the improved understanding of how these dietary factors contribute to the maintenance of joint fitness is helpful to interpret the association between OA and unfavorable diet and give promise to diet-based supplemental strategies.
Gut microbiota is highly shaped and modulated by the host’s dietary components [47]. Kaliannan et al. found that mice fed a diet high in n-6 PUFAs can increase the proportions of LPS-producing and/or proinflammatory bacteria including Proteobacteria and its members, and decrease levels of LPS-suppressing and/or anti-inflammatory bacterial groups, such as Bifidobacterium, Lactobacillus, Clostridium, and Enterococcus faecium, while transgenic conversion of tissue n-6 to n-3 fatty acids dramatically exhibited opposite effect, suggesting that the tissue n-6/n-3 PUFA ratio modifies gut microbiota profile composition and gut permeability, leading to differential inflammatory status and metabolic syndrome [48]. Moreover, recent evidence showed that vitamin D may influence disease risk by modifying the diversity of gut microbiota. The effects of vitamin D on Bacteroides phylum are not conclusive while some studies have reported that a low vitamin D diet or vitamin D receptor (VDR) knock-out results in a more inflammatory fecal microbiome characterized by an increased Bacteroidetes [49, 50]. Interestingly, very high-dose vitamin D diet is unexpectedly associated with an increase in Bacteroidetes, particularly of the orders Bacteroidales and Flavobacteriale, with a decrease in circulating vitamin D [51], suggesting that vitamin D may influence host systematic immunology by modifying the diversity of gut microbiota in a complex feedback loop. Vitamin D may play a role in maintaining the mucosal barrier integrity by upregulating the expression of tight junction and adherent junction proteins and suppressing epithelial cell apoptosis [52]. Also, dietary glutamine supplementation alters composition and metabolism of intestinal microbiota, inducing a shift in the Firmicutes/Bacteroidetes ratio and enhanced intestinal secretory IgA (SIgA) secretion [53]. Although these interesting findings indicate that dietary nutrients influence host physiological functions dependent on intestinal microbiota, limited evidence supports that dietary nutrients can modify the OA-relevant microbiota, as a result of which the link between diet, gut microbiota, and OA is still not convincing and needs more experimental validations.
Obesity and metabolic syndrome
Obesity is an established risk factor for osteoarthritis not only in weight-bearing joints, such as knee and hip, but also in non-weight-bearing joints, such as hand and temporomandibular joints, indicating that obesity contribute to the systemic factors relevant to OA [54, 55]. Metabolic syndrome-associated osteoarthritis (Met-OA) is the phenotype of OA characterized by obesity, diabetes, dyslipidemia, and hypertension [56]. Present studies have demonstrated several mechanisms linking osteoarthritis to obesity and metabolic syndrome partially, such as insulin resistance, the potential implication of oxidized low-density lipoprotein (ox-LDL) on ectopic bone formation and synovium inflammation, and the potential involvement of gut microbiota [57].
The most accepted connection between OA and obesity and metabolic syndrome is the low-grade chronic inflammation partially induced by the elevated microbiota-derived proinflammatory metabolites and relevant gut microbiota components, such as LPS. Collins et al. found that systematic LPS concentration was associated Lactobacillus species abundance and increased joint damage was associated with the abundance of Lactobacillus and Methanobrevibacter species and body fat, but not body mass, in a high-fat/high-sucrose diet-induced obese rat model [11]. Another observation performed by Guss et al. in a load-induced model of OA with/without a high-fat diet in Toll-like receptor-5 deficient (TLR5KO) mice that spontaneously develop metabolic syndrome due to gut microbiota alterations, suggests that severe obesity and inflammation increased load-induced cartilage damage and the modification of metabolic syndrome-associated phylotypes of gut microbiota may contribute to development of cartilage pathology and subchondral bone morphology [12]. More importantly, the finding of Schott et al. suggests that oligofructose supplementation restored the lean gut microbiome in obese mice by supporting favorable Bifidobacterium pseudolongum and reduced OA progression, which sheds light to potential novel OA therapeutics involving strategic manipulation of specific microbial species inhabiting the intestinal space [18].
Central nervous system (CNS)
It has been known for some time that the role of the central nervous system (CNS) is related to chronic pain in OA patients [58]. Progress of CNS theory in OA was accelerated in the early 1950s when neurophysiology was advancing [59]. So far, the new components of the CNS theory in OA pathophysiology include hypothalamic-pituitary (HPA) axis, nucleus tractus solitarus (NTS), hypothalamic suprachiasmatic nuclei (SCN), and other associated higher centers, and each with their own feedback circuits from the gut microbiota, OA joints, and cellular metabolism. Progression of OA is increasingly linked to dysregulation of central feedback circuits (e.g., HPA axis and NTS), which control circadian rhythm, gut microbiome, metabolism, and redox regulation [60].
Gut microbiota is regarded as one key element of the gut-brain axis in the CNS theory. Briefly, CNS modulates the gastrointestinal tract and enteric nervous system through sympathetic and parasympathetic axis while intestinal microbiota influence CNS function through vagal afferent nerves, immune system, HPA axis, and bacterially derived neurotransmitters [61, 62]. Additionally, due to the findings of Liang et al. that the absolute amount of fecal bacteria and the abundance of Bacteroidetes exhibited circadian rhythmicity, gut microbiota may communicate with host’s circadian clock to regulate cartilage homoeostasis [63, 64]. The interaction between CNS, gastrointestinal tract, and joint is an active area that remains to be investigated. Targeting gut microbiota to restore the balance of gut-brain axis might offer novel disease-modifying therapies for OA patients.
