Abstract
Background
Biologic disease-modifying antirheumatic drugs (bDMARDs) are important options for managing rheumatoid arthritis (RA). Once patients achieve disease control, clinicians may consider dose reduction or withdrawal of the bDMARD. Results from published studies indicate that some patients will maintain remission; however, others will flare. We analyzed data from three etanercept down-titration studies in patients with RA to determine what extent of remission provides the greatest predictability of maintaining remission following dose reduction or discontinuation.
Methods
Patients with moderate to severe RA from the PRESERVE, PRIZE, and Treat-to-Target (T2T) randomized controlled trials were included. We determined the proportion of patients achieving remission with etanercept at the last time point in the induction period, and sustained remission (last two time points), according to the Disease Activity Score 28-joints (DAS28), the American College of Rheumatology (ACR)/European League Against Rheumatism (EULAR) Boolean criteria, and the clinical disease activity index (CDAI). We also calculated the proportion achieving DAS28 deep remission (DAS28 ≤ 1.98), sustained deep remission (last two time points), and low disease activity (LDA), and LDA according to the CDAI. Then, we evaluated whether they maintained remission or LDA following etanercept dose reduction or withdrawal.
Results
Patients achieving sustained and/or deep remission were more likely than patients achieving remission or LDA to maintain remission/LDA after etanercept dose reduction or withdrawal. In PRESERVE, the proportions of patients with DAS28 sustained deep remission, deep remission, sustained remission, remission, and LDA who maintained remission following etanercept dose reduction were 81%, 67%, 58%, 56%, and 36%, respectively, P < 0.001 for trend. In PRESERVE, this trend was significant when etanercept was discontinued and when ACR/EULAR Boolean and CDAI remission criteria were used. Although some sample sizes were small, the PRIZE and T2T studies also demonstrated response trends according to ACR/EULAR Boolean and CDAI remission criteria, and T2T demonstrated response trends according to DAS28.
Conclusions
These results suggest that patients achieving disease control according to a stringent definition, such as sustained ACR/EULAR Boolean or CDAI remission, or a new definition of sustained deep remission by DAS28, have a higher probability of remaining in remission or LDA following etanercept dose reduction or withdrawal.
Trial registration
PRESERVE: ClinicalTrials.gov identifier: NCT00565409, registered 30 November 2007; PRIZE: ClinicalTrials.gov identifier: NCT00913458, registered 4 June 2009; T2T: ClinicalTrials.gov identifier: NCT01578850, registered 17 April 2012
Similar content being viewed by others
Background
Treatment guidelines for rheumatoid arthritis (RA) recommend intensive therapy targeting clinical remission early in the disease course, when patients have a higher likelihood of responding to treatment [1,2,3,4,5]. This treatment target has been shown to correlate with better patient-reported outcomes, greater productivity, and lower overall healthcare costs than achieving low disease activity (LDA) [6, 7].
Biologic disease-modifying antirheumatic drugs (bDMARDs) are important therapeutic options in this treat-to-target strategy. However, once patients achieve disease control, clinicians may consider dose reduction or withdrawal of the bDMARD out of concerns for infection risk, dose-dependent adverse events, or treatment cost [8, 9]. As noted in review articles, studies evaluating down-titration of bDMARDs have used various protocols with respect to baseline disease activity and the length of time that RA symptoms were under control before dose reduction or withdrawal of the bDMARD [8,9,10,11,12,13,14,15,16]. For example, studies have required patients to have LDA according to Disease Activity Score 28-joint count (DAS28 ≤ 3.2) for 6 months [17, 18] or DAS28 remission (DAS28 < 2.6) for 6 months [19, 20] or 12 months [21], LDA according to DAS28 or clinician judgment for 3 months [22, 23], moderate to good European League Against Rheumatism (EULAR) response at month 6 [24], or remission according to the clinical disease activity index (CDAI) at month 6 [25].
Published success rates following bDMARD dose reduction or withdrawal vary widely; in many studies, approximately 40–60% of patients were able to maintain remission or LDA, while the remaining patients experienced a flare [8,9,10,11,12,13,14,15,16]. A higher percentage of patients tend to flare if the bDMARD is withdrawn rather than decreased in dose [1, 8,9,10,11, 13].
According to treatment guidelines issued by EULAR, the Asia Pacific League of Associations for Rheumatology (APLAR), and the American College of Rheumatology (ACR), clinicians may consider tapering the bDMARD when a patient is in persistent remission [1,2,3]. Unfortunately, it is not possible to predict with 100% certainty which patients will maintain remission following dose reduction or withdrawal. This is an ongoing area of research; one study with a published protocol, PREDICTRA, is evaluating which disease and patient characteristics may be useful in predicting the outcome of tapering a bDMARD [26]. Evidence from published studies to date suggests that predictors for successful tapering include early RA, remission duration of at least 6 months, and certain clinical signs such as normal levels of inflammatory markers and/or absence of synovitis on ultrasound [8, 27]. One study that evaluated the relationship between psychological factors and flare with dose decrease found that baseline scores on the 36-Item Short Form Survey Mental Health component and the DAS28 were significant predictors of flare [28].
Analyses from two open-label, nonrandomized clinical studies (RRR and HONOR) evaluated whether achieving DAS28 remission according to a lower cut-off value than 2.6 (referred to as deep remission) would enable more patients to maintain DAS28 remission or LDA following bDMARD discontinuation [29, 30]. In the RRR trial (n = 102 patients), the significant DAS28 cut-off point was determined to be < 2.225; in the HONOR trial (n = 52 patients), it was 1.98 [29, 30].
However, measurement of remission with the DAS28 has been criticized since patients can achieve DAS28 remission but still have active disease, such as tender and swollen joints [31]. Additionally, studies have shown that if the DAS28 cut-points are used with therapies that directly affect the acute-phase response, such as interleukin (IL)-6 inhibitors or Janus kinase (JAK) inhibitors, significant residual disease activity is likely to remain [32,33,34]. This is the case even if the more stringent remission cut-points of DAS28 (calculated using C-reactive protein [CRP]) < 1.9 and DAS28 (calculated using erythrocyte sedimentation rate [ESR]) < 2.2 are used [32, 35]. Therefore, alternative outcome measures, such as the ACR/EULAR index-based or Boolean remission criteria, the CDAI, or the Simplified Disease Activity Index (SDAI), should also be considered when evaluating predictors for maintaining remission following bDMARD dose reduction or discontinuation.
Based on results from the literature, we hypothesized that achieving sustained remission (ACR/EULAR Boolean or CDAI remission criteria) or sustained deep remission (DAS28 remission criteria) will increase the likelihood of maintaining remission or LDA following dose reduction or discontinuation of bDMARD therapy. We conducted a post hoc analysis of data from three etanercept down-titration studies in patients with RA to determine what extent of remission will provide the greatest predictability of maintaining remission following dose reduction or discontinuation. The objectives of this analysis were to (1) compare baseline characteristics of patients who achieved sustained deep remission, deep remission, sustained remission, remission, and LDA with full-dose etanercept therapy; (2) determine if the extent of the initial response was predictive of the likelihood of maintaining remission or LDA after the etanercept dose was decreased or discontinued; and (3) compare rates of remission and LDA measured according to the DAS28 criteria, rates of remission measured according to the ACR/EULAR Boolean criteria, and rates of remission and LDA measured according to the CDAI criteria.
