Abstract
Background
Ultrasound is increasingly used to evaluate shoulder pain, but the benefits of this are unclear. In this study, we examined whether ultrasound-defined pathologies have implications for clinical outcomes.
Methods
We extracted reported pathologies from 3000 ultrasound scans of people with shoulder pain referred from primary care. In latent class analysis (LCA), we identified whether individual pathologies clustered in groups. Optimal group number was determined by the minimum Bayesian information criterion. A questionnaire was sent to all patients scanned over a 12-month period (n = 2322). Data collected included demographics, treatments received, current pain and function. The relationship between pathology-defined groups and clinical outcomes was examined.
Results
LCA revealed four groups: (1) bursitis with limited inflammation elsewhere (n = 1280), (2) bursitis with extensive inflammation (n = 595), (3) rotator cuff tears (n = 558) and (4) limited pathology (n = 567). A total of 777 subjects (33%) completed questionnaires. The median (IQR) duration post-ultrasound scan was 25 (22–29) months. Subsequent injections were most common in groups 1 and 2 (groups 1–4 76%, 67%, 48% and 61%, respectively); surgery was most common in group 3 (groups 1–4 23%, 21%, 28% and 16%, respectively). Shoulder Pain and Disability Index scores were highest in group 3 (median 48 and 30, respectively) and lowest in group 4 (median 32 and 9, respectively). Patients in group 4 who had surgery reported poor outcomes.
Conclusions
In a community-based population, we identified clusters of pathologies on the basis of ultrasound. Our retrospective data suggest that these groups have different treatment pathways and outcomes. This requires replication in a prospective study to determine the value of a pathology-based classification in people with shoulder pain.
Similar content being viewed by others
Background
Shoulder pain is common, with an estimated worldwide incidence of 0.9% to 2.5% and point prevalence of up to 26% [1]. Importantly for our ageing society, shoulder pain increases with age, with a prevalence of 21% in those over 70 years old [2]. In the United Kingdom, approximately 4% of adults consult their general practitioner (GP) about shoulder pain [3, 4]. Management remains challenging and often results in poor outcomes. Despite the short-term beneficial effects of community-based interventions, 50% of people continue to have pain at 18 months, though pain can also follow a remitting-relapsing course over time, making evaluation of treatment at single time points difficult [5, 6]. Shoulder pain has a significant impact on quality of life, and the economic burden has been estimated to be €689 per person annually [7, 8].
The clinical diagnosis of shoulder pathologies is difficult, and evidence suggests poor levels of reliability and reproducibility amongst clinicians when examining shoulder pain [9, 10]. Recent qualitative research has shown uncertainty amongst GPs in the diagnosis of patients with shoulder pain [11]. Diagnosis is complicated further by inconsistent nomenclature and classifications [12]; pathologies of the rotator cuff (RC) have been described by a variety of terms, including RC syndrome, shoulder impingement syndrome, subacromial bursitis and RC tendinitis.
Ultrasound offers accurate detection of pathology, and, in the context of the reported diagnostic uncertainty, it is unsurprising that its use is increasing. From 2001 to 2009 in Australia, there was a fourfold rise in shoulder ultrasound scans [13]. The number of primary care referrals for shoulder ultrasound scans in a U.K. regional centre tripled to 3000 between 2007 and 2015 (Leeds Teaching Hospitals NHS Trust, unpublished data). However, it is still unclear how information from ultrasound relates to treatment and long-term outcomes [14, 15]. The extent to which diagnostic tests on shoulder pain inform and affect patient management and outcomes has been highlighted previously in several systematic literature reviews as an area that needs to be investigated [13, 16].
Shoulder pain may have complex aetiologies, and pathologies often do not occur in isolation; some may respond to particular therapies better than others, which could complicate assessment of efficacy if they co-occur. Therefore, understanding patterns of shoulder pathology may help in targeting therapies more effectively. Given the uncertainty in clinical diagnosis, it seems reasonable to examine the potential of pathology-based diagnosis using ultrasound. If ultrasound cannot identify groups of patients who will achieve different outcomes, either in the current care pathway or in trials of targeted therapies, there would be limited justification for its continued use in this patient group. As a first step toward understanding the importance of a pathology-based classification, we aimed to determine whether distinct clusters of ultrasound-defined pathologies exist and whether there is any evidence that these have implications for long-term clinical outcomes.
