Abstract
Background
In cluster randomised controlled trials (cRCTs), groups of individuals (rather than individuals) are randomised to minimise the risk of contamination and/or efficiently use limited resources or solve logistic and administrative problems. A major concern in the primary analysis of cRCT is the use of appropriate statistical methods to account for correlation among outcomes from a particular group/cluster. This review aimed to investigate the statistical methods used in practice for analysing the primary outcomes in publicly funded cluster randomised controlled trials, adherence to the CONSORT (Consolidated Standards of Reporting Trials) reporting guidelines for cRCTs and the recruitment abilities of the cluster trials design.
Methods
We manually searched the United Kingdom’s National Institute for Health Research (NIHR) online Journals Library, from 1 January 1997 to 15 July 2021 chronologically for reports of cRCTs. Information on the statistical methods used in the primary analyses was extracted. One reviewer conducted the search and extraction while the two other independent reviewers supervised and validated 25% of the total trials reviewed.
Results
A total of 1942 reports, published online in the NIHR Journals Library were screened for eligibility, 118 reports of cRCTs met the initial inclusion criteria, of these 79 reports containing the results of 86 trials with 100 primary outcomes analysed were finally included. Two primary outcomes were analysed at the cluster-level using a generalized linear model. At the individual-level, the generalized linear mixed model was the most used statistical method (80%, 80/100), followed by regression with robust standard errors (7%) then generalized estimating equations (6%). Ninety-five percent (95/100) of the primary outcomes in the trials were analysed with appropriate statistical methods that accounted for clustering while 5% were not. The mean observed intracluster correlation coefficient (ICC) was 0.06 (SD, 0.12; range, − 0.02 to 0.63), and the median value was 0.02 (IQR, 0.001–0.060), although 42% of the observed ICCs for the analysed primary outcomes were not reported.
Conclusions
In practice, most of the publicly funded cluster trials adjusted for clustering using appropriate statistical method(s), with most of the primary analyses done at the individual level using generalized linear mixed models. However, the inadequate analysis and poor reporting of cluster trials published in the UK is still happening in recent times, despite the availability of the CONSORT reporting guidelines for cluster trials published over a decade ago.
Similar content being viewed by others
Background
Randomised controlled trials (RCTs) are the gold standard in medical and public health research when assessing the safety, clinical and cost-effectiveness of new drugs, new health technologies and new social interventions [1]. Conventionally, in RCTs, individuals are randomised to the experimental arms using either a randomisation or minimisation technique to ensure random allocation and balance in participants characteristics across the experimental arms.
Individually randomised controlled trials (iRCTs) are common, but in practice, this trial design may suffer from the potential contamination of outcomes from participants in the trial. Contamination could occur when participants in proximity are randomised to different experimental arms, there are chances that they will share their experiences of the trial which in turn may influence their outcomes. The cluster randomised controlled trial (cRCT) design can be used to minimise the risks posed by contamination [2, 3].Other rationales for using a cRCT design are maximisation of limited resources, problems with logistics, and administrative convenience [2].
A cRCT is potentially a more powerful design in handling the above-named issues, with groups of individuals (rather than individuals) randomly allocated to the experimental arms, resulting in outcome data that is clustered. Clustered data can also arise from repeated measurements over time on the same individuals in a longitudinal study. Going forward, for simplicity we have interchangeably used “cluster trials” to mean cRCTs.
In cluster trials, outcomes from a cluster/group tend to be more similar than outcomes from any other randomly selected cluster/group. This similarity (or correlation) of outcomes within a cluster is also known as the intracluster correlation. This correlation or non-independence of outcomes violates the assumptions of standard statistical methods used for assessing the effectiveness of an intervention to control, such as t-test, F-test, chi-square test or statistical regression methods used when researchers are also interested in adjusting for the effects of covariates and confounders, such as linear regression, Poisson regression and logistic regression. Standard statistical methods assume that the outcomes from participants in a trial are independent, most of the time this assumption does not hold in cluster trials. Ignoring the dependence among outcomes in the same cluster may lead to reduced standard errors which means—an increased value of the test statistic, smaller P-values and narrower confidence intervals which could increase the risk of false-positive results [1, 3, 4].Campbell and Walters [1] grouped the recognised statistical methods for analysing cluster trials into four broad approaches: (1) cluster-level analysis—using aggregate summary measures for each cluster, (2) individual-level analysis—using regression models with robust standard errors, (3) individual-level analysis—using generalized linear mixed models (random effects models), and (4) individual-level analysis—using a generalized linear model with generalized estimating equations (GEE) to estimate the model coefficients. These broad groupings relate to the way the statistical methods account for correlation among outcomes from the same cluster. The primary objective of this review is to investigate the use of these statistical methods in practice, with a focus on their prevalence.
The Consolidated Standards of Reporting Trials (CONSORT) statement was first published in 1996 to guide the reporting of iRCTs [5]. The extension of the CONSORT statement to cover cluster trials was first suggested in 2001 [6] and was then extended in 2004 [7], based on the revision of the CONSORT statement in 2001. There were still inadequacies in the reporting of iRCTs; hence, in 2010, the previous version of 2001 was updated [9]. The 2012 extension to cover cluster trials was based on this updated CONSORT 2010 statement [8]. These guidelines are meant to aid researchers in the planning, conducting, analysing and reporting of cluster trials to reduce the problems occurring from the poor reporting of cRCTs. Most of the information extracted from each trial reviewed in this study is based on this CONSORT statements extended for cluster trials.
