Abstract
Background
Although Plasmodium falciparum infection is largely documented and this parasite is the main target for malaria eradication, other Plasmodium species persist, and these require more attention in Africa. Information on the epidemiological situation of non-P. falciparum species infections is scarce in many countries, including in the Democratic Republic of the Congo (hereafter Republic of the Congo) where malaria is highly endemic. The aim of this study was to determine the prevalence and distribution of non-P. falciparum species infections in the region south of Brazzaville.
Methods
A cross-sectional survey was conducted in volunteers living in rural and urban settings during the dry and rainy seasons in 2021. Socio-demographic and clinical parameters were recorded. Plasmodium infection in blood samples was detected by microscopic analysis and nested PCR (sub-microscopic analysis).
Results
Of the 773 participants enrolled in the study, 93.7% were from the rural area, of whom 97% were afebrile. The prevalence of microscopic and sub-microscopic Plasmodium spp. infection was 31.2% and 63.7%, respectively. Microscopic Plasmodium malariae infection was found in 1.3% of participants, while sub-microscopic studies detected a prevalence of 14.9% for P. malariae and 5.3% for Plasmodium ovale. The rate of co-infection of P. malariae or P. ovale with P. falciparum was 8.3% and 2.6%, respectively. Higher rates of sub-microscopic infection were reported for the urban area without seasonal fluctuation. In contrast, non-P. falciparum species infection was more pronounced in the rural area, with the associated risk of the prevalence of sub-microscopic P. malariae infection increasing during the dry season.
Conclusion
There is a need to include non-P. falciparum species in malaria control programs, surveillance measures and eradication strategies in the Republic of the Congo.
Graphical Abstract

Similar content being viewed by others
Background
Malaria is a life-threatening disease caused by parasites that are transmitted to people through the bites of infected female Anopheles mosquitoes. The WHO estimated that in 2020 there were 241 million malaria cases in 85 malaria endemic countries worldwide, an increase from 227 million in 2019, mainly in countries in the WHO African Region [1]. Also, malaria deaths increased by 12% compared with 2019, to an estimated 627,000; an estimated 47,000 (68%) of the additional 69,000 deaths were due to service disruptions during the COVID-19 pandemic [1].
Among the Plasmodium species infecting humans in Africa, Plasmodium falciparum is the major cause of malaria cases (99.7%) [2], with a minor but underestimated prevalence of other Plasmodium species [3]. Plasmodium vivax is the predominant parasite in the WHO region of Americas, causing 75% of malaria cases [4]. Although few studies have identified P. vivax infections in Mali and Nigeria [5,6,7], this Plasmodium species remains non-endemic in West and Central Africa because of the lack of the Duffy antigen receptor for chemokines, which is essential for erythrocyte invasion by the parasite [8]. Plasmodium ovale infection represents < 1% of all malaria infections worldwide [9, 10]. Despite its low prevalence, however, P. ovale infections are directly linked to the danger of relapses after months or even years due to the presence of hypnozoites [11, 12], which may cause severe disease and even death [13]. The global distribution of Plasmodium malariae is sparse and variable, but frequently co-endemic with P. falciparum [14, 15]. A low prevalence of P. malariae infection is commonly reported with asymptomatic cases, however patients may occasionally develop severe symptoms [16]. In addition, the recrudescence of P. malariae blood-stage parasites can occur for long periods, even after the infected person has left endemic regions [17, 18].
Despite the decrease in malaria-related morbidity since 2016, the burden of malaria in the Democratic Republic of the Congo (hereafter Republic of the Congo) remains high, with P. falciparum as the most prevalent malaria-causing species. A systematic review of the epidemiology revealed that 37% of Congolese living in urban areas tested positive for microscopic P. falciparum infection compared to 59% in the peri-urban areas, with these populations showing 11% and 20% submicroscopic infections, respectively [19]. However, recent information on the epidemiology of non-Plasmodium falciparum species, mainly P. malariae and P. ovale, is limited. Taking into account the new malaria elimination strategies based on the interruption of local transmission of human Plasmodium [20], intensification of malaria species surveillance has been strongly recommended. Therefore, the aim of the present study was to determine the prevalence and the distribution of P. malariae and P. ovale infection, based on multiple community surveys in rural and urban settings in Brazzaville, the capital of the Republic of the Congo and home to > than 50% of the Congolese population.