Methods
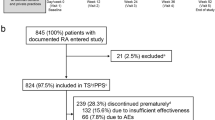
This analysis included patients with RA from three randomized, controlled clinical trials (PRESERVE, PRIZE, and Treat-to-Target [T2T]) that consisted of an open-label induction period with etanercept 50 mg weekly (period 1) followed by a double-blind maintenance, reduction, or withdrawal period (period 2) [17, 36, 37]. The populations differed among the studies, the patients in PRESERVE had moderate RA disease activity and a mean disease duration of 6.9 years, and the patients in PRIZE and T2T had moderate to high (“moderate-to-severe”) RA disease activity and mean disease durations of 6.5 months and 8.0 years, respectively [17, 36]. Additional details of the study designs are presented in Table 1. Patients were included in this analysis if they completed period 1 and were randomized into period 2.
The three studies were conducted according to the International Conference on Harmonization guidelines for Good Clinical Practice as well as the ethical principles of the Declaration of Helsinki. All patients provided informed consent prior to enrolment, and the institutional review board or independent ethics committee at each participating center reviewed and approved the study protocol and consent forms (see “Acknowledgments” for details).
For all treatment groups in the PRESERVE, PRIZE, and T2T studies, clinical response at the last time point in period 1 was determined according to three different remission criteria: DAS28, ACR/EULAR Boolean, and CDAI. Sustained responses were measured at the last two time points in period 1, which were as follows: PRESERVE—weeks 28 and 36; PRIZE—weeks 39 and 52; and T2T—weeks 16 and 24. In each study, DAS28 was calculated using ESR [38].
Specifically, the following responses, in order of disease activity, were measured at the end of period 1:
-
DAS28 remission criteria [38]:
-
Sustained deep remission (deep remission at the last two time points, with deep remission defined as DAS28 ≤ 1.98) [30]
-
Deep remission
-
Sustained remission (remission at the last two time points, with remission defined as DAS28 > 1.98 to < 2.6)
-
Remission
-
LDA (DAS28 ≥ 2.6 to < 3.2; PRESERVE and T2T)
-
-
ACR/EULAR Boolean remission criteria [39]:
-
Sustained Boolean remission (remission at the last two time points, with remission defined as tender joint count (TJC) ≤ 1, swollen joint count (SJC) ≤ 1, C-reactive protein (CRP) ≤ 1 mg/dL, and patient global assessment ≤ 1 on a 0–10 scale)
-
Remission
-
Nonremission
-
-
CDAI remission criteria [40]:
-
Sustained CDAI remission (remission at the last two time points, with remission defined as CDAI 0.0–2.8)
-
Remission
-
LDA (CDAI > 2.8–10.0)
-
Moderate disease activity (CDAI > 10.0–22.0; PRESERVE and T2T)
-
For the PRIZE study, we did not include DAS28 LDA at the end of period 1 because only patients who achieved remission at the end of period 1 were allowed to enter period 2. Additionally, we did not include CDAI moderate disease activity for PRIZE because there were no patients in this category at the end of period 1.
Then, the proportion of patients maintaining remission or LDA (DAS28 and CDAI criteria only) in period 2 was determined according to each response level in period 1. Period 2 response (remission or LDA) was measured only at the last time point in period 2 (PRESERVE: week 88, PRIZE: week 91, T2T: week 52). Patients with remission or LDA at the last time point in period 2 were considered to have maintained that response following dose decrease or withdrawal of etanercept. However, it is unknown whether those patients were in remission or LDA at other time points in period 2.
Demographic and baseline disease characteristics of the patients in each study were categorized according to the following DAS28 responses at the end of period 1: sustained deep remission, deep remission, sustained remission, remission, and LDA (LDA for PRESERVE and T2T), and also according to the following CDAI responses at the end of period 1: sustained remission, remission, LDA, and moderate disease activity (MDA) (MDA for PRESERVE and T2T).
Statistical analyses
Trend in baseline characteristics among the period 1 response categories (DAS28 or CDAI) was analyzed using one-way analysis of variance for continuous variables with response categories treated as ordered, and the Cochran-Mantel-Haenszel (CMH) test of linear association for categorical variables. The CMH test was also used to evaluate the trend in proportion of responders (i.e., remission or LDA) in period 2 among period 1 responders, using a last observation carried forward approach within period 2.
We conducted two additional analyses. We determined the proportion of patients with a normal value on the Health Assessment Questionnaire (HAQ ≤ 0.5) at the end of period 1 according to whether or not they achieved sustained DAS28 deep remission at the end of period 1. Finally, we conducted four stepwise predictor analyses and a sensitivity analysis to determine the best subset of significant predictors in maintaining DAS28 remission in period 2. The predictors from period 1 baseline that were included in the analyses were selected because each of them had a significant relationship with period 1 DAS28 response categories. In the first stepwise analysis, the predictors included sustained deep remission, age in 10-year units, gender, HAQ ≤ 0.5, ESR ≤ upper limit of normal (ULN), body mass index (BMI ≤ 18.5, > 18.5 to ≤ 30, > 30), SJC = 0 out of 28, and TJC = 0 out of 28. Additional stepwise predictor analyses included the following predictors: study and period 2 treatment group and/or continuous rather than dichotomous BMI and SJC/TJC.
Results
Clinical response in period 1 and baseline characteristics according to clinical response
This analysis includes 600, 598, and 594 patients in the ACR/EULAR Boolean, CDAI, and DAS28 remission criteria calculations, respectively, from the PRESERVE study; 193, 192, and 192 patients, respectively, from the PRIZE study; and 331 patients in all three remission criteria calculations from the T2T study. This variability is due to (1) five patients in PRESERVE with DAS28 values > 3.2 at week 36 and one patient with a missing DAS28 value being excluded from the DAS28 analysis, (2) one patient in PRIZE with DAS28 > 2.6 at week 52 being excluded from the DAS28 analysis, and (3) three patients (two from PRESERVE and one from PRIZE) missing component(s) required for calculating CDAI remission.
Table 2 presents the proportion of patients in each DAS28 response category at the end of period 1, as well as demographics and baseline disease characteristics according to each DAS28 response at the end of period 1. All three studies demonstrated a significant difference in mean age according to response category, with younger age being associated with a better DAS28 response in period 1. Lower values for ESR, DAS28-ESR, and HAQ were associated with a better response in PRESERVE and T2T; as were lower values for TJC and CDAI, and a lower proportion of females in T2T; lower BMI in women in PRESERVE and PRIZE; and lower SJC in PRIZE.
The proportion of patients in each CDAI response category at the end of period 1 and demographics and baseline disease characteristics according to each CDAI response are presented in Additional file 1: Table S1. In all three studies, younger age was associated with a better clinical response. In the PRESERVE and PRIZE studies, prior treatment with a corticosteroid was associated with a poorer clinical response, and higher baseline ESR, lower TJC, lower SJC, and lower BMI in women were associated with a better clinical response. In PRESERVE, lower CDAI, physician’s global assessment, and HAQ were each associated with a better clinical response, as were positive laboratory results for rheumatoid factor and anti-cyclic citrullinated peptide antibodies in PRIZE.
The proportion of patients achieving each ACR/EULAR Boolean criteria response at the end of period 1 is provided in Additional file 1: Table S2.
Predictor analyses
All four stepwise predictor analyses and the sensitivity analysis determined that at the end of period 1, the significant predictors of period 2 DAS28 remission were sustained deep remission, ESR ≤ ULN, SJC = 0, and TJC = 0. Since ESR is included in the DAS28 calculation, this association is expected. Study and treatment group were also determined to be significant predictors. Patients who continued etanercept 50 mg were most likely to have DAS28 remission at the end of period 2, followed by patients who decreased the dose to 25 mg, and lastly by patients who discontinued etanercept. When SJC and TJC were treated as continuous, they were found to be significant as well. HAQ ≤ 0.5, age, gender, and BMI were not significant predictors. The significant results from one of the predictor analyses are presented in Table 3.