Adherence to the CONSORT reporting guidelines for cluster trials and its impact on the quality of reporting cluster trials has attracted the interest of researchers since it was published [10,11,12]. The adherence to different aspects of the CONSORT statement for cluster trials is usually of interest to researchers, for example a review found that though some aspect of treatment compliance by the participants in the studies are reported, but in general, comprehensive reporting of treatment compliance by participants is poor and inadequate [12]. Another review concluded that despite the availability of the CONSORT reporting guidelines for cluster trials, the reporting of all aspects of sample size calculation was inadequate [11]. Ivers et al. [10] went a step further and investigated adherence to all the new items included in the CONSORT extension for cluster trials; they found that improvement was only evident in few aspects, while in general, the adherence to the CONSORT statement extension for cluster trials was inadequate. The success of any guideline can be measured by the rate of its implementation in practice [13].
One of the justifications for conducting this study was to contribute to the debate in the literature on the adherence to the CONSORT reporting guidelines extension for cluster trials; our focus is on the aspect of the reporting quality of the intracluster correlation coefficient in the cluster trials reviewed. It is justifiable to investigate how well the extended CONSORT reporting guidelines for cluster trials is been implemented in practice, with the aim of recommending how to improve the quality of reporting cluster trials (if necessary).
Established in 2006, the National Institute for Health Research (NIHR) is now the largest funder of public health and social research in England. The NIHR publishes its commissioned research in the online open access NIHR Journals Library which consists of five journals: Public Health Research (PHR; https://www.journalslibrary.nihr.ac.uk/phr/#/), Health Services and Delivery Research (HSDR; https://www.journalslibrary.nihr.ac.uk/hsdr/#/), Efficacy and Mechanism Evaluation (EME; https://www.journalslibrary.nihr.ac.uk/eme/#/), Programme Grants for Applied Research (PGfAR; https://www.journalslibrary.nihr.ac.uk/pgfar/#/) and Health Technology Assessment (HTA; https://www.journalslibrary.nihr.ac.uk/hta/#/). In 2019/2020, the NIHR awarded over £250 million to fund 310 research projects. The NIHR Health Technology Assessment (HTA) programme received the highest amount of about £96.1 million [14].
This review aimed to investigate the prevalence and appropriateness of the statistical methods considered, in the planning and the analyses of cluster trials in practice for publicly funded trials, to evaluate the adherence by researchers to the reporting guidelines stipulated in the CONSORT 2010 statement for cluster trials and the recruitment abilities of cluster randomised controlled trials.
Methods
Search strategy
We manually searched through the online table-of-contents of each of the five NIHR journals, from 1 January 1997 to 15 July 2021 chronologically. The title and abstract of each report were screened to identify if a cluster randomised controlled trial was reported in it. If the title and abstract did not provide sufficient information to determine whether a cluster trial was reported, we had to read through the introduction and methodology chapters of the report to decide if the report should be included.
Trial identification
To identify reports to be included in this review, we followed the procedure described in the “Search strategy” subsection. Apart from the HTA Journal that published its first volume in 1997, the other four journals are recent editions to the NIHR Journals Library. The HSDR, PGfAR and PHR journals published their first volume in 2013 while EME published its first volume in 2014. A search through the NIHR HTA archive from 1 January 1997 to 15 July 2021 showed that the first report of a cluster randomised controlled trial was published in 2000 [15]. However, choosing 1997 as the starting point enabled us to assess the adherence to the CONSORT reporting guidelines before and after the publication of the CONSORT 2010 statement extension for cluster trials. Our interest was solely on trials in which groups of individuals was the unit of randomisation.
One researcher (BCO) conducted the search and extraction of the information while two other independent reviewers (SJW and RMJ) supervised and validated a sample (25%) of the total trials reviewed. If the inclusion of a report was in doubt, this was discussed by all three reviewers until a consensus was reached. The cRCT reports were obtained from the NIHR Journals Library website (https://www.journalslibrary.nihr.ac.uk/#/ date last accessed 9 August 2021) along with any previously published trial paper, protocol paper or trial protocol, where available. For trials that had a published International Standardised Randomised Controlled Trial Number (ISRCTN) number, this was used to check the ISRCTN register of clinical trials for any additional information, a trial website or any previously unobtainable trial reports (cf. http://www.isrctn.com/). The trial reports published in the NIHR Journals Library were was used as the main resource where there were discrepancies in reporting. January 1997 was chosen as a start date for the review as this was the date of publication of the first report in the NIHR Journals Library (in the NIHR HTA Journal).
Eligibility criteria
For a study to be eligible, it must be a cluster randomised controlled trial (involving the randomisation of groups of individuals) or stepped wedge cRCT published in any of the five online NIHR Journals library, from 1 January 1997 to 15 July 2021. Reports on all other study designs were excluded. Pilot and/or feasibility cRCTs were excluded as these have separate specific design and analysis issues including outcomes, sample size and statistical analysis and reporting. Full texts of identified reports were retrieved for further assessment.