Methods
Study areas
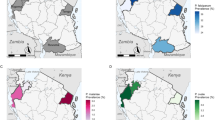
The study was conducted in rural areas of the Goma Tsé-Tsé District (Ntoula and Djoumouna villages) in the Department of Pool and in the urban area of Brazzaville Department (Mayanga in the West Quarter of Madibou District) of the Republic of the Congo (Fig. 1). The two departments have a tropical humid climate divided in two seasons: a short dry season (June to September) and a long rainy season (October to May). The geo-location of these zones is 4.36° S, 15.15° E, and the average altitude is 217 m a.s.l [21]. Djoumouna is a village located 25 km from Brazzaville. It is characterized by the presence of a gallery forest bordering the Djoumouna River. The locality is surrounded by four rivers (Lomba, Kinkoue, Loumbangala and Djoumouna rivers) which supply water to a series of fish farming ponds [22] that can serve as potential foci of malaria vectors. The population of Djoumouna village comprises about 800 inhabitants, with agriculture as the main economic activity. Ntoula is a neighboring village of Djoumouna and irrigated by two rivers. This village has around 635 inhabitants who mainly depend on agriculture and fishing for their livelihoods. Mayanga is an urban area located in the 8th Madibou District in the south of Brazzaville. With a population of about 28,422 inhabitants, Mayanga is characterized by the presence of market gardening sites (Agni-Congo 1 and 2 and the Groupement Jean Felicien Mahouna). Irrigation water is supplied by three rivers (Djoué, Laba and Matou rivers). Several public and private services are established in Mayanga, such as health centers and primary and secondary schools.
Map of the Republic of the Congo (a) showing the localities surveyed in Goma Tsé-Tsé District (b) and Madibou District (c). In Goma Tsé-Tsé District, the red dots represent the selected villages (Ntoula and Djoumouna), and in Madibou district the red striped area represents the urban area (Mayanga) selected for the survey
Study design
A cross-sectional survey was carried out from March to September 2021, covering both the rainy and dry seasons. Individuals aged at least 1 year who lived in the study areas for at least 3 months were included in the study. Volunteers from a random sample of households were recruited in each area. Participants who decided to withdraw their consent during the study were excluded from the analysis. Socio-demographic and clinical data of the participants were recorded in a well-structured collection sheet (age, gender, temperature, bed net use etc.). The axillary temperature was determined to define fever in the participants. Fever was diagnosed when the axillary temperature was ≥ 37.5 °C [23, 24]. Bed net use was defined based on the answers of participants, and on the observation of bed nets in each household. After an examination by a clinician (diagnosis of fever, headaches, vomiting, nausea etc.), blood samples (3 ml) were collected in EDTA tubes by a nurse and the tubes then transported to the “Centre de Recherches sur les Maladies Infectieuse-Christophe Merieux” (CeRMI) for further investigations, including thick and thin blood smears for microscopic examination. Participants presenting a positive blood smear were treated by the medical staff with artemisinin-based combination therapy (ACT) in accordance to WHO and national malaria program policies [25]. Hemoglobin level was determined performed using CYANHemato, a fully automated bench-top hematology cell counter (Cypress Diagostic, Hulshout, Belgium).
Microscopic screening of Plasmodium infections
Plasmodium infection was screened by microscopy using the Lambaréné method [26]. In brief, 10 µl of whole blood of each sample was distributed on a microscope slide over a rectangular area of 10 × 8 mm. The contour of the rectangle was drawn on a piece of paper placed under the slide before the whole blood sample was spread. The slides were air dried and stained for 20 min with 20% Giemsa solution (Giemsa R-Solution [Merck, Darmstadt, Germany], Titrisol buffer pH 7.2 [Merck]). Each slide was read by two microscopists. When no agreement was reached on a specific slide, a third microscopist was asked to decide. Positive slides of each parasite species served as the quality controls of the microscopy studies. The number of parasites and the number of high-power fields (HPF) were counted, and parasitemia per microliter was calculated using the microscope factor of 708 as follows:
where N is the number and para represents parasites.
Plasmodium species identification by PCR
The parasite’s DNA was extracted from 200 µl whole blood samples using the QIAamp DNA mini Kit (Qiagen, Hilden, Germany) according to the manufacturer’s instructions. DNA was recovered in 150 µl of elution buffer and stored at − 20 °C until use.
