Abstract
Background
Exercise is associated with major benefits in patients with rheumatic diseases for both cardiovascular and rheumatic status. However, information about exercise generally is not collected systematically in routine rheumatology care. A multidimensional health assessment questionnaire (MDHAQ), which was designed for busy clinical settings, includes a query about exercise status. We analyzed possible associations between change in MDHAQ exercise scores and other MDHAQ measures in patients with various rheumatic diseases over one year.
Methods
In one rheumatology clinical setting, all patients, regardless of diagnosis, complete an MDHAQ before seeing a rheumatologist. The MDHAQ includes scores for physical function, pain, and patient global estimate, compiled into an index, routine assessment of patient index data (RAPID3), as well as a self-report joint count and a query about exercise. Patients were classified into four groups according to their exercise status at baseline and one year later as: EXER-Yes (regular exercise), EXER-Yes; EXER-No (no regular exercise), EXER-Yes; EXER-Yes, EXER-No; and EXER-No, EXER-No. These groups were compared using the chi square and Kruskal-Wallis tests and analysis of variance (ANOVA).
Results
Patients who reported regular exercise at baseline were younger, had higher formal education, and better clinical status than other patients. The EXER-No, EXER-Yes group had greater improvement in other MDHAQ variables than patients in the other three groups. By contrast, the EXER-Yes, EXER-No group was the only group with poorer status one year later.
Conclusions
The MDHAQ exercise query indicates that regular exercise is associated with better clinical status. Patients in the EXER-No, EXER-Yes group reported the best clinical improvement, although it is not known whether exercise preceded or followed the improved clinical status.
Similar content being viewed by others
Background
The traditional approach to treatment of rheumatoid arthritis (RA) emphasized rest, and regular exercise was discouraged [1, 2]. However, over the last two decades exercise has been recognized as beneficial to people with RA and other rheumatic diseases, not only for cardiovascular and general fitness, but also for better rheumatologic clinical status [3–5]. Furthermore, the absence of exercise carries a similar risk for mortality 5 years later as the risk associated with smoking in a general elderly, non-diseased population [6].
Despite extensive evidence on the value of exercise in RA, most patients seen in rheumatology care do not participate in regular exercise. For example, in the QUEST RA database of 21 countries, regular exercise was reported by only 29 % of 5235 patients with RA, including more than 50 % in only 2 countries (Finland and Hungary), 21–50 % in 12 countries (Ireland, The Netherlands, Sweden, Lithuania, Greece, Denmark, USA, Germany, Canada, Estonia, and Serbia) and fewer than 20 % in 7 countries (Spain, Latvia, Poland, Turkey, France, Italy, and Argentina) [7].
The safety and effectiveness of exercise programs have been established primarily in structured research studies rather than in routine rheumatology care [3, 8–10]. In most busy clinical settings, data on exercise in individual patients generally are not collected systematically, if at all, and few data are available on levels of exercise. The capacity to collect information from patients on exercise in a pragmatic, feasible manner, without additional effort on the part of a rheumatologist, could advance the care and outcomes of patients with RA and other rheumatic diseases.
A multidimensional health assessment questionnaire (MDHAQ) is designed to be completed by patients in routine care [11]. The MDHAQ includes scores for physical function, pain and patient global estimate of status (PATGL) to provide a composite routine assessment of patient index data score of 0–30 (RAPID3) [12], as well as a query about exercise status.
Our objective was to analyze possible associations of demographic and clinical status variables with patient self-report exercise status at baseline and one year later in unselected patients with different rheumatic diseases seen in routine care.
Methods
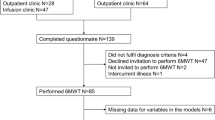
Patients
Since July 2005, all patients seen at the Seligman Center for Advanced Therapeutics at the NYU Hospital for Joint Diseases complete an MDHAQ at all visits, while waiting to see the rheumatologist, in the infrastructure of routine care. MDHAQ scores, laboratory tests, and medications are recorded in a database. A physician global estimate of status (DOCGL) also is collected in routine care. A primary diagnosis was assigned by the treating physician according to ICD-9 codes. Patients with available data on exercise status at baseline and one year later through April 2011 were included in the study. The Institutional Review Board (IRB) of New York University School of Medicine approved a retrospective chart review of the data; therefore, no specific consent was needed for this study.