Methods
Patients
Ultrasound reports were retrieved for consecutive primary care patients referred to a single centre’s radiology department (Chapel Allerton Hospital, Leeds, UK) for a scan of their shoulder. We included 3000 patients on the basis of estimated annual referrals and included scans between 2012 and 2013. Inclusion criteria were that patients be aged over 18 years, referred from primary care, referred for shoulder pain and attending for their first ultrasound scan. Patients were excluded if they had had previous surgery or had not been referred from primary care. These patients were identified by details on the referral card and electronic patient records.
In our centre, guidelines advise that patients be referred from primary care for an ultrasound scan if they have moderate-severe painful abduction, have not improved after physiotherapy or have suspected acromioclavicular joint (ACJ) pain. However, clinical experience of the broad range of presenting symptoms and signs raises questions about adherence to these recommendations and may further highlight discrepancies in clinical evaluation of shoulder pain.
Ultrasound scans
Data from a single shoulder per patient were utilised, and, where identifiable, the first symptomatic shoulder was included. Eligible patient records were examined to identify the first ultrasound scan for a selected shoulder (even if the first scan fell outside the collection dates). Scans were obtained by musculoskeletal radiologists and sonographers. Previous work has shown that inter-rater reliability for shoulder pathologies between two of the radiologists is substantial (all κ values >0.6) for full-thickness RC tear, calcification, impingement and tendon abnormalities [17]. The following features were documented as present or absent: bursitis, impingement, calcific tendinitis, ACJ degeneration, glenohumeral osteoarthritis, adhesive capsulitis, biceps tenosynovitis, RC tendinopathy and full or partial RC tear (see Additional file 1 for definitions). After discussion with the sonographers, impingement was assumed to be present if there was a full-thickness RC tear, even if impingement was not reported. Other pathologies were assumed to be absent if not reported. Other details recorded included age at time of scan, sex, whether an injection was given on the day of the scan, and (where available) duration of pain.
Questionnaire
A postal questionnaire was sent to all eligible patients scanned in 2013. A second wave of questionnaires was sent to those who had not replied after 4 weeks. Data collected included demographics; characteristics of pain; previous treatment; Shoulder Pain and Disability Index (SPADI), a validated self-administered questionnaire used to measure pain and disability in the shoulder in the past week [18–20]; EuroQol five dimensions scale (EQ-5D-5 L), a self-report measure used to define health status [21]; Marx shoulder activity scale [22]; and self-reported comorbidities. Returned questionnaires were matched to ultrasound findings.
Statistical analysis
Latent class analysis (LCA) was performed (see Additional file 1 for full details). LCA identifies clusters which group together people who share similar characteristics, in this case people who share a distinct pattern of shoulder pathology. The model calculates the probability of group membership for each person and assigns each individual to the group with the highest probability; the accuracy of the classification can be improved by including covariates such as age and sex. The classes we identified (hereafter groups) were then compared for age, sex, duration of pain (according to the initial scan record), injection (according to the initial scan record) and the presence of each pathology. To check for responder bias, these details were also compared between patients who completed the questionnaire and those who did not. Questionnaire responses were compared between the pathology groups using quantile, Poisson or binary logistic regression, according to the outcome type, adjusting for age and sex. Appropriate checks were made that the data satisfied the test assumptions. We used Stata version 13.1 software (StataCorp, College Station, TX, USA) for analysis.
Results
To identify 3000 eligible ultrasound scans, 3035 referral cards were reviewed. Reasons for exclusion included 6 scans technically difficult, 9 scan results inaccessible, 17 with soft tissue lumps examined and 3 with guided procedures without diagnostic scans.
Ultrasound pathologic findings
In the 3000 patients selected, the mean age was 54.6 years, and 52% were female (Table 1). For eight patients, impingement could not be assessed owing to difficulty in moving the patient’s arm; impingement status was set to ‘missing’ for these patients. The most common pathologies were subacromial impingement (69%) and bursitis (68%), followed by ACJ degeneration (40%), tendinopathy (36%), calcific tendonitis (12%), biceps tenosynovitis (7%), glenohumeral osteoarthritis (6%) and adhesive capsulitis (3%).