Patient and public involvement
Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
Data extraction
Once the NIHR Journals Library reports on cluster trials have been selected for inclusion, necessary information was extracted, using a standardised and piloted data extraction form. When the information of interest was not found, this was indicated with “Not Reported (NR)”; NR indicates that the author(s) did not consider or make use of the method/item of interest or might have used or considered the method/item of interest but did not report it.
The relevant information was extracted and stored in an Excel spreadsheet for further analysis. The information obtained was informed by the review of Walters et al .[16] and the relevant components for cRCTs as stipulated in the CONSORT 2004 statement and its subsequent update. These are the details of the article, information on sample size calculation, recruitment, follow-up, details on clustering, allocation, design/type of trial, primary outcome, primary analysis and results. An additional file presents the list and description (where necessary) of all the items extracted (see Additional file 1). The extracted information was analysed and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [17] guidelines where applicable (see Additional file 2 for the populated PRISMA checklist). In this review, the main outcome was the statistical methods used for analysing the primary outcome(s) of the cRCTs.
Analysis
During the review, we identified that several of the individual reports in the NIHR Journals Library reported the results of two or more separate cRCTs [18,19,20,21,22], as well as the results for two or more primary outcomes per trial [21, 23,24,25,26,27,28,29,30,31].
Descriptive statistics using frequencies and percentages were generated for the levels of all the categorical characteristics of the trials reviewed, while mean, standard deviation, range, median and interquartile range were obtained for continuous outcomes. All analysis was done using an Excel spreadsheet (Microsoft® Excel for Mac, version 16.51) and R studio (Version 1.4.1717).
Results
Trial characteristics
Reports were extracted from the five online NIHR Journals Library published from 1 January 1997 to 15 July 2021. In total, 1942 reports were screened for eligibility, 118 cRCTs reports met the initial inclusion criteria and 3 of the reports were stepped wedge cRCTs [29, 32, 33]. Two reports were excluded because their trials were stopped due to poor recruitment, and only qualitative findings were thereby reported [34, 35. Thirty-seven other pilot/feasibility cRCTs were further excluded. Seventy-nine reports containing the results of 86 cluster trials were included. Five reports contained the results of multiple cluster trials (4 reports of 2 cRCTs each and 1 report included 4 cRCTs) 19,20,21,22,23. A total of 100 primary outcomes (11 trials in 10 reports had multiple primary outcomes) were assessed in this review. The search and selection processes are presented in Fig. 1. The list and URL of all included reports are available in a separate (Additional file 3).
Table 1 summarises the characteristics of the 86 trials included in this review. Most of the trials reviewed were conducted in different regions but solely within the United Kingdom (UK) except for Simmons et al. [35] which involved other European locations. The trials design used was mostly a parallel-group cluster trial that involved a direct comparison between intervention and control experimental arms (85%, 73/86), and this was mostly done using two experimental arms for comparison (80%) (Table 1).
Statistical methods used for analysing cluster trials
Of the 100 primary outcomes reported in the 86 trials, the data type of most of the primary outcomes was continuous (63%, 63/100), followed by binary outcomes (28%), and then counts (5%), time-to-event [33, 36] and percentage [37, 38] were the least (2%, respectively). In the description of the statistical analysis of the primary outcomes of the cRCTs, a variety of phrases were used to describe the multilevel regression methods used to account for clustering, such as generalized linear mixed-model, two-level hierarchical model, mixed-effects, multilevel regression and two-level heteroscedastic linear regression model; hence, we used a generic name “generalized linear mixed model (GLMM)” to cover all the multilevel regression methods.
Of the 100 analysed primary outcomes in the trials, 80% (80/100) used a GLMM to account for clustering, 7% used regression methods with robust standard errors and 6% used generalized estimating equations (GEE) to estimate the regression coefficients of the models. Most of these analyses were carried out using individual participant outcomes. Only 2 trials used aggregated cluster level outcomes as data points in their primary analyses [31, 38]. The different statistical methods used to account for the clustering of outcomes at the analysis phase are presented in Table 2.
Overall, 95% of the primary analyses used recognised statistical methods to adjust for clustering in their analyses, 5% did not; they ignored clustering and used standard statistical methods such as the chi-square test, standard linear, logistic and Poisson regressions [15, 29, 39,40,41]. Continuous outcomes were dichotomised in some studies to enable the use of logistic regression. The trial hypothesis was “superiority” in all the cluster trials except for Heller et al. [42] which was a non-inferiority trial. Table 2 also shows that most trials recruited and followed up the cohort of participants until the end of the trial; this often leads to missing data due to loss to follow-up (88%, 76/86).
Although 92% of the trials acknowledged the occurrence of missing data, most of them went ahead to analyse only complete cases (84%). Imputation of missing outcome data was done for just 16% of the trials reviewed [20, 28, 30, 43,44,45,46,47,48,49,50,51,52,53].
Planned recruitment targets of participants and clusters
Recruitment characteristics are summarised in Table 3, with 67% (58/86) of cRCTs achieving their planned final individual participant recruitment target and 87% of the trials achieving ≥ 80% of their final individual participant recruitment target; this indicates successful recruitment to final targeted sample size for most of the cluster trials. This also applies to the original cluster recruitment target, with 89% of the trials successfully recruiting (and randomising) ≥ 80% of their original targeted number of clusters.