The detection of malaria parasite DNA was based on nested PCR amplification of the 18S ribosomal RNA (rRNA) gene in a total reaction volume of 20 µl using the appropriate primers (Additional File 1: Table S1). The first PCR reaction targeted the Plasmodium spp. and was performed in a reaction volume composed of 18 µl of a master mix (2.5 µl of 10× PCR buffer, 1.25 µl of 25 mM MgCl2, 0.5 µl of 10 mM dNTPs, 0.5 µl of each 10 µM primer, 0.25 µl of Taq DNA polymerase 5U/µl and 12.5 µl of nuclease-free water) and 2 μl of the extracted DNA. The reaction was carried out under the following cycling conditions: an initial denaturation at 94 °C for 4 min; followed by 35 cycles of denaturation at 94 °C for 30 s, annealing at 55 °C for 1 min and extension at 72 °C for 1 min, with a final extension at 72 °C for 4 min. In the second PCR, 19 µl of master mix (containing 13.5 µl of nuclease-free water and the same volume of reagents as described for the first PCR) and 1 µl of primary PCR product were added to the PCR tube, and the reaction was carried out under the same cycling conditions as described for the first PCR, except that the annealing temperature was 58 °C.
PCR products and the 100-bp molecular weight maker were stained with Syber Green solution (1:1, v/v), electrophesed at 100 V for 45 min in a 1.5% agarose gel and visualized on the GelDoc™ EZ Imager (Bio-Rad Laboratories, Hercules, CA, USA). A sample was considered positive for P. falciparum, P. malaria, P. ovalea or P. Vivax if a 205-bp, 144-bp, 800-bp or 120-bp band was detected, respectively. The known Plasmodium-positive samples from our library and distilled water served as positive and negative controls, respectively, in every set of reactions.
Statistical analysis
Management and tabulation of raw data were carried out using Microsoft Excel (Microsoft Inc., Redmond, WA, USA) version 2016. All statistical analyses were performed using SPSS version 22.1 (SPSS, IBM Corp., Armonk, NY, USA). The normality of data distribution was checked using the Shapiro–Wilk test [27]. Variables were expressed as proportions for categorical variables or as medians (with range)/means (standard deviations [SD}) for continuous variables. The prevalence of Plasmodium spp. infections was determined as the proportion of individuals identified as positive for the presence of parasites (either for all parasite species or for an individual species) in each community. Age was stratified into five groups according to WHO guidelines [28]: 1–4, 5–9, 10–14, 15–19 and ≥ 20 years.
Participants with a negative result in the microscopic examination, but positive in the PCR analysis were classified as the sub-microscopically infected group. Those who had microscopic Plasmodium-positive results were classified as the microscopically infected group.
Chi-square tests (or Fisher’s exact tests when appropriate) were used to calculate the differences in participant characteristics and prevalences among groups, and to assess associations between independent variables and Plasmodium spp infection. The strength of association between each risk factor and the occurrence of Plasmodium infection was calculated using univariate logistic regression. The relative risks (RR) and 95% confidence intervals (CIs) were calculated to determine the risk factors associated with Plasmodium infection. The level of significance was set at P < 0.05.
Ethical consideration
This study received ethical approval from the Institutional Ethics Committee of “Fondation Congolaise pour la Recherche Medical” (No. 013/CIE/FCRM/2018), administrative authorizations from the Marien Ngouabi University (No. 247/UMNG.FST.DFD.FD-SBIO) and approval from the major of each study area. Prior to enrollment, participants were informed in writing and orally about the study and its benefits. Before enrollment, a consent form was signed by each participant or by the parent of a participant who was a minor (< 18 years). Children aged between 15 to 17 years signed an assent form.
Results
Characteristics of the study population
Of the 773 participants enrolled in this study 573 and 200 were resided in Goma Tsé-Tsé District (District 1) and Madibou District (District 2), respectively (Table 1). The age of the participants ranged from 1 to 88 years, with a median age of 15 (range: 1–88) years in Goma Tsé-Tsé District and 16 (range: 2–81) years in Madibou District. There were more female than male participants in both districts (Goma Tsé-Tsé: 54.5% [312/573]; Madibou: 59.5% [119/200]). Of the five age groups, participants aged > 20 years formed the largest group in both districts (Goma Tsé-Tsé: 41.5% [238/573]; Madibou: 45.5% [91/200]). A total of 42 of the 773 participants (5.4%) presented an increased axillary temperature. Almost all study participants slept under bed nets in both study areas.
Microscopic Plasmodium spp. infection
The overall prevalence of Plasmodium spp. was 31.2% (241/773) (Table 2). Among the identified Plasmodium species, P. falciparum was detected in 30.7% (237/773) of the study population (including 29.9% [231/773] as mono-infection), while P. malariae was prevalent at a level of 1.3% (10/773) individuals (including 0.5% [4/773] as mono-infection). The rate of P. falciparum/P. malariae co-infection was 0.8% (6/773). According to the districts, the rate of positive microscopic infection was significantly (P < 0.0001) higher in Goma Tsé-Tsé (35.1%; 201/573) than in Madibou (20.0%; 40/200). Plasmodium malariae was identified in 1.4% (8/573) of the participants living in Goma Tsé-Tsé District with 0.7% (4/573) of cases co-infected or not with P. falciparum. Plasmodium malariae was detected in 1% (2/200) of the participants living in Madibou as co-infection with P. falciparum. Although the prevalence of microscopic Plasmodium spp. infection was low in participants aged < 5 years (28.4%; 21/74), parasite density in children in this age group was higher both for P. falciparum and P. malariae than in children aged between 6 and 14 years (Fig. 2).
