Abstract
Background
Namilumab (AMG203), an immunoglobulin G1 monoclonal antibody that binds with high affinity to granulocyte-macrophage colony-stimulating factor (GM-CSF), was evaluated in a phase II randomized, double-blind, placebo-controlled study to investigate the efficacy and safety in patients with rheumatoid arthritis (RA) with an inadequate response to methotrexate (MTX-IR) or anti-tumour necrosis factor therapy (TNF-IR).
Methods
Subcutaneous namilumab (20, 80, or 150 mg) or placebo was administered at baseline and weeks 2, 6, and 10 in patients on stable background methotrexate therapy who were with MTX-IR or TNF-IR. Primary endpoint was mean change from baseline in the 28-joint Disease Activity Score, C-reactive protein version (DAS28-CRP) at week 12 comparing each of the three doses of namilumab to placebo. Safety and tolerability were assessed by adverse events (AEs) and pulmonary parameters. Results were analysed using the per-protocol population.
Results
One hundred eight patients from Europe and Japan (48.4 ± 12.02 years old; 77.8% female; mean DAS28-CRP 5.60–5.79; rheumatoid factor/anti-citrullinated protein antibodies + 75%) were randomized to placebo or namilumab 20, 80, or 150 mg (n = 27, 28, 25, and 28, respectively). Ninety-two were MTX-IR; 16 were TNF-IR. At week 12, a statistically significant difference in DAS28-CRP (p = 0.005) was seen for namilumab 150 mg versus placebo and separation was seen as early as week 2 for namilumab 150 mg (p < 0.05), with higher ACR50 and response rates versus placebo at week 12. A dose-response effect was observed across the DAS28-CRP endpoint with separation versus placebo evident from week 2. The most common treatment-emergent AEs were nasopharyngitis (18.5%, 17.9%, 4.0%, 14.3%), dyspnoea (0.0%, 3.6%, 8.0%, 10.7%), bronchitis (7.4%, 3.6%, 4.0%, 3.6%), and headache (3.7%, 3.6%, 12.0%, 0.0%) for placebo and 20, 80, or 150 mg of namilumab, respectively. No serious infections were observed. One serious AE (myocardial infarction) was observed with 150 mg of namilumab. There was no apparent dose relationship for AEs. A biomarker-based disease activity score showed a dose-dependent decrease at week 12.
Conclusions
This phase II study demonstrates the benefit of inhibiting macrophage activity targeting the GM-CSF for RA. The study met its primary endpoint with a clear dose-response effect. An acceptable tolerability profile was demonstrated over the 12-week study.
Trial registration
ClinicalTrials.gov, NEXUS; NCT02379091, submitted November 28, 2014
Similar content being viewed by others
Introduction
Despite many treatments introduced for rheumatoid arthritis (RA), significant proportions of patients do not have their disease adequately controlled and thus are unable to achieve treatment goals [1,2,3]. There is a continuing need for the exploration and development of therapeutic strategies with novel mechanisms of action.
Granulocyte-macrophage colony-stimulating factor (GM-CSF) is a haematopoietic growth factor produced by a number of different cell types, including T cells, macrophages, mast cells, endothelial cells, smooth muscle cells, epithelial cells, and fibroblasts [4,5,6,7,8,9]. In patients with RA, GM-CSF is aberrantly overproduced [10,11,12,13]; GM-CSF levels are moderately elevated in the plasma and highly elevated in the synovial fluid [13, 14], particularly in the pannus at sites of cartilage erosion [15]. The contribution of GM-CSF to the development of RA has also been documented in various in vitro and in vivo mouse models [16,17,18,19,20,21,22]. Clinical proof of concept for GM-CSF–targeted therapy has been demonstrated in patients with RA for antibodies targeting the GM-CSF receptor (mavrilimumab) [23,24,25,26] and targeting soluble GM-CSF (MOR103) [27].
Namilumab (AMG203) is a human immunoglobulin G1 monoclonal antibody that binds with high affinity to the GM-CSF ligand, potently neutralizing GM-CSF [28]. Preclinical data showed that a surrogate mouse antibody of namilumab (22E9) neutralized GM-CSF, suppressed inflammation, and protected cartilage in an arthritis mouse model [29]. In a first-in-humans study, healthy volunteers showed that single doses of namilumab (up to 8.0 mg/kg) were generally well tolerated (Takeda; data on file). Subsequently, a phase Ib (PRIORA; clinicaltrials.gov ID No. NCT01317797), first-in-patient, multicentre, randomized, double-blind, placebo-controlled, dose-escalation study showed that subcutaneous namilumab was generally well tolerated and demonstrated preliminary evidence of efficacy, although patient numbers were small [30].
Here, we report the formal clinical proof-of-concept, dose-finding phase II global clinical trial in Europe and Asia of namilumab in patients with RA with either an inadequate response to background methotrexate (MTX-IR) or an inadequate response to an anti-tumour necrosis factor (TNF) biologic therapy (TNF-IR).