Cluster and sample size characteristics
In Table 4, the cluster and sample size characteristics of the included trials are summarised and presented. The design effect if not reported was calculated using the formula, 1 + (m − 1) × ICC or 1 + [(CV2 + 1)m − 1] × ICC for equal and unequal/varying cluster sizes respectively, where CV is the coefficient of variation, and m is the average cluster size. This is possible if the ICC and cluster size were reported. The median number of clusters randomised was 44 (IQR, 25–74), the minimum was 7 clusters randomised [42], and the maximum was 922 clusters randomised, in a trial of which households were the clusters [55]. A reasonable proportion of the randomised clusters were retained throughout the follow-up period, with a median of 43 clusters (IQR, 25–69) included in the analysis which is quite close to the number of clusters randomised. Also, for the number of subjects recruited/randomised, the median was 1184 (IQR, 597–3653), while the median number of subjects included in the analyses was 870 (IQR, 441–2356).
In the planning stage, 38% (33/86) of the planned ICCs used in the sample size calculations fell in the 0.03–0.05 range. The median planned ICC in the sample size calculation was 0.05 (IQR, 0.026–0.07). The observed ICCs from the analysed primary outcomes in the trials has a median value of approximately 0.02 (IQR, 0.001–0.060) with most of the reported ICCs occurring in the − 0.02 to 0.02 range (Table 4). After excluding two trials that were analysed at the cluster-level, we found that 42% (42/100) of the observed ICC from the primary analyses of the primary outcomes were not reported. Thirty-one percent of the observed ICC was not reported before the publication of CONSORT 2010 statement compared to 44% after its publication (Table 4). One study carried out a pair matched randomisation using a minimisation technique; however, they analysed their primary outcomes at the individual-level [28]. Pair matching of clusters reduces the population heterogeneity at the cluster level which could result in a negligible ICC from the analysed primary outcome and also improve the statistical efficiency of the trial [8, 10].
Not reporting the observed ICC for the analysed primary outcomes contradicts the CONSORT 2010 reporting guidelines for cluster trials, which recommends that authors should report “a coefficient of intracluster correlation (ICC or k) for each primary outcome”. The minimum observed ICC value appears to be an outlier (− 0.02) and was found in Heller et al. [42].
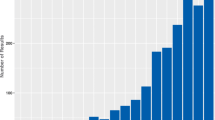
Figure 2 shows the trend and comparison of the practice of not reporting the observed ICCs for the analysed primary outcomes, before and after CONSORT 2010 statement. No observable trend appears to be present in Fig. 2. Before the publication of CONSORT 2010 guidelines for cRCT, the years that trials were carried out, 2003, 2005 and 2011 also recorded non-reporting of the observed ICCs for the analysed primary outcomes (20%, 100% and 50%, respectively). However, after the publication of the CONSORT 2010 statement, almost in each year aside 2013, some of the observed ICCs for the analysed primary outcomes were not reported, ranging from 28 to 90%. From Table 5, a higher proportion still did not report their observed ICCs from analysed primary outcomes after the publication of the CONSORT 2010 statement compared to the proportion that did not before its publication (44% vs 31%).
Discussion
This review was carried out to investigate the statistical methods used for analysing cluster randomised controlled trials in practice; to this end, we surveyed publicly funded cluster trials funded by the National Institute for Health Research.
Most of the trials used appropriate/recognised statistical methods to adjust for clustering in the main analyses of the primary outcomes from the trials (95%, 95/100). Few of the outcomes (and trials) 5% ignored clustering and used standard statistical methods that assumed independence among outcomes from participants in a cluster. This approach is not reccommended as it could lead to smaller standard errors and consequently, an increased value of the test statistic, smaller P-values, narrower confidence interval and possibly increase the type I error rate compared with the statistical methods that allow for clustering. If this happens to be the case, misleading conclusions and decisions will be made; this could have detrimental effects on public health.
The generalized linear mixed model (GLMM) was the most popular choice in adjusting for clustering and was more popular than GEE (80% vs 6%). For the GLMMs with two levels of clustering (trial participants nested within clusters), the cluster unit is usually incorporated as a random intercept to account for clustering. Where the primary outcome was measured more than once or the level of clustering is more than two levels, statistical models with random intercept and the random slope were used. Four trials that used the GEE method assumed an exchangeable working correlation structure in the primary analysis [18, 56,57,58], while 1 trial did not report the correlation structure that was assumed [42].
Fiero et al. [59] conducted a systematic review that focused more on the handling of missing data than on the statistical methods used for analysing cluster trials and found similar results to ours. They found that most of the trials analysed their primary outcome using GLMMs, and the cluster unit were modelled as the random intercept to account for clustering. Also, they found that all 14 (100%) of the trials that used GEE to account for clustering assumed an exchangeable correlation structure, which is similar to the findings of this current review (5/5, 100%; one study did not report their correlation structure [42]). Overall, they found that a lower proportion 79% (68/88) of the trials accounted for clustering compared to our review which observed a higher proportion 95% (95/100).