Joint injury
Joint injury is a well-established risk factor for development of OA, including anterior cruciate ligament (ACL) rupture, meniscal tear, and intra-articular fracture. Nearly 12% of all OA cases may be due to initial trauma [65]. Therefore, a better understanding of mechanisms triggered by joint injury is beneficial to develop more targeted strategies for prevention and treatment of post-traumatic OA (PTOA). Accumulating evidence demonstrates that perpetuating inflammation response to joint injury plays a critical role in the progression of PTOA, including the production of inflammatory mediators, such as cytokines/chemokines and damage-associated molecular patterns (DAMPs), low-grade synovial immune infiltration, and innate inflammatory pathway activation involving multiple tissues [66].
Toll-like receptors (TLRs), most studied in PTOA among several receptors, are associated with proinflammatory innate immune response to injury through recognizing fragments of the cartilage extracellular matrix, microbiome-derived metabolites. Additionally, the combination of LPS and DAMPs resulting from joint damage, synergistically activates macrophages to express elevated levels of OA-related cytokines [23, 67]. Beyond the impact of post-injury inflammation responses on cartilage and subchondral bone, a direct correlation between gut microbiota and development of injury-induced OA has been previously demonstrated. Significantly, in animal models induced by destabilized medial meniscus (DMM) surgery, the severity of PTOA was reduced in the germ-free situation compared to specific pathogen-free (SPF) mice, providing evidence for a role of the gut microbiota in PTOA pathogenesis [13]. These findings have illustrated the complexity of the inflammatory response to joint injury and gut microbiota is thought to be involved in PTOA progression.
Other OA risk factors
Other OA-relevant risk factors, such as smoking and alcohol consumption, are also identified as a perturbation on gut microbiota. It is wildly accepted that smoking and alcohol contribute to the unfavorable changes of the integrity of gastrointestinal barrier. Also, alcohol causes the depletion of anti-inflammatory bacteria, eventually resulting in intestinal damages [68]. Besides, in a population-based cross-sectional study, Lee et al. built the link between gut microbiota composition and current smokers [69]. Still, the connection between these OA-relevant risk factors, OA, and gut microbiota has not been demonstrated yet.
Gut microbiota modulation as treatment of OA
Considering the growing global prevalence of OA, effective disease-modifying therapeutic strategy for relieving symptoms and slowing down OA progress are greatly needed. In this context, it is feasible to hypothesize that the modulation of gut microbiota by external approaches may influence the progression OA. To date, some lines of evidence indicate that gut microbiota interventions may be realized through probiotics, prebiotics, nutraceuticals, exercise, and fecal microbiota transplantation (FMT).
Probiotics and prebiotics
Probiotics are composed of live microorganisms, generally lactic acid bacteria, which play a crucial part in the maintenance of healthy gut microbiota homeostasis by promoting the production of antimicrobial substances and immunoglobulins and inhibiting the production of bacterial toxins [70]. Recent observations gave rise to hopes that probiotics would provide beneficial treatment strategy in OA. To date, the most convincing evidence is a randomized double-blind placebo-controlled trial performed by Lei et al., in which a total of 537 patients with knee OA were enrolled and randomized to receive skimmed milk containing either Lactobacillus casei Shirota (LcS) or placebo daily for 6 months [14]. After 6 months of treatment, clinical outcomes assessed by WOMAC (Western Ontario and McMaster Universities Osteoarthritis Index) and VAS (visual analog scale) scores were significantly reduced in the LcS group compared to the placebo group. Moreover, systematic inflammation assessed by the serum high-sensitivity C-reactive protein (hs-CRP) was also significantly lower in patients receiving LcS than placebo. This study indicates that LcS consumption could serve as a novel therapeutic option in OA management, improving clinical outcomes probably through reducing serum hs-CRP levels. Another study in experimental rodent model of OA found that oral administration of LcS (2 × 1010 cfu/kg, 500 mg/kg) together with glucosamine (Gln; 250 mg/kg) and type II collagen (CII; 250 mg/kg) is effective to reduce pain compared to the control group, while LcS or Gln or CII/Gln alone failed to improve clinical outcome. This study indicated the synergistic effects of LcS/Gln/CII, while the exact weight of each individual treatment is hard to assess and the sample number is insufficient (n = 8~9 in each group) [15]. Sim et al. found that oral administration of tyndallized Clostridium butyricum effectively preserved articular cartilage and synovial membrane and significantly reduced the amount of fibrous tissue, serum concentration of various inflammatory mediators, and bone metabolism markers in a monosodium iodoacetate-induced (MIA) OA rat model [16]. In the same OA model, Kwon et al. claimed that dietary supplements of probiotic complex (12.5 mg/rat) combined with rosavin (100 mg/rat) and zinc (20 mg/rat) to MIA rats (weighted from 140 to 230 g) slowed down OA development through the inhibition of proinflammatory cytokines and cartilage destruction [17]. However, this evidence is far from convincing due to the limited sample number (n = 3) and observation period (13 days). Also, the results were over-interpreted because only pain assessment reached statistical significance while morphology assessments were not significant and the evidence supporting that the combination treatment inhibited inflammation was based on in vitro chondrocyte experiments.