Sub-microscopic Plasmodium spp. infection
Sub-microscopic Plasmodium spp. infections were found in 63.7% (339/532) of all samples (Table 2). Regardless of co-infections, P. falciparum, P. malariae and P. ovale were detected by PCR in 58.1% (309/532), 14.9% (79/532) and 5.3% (28/532) of participants, respectively. Dual Plasmodium infection with P. falciparum/P. malariae accounted for 8.3% (44/532) of Plasmodium spp. infections, while dual infections with P. falciparum/P. ovale and P. malariae/P. ovale accounted for 2.6% (14/532) and 0.2% (1/532), respectively. Triple infections were detected in 1.7% of all participants.
According to study site, sub-microscopic Plasmodium spp. infection was significantly higher (P = 0.0099) in Madibou (72.5%; 116/160) than in Goma Tsé-Tsé (59.9%; 223/372). A similar trend was observed for the prevalence of mono-infection by P. falciparum (Madibou: 56% (89/160); Goma Tsé-Tsé: 41% [153/372]), while the reverse was observed for P. malariae infection (Goma Tsé-Tsé: 5.1% [19/372]; Madibou: 3.8% [6/160]) and P. ovale infection (Goma Tsé-Tsé: 1.1% [4/372]; Madibou: 0.0% [0/160]). The prevalence of sub-microscopic infection was high in all age groups (Fig. 2), with study participants between the ages of 15 and 19 years harboring a highest proportion of sub-microscopic infection (77.3%).
Predictors of microscopic malaria infection
The relationship between participant characteristics and the presence of Plasmodium spp. infections was investigated. Those participants found to be anemic were classified according to their age group following the WHO guideline [29]. Plasmodium falciparum infection was significantly associated with anemia in children aged < 15 years (P = 0.0374 for children aged 1–4 years, P = 0.0001 for 5- to 9-year olds, P < 0.0001 for 10–to 14-year olds), but no relationship was observed between P. malariae infection and the risk of anemia (Table 3). As shown in Table 4, the rainy season was shown to be a risk factor (RR: 3.1, 95% CI: 1.7–5.7; P = 0.0003) for increased P. falciparum prevalence in Madibou. Plasmodium falciparum infection was associated with gender in Goma Tsé-Tsé (RR: 1.4, 95% CI: 1.1–1.7; P = 0.0072), but no such association was found in Madibou. According to the age group, P. falciparum prevalence for all age group was higher in Goma Tsé-Tsé District than in Mabidou District, with participants aged 5 to 14 years having a higher risk of malaria infection. The presence of fever was significantly (P = 0.0223 [Goma Tsé-Tsé]; P = 0.0306 [Madibou]) associated with P. falciparum infection in the two districts. No association was observed between the socio-demographic characteristics of the study population and the microscopic prevalence of P. malariae in the two districts (Table 5).
Predictors of sub-microscopic malaria infection
In Madibou District, the risk of sub-microscopic P. falciparum infection increased during the rainy season (RR: 1.3, 95% CI: 1.0—1.5; P = 0.020), and in the absence of bed net use. Participants aged between 15 and 19 years were at the highest risk (RR: 1.5, 95% CI: 1.0—2.1; P = 0.041) of sub-microscopic P. falciparum infection in Goma Tsé-Tsé District (Table 6). In the Goma Tsé-Tsé area, individuals were at a higher risk (RR: 1.7, 95% CI: 1.0—2.8; P = 0.045) of sub-microscopic P. malariae infection during the dry season. No risk factor was identified for the presence of sub-microscopic P. ovale infection (Tables 7, 8).