Latent class analysis
The LCA suggested four or five groups existed. (For full details, see Additional file 1: Tables S1–S3.) We retained the four-group solution. On the basis of patterns of pathology in each group, we interpreted that they represented bursitis with limited inflammation elsewhere (group 1), bursitis with extensive inflammation (group 2), RC tears (group 3) and limited pathology (group 4) (Table 2).
Group 1 was the largest (43%) (Table 2); the other three groups each represented approximately 20%. The groups were similar in gender balance or duration of pain prior to the first scan. Patients in group 4 were the youngest; 42% had no pathologies recorded, and a further 42% had just one pathology reported (Fig. 1). In group 4, mean age was similar to group 1; all patients in group 1 had bursitis, but few had tendinopathy or ACJ degeneration. In group 2, on average 20 years older than groups 1 and 4, almost all patients had bursitis, RC tendinopathy and ACJ degeneration, and one-fourth had biceps tenosynovitis. Patients in group 3 were the oldest on average; all had RC tears, which were full-thickness tears in the majority. Patients in this group had the highest rate of glenohumeral osteoarthritis, as might be expected for their age, but a smaller proportion in group 3 than in group 2 had ACJ degeneration. Nearly all patients in group 3 had impingement; however, comparatively few had bursitis compared with groups 1 and 2.
Patient questionnaire findings
A postal questionnaire was sent to all eligible patients scanned in 2013 (n = 2322). Of these patients, 777 completed questionnaires (33%), and we received replies from a further 233 (10%) who declined to participate. Responders and non-responders were similar in gender balance, age and ultrasound pathology findings (Table 1). Some respondents reported a diagnosis of rheumatoid arthritis (RA) (n = 87). Ultrasound findings did not show intra-articular synovitis in the RA-reporting group. Re-running the LCA in questionnaire respondents who did not report having RA (n = 690) resulted in very results similar to those of the full (n = 3000) LCA (see Additional file 1: Table S4 for details). We therefore retained the original pathology groupings; however, in the analyses of questionnaire outcomes, we excluded those reporting RA.
Questionnaires were completed by 30%, 36%, 34% and 25% of patients in groups 1–4, respectively. Older patients were more likely to respond; there were no differences in adjusted response rates between groups (probability of response in group 1 = 0.31 [0.28–0.34], group 2 = 0.33 [0.29–0.37], group 3 = 0.30 [0.26–0.35], group 4 = 0.28 [0.23–0.32]; chi-square = 3.04, p = 0.386).
Questionnaire results for all respondents are presented in Additional file 1: Table S5; 67% still experienced pain at a median (IQR) of 25 (22–29) months since their scan. Ultrasound findings by group (restricted to questionnaire respondents) are provided in Additional file 1: Table S6. Follow-up duration was similar in the four groups (Table 3). Between 63% (groups 1 and 2) and 77% (group 3) of patients reported persistent pain at follow-up.
The most commonly reported painful sites other than the target shoulder were lower back (36%), neck (33%), and knees either ipsilateral (27%) or contralateral (24%) to the target shoulder (Additional file 2: Figure S1). Adjusted estimates of the number of painful sites were highest in group 2 (mean 4.2) and lowest in group 4 (mean 3.0) (Table 4).
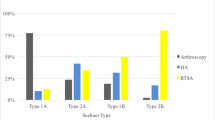
There was descriptive evidence that treatment differed according to presence of certain individual pathologies (Additional file 1: Table S7). There were clear differences in treatment at the group level for steroid injection (p < 0.001) and surgery (p = 0.015) (Table 4). Those in group 1 (bursitis with limited inflammation) were the most likely to have had steroid injection(s) (adjusted probability 76%), whereas those in group 3 (RC tears) were least likely (49%). Patients in group 3 were the most likely to have had surgery (35%); surgery was least likely in the limited pathology group (14%). In patients with bursitis, those in group 3 were less likely to have received a steroid injection at time of scan than those in groups 1 and 2 (estimated probability of injection [95% CI] group 1 = 0.48 [0.41, 0.54]; group 2 = 0.41 [0.33, 0.49]; group 3 = 0.20 [0.06, 0.33]; chi-square = 8.6, p = 0.014). Adjusted rates of physiotherapy did not differ between groups.