Prebiotics also is selectively utilized by host microorganisms and is able to stimulate the growth of different beneficial bacteria in the gastrointestinal tract [71, 72]. Schott et al. provided evidence that supplementation with oligofructose (OFS) prebiotic fiber, a non-digestible plant-derived carbohydrate, fermented by gut microbiota in the colon, could reverse the adverse effects of high-fat diets on gut microbial composition by increasing the abundance of Bifidobacterium, a species with anti-inflammatory properties, resulting in the reduction of systemic and knee joint inflammation, the preservation of articular cartilage, and the suppression of obesity-induced joint structural changes in the context of injury [18]. These findings indicated that prebiotic manipulation of the gut microbiota is a potentially novel candidate therapeutic strategy to treat OA.
Nutraceuticals
The clinical effects of glucosamine sulfate (GS) and chondroitin sulfate (CS) on OA management is still controversial, even some systematic reviews show their symptomatic and structure-modifying effects contributed by the anti-inflammatory effects on cartilage [73]. In the 2019 guidelines, low-dose, short-term pharmaceutical-grade glucosamine and chondroitin sulfate are recommended by the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) whereas Osteoarthritis Research Society International (OARSI) strongly recommends against their use (including all glucosamine and chondroitin formulations) [74].
Oral supplements of GS and CS have limited intestinal absorption and hence the effects of these supplements on the gut microbiome are of great interest. The systematic review performed by Shmagel et al. summarized the evidence supporting the effects of GS or CS on gut microbial composition that CS increased abundance of genus Bacteroides, while the evidence of GC on gut microbiome is limited [75]. Liu et al. found that CS supplementation was associated with increased Bacteroides acidifaciens, reduced inflammatory Proteobacteria, lower serum LPS levels, and increased level of fecal total SCFA and butyrate in the stressed mice, illustrating that the anti-inflammatory and gut-protective effects of CS supplementation may depend on the specific bacterial species [76]. In particular, Bacteroides species account for more than 10% of all human gut microbiota and are primarily responsible for degrading CS, which could help to explain the efficacy of CS as a potential therapeutic drug in OA treatment [77]. Similarly, Coulson et al. demonstrated that oral supplementation with green-lipped mussel extract or glucosamine sulfate have symptom-modulating effects on OA patients by regulating the composition, metabolic, and immunological activities of gut microbiota [19]. Furthermore, GS and CS are also significant components of intestinal mucin, acting as a defense barrier between gut flora and the intestinal wall and potentially affecting gut permeability and intestinal immune responses [78, 79]. Advanced understanding of the biological action of GS and CS on shaping gut microbiome provides a novel insight into their potential mechanisms in OA management, while the convincing evidence to link GS/CS, gut microbiota, and OA is still needed.
Exercise
The evidence of exercise therapy has indicated the therapeutic benefits by reducing pain and improving functioning for individuals with OA [80]. Beyond the changes of mechanical loading on cartilage and subchondral bone, exercise may modulate the composition, functions, and metabolites of gut microbiota to exert possible benefits for the host [81]. Several mechanisms are involved in the health-promoting effects of exercise, including the improvement of the Bacteroidetes/Firmicutes ratio, the alteration of bile acid profile, the increased production of SCFAs, the suppression of TLR signaling pathway, the mediation of mucosal immunity via production of immunoglobulin A (IgA), reduced intestinal transit time, and the activation of the HPA axis [82].
Exercise independently alters the composition and functional capacity of the gut microbiota or together with dietary supplements. Munukka et al. showed that taxonomic shifts included an enriched abundance of Akkermansia and a decrease in Proteobacteria after 6-week exercise among previously sedentary overweight women [83]. In addition, Jacob et al. performed a study to explore the effects of exercise on gut microbiota in lean and obese participants with multiple-day dietary controls, revealing that exercise increased the abundance of Faecalibacterium species and the concentrations of acetate, butyrate, and SCFAs only in lean subjects [84]. These findings suggest that exercise-induced changes in the human gut microbiota are largely dependent on obesity status. Furthermore, in response to exercise, the gut microbiota of lean individuals may be more responsive than that of obese or overweight individuals. Several studies also indicated that exercise might also be associated with diet determining the microbial biodiversity of the gut. Clarke et al. was the first to find that exercise increases gut microbial diversity that was positively correlated with dietary protein consumption in the athlete group [85].
In spite of the evidence supporting that exercise benefits host by the underlying involvement of gut microbiota, the finding regarding this effects upon the mechanism of exercise in OA patients, so far, is scarce. Rios et al. showed that prebiotic fiber supplementation, aerobic exercise, and the combination of these two interventions completely prevented the development of OA-like knee joint damage in a high-fat/high-sucrose diet-induced rat model of obesity [20]. In particular, the combination of the two interventions resulted in an increased relative abundance of Bifidobacterium and Roseburia negatively associated with knee joint damage induced by diet-induced obesity while a decrease in Clostridium leptum (cluster IV) and Akkemansia muciniphila which exhibited a positive association with joint damage. Future studies should be specifically designed to clarify whether exercise may positively influence this putative gut-joint axis and to investigate the degree to which exercise rebalance gut dysbiosis to influence OA development.