Discussion
Since publication of the systematic review on the malaria situation in the Republic of the Congo in 2016 [19], studies conducted in the country have mostly focused on the epidemiology and diversity of P. falciparum infection [30,31,32]. However, information on the epidemiological situation of non-Plasmodium falciparum species in the country is lacking. The aim of the present study was to evaluate the prevalence of Plasmodium species in two endemic areas for malaria of the Republic of the Congo, namely Goma Tsé-Tsé District, as representative of rural areas in the Republic of the Congo, and Madibou District, which is an urban area. Of 773 participants enrolled in this study, 573 and 200 were living in Goma Tsé-Tsé District and Madibou District, respectively. This vast difference in number of participants reflects the low interest of the population of Madibou to participate in the study, possibly due to the presence of health centers close by. Almost all study participants were sleeping under bed nets (97.4%), suggesting a strict compliance of the inhabitants of these localities to the malaria control measures.
The overall prevalence of Plasmodium spp. detected by microscopy was 31.2% in this study. Plasmodium falciparum remained the most prevalent species, in accordance with prevalences reported in many previous studies conducted in African malaria endemic areas [33,34,35,36]. The high prevalence of P. falciparum in the overall study population demonstrates the importance of malaria control strategies specifically against this species. The prevalence of malaria infection was significantly higher in villages of Goma Tsé-Tsé District than in Madibou District, which may be related to the different ecological situations in these two areas (rural vs. urban) [37]. The prevalence of Plasmodium spp. in this study was higher than that reported in recent studies in Benin (23.7%) by our research group [33], but similar to the findings of Amoah et al. (32%) [34].
Among the identified non-P. falciparum species in the whole study population, only P. malariae was detected by microscopy at a rate of 1.3% (with 0.8% of dual P. falciparum/P. malariae infection). This prevalence was higher in the rural area of Goma Tsé-Tsé District (1.4%) compared to the urban area of Madibou District (1%), suggesting that this variation in prevalence was probably due to the socio-demographic characteristics of each study area. Suitable containers or conditions for water to pool and persist, deforestation and agriculture have all been associated with an increased risk of malaria transmission [37]. The P. malariae prevalence observed in this study was comparable to that reported in Benin, in which an increase of this prevalence was observed over the past 10 years [33]. A potential explanation could be the differences in the use of bed nets by the population. Almost all participants of this study, compared to less than one quarter of the study population in Benin, slept under a bed net. This difference highlights a heath preoccupation related to this species among the non-Plasmodium falciparum parasites that must be taken into account in the WHO strategic plan for malaria eradication [20].
The rainy season was associated with a higher prevalence of P. falciparum infection in Madibou District. In the villages of Goma Tsé-Tsé District, where the prevalence of P. falciparum was high and almost stable throughout the year, men and children appeared to be at higher risk of getting malaria infection. All of these results suggest that malaria management strategies must be directly applicable to the area they are being used: in urban areas, they should take seasonality into account; in rural areas, they must be permanent, with a particular focus on the sensitization of men and adolescents. Fever was significantly associated with P. falciparum infection in the two districts of this study. We did not observe any association between socio-demographic factors or clinical outcomes with an increased prevalence of P. malariae, probably due to low number of events and, therefore, power issues. However, many studies have reported a significant association of P. malariae infection with severe anemia, probably due to prolonged erythrocyte destruction and bone marrow suppression with a minimal reduction in erythrocyte life-span at a low parasitemia level [38, 39]. Pulmonary complications and renal impairment have also been reported to be associated with P. malariae infection [40]. The pooled proportion of severe complication caused by P. malariae infection was reported to be 2% [16].
Compared to microscopic malaria infection, a higher sub-microscopic infection (63.7%) of Plasmodium spp. was observed, being more pronounced in older participants (> 15 years). These findings are similar to those reported in a previous study from Ghana (66%) [34], and higher than those reported from a study conducted in Benin [33]. This difference could be attributed to geographical zone, including the level of local Plasmodium infection endemicity. Indeed, in Benin, the survey was conducted in villages, while in Ghana, the study covered a mixture of communities. In addition, the sub-microscopic prevalence in our study varied with respect to the study district, being lower (59.8%) in the rural area compared to the urban areas (73%). The high prevalence of sub-microscopic infections observed in the present study, as well as in other studies [19, 30], represents a major challenge to malaria control programs in the Republic of the Congo since the management of malaria patients is based on the microscopic detection of parasites. Our findings suggest that despite the best efforts of the national malaria program, malaria transmission will continue to be high because half of infected individuals remain afebrile and will, therefore, not be identified as having malaria and subsequently treated. Among the non-P. falciparum identified by PCR, P. malariae and P. ovale were detected in 14.9% and 5.3% of participants, respectively. In terms of co-infection, participants co-infected with P. falciparum/P. malariae (8.3%) were the most prevalent, followed by participants co-infected with P. falciparum/P. ovale (2.6%). It is notable that although non-P. falciparum parasites were hardly detected by microscopy, the high rates of sub-microscopic detection of these parasites translate into perennial transmission of these species in endemic areas, thereby constituting a major challenge to achieving malaria eradication. The presence of persons with P. ovale and P. malariae co-infected with P. falciparum in this study highlights the impact of those two latter parasites in asymptomatic and chronic malaria infection. This becomes more critical with triple infection, which was detected at a sub-microscopic prevalence of 1.7% in the present study. Plasmodium malariae and P. ovale are rarely associated with severe cases of malaria, but their persistence in the body remains a great challenge for malaria eradication. Although P. malariae does not cause malarial relapse from persistent liver-stage parasites, recrudescence of blood-stage parasites can occur after long periods without signs or symptoms, even after the infected person has left the endemic region [17, 18]. Even with appropriate treatment, chronic sub-clinical P. malariae infection can occur because of its extended pre-patent period when inadequate drug levels in the blood cannot eliminate newly emerging merozoites [41, 42]. Plasmodium ovale is responsible for malaria relapses, even after months or even years without the person showing symptoms, due to the presence of hypnozoites [11, 12]. In the present study, the urban setting was revealed as a zone of higher perennial sub-microscopic infection, compared to the rural area where the non-P. falciparum species were more pronounced during the dry season. The reason for this association remains unclear. The small numbers of non-P. falciparum species detected in our study is a limitation to this study, especially in sub-analyses on demography or other clinical factors.