Clinical response in period 2
PRESERVE study
Patients in the PRESERVE study demonstrated significant remission response trends in period 2 for all three measurement criteria in all treatment groups. Patients who achieved DAS28 sustained deep remission in period 1 and then discontinued etanercept were more likely to maintain DAS28 remission in period 2 (25/41, 61%) than those who achieved deep remission (13/44, 30%), sustained remission (10/34, 29%), remission (8/39, 21%), or LDA (2/39, 5%), P < 0.001 for trend (Fig. 1a). These patients were also more likely to maintain DAS28 LDA (31/41, 76%) than those who initially achieved deep remission (16/44, 36%), sustained remission (14/34, 41%), remission (18/39, 46%), or LDA (10/39, 26%), P < 0.001. The patients who achieved sustained deep remission in period 1 and then decreased the dose of etanercept to 25 mg were more likely to maintain remission in period 2 (35/43, 81%) than those who achieved deep remission (29/43, 67%), sustained remission (22/38, 58%), remission (20/36, 56%), or LDA (14/39, 36%), P < 0.001. The response trend was not significant for maintenance of LDA.
Proportion of patients in the PRESERVE study maintaining remission or LDA in period 2, according to response category in period 1 for the remission criteria of DAS28 (a), ACR/EULAR Boolean (b), and CDAI (c). ACR American College of Rheumatology, CDAI Clinical Disease Activity Index, DAS28 Disease Activity Score in 28 joints, ETN50 etanercept 50 mg, EULAR European League Against Rheumatism, LDA low disease activity, MTX methotrexate, PBO placebo
The patients who achieved sustained remission in period 1 based on the ACR/EULAR Boolean criteria and then discontinued etanercept were more likely to maintain remission (10/34, 29%) than those who achieved remission (7/45, 16%) or did not achieve remission (4/119, 3%) in period 1, P < 0.001 (Fig. 1b). Patients who decreased the dose had a numerically greater response than those who discontinued; the patients with sustained remission in period 1 were more likely to maintain remission (32/44, 73%) than those who achieved remission (12/32, 38%) or did not achieve remission (23/125, 18%), P < 0.001.
In the CDAI analysis, patients in all treatment groups were more likely to maintain remission or LDA in period 2 if they achieved sustained remission in period 1. Additionally, patients who decreased the dose of etanercept had a numerically greater response than those who discontinued etanercept (Fig. 1c). Of the patients who achieved sustained remission in period 1 and then discontinued etanercept, 7/23 (30%) and 19/23 (83%) maintained remission and LDA, respectively, versus 4/33 (12%) and 16/33 (48%) who achieved remission, 11/129 (9%) and 70/129 (54%) who achieved LDA, and 0/11 (0%) and 2/11 (18%) who achieved moderate disease activity, P < 0.01 for both. Of the patients who achieved sustained remission in period 1 and then decreased the dose of etanercept, 26/36 (72%) and 33/36 (92%) maintained remission and LDA, respectively, versus 15/30 (50%) and 24/30 (80%) who achieved remission, 23/127 (18%) and 105/127 (83%) who achieved LDA, and 0/8 (0%) and 2/8 (25%) who achieved moderate disease activity, P < 0.001 for remission and P < 0.05 for LDA.
PRIZE study
Patients in the PRIZE study demonstrated significant response trends for all treatment groups according to ACR/EULAR Boolean criteria, and for two treatment groups according to CDAI criteria, with no significant response trends observed according to DAS28 criteria.
In the DAS28 analysis, the group that decreased the dose of etanercept demonstrated a better response than the groups that discontinued etanercept and discontinued etanercept+methotrexate (MTX) (Fig. 2a).
Proportion of patients in the PRIZE study maintaining remission or LDA in period 2, according to response category in period 1 for the remission criteria of DAS28 (a), ACR/EULAR Boolean (b), and CDAI (c). ACR American College of Rheumatology, CDAI Clinical Disease Activity Index, DAS28 Disease Activity Score in 28 joints, ETN50 etanercept 50 mg, EULAR European League Against Rheumatism, LDA low disease activity, MTX methotrexate, PBO placebo
In the ACR/EULAR Boolean remission criteria analysis, some of the sample sizes were small (Fig. 2b). In the group that decreased the dose of etanercept, period 2 remission was maintained by 7/8 (88%) patients with period 1 sustained remission, versus 3/11 (27%) with remission and 7/44 (16%) without remission in period 1, P < 0.01. In the group that discontinued etanercept, remission was maintained by 6/9 (67%), 2/10 (20%), and 5/46 (11%), respectively, P < 0.001. In the group that discontinued etanercept+MTX, remission was maintained by 8/13 (62%), 3/6 (50%), and 0/46 (0%), respectively, P < 0.001.
In the CDAI analysis, a significant response trend was present for the group that decreased the dose of etanercept and the group that discontinued etanercept+MTX (Fig. 2c). In the dose reduction group, period 2 remission was maintained by 34/40 (85%) of patients with sustained remission in period 1 versus 4/8 (50%) and 7/15 (47%) with remission and LDA, respectively, P < 0.01. In the group that discontinued etanercept+MTX, period 2 remission was maintained by 16/31 (52%) with sustained remission in period 1, versus 0/13 (0%) and 3/20 (15%) with remission and LDA, respectively, P < 0.01.
T2T study
Patients in the T2T study demonstrated significant response trends in period 2 across all measurement criteria in all treatment groups, although in many instances, the sample sizes were small. In most cases, the patients who continued etanercept 50 mg in period 2 demonstrated higher rates of remission and LDA than those who discontinued etanercept. For the group that discontinued etanercept, DAS28 remission was maintained in period 2 by 3/3 (100%) patients with sustained deep remission in period 1 and by 6/15 (40%), 2/8 (25%), 7/35 (20%), and 4/107 (4%) patients with deep remission, sustained remission, remission, and LDA, respectively, P < 0.001 (Fig. 3a). DAS28 LDA was maintained by 3/3 (100%), 6/15 (40%), 2/8 (25%), 10/35 (29%), and 8/107 (7%) patients, respectively, P < 0.001.
Proportion of patients in the T2T study maintaining remission or LDA in period 2, according to response category in period 1 for the remission criteria of DAS28 (a), ACR/EULAR Boolean (b), and CDAI (c). ACR American College of Rheumatology, CDAI Clinical Disease Activity Index, csDMARDs conventional synthetic disease-modifying antirheumatic drugs, DAS28 Disease Activity Score in 28 joints, ETN50 etanercept 50 mg, EULAR European League Against Rheumatism, LDA low disease activity, MTX methotrexate, PBO placebo
In the ACR/EULAR Boolean analysis, the proportion of patients who discontinued etanercept and maintained remission was 4/7 (57%), 9/29 (31%), and 4/132 (3%) of the patients with sustained remission, remission, and nonremission in period 1, respectively, P < 0.001 (Fig. 3b). In the CDAI analysis, the proportion of patients who discontinued etanercept and maintained remission was 2/6 (33%), 7/18 (39%), 11/128 (9%), and 0/16 (0%) of the patients with sustained remission, remission, LDA, and moderate disease activity in period 1, respectively, P < 0.001; LDA was maintained by 3/6 (50%), 13/18 (72%), 53/128 (41%), and 3/16 (19%), P < 0.01 (Fig. 3c).
In all three studies, continuing etanercept 50 mg or decreasing the dose to 25 mg resulted in a greater proportion of patients maintaining remission or LDA than discontinuing etanercept.