Fecal microbiota transplantation (FMT)
FMT is a manipulation aimed to treat diseases associated with gut microbiota by transferring of feces from a healthy donor into the distal gastrointestinal tract of a recipient patient [86]. Promising findings suggest that this method has already emerged as a successful treatment against Clostridium difficile infection [87] and is currently being demonstrated as a potential therapeutic option of inflammatory bowel disease (IBD) [88]. Also, emerging evidence demonstrates the promising application of FMT in the management of OA. Huang et al. designed a study to collect fecal samples from human healthy controls, knee OA without metabolic syndrome, and knee OA with metabolic syndrome groups, then transplant pooled samples into germ-free OA mice induced by meniscal/ligamentous injury (MLI). Interestingly, only the microbiota transplantation from the knee OA with metabolic syndrome and MLI resulted in an increase in the severity of OA, which was also consistently associated with elevated inflammatory biomarkers and gut permeability [21]. These findings support that an adverse microbiome would exacerbate the histopathological severity of OA induced by joint injury in a murine model. The study is a paradigm for the application of FMT in the investigation of OA pathogenesis and also give promise to the manipulation of gut microbiota in OA management, while more convincing studies are needed due to the limited sample number (n = 9).
Concluding remarks and future perspectives
OA represents a primary public health problem, which is a major source of pain, disability, and socioeconomic cost worldwide. Therefore, interpreting the potential mechanisms of OA pathogenesis is essential for developing novel prevention and disease-modifying therapeutic interventions.
In this narrative review, we summarized the evidence supporting the hypothesis of “gut-joint axis” and the interaction between gut microbiota and the OA-relevant factors and provided the reasonable speculations of the promising manipulation of gut microbiota in OA management. The evidence of the gut microbiota involvements upon the mechanisms of the risk factors, such as obesity and metabolic syndrome and joint injury, is more convincing compared to the others. Given that the intervention on gut microbiota to investigate its role in OA is scarce so far, the connections between gut microbiota and OA risk factors are still inconclusive. As a result, we call for the more convincing human longitudinal studies based on microbiota manipulation. Moreover, it is important to point out that this systematic low-degree inflammation induced by the disturbed gut microbiota is not specific for OA but rather favors the emergence of several potential diseases, such as metabolic syndrome and cardiovascular diseases. In this context, we speculate that the influence of gut microbiota on the OA subtypes may be different. Indeed, most of evidence is based on the Met-OA model, suggesting the potential interaction between gut microbiota, OA, and also other diseases. This adds another layer of complexity to the mechanisms of gut microbiota.
The detailed mechanisms of “gut-joint axis” remain reclusive. It is likely that gut microbiota influences joint by regulating inflammation and metabolism, while the gap between cartilage metabolism and gut microbiota still exists. In the context, multiple omics, such as metabonomic and transcriptomics, are helpful to link specific metabolites, genes, or signaling pathways contributing to the regulation of gut microbiota to decode this intricate matter in a molecular resolution. Also, single-cell technique is promising to reveal the relevance of distinct cell subgroups to gut microbiota. Besides the mechanism investigations, existing evidence also suggests the possibility of novel biomarkers related to inflammation and gut dysbiosis that are able to predict OA progression and monitor the efficacy of therapeutic intervention.
Availability of data and materials
Not applicable.
Abbreviations
- OA:
-
Osteoarthritis
- AGEs:
-
Advanced glycation end products
- SCFA:
-
Short-chain fatty acids
- IGF1:
-
Insulin-like growth factor 1
- GDF5:
-
Growth differentiation factor 5
- VDR:
-
Vitamin D receptor
- GWAS:
-
Genome-wide association analysis
- PUFA:
-
Polyunsaturated fatty acid
- AA:
-
Arachidonic acid
- DHA:
-
Docosahexaenoic acid
- LPS:
-
Lipopolysaccharide
- PGN:
-
Peptidoglycan
- LBP:
-
LPS-binding protein
- HPA:
-
Hypothalamic-pituitary axis
- NTS:
-
Nucleus tractus solitarus
- SCN:
-
Suprachiasmatic nuclei
- ACL:
-
Anterior cruciate ligament
- DAMPs:
-
Damage-associated molecular patterns
- TLRs:
-
Toll-like receptors
- DMM:
-
Destabilized medial meniscus
- SPF:
-
Specific pathogen-free
- LcS:
-
Lactobacillus casei Shirota
- Gln:
-
Glucosamine
- OFS:
-
Oligofructose
- GS:
-
Glucosamine sulfate
- CS:
-
Chondroitin sulfate
- FMT:
-
Fecal microbiota transplantation
- IBD:
-
Inflammatory bowel disease
References
Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, Bridgett L, Williams S, Guillemin F, Hill CL, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1323–30.
Centers for Disease C, Prevention. Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation--United States, 2010-2012. MMWR Morb Mortal Wkly Rep. 2013;62(44):869–73.
Zhao X, Shah D, Gandhi K, Wei W, Dwibedi N, Webster L, Sambamoorthi U. Clinical, humanistic, and economic burden of osteoarthritis among noninstitutionalized adults in the United States. Osteoarthr Cartil. 2019;27(11):1618–26.
Disease GBD, Injury I, Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–858.