Conclusions
The results of this study highlight the need to include non-P. falciparum species in malaria control programs, surveillance measures and eradication strategies in the Republic of the Congo. Therefore, a continuous systematic prevention promoting the use of bed nets and intermittent treatment of pregnant women, screening and treatment of Plasmodium-infected individuals living in high-transmission settings may strengthen malaria intervention measures.
Availability of data and materials
All data are fully available without restriction. Data are available from the FCRM Institutional Data Access. All request for Data should be addressed to the Executive Director of FCRM reachable by the following address Prof. Francine Ntoumi, Villa D6, Cité OMS-Djoué, Brazzaville, République du Congo (Tel. +242-06-9977980, email: francine.ntoumi@uni-tuebingen.de.
Abbreviations
- ACT:
-
Artemisinin-based combination therapy
- CeRMI:
-
Centre de recherche sur les maladies infectieuses—Christoph Merieux
- HPF:
-
High power field
- RR:
-
Relative risk
References
WHO. World malaria report 2021. 2021. Geneva: WHO/Global Malaria Programme.https://www.who.int/teams/global-malaria-programme/reports/world-malaria-report-2021.
WHO. World malaria report 2019. 2019. Geneva: WHO/Global Malaria Programme. https://www.who.int/publications/i/item/9789241565721.
Owusu EDA, Brown CA, Grobusch MP, Mens P. Prevalence of Plasmodium falciparum and non-P. falciparum infections in a highland district in Ghana, and the influence of HIV and sickle cell disease. Malar J. 2017;16:167.
WHO: World malaria report 2020: 20 years of global progress and challenges. 2020. Geneva: WHO. https://apps.who.int/iris/handle/10665/337660.
Niangaly A, Karthigayan G, Amed O, Coulibaly D, Sa JM, Adams M, et al. Plasmodium vivax infections over 3 Years in duffy blood group negative Malians in Bandiagara Mali. Am J Trop Med Hyg. 2017;97:744–52.
Bernabeu M, Gomez-Perez GP, Sissoko S, Niambele MB, Haibala AA, Sanz A, et al. Plasmodium vivax malaria in Mali: a study from three different regions. Malar J. 2012;11:405.
Oboh MA, Badiane AS, Ntadom G, Ndiaye YD, Diongue K, Diallo MA, et al. Molecular identification of Plasmodium species responsible for malaria reveals Plasmodium vivax isolates in Duffy negative individuals from southwestern Nigeria. Malar J. 2018;17:439.
Zimmerman PA, Ferreira MU, Howes RE, Mercereau-Puijalon O. Red blood cell polymorphism and susceptibility to Plasmodium vivax. Adv Parasitol. 2013;81:27–76.
Collins WE, Jeffery GM. Plasmodium ovale: parasite and disease. Clin Microbiol Rev. 2005;18:570–81.
Autino B, Noris A, Russo R, Castelli F. Epidemiology of malaria in endemic areas. Mediterr J Hematol Infect Dis. 2012;4:e2012060.
Robinson LJ, Wampfler R, Betuela I, Karl S, White MT, Li Wai Suen CS, et al. Strategies for understanding and reducing the Plasmodium vivax and Plasmodium ovale hypnozoite reservoir in Papua New Guinean children: a randomised placebo-controlled trial and mathematical model. PLoS Med. 2015;12:e1001891.