Groups differed in the severity of their reported symptoms. Group 3 (RC tears) was more likely to still have pain at follow-up (Table 4), and subjects in this group reported the highest levels of SPADI pain. A similar trend was seen for SPADI difficulty scores (Tables 3 and 4; Fig. 2). These trends were not explained by the higher rate of surgery in group 3; those who had surgery reported lower scores (adjusted difference in median total score [95% CI] −19 [−38, 0]; z-score = −1.98, p = 0.048). The differences in total SPADI by surgery were negligible for group 1 (−8 [−22, 5]; z-score = −1.23, p = 0.220) and group 2 (0 [−17, 17]; z-score = −0.04, p = 0.965). In contrast, in group 4, total SPADI was substantively higher in the patients who had surgery (25 [−1, 51]; z-score = 1.89, p = 0.059) (see Additional file 3: Figure S2).
Patients in group 4 who had surgery were more likely to report a diagnosis of depression than those who had not (adjusted probability [95% CI] 0.40 [0.15–0.66] vs. 0.09 [0.02–0.15]), whereas surgery was not associated with depression in the other groups (interaction effect for group × surgery chi-square = 9.4, p = 0.025). However, the nature of the association between symptoms, surgery and depression cannot be determined in this cross-sectional study. There were no substantive age- and sex-adjusted differences between the groups in shoulder activity level, EQ-5D index score, EQ-5D health VAS score, the number of comorbidities reported, or the odds of reporting difficulty standing from sitting (data not shown).
Discussion
This study has demonstrated, for the first time to our knowledge, clustering of ultrasound pathologies into four groups. These groups reported different treatments and to some extent had different age- and sex-adjusted outcomes at 2 years; however, owing to the low questionnaire completion rate, the longitudinal results need to be interpreted with caution.
Currently, there is limited evidence-based guidance on the role of imaging in the shoulder pain care pathway, and international guidance pre-dates the wide availability of ultrasound [23]. Though guidance for the diagnosis and management of many common painful musculoskeletal problems generally does not require imaging as part of routine care, the uncertainty in clinical evaluation, poor patient outcomes and increasing use of ultrasound support critical evaluation of the usefulness of a pathology-based classification. Researchers in a recent pragmatic randomised trial reported no evidence of difference in patient-perceived recovery between those with ultrasound-tailored treatment and usual-care groups [24]. Ultrasound-guided treatment was targeted at individual pathologies, and it would be interesting to see if outcomes would differ using our novel pathology-based classification.
The clinical validity of the pathology groups identified in this study require further evaluation in future studies. Conceivably, patients with just one pathology may respond differently to treatment compared with patients in whom the same pathology co-occurs with other pathologies. Although we did not attempt to examine the efficacy of different treatments, different patterns of treatment were reported. Group 1 was most likely to receive steroid injections. Steroid treatment may help with subacromial bursitis in the short term [25], which may explain the treatment in this group. Groups 1 and 2 may represent a spectrum; members of group 2 are older, and if we were to follow patients similar to those in group 1 over time, their patterns of shoulder pathology may eventually resemble those of group 2. Group 3 was the oldest group, confirming previous studies which have shown that RC tears increase with age [26]. Members of group 3 were less likely to receive steroid injections, even if they had concurrent bursitis, and they were more likely to undergo surgery. Steroid injections may impede tendon repair, and RC tears offer a surgical target, which may explain the variation in treatment. Group 3 also had the highest level of current pain and functional impairment. Surgical repair techniques of RC tears vary, and surgery has been shown to have conflicting results in improving outcomes in patients with shoulder pain [27–29]. Our data suggest that those who had surgery reported lower levels of pain and functional impairment. Group 4 was the youngest group, and a smaller proportion of these patients reported having surgery, because fewer had detectable pathologies present. Group 4 also had the lowest levels of pain and functional disability of all the groups.