Berenbaum F, Wallace IJ, Lieberman DE, Felson DT. Modern-day environmental factors in the pathogenesis of osteoarthritis. Nat Rev Rheumatol. 2018;14(11):674–81.
O'Neill TW, McCabe PS, McBeth J. Update on the epidemiology, risk factors and disease outcomes of osteoarthritis. Best Pract Res Clin Rheumatol. 2018;32(2):312–26.
Berenbaum F. Deep phenotyping of osteoarthritis: a step forward. Ann Rheum Dis. 2019;78(1):3–5.
Adak A, Khan MR. An insight into gut microbiota and its functionalities. Cell Mol Life Sci. 2019;76(3):473–93.
Backhed F, Ley RE, Sonnenburg JL, Peterson DA, Gordon JI. Host-bacterial mutualism in the human intestine. Science. 2005;307(5717):1915–20.
Biver E, Berenbaum F, Valdes AM, Araujo de Carvalho I, Bindels LB, Brandi ML, Calder PC, Castronovo V, Cavalier E, Cherubini A, et al. Gut microbiota and osteoarthritis management: an expert consensus of the European society for clinical and economic aspects of osteoporosis, osteoarthritis and musculoskeletal diseases (ESCEO). Ageing Res Rev. 2019;55:100946.
Collins KH, Paul HA, Reimer RA, Seerattan RA, Hart DA, Herzog W. Relationship between inflammation, the gut microbiota, and metabolic osteoarthritis development: studies in a rat model. Osteoarthr Cartil. 2015;23(11):1989–98.
Guss JD, Ziemian SN, Luna M, Sandoval TN, Holyoak DT, Guisado GG, Roubert S, Callahan RL, Brito IL, van der Meulen MCH, et al. The effects of metabolic syndrome, obesity, and the gut microbiome on load-induced osteoarthritis. Osteoarthr Cartil. 2019;27(1):129–39.
Ulici V, Kelley KL, Azcarate-Peril MA, Cleveland RJ, Sartor RB, Schwartz TA, Loeser RF. Osteoarthritis induced by destabilization of the medial meniscus is reduced in germ-free mice. Osteoarthr Cartil. 2018;26(8):1098–109.
Lei M, Guo C, Wang D, Zhang C, Hua L. The effect of probiotic Lactobacillus casei Shirota on knee osteoarthritis: a randomised double-blind, placebo-controlled clinical trial. Benefic Microbes. 2017;8(5):697–703.
So JS, Song MK, Kwon HK, Lee CG, Chae CS, Sahoo A, Jash A, Lee SH, Park ZY, Im SH. Lactobacillus casei enhances type II collagen/glucosamine-mediated suppression of inflammatory responses in experimental osteoarthritis. Life Sci. 2011;88(7–8):358–66.
Sim BY, Choi HJ, Kim MG, Jeong DG, Lee DG, Yoon JM, Kang DJ, Park S, Ji JG, Joo IH, et al. Effects of ID-CBT5101 in preventing and alleviating osteoarthritis symptoms in a monosodium iodoacetate-induced rat model. J Microbiol Biotechnol. 2018;28(7):1199–208.
Kwon JY, Lee SH, Jhun J, Choi J, Jung K, Cho KH, Kim SJ, Yang CW, Park SH, Cho ML. The combination of probiotic complex, rosavin, and zinc improves pain and cartilage destruction in an osteoarthritis rat model. J Med Food. 2018;21(4):364–71.
Schott EM, Farnsworth CW, Grier A, Lillis JA, Soniwala S, Dadourian GH, Bell RD, Doolittle ML, Villani DA, Awad H, et al. Targeting the gut microbiome to treat the osteoarthritis of obesity. JCI Insight. 2018;3(8):e95997. https://doi.org/10.1172/jci.insight.95997.
Coulson S, Butt H, Vecchio P, Gramotnev H, Vitetta L. Green-lipped mussel extract (Perna canaliculus) and glucosamine sulphate in patients with knee osteoarthritis: therapeutic efficacy and effects on gastrointestinal microbiota profiles. Inflammopharmacology. 2013;21(1):79–90.
Rios JL, Bomhof MR, Reimer RA, Hart DA, Collins KH, Herzog W. Protective effect of prebiotic and exercise intervention on knee health in a rat model of diet-induced obesity. Sci Rep. 2019;9(1):3893.
Huang Z, Chen J, Li B, Zeng B, Chou CH, Zheng X, Xie J, Li H, Hao Y, Chen G, et al. Faecal microbiota transplantation from metabolically compromised human donors accelerates osteoarthritis in mice. Ann Rheum Dis. 2020;79(5):646–56.
Huang ZY, Stabler T, Pei FX, Kraus VB. Both systemic and local lipopolysaccharide (LPS) burden are associated with knee OA severity and inflammation. Osteoarthr Cartil. 2016;24(10):1769–75.
Huang Z, Kraus VB. Does lipopolysaccharide-mediated inflammation have a role in OA? Nat Rev Rheumatol. 2016;12(2):123–9.
Dunn CM, Velasco C, Rivas A, Andrews M, Garman C, Jacob PB, Jeffries MA. Identification of cartilage microbial DNA signatures and associations with knee and hip osteoarthritis. Arthritis Rheumatol. 2020;72(7):1111–22.