Costescu Strachinaru DI, Wauters A, Van Esbroeck M, Strachinaru M, Vanbrabant P, Soentjens P. A cluster of Plasmodium ovale infections in Belgian military personnel after deployment in Kindu Democratic Republic of Congo: a retrospective study. Trop Med Infect Dis. 2021;6:125.
Lau YL, Lee WC, Tan LH, Kamarulzaman A, Syed Omar SF, Fong MY, et al. Acute respiratory distress syndrome and acute renal failure from Plasmodium ovale infection with fatal outcome. Malar J. 2013;12:389.
Collins WE, Jeffery GM. Plasmodium malariae: parasite and disease. Clin Microbiol Rev. 2007;20:579–92.
Culleton RL, Mita T, Ndounga M, Unger H, Cravo PV, Paganotti GM, et al. Failure to detect Plasmodium vivax in West and Central Africa by PCR species typing. Malar J. 2008;7:174.
Kotepui M, Kotepui KU, De Jesus Milanez G, Masangkay FR. Plasmodium spp. mixed infection leading to severe malaria: a systematic review and meta-analysis. Sci Rep. 2020;10:11068.
Hedelius R, Fletcher JJ, Glass WF 2nd, Susanti AI, Maguire JD. Nephrotic syndrome and unrecognized Plasmodium malariae infection in a US Navy sailor 14 years after departing Nigeria. J Travel Med. 2011;18:288–91.
Siala E, Khalfaoui M, Bouratbine A, Hamdi S, Hili K, Aoun K. Relapse of Plasmodium malariae malaria 20 years after living in an endemic area. Presse Med. 2005;34:371–2.
Koukouikila-Koussounda F, Ntoumi F. Malaria epidemiological research in the Republic of Congo. Malar J. 2016;15:598.
WHO. A framework for malaria elimination. 2017. Geneva: WHO/Global Malaria Programme. https://www.who.int/publications/i/item/9789241511988.
Getamap.net. Geography of the Republic of Congo. Jan 2022. http://fr.getamap.net/about/republic_of_the_congo/geography.html.
Nianga BGOT, Bitsindou P, Lenga A. Impact of the use of mosquito nets on malaria transmission in Djoumouna (Brazzaville-Congo). Int J Adv Res. 2019;7:285–94.
Oyakhirome S, Profanter K, Kremsner PG. Assessment of fever in African children: implication for malaria trials. Am J Trop Med Hyg. 2010;82:215–8.
Mackowiak PA, Wasserman SS, Levine MM. A critical appraisal of 98.6 degrees F, the upper limit of the normal body temperature, and other legacies of Carl Reinhold August Wunderlich. JAMA. 1992;268:1578–80.
Group AC, Zinsou C, Cherifath AB. The malaria testing and treatment landscape in Benin. Malar J. 2017;16:174.
Joanny F, Lohr SJ, Engleitner T, Lell B, Mordmuller B. Limit of blank and limit of detection of Plasmodium falciparum thick blood smear microscopy in a routine setting in Central Africa. Malar J. 2014;13:234.
Shapiro SS, Wilk MB. An analysis of variance test for normality (complete samples). Biometrika. 1965;52:591–611.
WHO. Age standardization of rates: A new WHO standard. 2001. Geneva: WHO. https://qmplus.qmul.ac.uk/pluginfile.php/154532/mod_book/chapter/3129/Age%20standardization%20of%20rates.pdf.
WHO. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. 2011. Geneva: WHO. https://apps.who.int/iris/handle/10665/85839.
Mbouamboua Y, Koukouikila-Koussounda F, Ntoumi F, Adukpo S, Kombo M, Vouvoungui C, et al. Sub-microscopic Plasmodium falciparum infections in matched peripheral, placental and umbilical cord blood samples from asymptomatic Congolese women at delivery. Acta Trop. 2019;193:142–7.
Singana BP, Mayengue PI, Niama RF, Ndounga M. Genetic diversity of Plasmodium falciparum infection among children with uncomplicated malaria living in Pointe-Noire, Republic of Congo. Pan Afr Med J. 2019;32:183.
Mayengue PI, Kouhounina Batsimba D, Niama RF, Ibara Ottia R, Malonga-Massanga A, Fila-Fila GPU, et al. Variation of prevalence of malaria, parasite density and the multiplicity of Plasmodium falciparum infection throughout the year at three different health centers in Brazzaville Republic of Congo. BMC Infect Dis. 2020;20:190.