It is worth noting that while the use of appropriate statistical methods is high, none of the trials considered the recent potentially improved statistical methods developed in other study designs where clustered data do arise, such as the quadratic inference function (QIF), the alternating logistic regression (ALR) and the targeted maximum likelihood (tMLE). These recent methods are improvements over the standard GEE method for estimating the regression coefficients in the model [60]. The results of our study revealed that the number of clusters randomised in a cRCT could be as large as 922 in a study where the clusters were households [55] and as few as 7 clusters [42]. This result is different from the findings of Arnup et al. [61] where they focused on cluster randomised cross-over trials, one reason for choosing a cross-over design is if the number of the prospective clusters is small. In their study, the lowest number of clusters randomised was 2 while 25% of the number of clusters randomised was below 4.
In practice, active controls are mostly used when assessing the effect of non-pharmacological interventions (86/86, 100%). As revealed in our results, most times, it is impractical to conduct studies where the participants are blinded to the experimental arms they are allocated to. However, to some extent, masking is achieved by blinding either the person randomising the subjects, the assessor and/or the statistician that will analyse the data. To carry out a robust cluster trial, it is preferable to conduct an internal pilot/feasibility study (84%, 72/86) to assess the viability of the items/phases of the trial, such as the data collection tools, the understanding (and safety) and acceptance of the intervention by the participants and the ability to recruit to target before proceeding with the main trial.
Recruiting participants (for clusters, see Table 3) into a trial seems not to be a problem in cluster trials, particularly when compared to iRCTs (see Table 6). In 87% of the cluster trials, researchers were able to recruit ≥ 80% of their final planned participant recruitment targets. This result also applies to the number of clusters recruited/randomised, where 76% of the trials were able to recruit ≥ 80% of their planned clusters recruitment target (see Table 6).
In Table 6, we compared the ability of cRCTs and iRCTs to recruit to their target the number of participants. In terms of recruiting to 100% of the original participant target, cluster trials seem more successful than iRCTs (66% vs 55%). This is confirmed by the fact that in cluster trials, the originally planned sample sizes are rarely revised (24%) and tend to be revised upward (57%, 12/21) rather than downward (43%). When compared to iRCTs, the number (and percentage) of upward revisions were higher in cluster trials (57% vs 36%). Even with the most upward revisions, cluster trial recruitment periods are rarely extended to meet up with recruitment targets compared to iRCTs (13%, 11/86 vs 54%, 65/122).
We also found that in practice the completely randomised parallel-group cluster trial design is the most used design involving two experimental arms in its simplest form. This cluster design is easy to set up, implement and analyse. Our results indicated that all the trials reviewed, except one, were superiority trials involving contrasting experimental arms. For the sample size calculation, our results indicated that the median assumed ICC value, used in the calculation, was 0.05, while the average was 0.065. However, we found observed that the ICC assumed in the sample size calculation could be as low as 0.0002 (Table 4). Our results also indicated that a disappointing trend of not reporting the observed ICC for each primary outcome is happening. About 4 out of 10 of the observed ICCs from the analysed primary outcomes in cRCTs are not being reported. The implication of not reporting the ICC cannot be overemphasised; the ICC is an important item in designing/planning future cluster trials as it is needed for sample size calculation. It is reasonable to make it available for researchers planning to undertake similar study. The importance of reporting the ICC was reemphasised by the development of a framework specifying how and what should be reported in association with the ICC to facilitate understanding and the planning of future cluster trials [62].
Surprisingly, this occurs more in recent times despite the availability and publicity of the CONSORT 2010 statement extension for cluster trials, although 2005 had the highest percentage of this disappointing practice (100%), but with only two analysed primary outcomes recorded.
It is worth noting that this was also after the publication of the CONSORT 2004 statement [8] extension for cluster trials. Ivers et al. [11] assessed the impact of the CONSORT 2004 statement extension for cluster trials on quality of reporting and study methodology, and one of the criteria compared was the “reporting of an estimated intracluster correlation”. They found only 18% of the 300 manuscripts reported an ICC estimate and 22% vs 14% before and after CONSORT 2004 statement respectively. This result indicated a decline in the practice of reporting indicated a decline in the practice of reporting the observed ICC which is similar to our current study. We found a 13% increase (change in non-adherence before to after CONSORT 2010) in non-adherence to the CONSORT reporting guidelines with regards to reporting the observed ICC for each primary outcome analysed, using CONSORT 2010 statement as the basis for comparison. CONSORT statements extensions for cluster trials are published to facilitate improved quality reporting of cluster trials. If used properly, they are supposed to help in the understanding, assessing and replicating of cluster trials by all stakeholders of clinical trials. Hence, all authors intending to write up the report for their cluster trial(s) should make good use of the updated CONSORT 2010 statement.
The observations made in this review is that in practice there are important issues in cRCTs that are still being ignored or handled inadequately or not reported.
Firstly, missing data is not adequately handled most of the time. The majority (79/86, 92%) of the studies reviewed acknowledged the existence of missing data, which is obvious due to inevitable loss to follow-up in a closed cohort follow-up study; however, the majority still went ahead to analyse only available observations (84%). To assess the robustness of the findings in the trials, especially when missing data was not technically handled, most researchers resorted to conducting sensitivity analysis. However, if they had handled the problem of missing data technically (e.g., using statistical imputations) in the original analysis, it could have improved the inferences made in the study.