Oliveria SA, Felson DT, Reed JI, Cirillo PA, Walker AM. Incidence of symptomatic hand, hip, and knee osteoarthritis among patients in a health maintenance organization. Arthritis Rheum. 1995;38(8):1134–41.
Loeser RF, Collins JA, Diekman BO. Ageing and the pathogenesis of osteoarthritis. Nat Rev Rheumatol. 2016;12(7):412–20.
Rahmati M, Nalesso G, Mobasheri A, Mozafari M. Aging and osteoarthritis: central role of the extracellular matrix. Ageing Res Rev. 2017;40:20–30.
Konturek PC, Haziri D, Brzozowski T, Hess T, Heyman S, Kwiecien S, Konturek SJ, Koziel J. Emerging role of fecal microbiota therapy in the treatment of gastrointestinal and extra-gastrointestinal diseases. J Physiol Pharmacol. 2015;66(4):483–91.
Bischoff SC. Microbiota and aging. Curr Opin Clin Nutr Metab Care. 2016;19(1):26–30.
Biagi E, Franceschi C, Rampelli S, Severgnini M, Ostan R, Turroni S, Consolandi C, Quercia S, Scurti M, Monti D, et al. Gut microbiota and extreme longevity. Curr Biol. 2016;26(11):1480–5.
O'Toole PW, Jeffery IB. Gut microbiota and aging. Science. 2015;350(6265):1214–5.
Biagi E, Nylund L, Candela M, Ostan R, Bucci L, Pini E, Nikkila J, Monti D, Satokari R, Franceschi C, et al. Through ageing, and beyond: gut microbiota and inflammatory status in seniors and centenarians. PLoS One. 2010;5(5):e10667.
Srikanth VK, Fryer JL, Zhai G, Winzenberg TM, Hosmer D, Jones G. A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthr Cartil. 2005;13(9):769–81.
Contartese D, Tschon M, De Mattei M, Fini M. Sex specific determinants in osteoarthritis: a systematic review of preclinical studies. Int J Mol Sci. 2020;21(10):3696. https://doi.org/10.3390/ijms21103696.
Li Y, Luo W, Deng Z, Lei G. Diet-intestinal microbiota axis in osteoarthritis: a possible role. Mediat Inflamm. 2016;2016:3495173.
Org E, Mehrabian M, Parks BW, Shipkova P, Liu X, Drake TA, Lusis AJ. Sex differences and hormonal effects on gut microbiota composition in mice. Gut Microbes. 2016;7(4):313–22.
Haro C, Rangel-Zuniga OA, Alcala-Diaz JF, Gomez-Delgado F, Perez-Martinez P, Delgado-Lista J, Quintana-Navarro GM, Landa BB, Navas-Cortes JA, Tena-Sempere M, et al. Intestinal microbiota is influenced by gender and body mass index. PLoS One. 2016;11(5):e0154090.
Li JY, Chassaing B, Tyagi AM, Vaccaro C, Luo T, Adams J, Darby TM, Weitzmann MN, Mulle JG, Gewirtz AT, et al. Sex steroid deficiency-associated bone loss is microbiota dependent and prevented by probiotics. J Clin Invest. 2016;126(6):2049–63.
Yucesoy B, Charles LE, Baker B, Burchfiel CM. Occupational and genetic risk factors for osteoarthritis: a review. Work. 2015;50(2):261–73.
Michou L. Genetics of digital osteoarthritis. Joint Bone Spine. 2011;78(4):347–51.
Palazzo C, Nguyen C, Lefevre-Colau MM, Rannou F, Poiraudeau S. Risk factors and burden of osteoarthritis. Ann Phys Rehabil Med. 2016;59(3):134–8.
Solovieva S, Hirvonen A, Siivola P, Vehmas T, Luoma K, Riihimaki H, Leino-Arjas P. Vitamin D receptor gene polymorphisms and susceptibility of hand osteoarthritis in Finnish women. Arthritis Res Ther. 2006;8(1):R20.
Wang J, Thingholm LB, Skieceviciene J, Rausch P, Kummen M, Hov JR, Degenhardt F, Heinsen FA, Ruhlemann MC, Szymczak S, et al. Genome-wide association analysis identifies variation in vitamin D receptor and other host factors influencing the gut microbiota. Nat Genet. 2016;48(11):1396–406.
Thomas S, Browne H, Mobasheri A, Rayman MP. What is the evidence for a role for diet and nutrition in osteoarthritis? Rheumatology. 2018;57(suppl_4):iv61–74.
Li Y, Xiao W, Luo W, Zeng C, Deng Z, Ren W, Wu G, Lei G. Alterations of amino acid metabolism in osteoarthritis: its implications for nutrition and health. Amino Acids. 2016;48(4):907–14.
Baker KR, Matthan NR, Lichtenstein AH, Niu J, Guermazi A, Roemer F, Grainger A, Nevitt MC, Clancy M, Lewis CE, et al. Association of plasma n-6 and n-3 polyunsaturated fatty acids with synovitis in the knee: the MOST study. Osteoarthr Cartil. 2012;20(5):382–7.
Mills S, Stanton C, Lane JA, Smith GJ, Ross RP. Precision Nutrition and the Microbiome, Part I: Current State of the Science. Nutrients. 2019;11(4):923. https://doi.org/10.3390/nu11040923.