Patient self-report MDHAQ
The MDHAQ is a two-page patient self-report questionnaire [13–15] developed for quantitative assessment in routine clinical care [16], which includes physical function in 10 activities, scored 0–3 (0 = without any difficulty, 1 = with some difficulty, 2 = with much difficulty, and 3 = unable to do) for a total physical function (FN) score of 0–30. The raw FN 0–30 score for the 10 activities is converted to 0–10 using a template on the MDHAQ, and added to two 0–10 visual analog scale (VAS) scores for pain and patient global estimate of status (PATGL), to provide a composite 0–30 RAPID3 score [12].
The MDHAQ also includes an RA disease activity index (RADAI) self-report joint count [17], which queries patients to score pain in 16 specific joint groups, 8 each on the right and left sides: fingers, wrists, elbows, shoulders, hips, knees, ankles, and toes. Scoring options are: 0 = none, 1 = mild, 2 = moderate, or 3 = severe pain; the total score range is 0–48 [17]. Queries about the back and neck in an identical format are added on the MDHAQ, but not included in scoring, to be comparable to RADAI scores elsewhere.
The MDHAQ also includes scores for anxiety, depression, and sleep quality, a 60-item symptom checklist, review of 12 recent medical history events, morning stiffness, fatigue VAS, change in status, demographic data, and a query about exercise [12, 13].
Self-report exercise status
The MDHAQ exercise query is: “How often do you exercise aerobically (sweating, increased heart rate, shortness of breath) for at least one-half hour?” Five possible response options are: “3 or more times a week”, “1–2 times per week”, “1–2 times per month”, “do not exercise regularly”, “cannot exercise due to disability/handicap”. In this study, no patient selected the option “1–2 times per month” at baseline or a year later. Responses of weekly exercise ≥3 times and 1–2 times were pooled as “regular exercise” (EXER-Yes). Responses of “do not exercise regularly” or “cannot exercise due to disability/handicap” were pooled as “no exercise” (EXER-No) [7]. Patients were classified into four groups according to exercise status at baseline and one year later: exercise at both baseline and one year later (EXER-Yes, EXER-Yes), no exercise at baseline but exercise one year later (EXER-No, EXER-Yes), exercise at baseline but not one year later (EXER-Yes, EXER-No), and no exercise at both baseline or one year later (EXER-No, EXER-No).
Statistical analysis
The MDHAQ is incorporated into the medical record for clinical care. The data also are entered into a database, which includes demographic, MDHAQ, medication and laboratory data. Means and standard deviations (SD) were calculated for normally distributed data, and medians and interquartile ranges (IQR) for non-normally distributed data. Baseline differences between patients in the four groups according to exercise status at baseline and one year later were compared using the chi square and Kruskall-Wallis tests. Mean change from baseline to one-year follow up was compared by analysis of variance (ANOVA) and presented as percentage of change. A negative change indicates improvement and a positive change indicates worsening. Bivariate regression analyses were performed to identify baseline variables associated with exercise or no exercise; variables that were significant in bivariate analyses were included as covariates in multivariate logistic regression analyses. All analyses were performed using STATA 12.0® for Mac (StataCorp LP, College Station, TX, USA).
Results
Patients
Overall, 795 patients with various rheumatic diagnoses were included in this study. The more prevalent diagnoses were RA (221 patients (27.8 %)), systemic lupus erythematosus (125 patients (15.7 %)), psoriatic arthritis (86 patients (10.8 %)), and osteoarthritis (58 patients (7.3 %)); 305 patients (38.4 %) had other diagnoses. Mean age was 51.1 years, 74.9 % were women, and 59 % were Caucasian. The proportion of patients with >12 years of education was 93 %, substantially higher than in the general population and in most patients seen in rheumatology clinical settings [18–20].