Methods
Patients
This study included patients with a diagnosis of adult-onset RA, defined by the 2010 American College of Rheumatology (ACR)/European League Against Rheumatism (EULAR) classification, who were being treated with stable doses of methotrexate of between 15 and 25 mg/week (between 6 and 16 mg/week in Japan) for at least 12 weeks prior to baseline (day 1), along with folic acid, and who had at least moderate disease activity (Disease Activity Score 28 [DAS28] ≥ 3.2), at least four swollen joints, and a visual analogue scale pain score > 40 mm. Concomitant nonsteroidal anti-inflammatory drugs with appropriate gastroprotection, low-dose corticosteroids (≤ 10-mg prednisone equivalence per day), and hydroxychloroquine (≤ 400 mg/day) or chloroquine (≤ 250 mg/day) were permitted at stable doses for at least 4 weeks before the first dose of the study drug. The MTX-IR population had been inadequately controlled by prior therapy comprising MTX alone or MTX in combination with other nonbiologic, disease-modifying antirheumatic drugs. The TNF-IR population had been inadequately controlled despite prior therapy with 1 TNF inhibitor. Subjects in this population had shown an inadequate response (insufficient initial response or loss of response after at least 12 weeks of treatment, and/or intolerance to a TNF inhibitor and/or due to safety, with the exception of the occurrence of serious adverse events).
Exclusion criteria included a history of or any current symptomatic or uncontrolled lung disease, active infection, or risk of infection or inflammatory joint disease other than RA or other systemic autoimmune disorders.
Study design
Patients were randomized using an Interactive Web Response System in a 1:1:1:1 ratio and received either 20-, 80-, or 150-mg subcutaneous doses of namilumab or placebo at baseline, week 2, week 6, and week 10. The study was stopped at 12 weeks. Doses and administration frequency were based on phase Ia and phase Ib data and pharmacokinetic-pharmacodynamic modelling [30].
Institutional review boards or ethics committees at the participating investigational centres approved the study, which was conducted according to the principles set out in the Declaration of Helsinki, International Conference on Harmonisation Guidelines for Good Clinical Practice, and additional local regulations. The study was registered on clinicaltrials.gov as NEXUS (NCT02379091; registered March 4, 2015).
Efficacy assessments
Efficacy assessments were performed at screening, baseline, week 2, week 6, week 10, and week 12. The primary endpoint was the mean change from baseline in DAS28-CRP (28-joint Disease Activity Score, C-reactive protein [CRP] version) at week 12 comparing each of the three dose levels of namilumab to placebo. This endpoint was analysed and controlled (balanced) for strata combined (TNF-IR and MTX-IR). Secondary endpoints included the proportion of subjects with an ACR20/50/70 response (≥ 20% improvement, ≥ 50% improvement, or ≥ 70% improvement in ACR score) at week 12 and change from baseline in DAS28-CRP at weeks 2 and 6. Additional endpoints included the proportion of patients achieving remission according to DAS28 (DAS28-CRP ≤ 2.6), improvements to the Health Assessment Questionnaire Disability Index (HAQ-DI) score, and change from baseline in quality of life as assessed by SF-36 v2 scales [31].
Safety and tolerability assessments
Respiratory monitoring (chest radiograph, forced expiratory volume [FEV1], forced vital capacity [FVC], and MRC [Medical Research Council] breathlessness scale) was performed at screening and baseline and throughout the study because of the theoretical risk of developing pulmonary alveolar proteinosis when using therapeutic antibodies that target GM-CSF [32]. The protocol mandated referral to a pulmonologist for > 12% deterioration in FEV1 or FVC or for deterioration by > 5% decrease in oxygen saturation (SpO2) or an increase in MRC breathlessness scale score of 2 from baseline. These changes had to be reported as adverse events (AEs). Serum surfactant D (SP-D) and KL-6 (Krebs von den Lungen-6) levels, both established biomarkers for lung damage, were also measured. Other safety assessments included the incidence of AEs and serious AEs and routine laboratory testing.
Pharmacodynamics
Pharmacodynamic assessments were performed of peripheral blood cytokines and other markers of inflammation, including disease activity (such as the multibiomarker disease activity [MBDA] Vectra DAscore [Crescendo Biosciences, South San Francisco, CA, USA] [33]) and structural damage biomarkers (such as C1M, a marker of tissue damage associated with structural disease progression [34] [Nordic Biosciences; Herlev, Denmark]).
Statistical analyses
The following analysis sets were used for analysis and presentation of the study data: (1) all-patients-randomized set, consisting of all randomized subjects; (2) all-patients-treated set, consisting of all subjects in the all-patients-randomized set who took at least 1 dose of double-blind investigational medicinal product (IMP); (3) full analysis set (FAS), consisting of all subjects in the all-patients-treated set who had at least 1 valid post-baseline assessment of DAS28-CRP in the double-blind period up to week 12; and (4) per-protocol set (PPS), consisting of all subjects in the FAS who received a complete set of doses of IMP who completed their week 12 assessments and who did not have any major protocol violations that could have affected the efficacy assessment, such as patient populations who did not fulfil the protocol in terms of eligibility, interventions, and outcome assessment with a potential effect on efficacy (e.g. those who had used prohibited concomitant medications or those who were not on a stable background dose of methotrexate or corticosteroids).