Many (42%) in group 4 had no pathology; some of these patients may have improved at the time of their ultrasound scan. Another explanation is that other pathologies were present that ultrasound could not detect. Ultrasound is as sensitive and specific as magnetic resonance imaging (MRI) in detecting RC disorders [30], but further work is required to understand its sensitivity and specificity in detecting other pathologies, such as calcific tendinopathy. Furthermore, pathologies such as labral tears require MRI for identification [31, 32]. In addition, imaging-detected pathologies may not correlate with clinical findings. In the present study, 16% of patients without detectable pathology received steroid injections at the time of their scan; many reports documented that this was after discussion with the patient, and in some cases because clinical impingement was suspected even though this was not confirmed by the scan. A further explanation could be that the pain may be referred from other regions, such as the neck. The cause of chronic pain is multifactorial, and other features apart from imaging pathology play a role in characterising pain. Psychological factors such as fear avoidance, depression and poor quality of life can result in worse pain, function and perceived recovery outcomes [33, 34]. Ultrasound-detected pathologies have previously been reported in asymptomatic individuals, and further work is required to understand which factors result in the development and progression of symptoms in these individuals [14, 26, 27, 35].
Although we looked at associations between baseline pathologies and outcomes, the absence of baseline clinical data means we could not fully evaluate the predictive value of ultrasound. Previous attempts at identifying predictors of outcomes in people with shoulder pain have been made [36–40]. Pain characteristics such as worse baseline pain, duration of pain, concomitant psychological complaints, other concomitant musculoskeletal problems and repetitive shoulder action resulted in worse outcomes [37, 39–41]. Existing prognostic models to improve shoulder pain management have yet to be validated and assessed for clinical utility [39, 42]. There are very limited studies evaluating the prognostic role of ultrasound in shoulder pain: One suggested that the absence of subacromial bursa pathology may be a predictor of excellent outcomes at 3 weeks [36].
This study has a number of limitations. This study was undertaken in a single centre, though the sample size was large; the demographics of included patients seem similar to those of other large community cohorts [4, 43]. There was no control group, limiting our interpretation of pathologies and symptoms. Our local care pathway recommends that patients over the age of 65 years with shoulder pain undergo radiography of their shoulder, which may result in a channelling bias because patients with radiographic osteoarthritis may not undergo ultrasonography. In this study, local recommendations suggested that patients were referred for an ultrasound scan if they had moderate-severe pain and were not responding to physiotherapy, which could have led to selection bias in our cohort. However, it would seem that this group would likely be typical of patients with shoulder pain requiring investigation in potential future care pathways. Although the radiographers in this study followed a standardised method of performing ultrasonography of shoulders [44], standardised reporting of all pathologies was not routine, so if pathology was not documented, it was assumed absent. It is possible that some pathologies may not have been reported, especially if lesions that are considered more severe or clinically relevant are primarily reported. Group 3 had the highest level of glenohumeral osteoarthritis but a lower frequency of ACJ degeneration; the latter finding may be a result of non-standardised reporting, although it may also be an artefact introduced as a result of the groupings formed on the basis of LCA. A prospective study using standardised criteria for the different diagnostic labels is needed. This was a retrospective study, so we were unable to explore inter-reader reliability, especially in partial RC tears, where authors of a recent review showed that ultrasound has some difficulty in diagnosing this pathology [30]. Previous work has shown that, for most shoulder pathologies, the inter-rater reliability for two of the present sonographers was acceptable [17]. Impingement was assumed in all patients with complete RC tears. The patient questionnaire was retrospective, raising the possibility of recall bias. Only 33% completed the questionnaires; therefore, there is potential for selection bias. However, our work suggests that completers and non-completers were very similar in demographic characteristics and pathologic findings. Importantly, though we recorded symptoms around 2 years after an initial scan, we were unable to determine initial symptoms and subsequent changes. The prognostic value of a pathology-based classification needs to be established before consequent treatment pathways can be explored.
Conclusions
This study demonstrates, for the first time to our knowledge, that patients undergoing ultrasound scans for shoulder pain can be grouped according to pathologic patterns. Our data suggest that these groups may receive different treatment and have different outcomes. These preliminary data support further exploration of the potential benefits of a pathology-based classification for shoulder pain.