Sustained DAS28 deep remission and the Health Assessment Questionnaire
The proportion of patients with a normal HAQ score at the end of period 1 was significantly higher for those patients who achieved sustained DAS28 deep remission at the end of period 1 than for those who did not, in all three studies (Additional file 1: Figure S1). In PRESERVE, 82.0% of patients with sustained DAS28 deep remission had a HAQ score ≤ 0.5, compared with 59.2% of patients who did not achieve sustained DAS28 deep remission, P < 0.001. The corresponding values for PRIZE were 94.0% vs 75.0%, P = 0.001, and for T2T, 91.7% vs 51.4%, P = 0.006.
Discussion
The results of this analysis demonstrate that overall, the likelihood of patients maintaining remission or LDA following dose reduction or discontinuation of etanercept follows a significant trend, with those initially achieving sustained deep remission being the most likely to maintain a response, followed by those achieving deep remission and sustained remission. This was the case whether remission was measured using DAS28 (except in PRIZE), ACR/EULAR Boolean, or CDAI criteria. Additionally, a greater proportion of patients maintained LDA than remission.
It is of interest to note that most of the remission trend results were similar across the studies, even though the patient populations were different. The PRESERVE and T2T studies represented an established RA population; patients had a disease duration of approximately 7 to 8 years. Conversely, the PRIZE study represented an early RA population with a mean disease duration of 6.5 months. The mean number of prior csDMARDs was slightly higher in the PRESERVE and T2T studies (1.3 for each) than in the PRIZE study (1.0), likely owing to the shorter disease duration in PRIZE. Patients in the PRESERVE and PRIZE studies were bDMARD naïve; only one patient in T2T had a history of bDMARD therapy.
In the PRIZE study, a relatively high proportion of patients achieved sustained deep remission in period 1 compared to the other levels of remission and compared to the other two studies. This result may be related to these patients having early disease, although the PRIZE study also had the longest period of open-label etanercept treatment. In this study only, the response trend according to the DAS28 criteria was not significant, suggesting that in patients with early disease, it may be more appropriate to use the ACR/EULAR Boolean or CDAI remission criteria than the DAS28.
In the HONOR and RRR trials, 80% and 71% of patients with DAS28 deep remission were able to maintain LDA following discontinuation of adalimumab and infliximab, respectively [29, 30]. In the current analysis, the proportions of patients with DAS28 sustained deep remission/deep remission in period 1 who maintained LDA following discontinuation of etanercept were 76%/36%, 75%/78%, and 100%/40% for PRESERVE, PRIZE, and T2T, respectively. Many of these values are similar to those reported in HONOR and RRR [29, 30].
For patients, improvement in functional disability is an important aspect of RA treatment, because it affects daily activities, the ability to work, and long-term morbidity and mortality [41,42,43]. We found that the proportion of patients with a normal HAQ score at the end of period 1 was significantly higher for those patients who achieved sustained DAS28 deep remission at the end of period 1 than for those who did not, in all three studies. These results are in line with a published study that found that improvement in the HAQ score continues if LDA or remission is achieved and sustained [44]. Another study determined through multivariate analyses that having a lower HAQ score at the start of treatment predicts 2-year sustained DAS28 remission [45]. In our analysis, we did not find HAQ ≤ 0.5 to be among the best subset of significant predictors in maintaining DAS28 remission; however, lower baseline values for HAQ were associated with a better period 1 DAS28 response in PRESERVE and T2T, and a better CDAI response in PRESERVE.
This study has several limitations. The data pertain to etanercept and likely to other tumor necrosis factor (TNF) inhibitors, but not to IL-6 or JAK inhibitors that directly affect the acute-phase response and as a result, may lead to unduly low DAS28 values. Further, the patients included in this study had moderate or moderate-to-severe RA disease activity, so these results may not be applicable to patients with mild or low RA disease activity; however, in these patients, bDMARDs are rarely indicated or reimbursed. In the PRIZE and T2T studies, the sample sizes were small for many of the remission categories at the end of period 1; therefore, the period 2 results need to be interpreted with caution. Also, the duration of exposure to etanercept differed among the three studies, and this is a variable that must be considered when evaluating the results. Additionally, we cannot draw conclusions regarding maintenance of remission or LDA for periods longer than in these studies. Finally, caution should be exercised when generalizing these results to all patients, because the patients in these clinical trials were selected based on strict inclusion and exclusion criteria.
In future studies, it would be interesting to evaluate whether differences between sustained deep remission, deep remission, sustained remission, remission, and LDA are noted on ultrasound. Studies have found that approximately 50–75% of patients with RA in clinical remission still have active synovitis on ultrasound [46,47,48,49,50,51]. One study that evaluated patients with deep clinical remission (DAS28 ≤ 1.98) and remission (DAS28 ≤ 2.6 but > 1.98) found that significantly fewer patients with deep remission compared to remission had evidence of synovitis on ultrasound [51]. This is in line with using more stringent remission criteria, such as the ACR/EULAR Boolean definition, which does not require definition of “deep” remission, since, as also seen here, it already reflects deep remission.
Conclusions
The results of this study add to the published evidence that some patients can successfully decrease the dose or discontinue bDMARD therapy [8,9,10,11,12,13,14,15,16]. In certain cases, this may be desirable for the purposes of decreasing the risk of adverse events and/or reducing costs. Although the most appropriate patients and dose reduction strategy remain unclear, this study found that sustained deep remission, normal ESR, SJC = 0, and TJC = 0 at the end of period 1 were significant predictors of maintaining DAS28 remission after etanercept dose reduction or discontinuation. Additionally, our results suggest that clinicians should consider using a stringent definition of disease control, such as sustained deep remission according to DAS28, or sustained remission according to CDAI/SDAI or ACR/EULAR Boolean criteria. Controlled clinical studies evaluating the endpoints of sustained and/or deep remission are needed.
Availability of data and materials
Upon request, and subject to certain criteria, conditions, and exceptions (see https://www.pfizer.com/science/clinical-trials/trial-data-and-results for more information), Pfizer will provide access to individual de-identified participant data from Pfizer-sponsored global interventional clinical studies conducted for medicines, vaccines, and medical devices (1) for indications that have been approved in the USA and/or EU or (2) in programs that have been terminated (i.e., development for all indications has been discontinued). Pfizer will also consider requests for the protocol, data dictionary, and statistical analysis plan. Data may be requested from Pfizer trials 24 months after study completion. The de-identified participant data will be made available to researchers whose proposals meet the research criteria and other conditions, and for which an exception does not apply, via a secure portal. To gain access, data requestors must enter into a data access agreement with Pfizer.
Abbreviations
- ACR:
-
American College of Rheumatology
- APLAR:
-
Asia Pacific League of Associations for Rheumatology
- bDMARD:
-
Biologic disease-modifying antirheumatic drug
- BMI:
-
Body mass index
- CDAI:
-
Clinical Disease Activity Index
- CMH:
-
Cochran-Mantel-Haenszel
- CRP:
-
C-reactive protein
- csDMARD:
-
Conventional synthetic DMARD
- DAS28:
-
Disease Activity Score 28-joint count
- ESR:
-
Erythrocyte sedimentation rate
- ETN:
-
Etanercept
- EULAR:
-
European League Against Rheumatism
- HAQ:
-
Health Assessment Questionnaire
- IL:
-
Interleukin
- JAK:
-
Janus kinase
- LDA:
-
Low disease activity
- MTX:
-
Methotrexate
- PBO:
-
Placebo
- PGA:
-
Physician global assessment
- QW:
-
Weekly
- RA:
-
Rheumatoid arthritis
- SDAI:
-
Simplified Disease Activity Index
- SJC:
-
Swollen joint count
- T2T:
-
Treat-to-Target
- TJC:
-
Tender joint count
- TNF:
-
Tumor necrosis factor
- ULN:
-
Upper limit of normal
References
Smolen JS, Landewé R, Bijlsma J, Burmester G, Chatzidionysiou K, Dougados M, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Ann Rheum Dis. 2017;76(6):960–77.