Sample size calculations were based on the primary endpoint with the study powered for change in DAS28-CRP at 12 weeks. The total sample size of the study was expected to be approximately 100 (~ 25 subjects per arm). The study was designed as a proof-of-concept study to support dose finding but was not formally powered for dose-finding testing.
The treatment effect was implicitly assumed to be a 0.8 difference between placebo and test drug for improvement in DAS28-CRP for all active doses. According to Mandema et al. [35], a plot of the response against the dose reaches an upper plateau even at small doses for many biologic agents within RA, and an assumption of similar treatment effects for different doses therefore seems reasonable. The SD was assumed to be 1.15 [36]. The primary analysis was conducted using a detailed mixed-effect model repeated-measurement model. The test was the least squares (LS) means of the contrast between each of the active treatments and placebo.
For illustrative purposes, with these assumptions (difference from placebo = 0.80; SD of change from baseline = 1.15), 25 subjects per arm would provide 70% power to detect the treatment difference of 0.80 between active treatment group and placebo using a type I error level of 0.05 (two-sided, e.g. with no multiplicity adjustment).
Results
Patients
From a total of 171 patients screened, 108 were randomized between February 2015 and February 2016 in the study at 28 investigational sites in 7 countries (Bulgaria, Czech Republic, Poland, Russia, Spain, UK, and Japan). Of these, 88 were included in the PPS; 97 completed the 12-week period.
Patient demographics and baseline clinical characteristics are shown in Tables 1 and 2, respectively. The number of patients randomized per cohort was 27, 28, 25, and 28 for placebo and namilumab 20, 80, and 150 mg, respectively (2 patients were subsequently excluded from the FAS because of data integrity, which left 26, 28, 24, and 28 patients, respectively). For the PPS, the number of patients randomized per cohort was 20, 24, 23, and 21 for placebo and namilumab 20, 80, and 150 mg, respectively. The treatment groups were generally balanced in terms of baseline and disease characteristics (Table 2). There was a slightly higher proportion of male subjects taking 80 mg of namilumab and a lower proportion taking placebo compared with namilumab 20 and 150 mg, and there was a higher proportion of subjects taking corticosteroids in the 20-mg group compared with the other arms. Finally, there was a higher HAQ-DI score with placebo compared with the active treatment arm, and there was a higher mean CRP with placebo and with 150 mg of namilumab than with the other two study arms.
Most of the patients completed the week 12 treatment, with only 7 withdrawing early (2 receiving placebo and 3, 2, and 1 receiving namilumab 20, 80, and 150 mg, respectively). Three of these early withdrawals were because of AEs (Fig. 1).
Efficacy
DAS28-CRP scores were similar at baseline for subjects receiving placebo and those receiving namilumab (Table 2). Treatment with namilumab was associated with a clinically significant reduction in disease activity and ACR scores. At week 12, a statistically significant difference in DAS28-CRP score was seen for all doses of namilumab versus placebo both for the per-protocol analysis (p = 0.022) and the full analysis set (p = 0.015) (Fig. 2). The mean change from baseline in DAS28-CRP score at week 12 was statistically significantly different for namilumab 150 mg compared with placebo in the FAS population (p = 0.010). Results of the PPS analyses were consistent with the FAS analyses (p = 0.005 for namilumab 150 mg vs placebo). A significant separation versus placebo for this parameter was seen as early as week 2, after only 1 dose of namilumab 150 mg (p = 0.021) and thereafter at week 6 (p = 0.037) and at week 10 (p = 0.018). A dose-dependent response was observed over the namilumab dose range tested (Fig. 3). There was improvement in disease activity in all namilumab treatment groups, with a mean reduction from baseline to week 12 in DAS28-CRP scores versus placebo as follows: − 1.63, − 1.47, and − 1.80 for namilumab 20, 80, and 150 mg, respectively, versus − 0.99 for placebo. At week 12, the LS mean change in DAS28-CRP score from baseline was − 1.38, − 1.36, and − 1.69 for the namilumab treatment groups (20, 80, and 150 mg, respectively) versus 0.77 for placebo, which indicates improvement in disease activity, corresponding to a difference from placebo of − 0.61, − 0.59, and − 0.92 for namilumab 20, 80, and 150 mg, respectively. DAS28 changes from baseline were also analysed for MTX-IR and the TNF-IR patients, separately. The same changes were observed with MTX-IR patients (Additional file 1: Figure S1). For the TNF-IR patients, we observed a separation between placebo and 20-mg and 150-mg doses of namilumab (Additional file 2: Figure S2). However, this separation was not evident with the 80-mg dose, and this is likely due to the small sample size of the TNF-IR patients in this study, especially the sample size for the 80-mg dose cohorts (n = 3).