Abbreviations
- ACJ:
-
Acromioclavicular joint
- EQ-5D-5L:
-
EuroQol five dimensions scale
- GP:
-
General practitioner
- LCA:
-
Latent class analysis
- MRI:
-
Magnetic resonance imaging
- NIHR:
-
National Institute for Health Research
- OA:
-
Osteoarthritis
- RA:
-
Rheumatoid arthritis
- RC:
-
Rotator cuff
- SPADI:
-
Shoulder Pain and Disability Index
- US:
-
Ultrasound
- VAS:
-
Visual analogue scale
References
Luime JJ, Koes BW, Hendriksen IJ, Burdorf A, Verhagen AP, Miedema HS, et al. Prevalence and incidence of shoulder pain in the general population; a systematic review. Scand J Rheumatol. 2004;33(2):73–81.
Chard MD, Hazleman R, Hazleman BL, King RH, Reiss BB. Shoulder disorders in the elderly: a community survey. Arthritis Rheum. 1991;34(6):766–9.
Greving K, Dorrestijn O, Winters JC, Groenhof F, van der Meer K, Stevens M, et al. Incidence, prevalence, and consultation rates of shoulder complaints in general practice. Scand J Rheumatol. 2012;41(2):150–5.
Jordan KP, Kadam UT, Hayward R, Porcheret M, Young C, Croft P. Annual consultation prevalence of regional musculoskeletal problems in primary care: an observational study. BMC Musculoskelet Disord. 2010;11:144.
Croft P, Pope D, Silman A, Primary Care Rheumatology Society Shoulder Study Group. The clinical course of shoulder pain: prospective cohort study in primary care. BMJ. 1996;313(7057):601–2.
Murphy RJ, Carr AJ. Shoulder pain. BMJ Clin Evid. 2010;2010:1107.
Kuijpers T, van Tulder MW, van der Heijden GJ, Bouter LM, van der Windt DA. Costs of shoulder pain in primary care consulters: a prospective cohort study in The Netherlands. BMC Musculoskelet Disord. 2006;7:83.
Smith KL, Harryman 2nd DT, Antoniou J, Campbell B, Sidles JA, Matsen 3rd FA. A prospective, multipractice study of shoulder function and health status in patients with documented rotator cuff tears. J Shoulder Elbow Surg. 2000;9(5):395–402.
May S, Chance-Larsen K, Littlewood C, Lomas D, Saad M. Reliability of physical examination tests used in the assessment of patients with shoulder problems: a systematic review. Physiotherapy. 2010;96(3):179–90.
Bamji AN, Erhardt CC, Price TR, Williams PL. The painful shoulder: can consultants agree? Br J Rheumatol. 1996;35(11):1172–4.
Ottenheijm RP, Hesselmans NJ, Kemper A, Moser A, de Bie RA, Dinant GJ, et al. GPs’ perspectives on the diagnostic work-up in patients with shoulder pain: a qualitative study. J Eval Clin Pract. 2014;20(3):239–45.
Shanahan EM, Sladek R. Shoulder pain at the workplace. Best Pract Res Clin Rheumatol. 2011;25(1):59–68.
Dinnes J, Loveman E, McIntyre L, Waugh N. The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: a systematic review. Health Technol Assess. 2003;7(29):1–166.
Yamaguchi K, Tetro AM, Blam O, Evanoff BA, Teefey SA, Middleton WD. Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Shoulder Elbow Surg. 2001;10(3):199–203.
Schibany N, Zehetgruber H, Kainberger F, Kainberger F, Wurnig C, Ba-Ssalamah A, et al. Rotator cuff tears in asymptomatic individuals: a clinical and ultrasonographic screening study. Eur J Radiol. 2004;51(3):263–8.
Arthritis Research UK. Early diagnostic ultrasound for shoulder pain: effect on clinical decision-making and patient outcomes. October 2012
O’Connor PJ, Rankine J, Gibbon WW, Richardson A, Winter F, Miller JH. Interobserver variation in sonography of the painful shoulder. J Clin Ultrasound. 2005;33(2):53–6.
Roach KE, Budiman-Mak E, Songsiridej N, Lertratanakul Y. Development of a shoulder pain and disability index. Arthritis Care Res. 1991;4(4):143–9.