Secondly, there appears to be a slow uptake of improved statistical methods developed in other study designs where clustered data can arise, such as the QIF, tMLE and ALR that are potentially better in certain situations than the popular statistical methods used currently for analysing cluster trials. It would be ideal if these methods are publicised by methodologists of cluster trials so that researchers can use them when necessary to make optimal inferences [60].
Limitation
We acknowledge that searching and retrieving cluster trial reports from one source could lead to publication bias. We optimized the study by including all cluster trials instead of a random sample, and the reports published in the NIHR Journals Library were also published independently as result articles in other journals; hence, reports included in this review represent a collection of articles from several journals independent of NIHR Journals Library.
Conclusion and recommendation
In practice, most of the publicly funded cluster trials adjusted for clustering using an appropriate/recognised statistical method with most of the primary analyses done at the individual level using generalized linear mixed models. However, the inadequate analysis and poor reporting of cluster trials, particularly not reporting the observed ICC for the analysed primary outcomes is still happening in recent times despite the availability of the CONSORT reporting guidelines extension for cluster trials published over a decade ago. One way of addressing this issue is to encourage journal editors and peer reviewers to insist that authors should adhere to CONSORT reporting guidelines for cluster trials when submitting their manuscripts. This review will serve as a reference tool in conducting systematic reviews of statistical methods used in practice and statistical methods available in the literature for analysing cluster trials.
Patient and public involvement
Patients and/or the public were not involved in the design, conduct, reporting or dissemination plans of this research.
Availability of data and materials
The information extracted in this review is based on published trials in the NIHR Journals library. The data extracted from the NIHR Journals Library supporting the finding of this study is available upon reasonable request from the corresponding author.
Abbreviations
- cRCT:
-
Cluster randomised controlled trial
- CONSORT:
-
Consolidated standards of reporting trials
- NIHR:
-
National institute for health research
- SD:
-
Standard deviation
- ICC:
-
Intracluster correlation coefficient
- IQR:
-
Interquartile range
- RCT:
-
Randomised controlled trial
- iRCT:
-
Individually randomised controlled trial
- GEE:
-
Generalized estimating equation
- GLMM:
-
Generalized linear mixed model
- QIF:
-
Quadratic inference function
- tMLE:
-
Targeted maximum likelihood
- ALR:
-
Alternating logistic regression
- PHR:
-
Public health research
- HSDR:
-
Health services and delivery research
- EME:
-
Efficacy and mechanism evaluation
- PGfAR:
-
Programme grants for applied research
- HTA:
-
Health technology assessment
- NR:
-
Not reported
References
Campbell MJ, Walters SJ. How to design, analyse and report cluster randomised trials in medicine and health related research: Wiley; 2014. https://doi.org/10.1002/9781118763452.
Christie J, O’Halloran P, Stevenson M. Planning a cluster randomized controlled trial. Nurs Res. 2009;58(2):128–34. https://doi.org/10.1097/NNR.0b013e3181900cb5.
Wears RL. Advanced statistics: statistical methods for analyzing cluster and cluster-randomized data. Acad Emerg Med. 2002;9(4):330–41. https://doi.org/10.1197/aemj.9.4.330.
Bland JM. Cluster randomised trials in the medical literature: two bibliometric surveys. BMC Med Res Methodol. 2004;4(1):2–7. https://doi.org/10.1186/1471-2288-4-21.
Begg C, Cho M, Eastwood S, et al. Improving the quality of reporting of randomized controlled trials: the CONSORT statement. J Am Med Assoc. 1996;276(8):637–9. https://doi.org/10.1001/jama.276.8.637.
Elbourne DR, Campbell MK. D.R. E. Extending the CONSORT statement to cluster randomized trials: For discussion. Stat Med. 2001;20(3):489–96. https://doi.org/10.1002/1097-0258(20010215)20:3<489::AID-SIM806>3.0.CO;2-S
Campbell MK, Elbourne DR, Altman DG. CONSORT statement: extension to cluster randomised trials. BMJ. 2004;328(7441):702 LP–708. https://doi.org/10.1136/bmj.328.7441.702.
Campbell MK, Piaggio G, Elbourne DR, Altman DG. Consort 2010 statement: extension to cluster randomised trials. BMJ Online. 2012;345(7881):1–21. https://doi.org/10.1136/bmj.e5661.
Schulz KF, Altman DG, Moher D, the CONSORT Group. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMC Med. 2010;8(1):18. https://doi.org/10.1186/1741-7015-8-18.
Ivers NM, Taljaard M, Dixon S, Bennett C, McRae A, Taleban J, et al. Impact of CONSORT extension for cluster randomised trials on quality of reporting and study methodology: review of random sample of 300 trials, 2000-8. BMJ Online. 2011;343(7827):1–14. https://doi.org/10.1136/bmj.d5886.
Rutterford C, Taljaard M, Dixon S, Copas A, Eldridge S. Reporting and methodological quality of sample size calculations in cluster randomized trials could be improved: a review. J Clin Epidemiol. 2015;68(6):716–23. https://doi.org/10.1016/j.jclinepi.2014.10.006.
Agbla SC, DiazOrdaz K. Reporting non-adherence in cluster randomised trials: a systematic review. Clin Trials. 2018;15(3):294–304. https://doi.org/10.1177/1740774518761666.