Exercise performance and clinical status at baseline and one year later
Participation in exercise at baseline and one year later (EXER-Yes, EXER-Yes) was reported by 324 patients (40.2 %), compared to 126 (15.8 %) who reported no exercise at baseline and exercise one year later (EXER-No, EXER-Yes), 77 (9.7 %) who reported exercise at baseline and no exercise at one year (EXER-Yes, EXER-No), and 268 (33.7 %), who reported no exercise at both time points (EXER-No, EXER-No) (Table 1). Patients who reported exercise at baseline and one year later (EXER-Yes, EXER-Yes group) had the lowest MDHAQ and DOCGL scores, indicating the best clinical status (p < 0.001) (Table 1). By contrast, patients in the EXER-No, EXER-No group were older, had a lower formal educational level, were more likely Hispanic, and had the poorest MDHAQ scores for physical function, pain, PATGL, RAPID3, fatigue, RADAI, and DOCGL compared to patients in the other groups (p < 0.001) (Table 1).
Associations between demographic and clinical variables and changes in exercise status from baseline to one-year follow up
Patients in the entire cohort improved (negative change) in each MDHAQ variable, including 15.5 % improvement in RAPID3 and 26.7 % improvement in RADAI scores. The highest level of improvement in RAPID3 and other MDHAQ scores (23.2–40 %) was in patients who reported no exercise at baseline but did report exercise one year later (EXER-No, EXER-Yes) (Table 2). By contrast, the patient group that reported exercise at baseline but not at one year later (EXER-Yes, EXER-No) was the only group with unchanged or poorer status one year later, albeit less than 6 % poorer, except for 15 % poorer physical function. The percentage improvement according to DOCGL did not differ significantly in the four groups (Table 2).
In bivariate logistic regression including all patients, older age (>50 years), lower educational level, poor physical function (score >1.3), high pain (score >5), high baseline RAPID3 (score >6), and high fatigue (score >5) at baseline were associated significantly with no exercise at baseline (Table 3). In multivariate analyses, older age, lower educational level, poorer function, and high fatigue remained significant independently; baseline age over 50 years and poor physical function were most strongly associated with no exercise.
Discussion
Our results indicate that 50.4 % of patients seen in routine care at one site in New York reported exercising one or more times per week at baseline [7]. This proportion was higher than seen in 31 % of US patients in the QUEST-RA database (29.1 % of 5235 patients from 21 countries) in response to the same query [7]. This finding may be explained in part by the considerably higher educational level of patients seen at NYU, with a median level of 16 years of formal education of, compared to 13.5 years for US patients in QUEST-RA and 10.9 years in all patients, as more educated patients are significantly more likely to exercise regularly [7].
Baseline MDHAQ scores were lowest (indicating better status) in patients who reported exercise at both time points, and highest in patients who reported no exercise at either time point. Mean changes in each MDHAQ score were highest in patients who reported no exercise at baseline, but regular exercise one year later, consistent with an observation that the greatest benefit of exercise is seen among the least fit individuals [21]. No significant differences were seen in the percentage of improvement according to DOCGL in any group. However, there was numerically greater improvement in the group which reported exercise at baseline but no exercise at one year, consistent with evidence of discordance between PATGL and DOCGL reported in an earlier study of many patients in the same cohort as in this report [22].
This study has several important limitations. The primary limitation involves the absence of information on causality - whether a change in exercise status may have preceded or resulted from a change in clinical status. Other limitations include the absence of any specific information on the type of exercise performed, whether rheumatologists reviewed the information about exercise, or how they might have used this information to counsel patients. Nonetheless, the data indicate that a simple query on an MDHAQ can assess exercise status quantitatively in routine care with no extra effort on the part of the rheumatologist or office staff, and indicates changes associated with other variables. Long-term exercise appeared not only to have no deleterious effects, but on the contrary, clinical benefit was seen, confirming results from previous studies [3–5].