Analysis of change from baseline in DAS28-CRP score. Change from baseline in DAS28-CRP score by visit for the a per-protocol set [p < 0.05 are shown by asterisk; week 12, p = 0.022] and b full analysis set [p < 0.05 are shown by asterisk; week 6, p = 0.026; week 10, p = 0.031; week 12, p = 0.015]. DAS28-CRP 28-joint Disease Activity Score, C-reactive protein version
DAS28-CRP-adjusted mean change from baseline (per-protocol set). Significant p values compared to placebo are shown (p < 0.05 as one asterisk and p < 0.01 as two asterisks) [150 mg at week 2, p = 0.021; at week 6, p = 0.037; at week 10, p = 0.018; and at week 12, p = 0.005]. DAS28-CRP, 28-joint Disease Activity Score, C-reactive protein version; PBO placebo
For the secondary endpoints of ACR categorical responses (ACR20/50/70) and DAS28-CRP remission, higher doses of namilumab showed better efficacy than placebo (Figs. 4 and 5). For the PPS, the incidence of DAS28-CRP remission (≤ 2.6) was significantly greater for the namilumab 150-mg group (26.9%) versus placebo (9%) at week 12 (p = 0.048). Results of the PPS were consistent with the FAS at all post-baseline visits (full analysis set (FAS) for ACR is shown in Additional file 3: Figure S3, and FAS for DAS28-CRP remission at 12 weeks is shown in Additional file 4: Figure S4).
ACR20, ACR50, and ACR70 at week 12 (per-protocol set). Significant p values compared to placebo are shown by an asterisk (ACR20 for 20 mg, p = 0.031, and ACR50 for 150 mg, p = 0.049). ACR American College of Rheumatology, ACR20 ≥ 20% improvement, ACR50 ≥ 50% improvement, ACR70 ≥ 70% improvement, PBO placebo
Percentage of ACR20/50/70 and DAS28-CRP remission (≤ 2.6) by study visit (PPS). ACR, American College of Rheumatology; ACR20, ≥ 20% improvement; ACR50, ≥ 50% improvement; ACR70, ≥ 70% improvement; DAS28-CRP, 28-joint Disease Activity Score, C-reactive protein version; PBO, placebo; PPS, per-protocol set. p value of less than 0.05 is shown by an asterisk
At week 12, the proportion of subjects with ≥ 40% reduction in pain was 44.0%, 39.1%, and 30.8% for namilumab 20, 80, and 150 mg, respectively, versus 20.0% for placebo, but it did not reach statistical significance (p values namilumab versus placebo were 0.075, 0.151, and 0.381 for 20 mg, 80 mg, and 150 mg, respectively). At week 12, the LS mean change from baseline was − 8.55 for placebo, − 14.55 for 20 mg namilumab, − 13.6 for 80 mg, and − 13.7 for 150 mg. However, again, this did not reach statistical significance (p values for namilumab versus placebo were 0.055, 0.083, and 0.072 for 20 mg, 80 mg, and 150 mg, respectively). At week 12, the LS mean change from baseline in SF-36 (36-Item Short-Form Health Survey) mental health score was 7.8, 5.2, and 14.4 for namilumab 20, 80, and 150 mg, respectively, versus 3.07 for placebo. A statistically significant difference was seen between namilumab 150 mg versus placebo (p = 0.019). The LS mean change from baseline in SF-36 vitality score was 12.8, 12.2, and 17.3 for namilumab (20, 80, and 150 mg, respectively) versus 6.5 for placebo. A statistically significant difference was seen between namilumab 150 mg versus placebo (p = 0.035). There were no statistically significant differences between any of the namilumab treatment groups versus placebo for any of the other health and physical summary scores from baseline to week 12.
At week 12, EULAR good/moderate response rates for namilumab 20, 80, and 150 mg were 76.0%, 68.2%, and 76.9%, respectively, versus 45.8% for placebo. This reached statistical significance for the namilumab 20- and 150-mg treatment groups versus placebo (p = 0.032 and p = 0.025, respectively).
As previously observed [30], there were dose-dependent increases in blood GM-CSF concentrations over the namilumab dose range investigated. There was no change in GM-CSF concentrations for placebo. In addition, no clear trends were associated with namilumab treatment with regard to change in anti-citrullinated protein antibodies and rheumatoid factor versus baseline at any of the applicable visits. With regard to change from baseline in biomarkers with the potential for early detection of pulmonary alveolar proteinosis (carcinoembryonic antigen, KL-6, and SP-D), there were no trends associated with namilumab treatment. Peripheral blood cell types known to demonstrate GM-CSF responsiveness (including monocytes and macrophages, natural killer cells, neutrophils, B cells, and T cells) were assessed using flow cytometry, subtyping, and activation markers. There were no notable changes from baseline of cell types known to demonstrate GM-CSF responsiveness at any of the applicable visits.
At baseline, the majority of subjects (96.0%; 95 of 106) had negative screening results for anti-drug antibodies (ADAs). Four subjects (4.0%) had positive ADA results, with 2 (50.0%) confirmed positive and 2 (50.0%) confirmed negative in the ADA confirmatory assay. At week 12, 3 subjects (2.3%; 3 of 106) had positive ADA screening results, of which 1 (33.3%) was confirmed positive and 2 (66.7%) were confirmed negative in the ADA confirmatory assay.