Gogtay NJ. Reporting of randomized controlled trials: will it ever improve? Perspect Clin Res. 2019;10(2):49–50. https://doi.org/10.4103/picr.PICR_11_19.
NIHR. National Institute for Health Research. Annu Rep. 2019;(December):1–50.
Turner J, Nicholl J, Webber L, Cox H, Dixon S, Yates D. A randomised controlled trial of prehospital intravenous fluid. Health Technol Assess Winch Engl. 2000;4(31):1–57.
Walters SJ, Dos Anjos Henriques-Cadby IB, Bortolami O, et al. Recruitment and retention of participants in randomised controlled trials: a review of trials funded and published by the United Kingdom Health Technology Assessment Programme. BMJ Open. 2017;7(3):1–10. https://doi.org/10.1136/bmjopen-2016-015276.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. The BMJ. 2021;372. https://doi.org/10.1136/bmj.n71.
Kitchener HC, Gittins M, Rivero-Arias O, et al. A cluster randomised trial of strategies to increase cervical screening uptake at first invitation (STRATEGIC). Health Technol Assess. 2016;20(68). https://doi.org/10.3310/hta20680.
Christian MS, EL Evans C, Cade JE. Does the Royal Horticultural Society Campaign for School Gardening increase intake of fruit and vegetables in children? Results from two randomised controlled trials. Public Health Res. 2014;2(4):1–162. https://doi.org/10.3310/phr02040.
Raine R, Atkin W, Von Wagner C, et al. Testing innovative strategies to reduce the social gradient in the uptake of bowel cancer screening: a programme of four qualitatively enhanced randomised controlled trials. Programme Grants Appl Res. 2017;5(8):338–02. https://doi.org/10.3310/pgfar05080.
Foy R, Willis T, Glidewell L, et al. Developing and evaluating packages to support implementation of quality indicators in general practice: the ASPIRE research programme, including two cluster RCTs. Programme Grants Appl Res. 2020;8(4). https://doi.org/10.3310/pgfar08040.
Ballard C, Orrell M, Moniz-Cook E, et al. Improving mental health and reducing antipsychotic use in people with dementia in care homes: the WHELD research programme including two RCTs. Programme Grants Appl Res. 2020;8(6). https://doi.org/10.3310/pgfar08060.
Ramsay CR, Clarkson JE, Duncan A, Lamont TJ, Heasman PA, Boyers D, et al. Improving the quality of dentistry (IQuaD): a cluster factorial randomised controlled trial comparing the effectiveness and cost-benefit of oral hygiene advice and/or periodontal instrumentation with routine care for the prevention and management of perio. Health Technol Assess. 2018;22(38):vii–143. https://doi.org/10.3310/hta22380.
MacArthur C, Winter HR, Bick DE, Lilford, RJ, Lancashire RJ, Knowles H, et al. Redesigning postnatal care: a randomised controlled trial of protocol-based midwifery-led care focused on individual women’s physical and psychological health needs.Health Technol Assess. 2003;7(37):1–98.
Lawlor DA, Kipping RR, Anderson EL, Howe LD, Chittleborough CR, Moure-Fernandez A, et al. Active for Life Year 5: a cluster randomised controlled trial of a primary school-based intervention to increase levels of physical activity, decrease sedentary behaviour and improve diet. Public Health Res. 2016;4(7):1–156. https://doi.org/10.3310/phr04070.
Sumnall H, Agus A, Cole J, Doherty P, Foxcroft D, Harvey S, et al. Steps Towards Alcohol Misuse Prevention Programme (STAMPP): a school- and community-based cluster randomised controlled trial. Public Health Res. 2017;5(2):1–154. https://doi.org/10.3310/phr05020.
Connolly P, Miller S, Kee F, Sloan S, Gildea A, McIntosh E, et al. A cluster randomised controlled trial and evaluation and cost-effectiveness analysis of the Roots of Empathy schools-based programme for improving social and emotional well-being outcomes among 8- to 9-year-olds in Northern Ireland. Public Health Res. 2018;6(4):1–108. https://doi.org/10.3310/phr06040.
Thompson DG, O’Brien S, Kennedy A, Rogers A, Whorwell P, Lovell K, et al. A randomised controlled trial, cost-effectiveness and process evaluation of the implementation of self-management for chronic gastrointestinal disorders in primary care, and linked projects on identification and risk assessment. Programme Grants Appl Res. 2018;6(1):1–154. https://doi.org/10.3310/pgfar06010.
Wykes T, Csipke E, Rose D, Craig T, McCrone P, Williams P, et al. Patient involvement in improving the evidence base on mental health inpatient care: the PERCEIVE programme. Programme Grants Appl Res. 2018;6(7):1–182. https://doi.org/10.3310/pgfar06070.
Gaughran F, Stahl D, Patel A, et al. A health promotion intervention to improve lifestyle choices and health outcomes in people with psychosis: a research programme including the IMPaCT RCT. Programme Grants Appl Res. 2020;8(1). https://doi.org/10.3310/pgfar08010.
Wright J, Lawton R, O’Hara J, Armitage G, Sheard L, Marsh C, et al. Improving patient safety through the involvement of patients: development and evaluation of novel interventions to engage patients in preventing patient safety incidents and protecting them against unintended harm. Programme Grants Appl Res. 2016;4(15):1–296. https://doi.org/10.3310/pgfar04150.