Conclusions
In summary, our data indicate the pragmatic feasibility of screening for patient exercise status as a simple procedure in routine care, with no extra work on the part of the doctor, by having the patient complete an MDHAQ in the waiting area prior to seeing the rheumatologist. Such assessment provides a relatively easy strategy for rheumatologists to encourage patients to exercise regularly. Furthermore, eliciting the data through self-report could stimulate patients concerning the desirability of exercise in rheumatic conditions, and possibly motivate behavior change over time. The data indicate that the differences in the self-report exercise query were correlated with changes in clinical status, as no exercise at baseline but regular exercise one year later was associated with significant clinical improvement, although they do not explain whether improved clinical status resulted from or preceded regular exercise. Initial assessment of exercise in a feasible manner on a patient self-report MDHAQ appears to be a potentially helpful measure toward encouraging exercise as a component of care for all rheumatic diseases, toward better patient care and long-term outcomes, with no additional effort on the part of the rheumatologist.
Abbreviations
- ANOVA:
-
analysis of variance
- DOCGL:
-
physician global estimate of status
- EXER-No:
-
no regular exercise
- EXER-Yes:
-
regular exercise
- FN:
-
physical function
- IQR:
-
interquartile range
- MDHAQ:
-
multidimensional health assessment questionnaire
- NYU:
-
New York University
- PATGL:
-
patient global estimate of status
- RA:
-
rheumatoid arthritis
- RADAI:
-
rheumatoid arthritis disease activity index
- RAPID3:
-
routine assessment of patient index data
- SD:
-
standard deviation
- VAS:
-
visual analog scale
References
Short CL, Bauer W. The course of rheumatoid arthritis in patients receiving simple medical and orthopedic measures. N Engl J Med. 1948;238(5):142–8.
Smith RD, Polley HF. Rest therapy for rheumatoid arthritis. Mayo Clin Proc. 1978;53(3):141–5.
Hakkinen A, Sokka T, Kotaniemi A, Hannonen P. A randomized two-year study of the effects of dynamic strength training on muscle strength, disease activity, functional capacity, and bone mineral density in early rheumatoid arthritis. Arthritis Rheum. 2001;44(3):515–22.
de Jong Z, Munneke M, Zwinderman AH, Kroon HM, Ronday KH, Lems WF, Dijkmans BA, Breedveld FC, Vliet Vlieland TP, Hazes JM, et al. Long term high intensity exercise and damage of small joints in rheumatoid arthritis. Ann Rheum Dis. 2004;63(11):1399–405.
Perandini LA, de Sa-Pinto AL, Roschel H, Benatti FB, Lima FR, Bonfa E, Gualano B. Exercise as a therapeutic tool to counteract inflammation and clinical symptoms in autoimmune rheumatic diseases. Autoimmun Rev. 2012;12(2):218–24.
Sokka T, Pincus T. Poor physical function, pain and limited exercise: risk factors for premature mortality in the range of smoking or hypertension, identified on a simple patient self-report questionnaire for usual care. BMJ Open. 2011;1(1):e000070.
Sokka T, Hakkinen A, Kautiainen H, Maillefert JF, Toloza S, Mork Hansen T, Calvo-Alen J, Oding R, Liveborn M, Huisman M, et al. Physical inactivity in patients with rheumatoid arthritis: data from twenty-one countries in a cross-sectional, international study. Arthritis Rheum. 2008;59(1):42–50.
de Jong Z, Munneke M, Zwinderman AH, Kroon HM, Jansen A, Ronday KH, van Schaardenburg D, Dijkmans BA, Van den Ende CH, Breedveld FC, et al. Is a long-term high-intensity exercise program effective and safe in patients with rheumatoid arthritis? Results of a randomized controlled trial. Arthritis Rheum. 2003;48(9):2415–24.
van den Ende CH, Hazes JM, le Cessie S, Mulder WJ, Belfor DG, Breedveld FC, Dijkmans BA. Comparison of high and low intensity training in well controlled rheumatoid arthritis. Results of a randomised clinical trial. Ann Rheum Dis. 1996;55(11):798–805.
Munneke M, de Jong Z, Zwinderman AH, Jansen A, Ronday HK, Peter WF, Boonman DC, van den Ende CH, Vliet Vlieland TP, Hazes JM. Adherence and satisfaction of rheumatoid arthritis patients with a long-term intensive dynamic exercise program (RAPIT program). Arthritis Rheum. 2003;49(5):665–72.