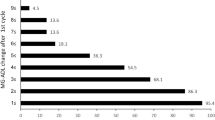
For the total MBDA score (Fig. 6), there were highly significant reductions in all namilumab treatment arms versus placebo from week 2. At week 12, the mean decrease in MBDA score was − 0.54 for the placebo cohort and − 8.50, − 7.81, and − 9.04 for the 20-mg, 80-mg, and 150-mg cohorts, with p values of 0.035, 0.036, and 0.008 for the 20-mg, 80-mg, and 150-mg cohorts compared to placebo, respectively. The number of patients for whom serum samples were analysed at each time point ranged from 22 to 27, 18 to 23, 22 to 25, and 18 to 26 for namilumab 150, 80, and 20 mg and placebo, respectively. In relation to the Nordic biomarkers, there was a significant difference in change in C1M from baseline between namilumab 150 mg and placebo (p value 0.0227; Fig. 7). Apart from MBDA and Nordic biomarkers, there were no notable changes in biomarker parameters during the study, and no clear trends were associated with namilumab treatment.
Safety
Over the 12-week study period, 14 of 27 subjects receiving placebo (51.9%; 25 events) and 45 of 81 receiving namilumab (55.6%; 84 events) experienced a treatment-emergent adverse event (TEAE; namilumab 20 mg, 42.8%; namilumab 80 mg, 68%; namilumab 150 mg, 57.1%). The most common TEAEs (Table 3) were nasopharyngitis (18.5%, 17.9%, 4.0%, 14.3%), dyspnoea (0.0%, 3.6%, 8.0%, 10.7%), bronchitis (7.4%, 3.6%, 4.0%, 3.6%), and headache (3.7%, 3.6%, 12.0%, 0.0%) for placebo and namilumab 20, 80, or 150 mg, respectively. Two mild AEs of urticaria developed in patients on the namilumab 20-mg arm. One AE of urticaria occurred after the first IMP injection in the abdomen: urticaria, dry mouth, and tachycardia. The patient fully recovered within 24 h without any treatment. The urticaria developed around the face and on the upper chest of the patient. The PI assessed the AE as related to the study medication and withdrew the patient from the study. The second AE of urticaria developed 2 days after the first dose and resolved 5 days later without any treatment. The study medication was maintained, and the AE did not reoccur. The PI assessed the AE as related to the study medication.
One serious TEAE was reported in the namilumab 150-mg arm in a 63-year-old Japanese man who experienced a myocardial infarction on day 83 after having received the fourth scheduled and his last dose of IMP. The patient was a smoker (11 to 20 pack-years). Medical history was otherwise unremarkable. The patient was withdrawn from the study and recovered after cardiac catheterization. One additional TEAE led to study discontinuation: 1 patient initially randomized to namilumab 20 mg experienced three different AEs, on day 1, moments after the first IMP injection in the abdomen: urticaria, dry mouth, and tachycardia. The patient fully recovered within 24 h without any treatment, and therefore, this AE was qualified as severe.
Treatment-emergent adverse events of special interest which could be suggestive of pulmonary alveolar proteinosis were reported in small numbers, and their low frequency (below 5%) excluded them from Table 3. These AEs were reviewed by the pulmonary panel and DSMB and were not deemed indicative of pulmonary alveolar proteinosis but considered to be reflective an alternative diagnosis.
Discussion
There is a growing body of evidence in support of the potential importance of the role of GM-CSF in the pathogenesis of RA. Moreover, rapid and sustained efficacy and normalization of acute-phase reactants have been consistently shown in studies targeting the GM-CSF pathway [37]. In a previous phase I study designed to assess the safety of repeated dosing in a small number of patients of subjects with RA, namilumab demonstrated preliminary evidence of efficacy [30]. This phase II trial is the first study statistically powered to evaluate the efficacy of different doses of namilumab versus placebo in a population with moderate to severe disease activity in RA. The findings show that namilumab, an investigational human monoclonal antibody targeting GM-CSF, improves the signs and symptoms of RA in such subjects. The study met its primary endpoint, and rapid and sustained improvement was demonstrated by DAS28-CRP, HAQ-DI, and ACR responses. Significant improvement was seen as early as week 2 for the highest dose (150 mg), and for all doses, scores continued to improve throughout the 12-week treatment. Of note, and a limitation of the present study, the observed placebo response rate was higher than assumed in the sample size. Despite this, the primary endpoint was met, and significant improvements were observed with namilumab over placebo. Another limitation of this phase II study was the relatively short time that subjects were exposed to the test biological. Nonetheless, although we only evaluated the effects of namilumab over 12 weeks, it was particularly encouraging that at the highest (150 mg) dose, 26.9% of subjects achieved DAS28-CRP < 2.6 (placebo 9.0%) and 42.9% showed an ACR50 response (placebo 15%). The number of subjects achieving DAS28-CRP < 2.6 or ACR50 and ACR70 responses was still rising at 12 weeks, which suggests that peak efficacy might not have been achieved. It has been shown previously that response to some biologic treatments continues to increase over the first 24 weeks of treatment, and a significant proportion of partial responders and nonresponders at week 12 can go on to achieve a clinical response with continued treatment [38]. For clinical practice, in future clinical trials, from the results of this study, 150-mg dose of namilumab should be used to offer maximum efficacy to patients, with acceptable safety. From a manufacturing point of view and tolerability for the patient as a subcutaneous injection, 150-mg dose is the maximum feasible dose at the current concentration of the antibody as the investigational product.