Kaliannan K, Wang B, Li XY, Kim KJ, Kang JX. A host-microbiome interaction mediates the opposing effects of omega-6 and omega-3 fatty acids on metabolic endotoxemia. Sci Rep. 2015;5:11276.
Ooi JH, Li Y, Rogers CJ, Cantorna MT. Vitamin D regulates the gut microbiome and protects mice from dextran sodium sulfate-induced colitis. J Nutr. 2013;143(10):1679–86.
Assa A, Vong L, Pinnell LJ, Avitzur N, Johnson-Henry KC, Sherman PM. Vitamin D deficiency promotes epithelial barrier dysfunction and intestinal inflammation. J Infect Dis. 2014;210(8):1296–305.
Ghaly S, Kaakoush NO, Lloyd F, McGonigle T, Mok D, Baird A, Klopcic B, Gordon L, Gorman S, Forest C, et al. High dose vitamin D supplementation alters faecal microbiome and predisposes mice to more severe colitis. Sci Rep. 2018;8(1):11511.
Del Pinto R, Ferri C, Cominelli F. Vitamin D Axis in Inflammatory Bowel Diseases: Role, Current Uses and Future Perspectives. Int J Mol Sci. 2017;18(11):2360. https://doi.org/10.3390/ijms18112360.
Ren W, Duan J, Yin J, Liu G, Cao Z, Xiong X, Chen S, Li T, Yin Y, Hou Y, et al. Dietary L-glutamine supplementation modulates microbial community and activates innate immunity in the mouse intestine. Amino Acids. 2014;46(10):2403–13.
Visser AW, Ioan-Facsinay A, de Mutsert R, Widya RL, Loef M, de Roos A, le Cessie S, den Heijer M, Rosendaal FR, Kloppenburg M, et al. Adiposity and hand osteoarthritis: the Netherlands epidemiology of obesity study. Arthritis Res Ther. 2014;16(1):R19.
Jiang L, Xie X, Wang Y, Wang Y, Lu Y, Tian T, Chu M, Shen Y. Body mass index and hand osteoarthritis susceptibility: an updated meta-analysis. Int J Rheum Dis. 2016;19(12):1244–54.
Puenpatom RA, Victor TW. Increased prevalence of metabolic syndrome in individuals with osteoarthritis: an analysis of NHANES III data. Postgrad Med. 2009;121(6):9–20.
Courties A, Sellam J, Berenbaum F. Metabolic syndrome-associated osteoarthritis. Curr Opin Rheumatol. 2017;29(2):214–22.
Murphy SL, Phillips K, Williams DA, Clauw DJ. The role of the central nervous system in osteoarthritis pain and implications for rehabilitation. Curr Rheumatol Rep. 2012;14(6):576–82.
Dobson GP, Letson HL, Grant A, McEwen P, Hazratwala K, Wilkinson M, Morris JL. Defining the osteoarthritis patient: back to the future. Osteoarthr Cartil. 2018;26(8):1003–7.
Morris JL, Letson HL, Gillman R, Hazratwala K, Wilkinson M, McEwen P, Dobson GP. The CNS theory of osteoarthritis: opportunities beyond the joint. Semin Arthritis Rheum. 2019;49(3):331–6.
Mayer EA, Tillisch K, Gupta A. Gut/brain axis and the microbiota. J Clin Invest. 2015;125(3):926–38.
Tillisch K. The effects of gut microbiota on CNS function in humans. Gut Microbes. 2014;5(3):404–10.
Leone V, Gibbons SM, Martinez K, Hutchison AL, Huang EY, Cham CM, Pierre JF, Heneghan AF, Nadimpalli A, Hubert N, et al. Effects of diurnal variation of gut microbes and high-fat feeding on host circadian clock function and metabolism. Cell Host Microbe. 2015;17(5):681–9.
Liang X, Bushman FD, FitzGerald GA. Rhythmicity of the intestinal microbiota is regulated by gender and the host circadian clock. Proc Natl Acad Sci U S A. 2015;112(33):10479–84.
Thomas AC, Hubbard-Turner T, Wikstrom EA, Palmieri-Smith RM. Epidemiology of posttraumatic osteoarthritis. J Athl Train. 2017;52(6):491–6.
Lieberthal J, Sambamurthy N, Scanzello CR. Inflammation in joint injury and post-traumatic osteoarthritis. Osteoarthr Cartil. 2015;23(11):1825–34.
Shi H, Kokoeva MV, Inouye K, Tzameli I, Yin H, Flier JS. TLR4 links innate immunity and fatty acid-induced insulin resistance. J Clin Invest. 2006;116(11):3015–25.
Capurso G, Lahner E. The interaction between smoking, alcohol and the gut microbiome. Best Pract Res Clin Gastroenterol. 2017;31(5):579–88.
Lee SH, Yun Y, Kim SJ, Lee EJ, Chang Y, Ryu S, Shin H, Kim HL, Kim HN, Lee JH. Association between cigarette smoking status and composition of gut microbiota: population-based cross-sectional study. J Clin Med. 2018;7(9):282. https://doi.org/10.3390/jcm7090282.
de Oliveira GLV, Leite AZ, Higuchi BS, Gonzaga MI, Mariano VS. Intestinal dysbiosis and probiotic applications in autoimmune diseases. Immunology. 2017;152(1):1–12.