Lau CS, Chia F, Harrison A, Hsieh T-Y, Jain R, Jung SM, et al. APLAR rheumatoid arthritis treatment recommendations. Int J Rheum Dis. 2015;18(7):685–713.
Singh JA, Saag KG, Bridges SL, Akl EA, Bannuru RR, Sullivan MC, et al. 2015 American College of Rheumatology Guideline for the treatment of rheumatoid arthritis. Arthritis Rheumatol. 2016;68(1):1–26.
Smolen JS, Breedveld FC, Burmester GR, Bykerk V, Dougados M, Emery P, et al. Treating rheumatoid arthritis to target: 2014 update of the recommendations of an international task force. Ann Rheum Dis. 2016;75:3–15.
van Nies JAB, Tsonaka R, Gaujoux-Viala C, Fautrel B, van der Helm-van Mil AHM. Evaluating relationships between symptom duration and persistence of rheumatoid arthritis: does a window of opportunity exist? Results on the Leiden early arthritis clinic and ESPOIR cohorts. Ann Rheum Dis. 2015;74:806–12.
Barnabe C, Thanh NX, Ohinmaa A, Homik J, Barr SG, Martin L, et al. Healthcare service utilisation costs are reduced when rheumatoid arthritis patients achieve sustained remission. Ann Rheum Dis. 2013;72(10):1664–8.
Radner H, Smolen JS, Aletaha D. Remission in rheumatoid arthritis: benefit over low disease activity in patient-reported outcomes and costs. Arthritis Res Ther. 2014;16(1):R56.
Schett G, Emery P, Tanaka Y, Burmester G, Pisetsky DS, Naredo E, et al. Tapering biologic and conventional DMARD therapy in rheumatoid arthritis: current evidence and future directions. Ann Rheum Dis. 2016;75(8):1428–37.
Kuijper TM, Lamers-Karnebeek FBG, Jacobs JWG, Hazes JMW, Luime JJ. Flare rate in patients with rheumatoid arthritis in low disease activity or remission when tapering or stopping synthetic or biologic DMARD: a systematic review. J Rheumatol. 2015;42(11):2012–22.
Tanaka Y, Hirata S, Saleem B, Emery P. Discontinuation of biologics in patients with rheumatoid arthritis. Clin Exp Rheumatol. 2013;31(4 Suppl 78):S22–S7.
van Herwaarden N, den Broeder AA, van der Maas A, Bijlsma JWJ, van Vollenhoven RF, van den Bemt BJF. Down-titration and discontinuation strategies of tumor necrosis factor-blocking agents for rheumatoid arthritis in patients with low disease activity. Cochrane Database Syst Rev. 2014;9:CD010455.
Yoshida K, Sung Y-K, Kavanaugh A, Bae S-C, Weinblatt ME, Kishimoto M, et al. Biologic discontinuations studies: a systematic review of methods. Ann Rheum Dis. 2014;73(3):595–9.
Edwards CJ, Fautrel B, Schulze-Koops H, Huizinga TWJ, Kruger K. Dosing down with biologic therapies: a systematic review and clinicians’ perspective. Rheumatology (Oxford). 2017;56(11):1847–56.
Tanaka Y. Intensive treatment and treatment holiday of TNF-inhibitors in rheumatoid arthritis. Curr Opin Rheumatol. 2012;24(3):319–26.
Chen D-Y, Lau CS, Elzorkany B, Hsu P-N, Praprotnik S, Vasilescu R, et al. Dosing down and then discontinuing biologic therapy in rheumatoid arthritis: a review of the literature. Int J Rheum Dis. 2018;21(2):362–72.
Lau CS, Gibofsky A, Damjanov N, Lula S, Marshall L, Jones H, et al. Down-titration of biologics for the treatment of rheumatoid arthritis: a systematic literature review. Rheumatol Int. 2017;37(11):1789–98.
Smolen JS, Nash P, Durez P, Hall S, Ilivanova E, Irazoque-Palazuelos F, et al. Maintenance, reduction, or withdrawal of etanercept after treatment with etanercept and methotrexate in patients with moderate rheumatoid arthritis (PRESERVE): a randomised controlled trial. Lancet. 2013;381(9870):918–29.
van der Maas A, Kievit W, van den Bemt BJF, van den Hoogen FHJ, van Riel PL, den Broeder AA. Down-titration and discontinuation of infliximab in rheumatoid arthritis patients with stable low disease activity and stable treatment: an observational cohort study. Ann Rheum Dis. 2012;71(11):1849–54.
Fautrel B, Pham T, Alfaiate T, Gandjbakhch F, Foltz V, Morel J, et al. Step-down strategy of spacing TNF-blocker injections for established rheumatoid arthritis in remission: results of the multicentre non-inferiority randomised open-label controlled trial (STRASS: spacing of TNF-blocker injections in rheumatoid ArthritiS study). Ann Rheum Dis. 2016;75(1):59–67.
Haschka J, Englbrecht M, Hueber AJ, Manger B, Kleyer A, Reiser M, et al. Relapse rates in patients with rheumatoid arthritis in stable remission tapering or stopping antirheumatic therapy: interim results from the prospective randomised controlled RETRO study. Ann Rheum Dis. 2016;75(1):45–51.
Borrás-Blasco J, Gracia-Pérez A, Rosique-Robles JD, Casterá ME, Abad FJ. Clinical and economic impact of the use of etanercept 25 mg once weekly in rheumatoid arthritis, psoriatic arthropathy and ankylosing spondylitis patients. Expert Opin Biol Ther. 2014;14(2):145–50.
den Broeder AA, van Herwaarden N, van der Maas A, van den Hoogen FHJ, Bijlsma JW, van Vollenhoven RF, et al. Dose REduction strategy of subcutaneous TNF inhibitors in rheumatoid arthritis: design of a pragmatic randomised non inferiority trial, the DRESS study. BMC Musculoskelet Disord. 2013;14:299.
van Herwaarden N, van der Maas A, Minten MJM, van den Hoogen FHJ, Kievit W, van Vollenhoven RF, et al. Disease activity guided dose reduction and withdrawal of adalimumab or etanercept compared with usual care in rheumatoid arthritis: open label, randomised controlled, non-inferiority trial. BMJ. 2015;350:h1389.
Mariette X, Rouanet S, Sibilia J, Combe B, Le Loët X, Tebib J, et al. Evaluation of low-dose rituximab for the retreatment of patients with active rheumatoid arthritis: a non-inferiority randomised controlled trial. Ann Rheum Dis. 2014;73(8):1508–14.
Smolen JS, Emery P, Ferraccioli GF, Samborski W, Berenbaum F, Davies OR, et al. Certolizumab pegol in rheumatoid arthritis patients with low to moderate activity: the CERTAIN double-blind, randomised, placebo-controlled trial. Ann Rheum Dis. 2015;74(5):843–50.
Emery P, Burmester GR, Naredo E, Zhou Y, Hojnik M, Conaghan PG. Design of a phase IV randomised, double-blind, placebo-controlled trial assessing the ImPact of residual inflammation detected via imaging TEchniques, drug levels and patient characteristics on the outcome of dose TaperIng of adalimumab in clinical remission rheumatoid ArThritis (RA) patients (PREDICTRA). BMJ Open. 2018;8(2):e019007.
Smolen JS, Szumski A, Koenig AS, Jones TV, Marshall L. Predictors of remission with etanercept-methotrexate induction therapy and loss of remission with etanercept maintenance, reduction, or withdrawal in moderately active rheumatoid arthritis: results of the PRESERVE trial. Arthritis Res Ther. 2018;20(1):8.