The safety profile was consistent with a previous phase I study of namilumab in subjects with RA [30]. Because of the link between GM-CSF and alveolar macrophage function and clearance of lung surfactant proteins, we performed intensive pulmonary lung function tests and assays for biomarkers of lung damage such as SP-D and KL-6. No meaningful differences were noted for SP-D and KL-6 between the active treatment and placebo groups. Furthermore, SP-D and KL-6 levels during the study were comparable to those described for healthy control subjects and RA patients with no interstitial lung disease [32]. No serious or opportunistic infections or severe hypersensitivity reactions were reported in this patient population during the observation period.
Conclusion
In conclusion, the results of this study showed that namilumab induced rapid and sustained clinically significant responses in subjects with RA over the period of the study, with a favourable risk-benefit profile. The results presented in this manuscript are in line with other anti-GM-CSF antibodies and confirm the validity of the target in RA [27, 37].
Abbreviations
- ACR:
-
American College of Rheumatology
- ADA:
-
Anti-drug antibody
- AE:
-
Adverse event
- CRP:
-
C-reactive protein
- DAS28-CRP:
-
28-joint Disease Activity Score, C-reactive protein version
- EULAR:
-
European League Against Rheumatism
- FAS:
-
Full analysis set
- GM-CSF:
-
Granulocyte-macrophage colony-stimulating factor
- HAQ-DI:
-
Health Assessment Questionnaire Disability Index
- KL-6:
-
Krebs von den Lungen-6
- LS:
-
Least squares
- MBDA:
-
Multibiomarker disease activity
- MTX:
-
Methotrexate therapy
- MTX-IR:
-
Inadequate response to methotrexate therapy
- PPS:
-
Per-protocol set
- RA:
-
Rheumatoid arthritis
- SF-36:
-
36-Item Short-Form Health Survey
- SP-D:
-
Serum surfactant D
- TEAE:
-
Treatment-emergent adverse event
- TNF:
-
Tumour necrosis factor
- TNF-IR:
-
Inadequate response or intolerance to an anti-tumour necrosis factor biologic therapy
References
Scott DL, Wolfe F, Huizinga TW. Rheumatoid arthritis. Lancet. 2010;376:1094–108.
Kievit W, Fransen J, Oerlemans AJ, Kuper HH, van der Laar MA, de Rooij DJ, et al. The efficacy of anti-TNF in rheumatoid arthritis, a comparison between randomised controlled trials and clinical practice. Ann Rheum Dis. 2007;66:1473–8.
Hetland ML, Christensen IJ, Tarp U, Dreyer L, Hansen A, Hansen IT, et al. Direct comparison of treatment responses, remission rates, and drug adherence in patients with rheumatoid arthritis treated with adalimumab, etanercept, or infliximab: results from eight years of surveillance of clinical practice in the nationwide Danish DANBIO registry. Arthritis Rheum. 2010;62:22–32.
Fleetwood AJ, Cook AD, Hamilton JA. Functions of granulocyte-macrophage colony-stimulating factor. Crit Rev Immunol. 2005;25:405–28.
Hamilton JA. Colony-stimulating factors in inflammation and autoimmunity. Nat Rev Immunol. 2008;8:533–44.
Griffin JD, Cannistra SA, Sullivan R, Demetri GD, Ernst TJ, Kanakura Y. The biology of GM-CSF: regulation of production and interaction with its receptor. Int J Cell Cloning. 1990;8(Suppl 1):35–44 (discussion 44-5).
Gasson JC. Molecular physiology of granulocyte-macrophage colony-stimulating factor. Blood. 1991;77:1131–45.
Hamilton JA. GM-CSF as a target in inflammatory/autoimmune disease: current evidence and future therapeutic potential. Expert Rev Clin Immunol. 2015;11:457–65.
Hamilton JA, Anderson GP. GM-CSF biology. Growth Factors. 2004;22:225–31.
Zvaifler NJ, Firestein GS. Cytokines in chronic inflammatory synovitis. Scand J Rheumatol. 1988;17:203–10.
Xu WD, Firestein GS, Taetle R, Kaushansky K, Zvaifler NJ. Cytokines in chronic inflammatory arthritis. II. Granulocyte-macrophage colony-stimulating factor in rheumatoid synovial effusions. J Clin Invest. 1989;83:876–82.
Alvaro-Gracia JM, Zvaifler NJ, Brown CB, Kaushansky K, Firestein GS. Cytokines in chronic inflammatory arthritis. VI. Analysis of the synovial cells involved in granulocyte-macrophage colony-stimulating factor production and gene expression in rheumatoid arthritis and its regulation by IL-1 and tumor necrosis factor-alpha. J Immunol. 1991;146:3365–71.
Fiehn C, Wermann M, Pezzutto A, Hufner M, Heilig B. Plasma GM-CSF concentrations in rheumatoid arthritis, systemic lupus erythematosus and spondyloarthropathy. Z Rheumatol. 1992;51:121–6.
Ulfgren AK, Lindblad S, Klareskog L, Andersson J, Andersson U. Detection of cytokine producing cells in the synovial membrane from patients with rheumatoid arthritis. Ann Rheum Dis. 1995;54:654–61.