Gibson GR, Hutkins R, Sanders ME, Prescott SL, Reimer RA, Salminen SJ, Scott K, Stanton C, Swanson KS, Cani PD, et al. Expert consensus document: The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of prebiotics. Nat Rev Gastroenterol Hepatol. 2017;14(8):491–502.
Markowiak P, Slizewska K. Effects of probiotics, prebiotics, and synbiotics on human health. Nutrients. 2017;9(9):1021. https://doi.org/10.3390/nu9091021.
Bruyere O, Altman RD, Reginster JY. Efficacy and safety of glucosamine sulfate in the management of osteoarthritis: evidence from real-life setting trials and surveys. Semin Arthritis Rheum. 2016;45(4 Suppl):S12–7.
Arden NK, Perry TA, Bannuru RR, Bruyere O, Cooper C, Haugen IK, Hochberg MC, McAlindon TE, Mobasheri A, Reginster JY. Non-surgical management of knee osteoarthritis: comparison of ESCEO and OARSI 2019 guidelines. Nat Rev Rheumatol. 2021;17(1):59–66.
Shmagel A, Demmer R, Knights D, Butler M, Langsetmo L, Lane NE, Ensrud K. The effects of glucosamine and chondroitin sulfate on gut microbial composition: a systematic review of evidence from animal and human studies. Nutrients. 2019;11(2):294. https://doi.org/10.3390/nu11020294.
Liu F, Zhang N, Li Z, Wang X, Shi H, Xue C, Li RW, Tang Q. Chondroitin sulfate disaccharides modified the structure and function of the murine gut microbiome under healthy and stressed conditions. Sci Rep. 2017;7(1):6783.
Shang Q, Yin Y, Zhu L, Li G, Yu G, Wang X. Degradation of chondroitin sulfate by the gut microbiota of Chinese individuals. Int J Biol Macromol. 2016;86:112–8.
Lee HS, Han SY, Ryu KY, Kim DH. The degradation of glycosaminoglycans by intestinal microflora deteriorates colitis in mice. Inflammation. 2009;32(1):27–36.
Sicard JF, Vogeleer P, Le Bihan G, Rodriguez Olivera Y, Beaudry F, Jacques M, Harel J. N-acetyl-glucosamine influences the biofilm formation of Escherichia coli. Gut Pathog. 2018;10:26.
Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty M, et al. OARSI recommendations for the management of hip and knee osteoarthritis, part II: OARSI evidence-based, expert consensus guidelines. Osteoarthr Cartil. 2008;16(2):137–62.
Monda V, Villano I, Messina A, Valenzano A, Esposito T, Moscatelli F, Viggiano A, Cibelli G, Chieffi S, Monda M, et al. Exercise modifies the gut microbiota with positive health effects. Oxidative Med Cell Longev. 2017;2017:3831972.
Cerda B, Perez M, Perez-Santiago JD, Tornero-Aguilera JF, Gonzalez-Soltero R, Larrosa M. Gut microbiota modification: another piece in the puzzle of the benefits of physical exercise in health? Front Physiol. 2016;7:51.
Munukka E, Ahtiainen JP, Puigbo P, Jalkanen S, Pahkala K, Keskitalo A, Kujala UM, Pietila S, Hollmen M, Elo L, et al. Six-week endurance exercise alters gut metagenome that is not reflected in systemic metabolism in over-weight women. Front Microbiol. 2018;9:2323.
Allen JM, Mailing LJ, Niemiro GM, Moore R, Cook MD, White BA, Holscher HD, Woods JA. Exercise alters gut microbiota composition and function in lean and obese humans. Med Sci Sports Exerc. 2018;50(4):747–57.
Clarke SF, Murphy EF, O'Sullivan O, Lucey AJ, Humphreys M, Hogan A, Hayes P, O'Reilly M, Jeffery IB, Wood-Martin R, et al. Exercise and associated dietary extremes impact on gut microbial diversity. Gut. 2014;63(12):1913–20.
Cammarota G, Ianiro G, Tilg H, Rajilic-Stojanovic M, Kump P, Satokari R, Sokol H, Arkkila P, Pintus C, Hart A, et al. European consensus conference on faecal microbiota transplantation in clinical practice. Gut. 2017;66(4):569–80.
Hamilton MJ, Weingarden AR, Sadowsky MJ, Khoruts A. Standardized frozen preparation for transplantation of fecal microbiota for recurrent Clostridium difficile infection. Am J Gastroenterol. 2012;107(5):761–7.
Weingarden AR, Vaughn BP. Intestinal microbiota, fecal microbiota transplantation, and inflammatory bowel disease. Gut Microbes. 2017;8(3):238–52.
Acknowledgements
This study was supported by National Natural Science Foundation of China (Grant No. 81772440).
Funding
This study was supported by National Natural Science Foundation of China (Grant No. 81772440).
Author information
Authors and Affiliations
Contributions
XXH performed the literature research and wrote the original draft of the manuscript; XRS, JWL, and RMC studied conception and literature search; JMZ and TX evaluated the information and reviewed and defined the last version of manuscript. The authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All the authors agree for publication.
Competing interests
The authors declared no conflict of interests about the publication of this paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hao, X., Shang, X., Liu, J. et al. The gut microbiota in osteoarthritis: where do we stand and what can we do?. Arthritis Res Ther 23, 42 (2021). https://doi.org/10.1186/s13075-021-02427-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13075-021-02427-9