Pincus T, Maclean R, Yazici Y, Harrington JT. Quantitative measurement of patient status in the regular care of patients with rheumatic diseases over 25 years as a continuous quality improvement activity, rather than traditional research. Clin Exp Rheumatol. 2007;25(6 Suppl 47):69–81.
Pincus T, Swearingen C, Wolfe F. Toward a multidimensional Health Assessment Questionnaire (MDHAQ): assessment of advanced activities of daily living and psychological status in the patient-friendly health assessment questionnaire format. Arthritis Rheum. 1999;42(10):2220–30.
Pincus T, Sokka T, Kautiainen H. Further development of a physical function scale on a MDHAQ [corrected] for standard care of patients with rheumatic diseases. J Rheumatol. 2005;32(8):1432–9.
Pincus T, Askanase AD, Swearingen CJ. A multi-dimensional health assessment questionnaire (MDHAQ) and routine assessment of patient index data (RAPID3) scores are informative in patients with all rheumatic diseases. Rheum Dis Clin North Am. 2009;35(4):819–27.
Pincus T, Castrejon I. MDHAQ/RAPID3 scores: quantitative patient history data in a standardized “scientific” format for optimal assessment of patient status and quality of care in rheumatic diseases. Bull NYU Hosp Jt Dis. 2011;69(3):201–14.
Pincus T, Yazici Y, Bergman M. Development of a multi-dimensional health assessment questionnaire (MDHAQ) for the infrastructure of standard clinical care. Clin Exp Rheumatol. 2005;23(5 Suppl 39):S19–28.
Stucki G, Liang MH, Stucki S, Bruhlmann P, Michel BA. A self-administered rheumatoid arthritis disease activity index (RADAI) for epidemiologic research. Psychometric properties and correlation with parameters of disease activity. Arthritis Rheum. 1995;38(6):795–8.
U.S. Census Bureau [http://www.census.gov/] Accessed 2015.
Sokka T, Kautiainen H, Toloza S, Makinen H, Verstappen SM, Lund Hetland M, Naranjo A, Baecklund E, Herborn G, Rau R, et al. QUEST-RA: quantitative clinical assessment of patients with rheumatoid arthritis seen in standard rheumatology care in 15 countries. Ann Rheum Dis. 2007;66(11):1491–6.
Pincus T, Marcum SB, Callahan LF, Adams RF, Barber J, Barth WF, Gordon GV, Huston JW, Polk JR, Whelton JC, et al. Longterm drug therapy for rheumatoid arthritis in seven rheumatology private practices: I. Nonsteroidal antiinflammatory drugs. J Rheumatol. 1992;19(12):1874–84.
Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346(11):793–801.
Castrejon I, Yazici Y, Samuels J, Luta G, Pincus T. Discordance of global estimates by patients and their physicians in usual care of many rheumatic diseases: association with 5 scores on a multidimensional health assessment questionnaire (MDHAQ) that are not found on the health assessment questionnaire (HAQ). Arthritis Care Res (Hoboken). 2014;66(6):934–42.
Acknowledgements
We are indebted to all colleagues and staff in the NYU Hospital for Joint Diseases for their cooperation and data supply. The authors are grateful to all patients who completed the questionnaires. This work was supported by internal funding.
Authors’ contributions
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. Study conception and design: IC and TP. Acquisition of data: YY and SC. Analysis and interpretation of data: IC, TP, YY and SC.
Competing interests
Dr. Pincus is president of Health Report Services, Inc., which owns a copyright and trademark for MDHAQ and RAPID3. Royalties and license fees are received from for-profit pharmaceutical and electronic medical record companies for the use of MDHAQ/RAPID3, all of which are transferred to medical schools for further development of quantitative measurement in clinical rheumatology care. The authors declare that they have no other competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Castrejón, I., Yazici, Y., Celik, S. et al. Pragmatic assessment of exercise in routine care using an MDHAQ: associations with changes in RAPID3 and other clinical variables. Arthritis Res Ther 18, 199 (2016). https://doi.org/10.1186/s13075-016-1095-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13075-016-1095-x