Chu CQ, Field M, Allard S, Abney E, Feldmann M, Maini RN. Detection of cytokines at the cartilage/pannus junction in patients with rheumatoid arthritis: implications for the role of cytokines in cartilage destruction and repair. Br J Rheumatol. 1992;31:653–61.
Campbell IK, Rich MJ, Bischof RJ, Dunn AR, Grail D, Hamilton JA. Protection from collagen-induced arthritis in granulocyte-macrophage colony-stimulating factor-deficient mice. J Immunol. 1998;161:3639–44.
Cook AD, Braine EL, Campbell IK, Rich MJ, Hamilton JA. Blockade of collagen-induced arthritis post-onset by antibody to granulocyte-macrophage colony-stimulating factor (GM-CSF): requirement for GM-CSF in the effector phase of disease. Arthritis Res. 2001;3:293–8.
Hashimoto M, Hirota K, Yoshitomi H, Maeda S, Teradaira S, Akizuki S, et al. Complement drives Th17 cell differentiation and triggers autoimmune arthritis. J Exp Med. 2010;207:1135–43.
Cook AD, Turner AL, Braine EL, Pobjoy J, Lenzo JC, Hamilton JA. Regulation of systemic and local myeloid cell subpopulations by bone marrow cell-derived granulocyte-macrophage colony-stimulating factor in experimental inflammatory arthritis. Arthritis Rheum. 2011;63:2340–51.
Cook AD, Pobjoy J, Sarros S, Steidl S, Durr M, Lacey DC, et al. Granulocyte-macrophage colony-stimulating factor is a key mediator in inflammatory and arthritic pain. Ann Rheum Dis. 2013;72:265–70.
De Vries EGE, Willemse PHB, Biesma B, Stern AC, Limburg PC, Vellenga E. Flare-up of rheumatoid arthritis during GM-CSF treatment after chemotherapy. Lancet. 1991;338:517–8.
Hazenberg BP, Van Leeuwen MA, Van Rijswijk MH, Stern AC, Vellenga E. Correction of granulocytopenia in Felty’s syndrome by granulocyte-macrophage colony-stimulating factor. Simultaneous induction of interleukin-6 release and flare-up of the arthritis. Blood. 1989;74:2769–70.
Burmester GR, Feist E, Sleeman MA, Wang B, White B, Magrini F. Mavrilimumab, a human monoclonal antibody targeting GM-CSF receptor-alpha, in subjects with rheumatoid arthritis: a randomised, double-blind, placebo-controlled, phase I, first-in-human study. Ann Rheum Dis. 2011;70:1542–9.
Burmester GR, Weinblatt ME, McInnes IB, Porter D, Barbarash O, Vatutin M, et al. Efficacy and safety of mavrilimumab in subjects with rheumatoid arthritis. Ann Rheum Dis. 2013;72:1445–52.
Takeuchi T, Tanaka Y, Close D, Godwood A, Wu CY, Saurigny D. Efficacy and safety of mavrilimumab in Japanese subjects with rheumatoid arthritis: findings from a phase IIa study. Mod Rheumatol. 2015;25:21–30.
Burmester GR, McInnes IB, Kremer JM, Miranda P, Mariusz Korkosz JV, Rubbert-Roth A, et al. Efficacy and safety/tolerability of mavrilimumab, a human GM-CSF monoclonal antibody in patients with rheumatoid arthritis. Arthritis Rheum. 2014;66(abstract):2821.
Behrens F, Tak PP, Ostergaard M, Stoilov R, Wiland P, Huizinga TW, et al. MOR103, a human monoclonal antibody to granulocyte-macrophage colony-stimulating factor, in the treatment of patients with moderate rheumatoid arthritis: results of a phase Ib/IIa randomised, double-blind, placebo-controlled, dose-escalation trial. Ann Rheum Dis. 2015;74:1058–64.
Krinner EM, Raum T, Petsch S, Bruckmaier S, Schuster I, Petersen L, et al. A human monoclonal IgG1 potently neutralizing the pro-inflammatory cytokine GM-CSF. Mol Immunol. 2007;44:916–25.
Plater-Zyberk C, Joosten LA, Helsen MM, Hepp J, Baeuerle PA, van den Berg WB. GM-CSF neutralisation suppresses inflammation and protects cartilage in acute streptococcal cell wall arthritis of mice. Ann Rheum Dis. 2007;66:452–7.
Huizinga TW, Batalov A, Stoilov R, Lloyd E, Wagner T, Saurigny D, Souberbielle B, Esfandiari E. Phase 1b randomized, double-blind study of namilumab, an anti-granulocyte macrophage colony-stimulating factor monoclonal antibody, in mild-to-moderate rheumatoid arthritis. Arthritis Res Ther. 2017;19:53.
Ware JE, Kosinski M. Interpreting SF-36 summary health measures: a response. Qual Life Res. 2001;10:405–13.
Inoue Y, Trapnell BC, Tazawa R, et al. Characteristics of a large cohort of patients with autoimmune pulmonary alveolar proteinosis in Japan. Am J Respir Crit Care Med. 2008;177:752–62.
Curtis JR, van der Helm-van Mil AH, Knevel R, Huizinga TW, Haney DJ, Shen Y, et al. Validation of a novel multibiomarker test to assess rheumatoid arthritis disease activity. Arthritis Care Res (Hoboken). 2012;64:1794–803.