Agonhossou R, Akoton R, Dossou YA, Avokpaho E, Mbama DNJ, Boussougou-Sambe TS, et al. Surveillance of Plasmodium malariae infection among inhabitants of rural areas in Ouidah-Kpomasse-Tori Bossito health district Benin. Parasitol Res. 2022;121:275–86.
Amoah LE, Donu D, Abuaku B, Ahorlu C, Arhinful D, Afari E, et al. Probing the composition of Plasmodium species contained in malaria infections in the Eastern region of Ghana. BMC Public Health. 2019;19:1617.
Damien GB, Djenontin A, Rogier C, Corbel V, Bangana SB, Chandre F, et al. Malaria infection and disease in an area with pyrethroid-resistant vectors in southern Benin. Malar J. 2010;9:380.
Doritchamou JYA, Akuffo RA, Moussiliou A, Luty AJF, Massougbodji A, Deloron P, et al. Submicroscopic placental infection by non-falciparum Plasmodium spp. PLoS Negl Trop Dis. 2018;12:e0006279.
Stresman GH. Beyond temperature and precipitation: ecological risk factors that modify malaria transmission. Acta Trop. 2010;116:167–72.
Douglas NM, Lampah DA, Kenangalem E, Simpson JA, Poespoprodjo JR, Sugiarto P, et al. Major burden of severe anemia from non-falciparum malaria species in Southern Papua: a hospital-based surveillance study. PLoS Med. 2013;10:e1001575.
Langford S, Douglas NM, Lampah DA, Simpson JA, Kenangalem E, Sugiarto P, et al. Plasmodium malariae Infection associated with a high burden of anemia: a hospital-based surveillance study. PLoS Negl Trop Dis. 2015;9:e0004195.
Chaparro P, Padilla J, Vallejo AF, Herrera S. Characterization of a malaria outbreak in Colombia in 2010. Malar J. 2013;12:330.
McKenzie FE, Jeffery GM, Collins WE. Plasmodium malariae blood-stage dynamics. J Parasitol. 2001;87:626–37.
Maguire JD, Baird JK. The ‘non-falciparum’ malarias: the roles of epidemiology, parasite biology, clinical syndromes, complications and diagnostic rigour in guiding therapeutic strategies. Ann Trop Med Parasitol. 2010;104:283–301.
Acknowledgements
We are grateful to the residents of Ntoula, Djoumouna and Mayanga for their participation in this study and the administration of the health district of Goma Tsé-Tsé and Madibou for their strong and fruitful collaboration. We thank Destin Tati, logistic manager at FCRM, for promptly providing the material needed. We also thank the Foundation MERIEUX for their support.
Funding
This study was supported by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) grant (BO 2494/3–1) awarded to the CoMAL project consortium. AL is funded through the Fondation Merieux. This work also received support from CANTAM (EDCTP-CSA2020NoE-3100). The funders did not play a role in the design of the study, collection, analysis, and interpretation of data, as well as the writing of the manuscript.
Author information
Authors and Affiliations
Contributions
JDMN: Investigation, methodology, writing of original draft, formal analysis, review and editing. AL: Investigation, methodology, writing of original draft, review and editing. JCD: Methodology, review and editing. SDK: Investigation, review and editing. KRB: Patient’s monitoring. JM: Investigation, review and editing. CV: Data analysis. DNN: Investigation. FNN: Investigation. CN: Investigation. RA: Investigation. RA: Investigation. TSB: Investigation. AL: Review and editing. FN: Conceptualization, funding acquisition, investigation, methodology, project administration, supervision, validation, visualization, review and editing. CW: Review and editing. AAA: Review and editing. SB: Conceptualization, funding acquisition, methodology, project administration, review and editing. LD: Review and editing. All authors read and approved the final manuscript
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study received ethical approval from the Institutional Ethics Committee of Fondation Congolaise pour la Recherche Medical No. 013/CIE/FCRM/2018, administrative authorizations from Marien Ngouabi University (No. 247/UMNG.FST.DFD.FD-SBIO) and from each mayor of the study areas. Prior to enrollment, participants were informed in writing and orally about the study, the benefits of the study and on the use of the collected data. Also prior to enrollment in the study, a consent form was signed by the participants or the parent of a minor child (< 18 years of age). An assent form was signed by children aged between 15 to 17 years.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
List of primers used for the nested PCR.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mbama Ntabi, J.D., Lissom, A., Djontu, J.C. et al. Prevalence of non-Plasmodium falciparum species in southern districts of Brazzaville in The Republic of the Congo. Parasites Vectors 15, 209 (2022). https://doi.org/10.1186/s13071-022-05312-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13071-022-05312-9