Heald SL, Riddle DL, Lamb RL. The shoulder pain and disability index: the construct validity and responsiveness of a region-specific disability measure. Phys Ther. 1997;77(10):1079–89.
Paul A, Lewis M, Shadforth MF, Croft PR, Van Der Windt DA, Hay EM. A comparison of four shoulder-specific questionnaires in primary care. Ann Rheum Dis. 2004;63(10):1293–9.
Brooks R. EuroQol: the current state of play. Health Policy. 1996;37(1):53–72.
Sangha O, Stucki G, Liang MH, Fossel AH, Katz JN. The Self-Administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 2003;49(2):156–63.
New Zealand Guidelines Group (NZGG). The diagnosis and management of soft tissue shoulder injuries and related disorders: best practice evidence-based guideline. Wellington, NZ: NZGG; 2004. http://www.acc.co.nz/PRD_EXT_CSMP/groups/external_communications/documents/guide/wcm001684.pdf. Accessed 22 Nov 2016.
Ottenheijm RPG, Cals JWL, Winkens B, Weijers RE, de Bie RA, Dinant GJ. Ultrasound imaging to tailor the treatment of acute shoulder pain: a randomised controlled trial in general practice. BMJ Open. 2016;6(11), e011048.
Crawshaw DP, Helliwell PS, Hensor EM, Hay EM, Aldous SJ, Conaghan PG. Exercise therapy after corticosteroid injection for moderate to severe shoulder pain: large pragmatic randomised trial. BMJ. 2010;340:c3037.
Moosmayer S, Tariq R, Stiris M, Smith HJ. The natural history of asymptomatic rotator cuff tears: a three-year follow-up of fifty cases. J Bone Joint Surg Am. 2013;95(14):1249–55.
Kuhn JE, Dunn WR, Sanders R, An Q, Baumgarten KM, Bishop JY, et al. Effectiveness of physical therapy in treating atraumatic full-thickness rotator cuff tears: a multicenter prospective cohort study. J Shoulder Elbow Surg. 2013;22(10):1371–9.
Slabaugh MA, Nho SJ, Grumet RC, Wilson JB, Seroyer ST, Frank RM, et al. Does the literature confirm superior clinical results in radiographically healed rotator cuffs after rotator cuff repair? Arthroscopy. 2010;26(3):393–403.
Carr AJ, Rees JL, Ramsay CR, Fitzpatrick R, Gray A, Moser J, et al. Protocol for the United Kingdom Rotator Cuff Study (UKUFF): a randomised controlled trial of open and arthroscopic rotator cuff repair. Bone Joint Res. 2014;3(5):155–60.
Roy JS, Braen C, Leblond J, Desmeules F, Dionne CE, MacDermid JC, et al. Diagnostic accuracy of ultrasonography, MRI and MR arthrography in the characterisation of rotator cuff disorders: a systematic review and meta-analysis. Br J Sports Med. 2015;49(20):1316–28.
Weber SC, Martin DF, Seiler 3rd JG, Harrast JJ. Superior labrum anterior and posterior lesions of the shoulder: incidence rates, complications, and outcomes as reported by American Board of Orthopedic Surgery Part II candidates. Am J Sports Med. 2012;40(7):1538–43.
Schwartzberg R, Reuss BL, Burkhart BG, Butterfield M, Wu JY, McLean KW. High prevalence of superior labral tears diagnosed by MRI in middle-aged patients with asymptomatic shoulders. Orthop J Sports Med. 2016;4(1):2325967115623212.
Bot SD, van der Waal JM, Terwee CB, van der Windt DA, Scholten RJ, Bouter LM, et al. Predictors of outcome in neck and shoulder symptoms: a cohort study in general practice. Spine (Phila Pa 1976). 2005;30(16):E459–70.
Roh YH, Lee BK, Noh JH, Oh JH, Gong HS, Baek GH. Effect of depressive symptoms on perceived disability in patients with chronic shoulder pain. Arch Orthop Trauma Surg. 2012;132(9):1251–7.
Unruh KP, Kuhn JE, Sanders R, An Q, Baumgarten KM, Bishop JY, et al. The duration of symptoms does not correlate with rotator cuff tear severity or other patient-related features: a cross-sectional study of patients with atraumatic, full-thickness rotator cuff tears. J Shoulder Elbow Surg. 2014;23(7):1052–8.