Bechman K, Sin FE, Ibrahim F, Norton S, Matcham F, Scott DL, et al. Mental health, fatigue and function are associated with increased risk of disease flare following TNF inhibitor tapering in patients with rheumatoid arthritis: an exploratory analysis of data from the optimizing TNF tapering in RA (OPTTIRA) trial. RMD Open. 2018;4(1):e000676.
Tanaka Y, Takeuchi T, Mimori T, Saito K, Nawata M, Kameda H, et al. Discontinuation of infliximab after attaining low disease activity in patients with rheumatoid arthritis: RRR (remission induction by Remicade in RA) study. Ann Rheum Dis. 2010;69(7):1286–91.
Tanaka Y, Hirata S, Kubo S, Fukuyo S, Hanami K, Sawamukai N, et al. Discontinuation of adalimumab after achieving remission in patients with established rheumatoid arthritis: 1-year outcome of the HONOR study. Ann Rheum Dis. 2015;74(2):389–95.
Makinen H, Kautiainen H, Hannonen P, Sokka T. Is DAS28 an appropriate tool to assess remission in rheumatoid arthritis? Ann Rheum Dis. 2005;64(10):1410–3.
Schoels M, Alasti F, Smolen JS, Aletaha D. Evaluation of newly proposed remission cut-points for disease activity score in 28 joints (DAS28) in rheumatoid arthritis patients upon IL-6 pathway inhibition. Arthritis Res Ther. 2017;19:155.
Smolen JS, Aletaha D, Gruben D, Zwillich SH, Krishnaswami S, Mebus C. Brief report: remission rates with Tofacitinib treatment in rheumatoid arthritis: a comparison of various remission criteria. Arthritis Rheumatol. 2017;69(4):728–34.
Smolen JS, Collaud Basset S, Boers M, Breedveld F, Edwards CJ, Kvien TK, et al. Clinical trials of new drugs for the treatment of rheumatoid arthritis: focus on early disease. Ann Rheum Dis. 2016;75(7):1268–71.
Fleischmann R, van der Heijde D, Koenig AS, Pedersen R, Szumski A, Marshall L, et al. How much does disease activity score in 28 joints ESR and CRP calculations underestimate disease activity compared with the simplified disease activity index? Ann Rheum Dis. 2015;74(6):1132–7.
Pavelka K, Akkoç N, Al-Maini M, Zerbini CAF, Karateev DE, Nasonov EL, et al. Maintenance of remission with combination etanercept–DMARD therapy versus DMARDs alone in active rheumatoid arthritis: results of an international treat-to-target study conducted in regions with limited biologic access. Rheumatol Int. 2017;37(9):1469–79.
Emery P, Hammoudeh M, FitzGerald O, Combe B, Martin-Mola E, Buch MH, et al. Sustained remission with etanercept tapering in early rheumatoid arthritis. N Engl J Med. 2014;371(19):1781–92.
Anderson JK, Zimmerman L, Caplan L, Michaud K. Measures of rheumatoid arthritis disease activity: Patient (PtGA) and Provider (PrGA) Global Assessment of Disease Activity, Disease Activity Score (DAS) and Disease Activity Score With 28-Joint Counts (DAS28), Simplified Disease Activity Index (SDAI), Clinical Disease Activity Index (CDAI), Patient Activity Score (PAS) and Patient Activity Score-II (PASII), Routine Assessment of Patient Index Data (RAPID), Rheumatoid Arthritis Disease Activity Index (RADAI) and Rheumatoid Arthritis Disease Activity Index-5 (RADAI-5), Chronic Arthritis Systemic Index (CASI), Patient-Based Disease Activity Score With ESR (PDAS1) and Patient-Based Disease Activity Score Without ESR (PDAS2), and Mean Overall Index for Rheumatoid Arthritis (MOI-RA). Arthritis Care Res. 2011;63(S11):S14–36.
Bykerk VP, Massarotti EM. The new ACR/EULAR remission criteria: rationale for developing new criteria for remission. Rheumatology. 2012;51(Suppl 6):vi16–20.
Smolen JS, Aletaha D. Scores for all seasons: SDAI and CDAI. Clin Exp Rheumatol. 2014;32(Suppl 85):S75–S9.
Pincus T, Callahan L. Rheumatology function tests: grip strength, walking time, button test and questionnaires document and predict longterm morbidity and mortality in rheumatoid arthritis. J Rheumatol. 1992;19(7):1051–7.
Boot CRL, de Wind A, van Vilsteren M, van der Beek AJ, van Schaardenburg D, Anema JR. One-year predictors of presenteeism in workers with rheumatoid arthritis: disease-related factors and characteristics of general health and work. J Rheumatol. 2018;45(6):766–70.
Böhler C, Radner H, Ernst M, Binder A, Stamm T, Aletaha D, et al. Rheumatoid arthritis and falls: the influence of disease activity. Rheumatology. 2012;51(11):2051–7.
Radner H, Alasti F, Smolen JS, Aletaha D. Physical function continues to improve when clinical remission is sustained in rheumatoid arthritis patients. Arthritis Res Ther. 2015;17(1):203.
Lee K, Choi S, Xu H, Kang J, Park D, Lee S. HAQ score is an independent predictor of sustained remission in patients with rheumatoid arthritis. Rheumatol Int. 2017;37(12):2027–34.
Brown AK, Quinn MA, Karim Z, Conaghan PG, Peterfy CG, Hensor E, et al. Presence of significant synovitis in rheumatoid arthritis patients with disease-modifying antirheumatic drug–induced clinical remission: evidence from an imaging study may explain structural progression. Arthritis Rheum. 2006;54(12):3761–73.
Hazes JM, Luime JJ, Kuijper TM, van der Ven M, Weel AE, Gerards AH, et al. No clear association between ultrasound remission and health status in rheumatoid arthritis patients in clinical remission. Rheumatology. 2017;56(8):1276–81.
Ozgocmen S, Ozdemir H, Kiris A, Bozgeyik Z, Ardicoglu O. Clinical evaluation and power Doppler sonography in rheumatoid arthritis: evidence for ongoing synovial inflammation in clinical remission. South Med J. 2008;101(3):240–5.
Peluso G, Michelutti A, Bosello S, Gremese E, Tolusso B, Ferraccioli G. Clinical and ultrasonographic remission determines different chances of relapse in early and long standing rheumatoid arthritis. Ann Rheum Dis. 2011;70(1):172–5.
Saleem B, Brown AK, Keen H, Nizam S, Freeston J, Karim Z, et al. Disease remission state in patients treated with the combination of tumor necrosis factor blockade and methotrexate or with disease-modifying antirheumatic drugs: a clinical and imaging comparative study. Arthritis Rheum. 2009;60(7):1915–22.
Geng Y, Han J, Deng X, Zhang Z. Deep clinical remission: an optimised target in the management of rheumatoid arthritis? Experience from an ultrasonography study. Clin Exp Rheumatol. 2016;34:281–6.