Siebuhr AS, Bay-Jensen AC, Leeming DJ, Plat A, Byrialsen I, Christiansen C, et al. Serological identification of fast progressors of structural damage with rheumatoid arthritis. Arthritis Res Ther. 2013;15:R86.
Mandema JW, Gibbs M, Boyd RA, Wada DR, Pfister M. Model-based meta-analysis for comparative efficacy and safety: application in drug development and beyond. Clin Pharmacol Ther. 2011;90:766–9.
Landewé RB, et al. Efficacy assessed in follow-ups of clinical studies: methodological conundrum. Arthritis Res Ther. 2010;12:132.
Burmester GR, McInnes IB, Kremer J, Miranda P, Korkosz M, Vencovsky J, et al; EARTH EXPLORER 1 Study Investigators. A randomised phase IIb study of mavrilimumab, a novel GM-CSF receptor alpha monoclonal antibody, in the treatment of rheumatoid arthritis. Ann Rheum Dis 2017;76:1020–1030.
Bathon JM, Martin RW, Fleishmann RM, Tesser JR, Schiff MH, Keystone EC, et al. A comparison of etanercept and methotrexate in patients with early rheumatoid arthritis. N Engl J Med. 2000;343:1586–93.
Acknowledgements
The authors would like to thank all patients who participated in the study. The authors also acknowledge the study investigators - Bulgaria: Drs Batalov, Goranov, Nestorova, Stoilov; Czech Republic: Dr. Augustinova, Dokoupilova, Vencovsky, Vitek; Japan: Dr. Hagiwara, Miyagawa, Nakamura, Okada, Sagawa, Sakata, Shono; Poland: Drs Stopinska, Jeka; Russia: Drs Chernykh, Galustyan, Matsievskaia, Myasoutova, Uspensliv, Vinogradova; Spain: Dr. Sanchez-Burson; UK: Drs Tahir, Roussou, as well as the physicians, study coordinators, and research staff involved in the conduct of the study. PCT would like to acknowledge support by the National Institute for Health Research (NIHR) Oxford Biomedical Research Centre (BRC) and by AR UK. Editorial support was provided by Caudex, UK and by Brian Shearer, Takeda and was funded by Takeda Pharmaceuticals.
Funding
This study was sponsored by Takeda Development Centre, UK, and Takeda Pharmaceutical Company Limited, Japan.
Availability of data and materials
All relevant data generated or analysed during this study are included in this published article.
Author information
Authors and Affiliations
Consortia
Contributions
PT was the principal investigator of the study, contributed to the protocol design and the conduct and analysis of the study as well as the writing of the manuscript. DS and BS were the clinical science and clinical medical leads of the study, respectively. They contributed to the protocol design and conduct and analysis of the study, as well as the writing of the manuscript. JV, ED, TN, and GM were principal investigators in their respective countries, recruited patients into the study, and commented on the manuscript. BH and TW were the statistician and the pharmacometrician of the study, respectively. They contributed to the design, analysis of the study, and the writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional review boards or ethics committees at the participating investigational centres approved the study, which was conducted according to the principles set out in the Declaration of Helsinki, International Conference on Harmonisation Guidelines for Good Clinical Practice, and additional local regulations.
Consent for publication
Not applicable.
Competing interests
Dr. Wagner was an employee of Takeda Pharmaceuticals International GmbH. Both Bernard Souberbielle and Didier Saurigny were employees of Takeda at the time of the study. Barbara Hunt is an employee of Takeda International, Deerfield, IL, USA. The other authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Figure S1. Analysis of change from baseline in DAS28-CRP score in MTX-IR patients 1a/ Graph of the mean change of DAS28 in the MTX-IR patients from baseline over the 12 weeks study duration period (DAS28-CRP = 28-joint Disease Activity Score) 1b/ table of the DAS-28 values corresponding to the graph. (DOCX 17 kb)
Additional file 2:
Figure S2. Analysis of change from baseline in DAS28-CRP score in TNF-IR patients 1a/ Graph of the mean change of DAS28 in the TNF-IR patients from baseline over the 12 weeks study duration period (DAS28-CRP = 28-joint Disease Activity Score) 1b/ table of the DAS-28 values corresponding to the graph. (DOCX 17 kb)
Additional file 3:
Figure S3. Data are shown for the full set analysis of outcomes for the ACR categorical responses at week 12. (DOCX 20 kb)
Additional file 4:
Figure S4. Data are shown for the full set analysis of DAS28-CRP remission criteria at week 12. (DOCX 80 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Taylor, P.C., Saurigny, D., Vencovsky, J. et al. Efficacy and safety of namilumab, a human monoclonal antibody against granulocyte-macrophage colony-stimulating factor (GM-CSF) ligand in patients with rheumatoid arthritis (RA) with either an inadequate response to background methotrexate therapy or an inadequate response or intolerance to an anti-TNF (tumour necrosis factor) biologic therapy: a randomized, controlled trial. Arthritis Res Ther 21, 101 (2019). https://doi.org/10.1186/s13075-019-1879-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13075-019-1879-x