Laslett M, Steele M, Hing W, McNair P, Cadogan A. Shoulder pain in primary care – part 2: predictors of clinical outcome to 12 months. J Rehabil Med. 2015;47(1):66–71.
Feleus A, Bierma-Zeinstra SM, Miedema HS, Verhagen AP, Nauta AP, Burdorf A, et al. Prognostic indicators for non-recovery of non-traumatic complaints at arm, neck and shoulder in general practice – 6 months follow-up. Rheumatology (Oxford). 2007;46(1):169–76.
Chester R, Shepstone L, Lewis JS, Jerosch-Herold C. Predicting response to physiotherapy treatment for musculoskeletal shoulder pain: protocol for a longitudinal cohort study. BMC Musculoskelet Disord. 2013;14:192.
Kuijpers T, van der Windt DA, Boeke AJ, Twisk JW, Vergouwe Y, Bouter LM, et al. Clinical prediction rules for the prognosis of shoulder pain in general practice. Pain. 2006;120(3):276–85.
Bruls VE, Bastiaenen CH, de Bie RA. Prognostic factors of complaints of arm, neck, and/or shoulder: a systematic review of prospective cohort studies. Pain. 2015;156(5):765–88.
van der Windt DA, Koes BW, Boeke AJ, Deville W, De Jong BA, Bouter LM. Shoulder disorders in general practice: prognostic indicators of outcome. Br J Gen Pract. 1996;46(410):519–23.
Vergouw D, Heymans MW, de Vet HC, van der Windt DA, van der Horst HE. Prediction of persistent shoulder pain in general practice: comparing clinical consensus from a Delphi procedure with a statistical scoring system. BMC Fam Pract. 2011;12:63.
Linsell L, Dawson J, Zondervan K, Rose P, Randall T, Fitzpatrick R, et al. Prevalence and incidence of adults consulting for shoulder conditions in UK primary care; patterns of diagnosis and referral. Rheumatology (Oxford). 2006;45(2):215–21.
Martinoli C. Musculoskeletal ultrasound: technical guidelines. Insights Imaging. 2010;1(3):99–141.
Acknowledgements
We thank the National Institute for Health Research (NIHR) and Arthritis Research UK for financial support of this study.
Funding
This study was funded through an Arthritis Research UK Experimental Osteoarthritis Treatment Centre grant. PGC, EMAH, PO’C and SRK are partly supported by the NIHR through the Leeds Musculoskeletal Biomedical Research Unit. GT is supported by an NIHR doctoral research fellowship. This article presents independent research funded by the NIHR. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Availability of data and materials
The datasets are available from the corresponding author on reasonable request.
Authors’ contributions
GT and PGC made substantial contributions to the conception and design of the study, data acquisition, data interpretation, and the drafting and revision of the manuscript. EMAH made substantial contributions to the conception and design of the study, performed the statistical analysis and data interpretation, and helped to draft and revise the manuscript. AR made substantial contributions to data acquisition and interpretation and to the drafting of the manuscript. SRK made substantial contributions to the conception and design of the study and helped to draft and revise the manuscript. PO’C made substantial contributions to the conception and design of the study, data acquisition, and drafting and revision of the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
This study received ethics approval from the North East – Newcastle and North Tyneside 1 Research Ethics Committee (reference number 15/NE/0115). All participants gave informed consent before taking part in this study.
Author information
Authors and Affiliations
Corresponding author
Additional files
Additional file 1:
Supplementary materials, including ultrasound reporting definitions, LCA analysis and supplementary tables mentioned in the body of main text. (DOCX 33 kb)
Additional file 2: Figure S1.
Joint pain reported. (JPG 2553 kb)
Additional file 3: Figure S2.
Total SPADI by surgery. (JPG 2552 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tran, G., Hensor, E.M.A., Ray, A. et al. Ultrasound-detected pathologies cluster into groups with different clinical outcomes: data from 3000 community referrals for shoulder pain. Arthritis Res Ther 19, 30 (2017). https://doi.org/10.1186/s13075-017-1235-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13075-017-1235-y