Acknowledgements
We thank all patients who participated in this study as well as the investigators and medical staff at all of the participating centers. This study was funded by Pfizer. Medical writing support was provided by Jennica Lewis of Engage Scientific Solutions and was funded by Pfizer. The specific ethical bodies that approved the PRESERVE study are as follows: Australia—Bellberry Limited, Dulwich, SA; Flinders Clinical Research Ethics Committee, Repatriation General Hospital, Daw Park, SA; The Austin Health Human Research Ethics Committee, Heidelberg, VIC. Austria—Ethikkommission der Stadt Wien, Wien. Belgium—Comite d’ethique Hospitalo-Facultaire Universitaire de Liege, Centre Hospitalier Universitaire du Sart Tilman, Liege; CHU Liege, Comité d’Ethique de la Faculté de Médicine, Centre Hospitalier Universitaire du Sart Tilman, Liege. Chile—Comite Etico Cientifico, Servicio de Salud Metropolitano Oriente, Santiago, RM. Colombia—Comite de etica de la fundacion instituto de reumatologia Fernando Chalem, Bogota, Cundinamarca; Comité de etica independiente centro de reumatologia y ortopedia, Barranquilla, Atlantico; Comite de Etica de la Investigacion Riesgo de Fractura S.A., Bogota, Cundinamarca. Czech Republic—Eticka komise Fakultni nemocnice Olomouc a Lekarske fakulty, Univerzity Palackeho, Olomouc; Ethics Committee of Institute of Rheumatology, Praha; Eticka komise pro multicentricka klinicka hodnoceni Fakultni nemocnice v Motole, Praha; Multicentricka eticka komise Fakultni nemocnice u sv. Anny v Brne - detasovane pracoviste, Brno. France—Comité de Protection des Personnes, Sud-Ouest et Outre-Mer II Hôpital Purpan, Toulouse Cedex 9. Germany—Ethik-Kommission bei der Medizinischen Fakultaet der Universitaet Wuerzburg, Institut fuer Pharmakologie und Toxikologie, Wuerzburg. Hungary—Egeszsegugyi Tudomanyos Tanacs Klinikai Farmakologiai Etikai Bizottsaga, Budapest. Italy—Comitato Etico Scientifico dell’Azienda Ospedaliera Ospedale Niguarda Ca′ Granda di Milano, Milano; Comitato Etico Azienda Ospedaliera Universitaria San Luigi Gonzaga di Orbassano, Orbassano; Comitato Etico dell’Universita’ Campus Bio-Medico di Roma, Roma; Comitato Etico dell’Azienda Ospedali Vittorio Emanuele, Ferrarotto, S. Bambino, Catania. Republic of Korea—Institutional Review Board, Gangnam Severance Hospital, Seoul; Institutional Review Board/Ethics Commitee of Kangdong Sacred Heart Hospital, Seoul; Hallym University Sacred Heart Hospital Institutional Review Board, Anyang-Si, Gyeonggi-do; Institutional Review Board for Human Research, Konkuk University Hospital, Seoul; Institutional Review Board, Gachon Gil Medical Center, Incheon; Hanyang University Hospital IRB, Seoul; IRB of Eulji University Hospital, Daejeon. Mexico—Comite de Etica de la Facultad de Medidna de la UANL Hospital Universitario Dr. Jose Eleuterio Gonzalez, Monterrey NL; Comite Bioetico para la Investigacion Clinica S. C., Puebla 422, Mexico, DF; Comite de Etica del Hospital San Javier, Guadalajara, Jalisco; Comité de Investigación del Hospital CEM, Merida, Yucatán. The Netherlands—Independent Review Board Nijmegen (IRBN) Nijmegen, Wijchen. Poland—Komisja Etyczna Przy Instytucie Reumatologicznym ul Spartanska 1, Warszawa. Russian Federation—Biomedical Ethics Committee at FGU “Severo-Zapadny District Medical Center of Rozdrav,” St. Petersburg; Ethical council under responsibility of department of state regulation of circulation of medicines, Ministry of Public Health and Social Development of Russian Federation, Moscow; Local Ethics Committee at GU Institute of Rheumatology of RAMS, Moscow; Local Ethics Committee at GUZ “City Clinical Hospital #1 n.a., N.I.Pirogov,” Rheumatology Department, Moscow; Local Ethics Committee at GUZ at Leningrad Regional Clinical Hospital, St. Petersburg; Local Ethics Committee at Moscow Regional Research Clinical Institute, n.a. M.F. Vladimirskogo, Moscow. Serbia and Montenegro—Ethics Committee of Institute of Rheumatology-Belgrade, Belgrade; Ethics Committee of Institute for Treatment and Rehabilitation “Niska Banja,” Niska Banja; Ethics Committee Military Medical Academy, Belgrade. Spain—Hospital General Universitario Gregorio Marañon, Comite etico de Investigacion Clinica c/ Doctor, Madrid. Sweden—Regionala etikprovningsnamnden i Uppsala, Uppsala. Taiwan—Institutional Review Board of Tri-Service General Hospital National Defense Medical Center, Neihu, Taipei; Kaohsiung Medical University Chung-Ho Memorial Hospital, Institutional Review Board, Kaohsiung. UK—Liverpool Adult Research Ethics Committee, Research Ethics Office, Liverpool; Wrightington, Wigan and Leigh LREC, Greater Manchester Strategic Health Authority, Manchester; West Midlands Research Ethics Committee, Redditch, Worcestershire.
The specific ethical bodies that approved the PRIZE study are as follows: France—CPP Sud Méditerranée IV Hôpital Saint Eloi, Montpellier; Germany—Ethik-Kommission der Medizinischen Fakultaet der Ludwig-Maximilians Universitaet, Muenchen; Ireland—Ethics and Medical Research Committee, St. Vincent’s Healthcare Group Education Research Centre, Elm Park, Dublin; Italy—Comitato Etico dell’Azienda Ospedaliera Maggiore della Carita’ di Novara, Corso Mazzini, 18, Novara; Comitato per la Sperimentazione Clinica dei Medicinali dell’Azienda, Ospedaliero Universitaria Pisana, Via Roma, 67, Pisa; Comitato di Bioetica Fondazione, IRCCS Policlinico San Matteo, Viale Golgi, 19, Pavia; Comitato etico Ospedale Civile di Legnano, Via Candiani, 2 Legnano; Comitato di Bioetica Azienda Ospedaliera Universitaria Policlinico, Paolo Giaccone, Via del Vespro, 129, Palermo; Monaco—Comité Consultatif d’Ethique en Matière de Recherche Biomedicale Direction de l’action sanitaire et sociale, “Le Puccini,” 48 Bd d’Italie; Netherlands—Amsterdam Medical Centre Medical Ethics Committee (METC), Meibergdreef 9,NL-1105 AZ, Amsterdam; Poland—Komisja Bioetyczna przy Akademii Medycznej we Wroclawiu ul. Pasteura 1, Wroclaw, 50-367; Qatar—Research Committee Hamad Medical City Corporation, 3050, Doha; Romania—Ministerul Sanatatii Comisia, Nationala de Etica pentru Studiul, Clinic al Medicamentului, Str Av Sanatescu nr 48, Bucuresti, sector 1 011478; Russian Federation—Ethics Committee Affiliated with the Federal Services on Surveillance in Healthcare and Social Development, Building 2, No. 8 Petrovskiy Boulevard, Moscow, 127051; Local Ethics Committee at Institution of RAMs Scientific-Research, Institute of Rheumatology, Department of Clinical Trials, 34A, Kashirskoe shosse, Moscow, 115522; Central Ethics Committee at Federal service for supervision of public health and social development 8, build 2, Petrovskiy boulevard, Moscow, 127051; Local Ethics Committee at Federal state institution North-West District Medical Center of Roszdrav 13-15, Kadetskaya linia VO, Saint-Petersburg, 199004; Ethics Council at the Ministry of Healthcare and Social Development of Russian Federation 3, Rakhmanovskij per. Moscow, 127994; Local Ethics committee at the Yaroslavl Regional clinical Hospital, Yakovlevskaya str. 7, Yaroslavl, 150062; Local Ethics Committee at State Educational Institution of Additional Professional Education, Saint-Petersburg Medical Academy of Postgraduate Education of Roszdrav 41, Kirochnaya ul., Saint-Petersburg, 191015; Spain—Hospital Universitario La Paz, COMITE ETICO DE INVESTIGACION CLINICA, CEIC AREA 5, C/ PASEO DE LA CASTELLANA, 261, MADRID; Sweden—Regionala etikprovningsnamnden i, Stockholm; Switzerland—Ethikkommission des Kantons St. Gallen, Prof. Dr. Ulrico Schmid, Flurhof 7, Büro 014, St. Gallen; Kantonale Ethik-Kommission (KEK), lic. Iur. et theol. Niklaus Herzog, Sonneggstrasse 12, Zuerich; Commission d’Ethique de la Recherche Clinique, de la Faculté de Biologie et de Médecine, Faculté de Médecine, Sécretariat central, Rue du Bugnon 21, Lausanne; UK—Yorkshire and the Humber - Leeds West, Yorkshire and the Humber REC, Centre Office, First Floor, Millside, Mill Pond Lane, Leeds.
The specific ethical bodies that approved the T2T study are as follows: Brazil—Comitê de Ética em Pesquisa do Hospital Universitário; Comitê de Ética em Pesquisa do Hospital Heliópolis; Comitê de Ética em Pesquisa do Hospital Alberto Rassi; Comitê de Ética em Pesquisa; China—Shanghai Changhai Hospital Ethics Committee; Ethics Committee of Guangdong General Hospital; Ethics Committee of Peking Union Medical College Hospital; Ethics Committee of Guanghua Hospital of Intergrated Traditional Chinese and Western Medicine; Colombia—Comité de Ética de la Investigación Riesgo de Fractura; Comité de Investigaciones y Etica en Investigaciones; Comité de Etica en Investigacion en el area de la salud; Czech Republic—Eticka komise Krajska nemocnice T. Bati; Eticka komise Fakultni nemocnice Olomouc a Lekarske; Etická komise pro multicentrické klinické hodnocení; Eticka komise Revmatologickeho ustavu; Egypt—Ain Shams University, Faculty of Medicine Research Ethics Committee, El Azhar University; Faculty of Medicine Ethics Committee, Alexandria University; Hungary—Egészségügyi Tudományos Tanács Klinikai Farmakológiai Etikai Bizottsága; Jordan—Jordan Univ of Science & Tech King Abdullah University Hospital; Lebanon—American University of Beirut Medical Center Institutional Review Board; Malaysia—Medical Research & Ethics Committee, Ministry of Health Malaysia; Medical Ethics Committee, University Malaya Medical Centre; Mexico—Comité de Ética en Investigación Av. Venustiano Grranza No. 2395, Colonia Universitaria; Comité Bioético para la investigación Clínica SC - Centro de Investigación y Atención Integral de Durango AC; Comité Bioético para la investigación Clínica SC - Centro de Alta Especialidad en Reumatología e Investigación del Potosi S.C.; Comite de Etica en Investigacion del Grupo Calydes SCP - Unidad Reumatologica Las Americas S.C.P. del Centro Medico de Las Americas; Philippines—De La Salle Health Sciences Institute Independent Ethics Committee; University of the Philippines Manila Research Ethics Board; Institutional Review Board Angeles University Foundation; Institutional Review Board - Chong Hua Hospital; Institutional Ethics Review Committee St. Luke’s Medical Center; Qatar—Hamad Medical Corporation Medical Research Center; Romania—Comisia Naţională de Bioetică a Medicamentului şi a Dispozitivelor Medicale; Russian Federation—Ethics Council under the Ministry of Health of the Russian Federation; Ethics Committee of GBOU VPO “Krasnoyarsk State Medical University named after professor V.F. Voyno- Yasenetskiy of Ministry of Health of Russian Federation;” Local Ethics Committee at the LLC Institute of Medical Trials, Pharma-Ethics; Taiwan—Taipei Medical University, Joint Institutional Review; The Institutional Review Board, China Medical University Hospital; Institutional Review Board of the Cathay General Hospital; Research Ethics Committee of Buddhist Tzu Chi General Hospital; Thailand—Research Ethics Committee 2, Faculty of Medicine, Chiang Mai University; Office of Human Research Ethics Committee, Faculty of Medicine, Prince of Songkla University; The Khon Kaen University Ethics Committee for Human Research; Siriraj Institutional Review Board Faculty of Medicine; Ukraine—Komisiia z pytan etyky KU “Odeska oblasna klinichna likarnia;” Komisiia z pytan etyky Vinnytskoi oblasnoi klinichnoi likarni im. M.I. Pyrohova; Komisiia z pytan etyky pry Ternopilskii universytetskii likarni; Komisiia z pytan etyky pry Kyivskii oblasnii klinichnii likarni; Komisiia z pytan etyky pry Krymskii respublikanskii ustanovi “Universytetska klinika;” United Arab Emirates—Al Qassimi Clinical Research Center, Research Ethics Committee, Al Qassimi Hospital, Sharjah.
Funding
These studies were funded by Pfizer. Editorial/medical writing support was provided by Jennica Lewis, PharmD, CMPP, of Engage Scientific Solutions, and was funded by Pfizer.
Author information
Authors and Affiliations
Contributions
YT, JSS, HJ, AS, LM, and PE made substantial contributions to the conception or design of the study. YT, JSS, HJ, AS, LM, and PE made substantial contributions to the acquisition, analysis, and interpretation of data from the study. AS conducted the statistical analyses. YT, JSS, HJ, AS, LM, and PE contributed to writing the manuscript and revising it critically for important intellectual content. All authors read and approved the final manuscript, and all authors agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
These studies were conducted in accordance with the International Conference on Harmonization guidelines for Good Clinical Practice and the ethical principles of the Declaration of Helsinki. Written informed consent was obtained from all patients prior to enrollment. The institutional review board or independent ethics committee at each participating center reviewed and approved all consent forms and the study protocol.
Consent for publication
Not applicable.
Competing interests
YT has received speaking fees and/or honoraria from Daiichi-Sankyo, Astellas, Eli Lilly, Chugai, Sanofi, AbbVie, Pfizer, YL Biologics, Bristol-Myers, GlaxoSmithKline, UCB, Mitsubishi-Tanabe, Novartis, Eisai, Takeda, Janssen, and Asahi-kasei and has received research grants from Mitsubishi-Tanabe, Bristol-Myers, Eisai, Chugai, Takeda, AbbVie, Astellas, Daiichi-Sankyo, Ono, MSD, and Taisho-Toyama. JSS has received research grant support from Abbott, BMS, MSD, Pfizer, Roche, and UCB and consultation and/or speaking honoraria from Abbott, Astra-Zeneca, BMS, Celgene, Celltrion, Glaxo, Janssen, MSD, Pfizer, Roche, Samsung, Sanofi-Aventis, and UCB. HJ and LM were employees of Pfizer at the time the manuscript was written. AS is an employee of Syneos Health and was contracted by Pfizer to provide statistical support for the development of this paper. PE has received grant/research support and consultancy fees from AbbVie, BMS, Lilly, MSD, Novartis, Pfizer, Roche, Samsung, Sandoz, and UCB.
No nonfinancial competing interest exists for any author.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Table S1. Demographic and baseline disease characteristics according to CDAI response in period 1; Table S2. Proportion of patients achieving each ACR/EULAR Boolean criteria response at the end of period 1; Figure S1. Proportion of patients with a normal HAQ score at the end of period 1 according to achievement of period 1 sustained DAS28 deep remission (yes/no). (PDF 283 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tanaka, Y., Smolen, J.S., Jones, H. et al. The effect of deep or sustained remission on maintenance of remission after dose reduction or withdrawal of etanercept in patients with rheumatoid arthritis. Arthritis Res Ther 21, 164 (2019). https://doi.org/10.1186/s13075-019-1937-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13075-019-1937-4