Snooks H, Bailey-Jones K, Burge-Jones D, Dale J, Davies J, Evans B, et al. Predictive risk stratification model: a randomised stepped-wedge trial in primary care (PRISMATIC). Health Serv Deliv Res. 2018;6(1):1–164. https://doi.org/10.3310/hsdr06010.
Peden CJ, Stephens T, Martin G, Kahan BC, Thomson A, Everingham K, et al. A national quality improvement programme to improve survival after emergency abdominal surgery: the EPOCH stepped-wedge cluster RCT. Health Serv Deliv Res. 2019;7(32):1–96. https://doi.org/10.3310/hsdr07320.
Speed C, Heaven B, Adamson A, et al. LIFELAX – diet and LIFEstyle versus LAXatives in the management of chronic constipation in older people : randomised controlled trial. 2010;14(52). https://doi.org/10.3310/hta14520.
Simmons RK, Borch-Johnsen K, Lauritzen T, Rutten GEHM, Sandbæk A, van den Donk M, et al. A randomised trial of the effect and cost-effectiveness of early intensive multifactorial therapy on 5-year cardiovascular outcomes in individuals with screen-detected type 2 diabetes: the Anglo–Danish–Dutch Study of Intensive treatment in people with scr. Health Technol Assess. 2016;20(64):1–86. https://doi.org/10.3310/hta20640.
Davies MJ, Gray LJ, Ahrabian D, Carey M, Farooqi A, Gray A, et al. A community-based primary prevention programme for type 2 diabetes mellitus integrating identification and lifestyle intervention for prevention: a cluster randomised controlled trial. Programme Grants Appl Res. 2017;5(2):1–290. https://doi.org/10.3310/pgfar05020.
Priebe S, Bremner SA, Lauber C, Henderson C, Burns T. Financial incentives to improve adherence to antipsychotic maintenance medication in non-adherent patients: a cluster randomised controlled trial. Health Technol Assess. 2016;20(70):v-121. https://doi.org/10.3310/hta20700.
Cameron ST, Glasier A, McDaid L, Radley A, Patterson S, Baraitser P, et al. Provision of the progestogen-only pill by community pharmacies as bridging contraception for women receiving emergency contraception: the Bridge-it RCT. Health Technol Assess Winch Engl. 2021;25(27):1–92. https://doi.org/10.3310/hta25270.
Morgan K, Dixon S, Mathers N, Thompson J, Tomeny M. Psychological treatment for insomnia in the regulation of long-term hypnotic drug use. Health Technol Assess. 2004;8(8). https://doi.org/10.3310/hta8080.
Gates S, Lall R, Quinn T, Deakin CD, Cooke MW, Horton J, et al. Prehospital randomised assessment of a mechanical compression device in out-of-hospital cardiac arrest (PARAMEDIC): a pragmatic, cluster randomised trial and economic evaluation. Health Technol Assess. 2017;21(11):1–175. https://doi.org/10.3310/hta21110.
Perez J, Russo DA, Stochl J, et al. Understanding causes of and developing effective interventions for schizophrenia and other psychoses. Programme Grants Appl Res. 2016;4(2). https://doi.org/10.3310/pgfar04020.
Heller S, Lawton J, Amiel S, Cooke D, Mansell P, Brennan A, et al. Improving management of type 1 diabetes in the UK: the Dose Adjustment For Normal Eating (DAFNE) programme as a research test-bed. A mixed-method analysis of the barriers to and facilitators of successful diabetes self-management, a health economic analys. Programme Grants Appl Res. 2014;2(5):1–188. https://doi.org/10.3310/pgfar02050.
Salisbury C, Man MS, Chaplin K, Mann C, Bower P, Brookes S, et al. A patient-centred intervention to improve the management of multimorbidity in general practice: the 3D RCT. Health Serv Deliv Res. 2019;7(5):1–238. https://doi.org/10.3310/hsdr07050.
Mouncey PR, Wade D, Richards-Belle A, Sadique Z, Wulff J, Grieve R, et al. A nurse-led, preventive, psychological intervention to reduce PTSD symptom severity in critically ill patients: the POPPI feasibility study and cluster RCT. Health Serv Deliv Res. 2019;7(30):1–174. https://doi.org/10.3310/hsdr07300.
Killaspy H, King M, Holloway F, Craig TJ, Cook S, Mundy T, et al. The Rehabilitation Effectiveness for Activities for Life (REAL) study: a national programme of research into NHS inpatient mental health rehabilitation services across England. Programme Grants Appl Res. 2017;5(7):1–284. https://doi.org/10.3310/pgfar05070.
Moniz-Cook E, Hart C, Woods B, Whitaker C, James I, Russell I, et al. Challenge Demcare: management of challenging behaviour in dementia at home and in care homes – development, evaluation and implementation of an online individualised intervention for care homes; and a cohort study of specialist community mental health car. Programme Grants Appl Res. 2017;5(15):1–290. https://doi.org/10.3310/pgfar05150.
Surr CA, Holloway I, Walwyn REA, Griffiths AW, Meads D, Kelley R, et al. Dementia care mappingTM to reduce agitation in care home residents with dementia: the epic cluster rct. Health Technol Assess. 2020;24(16):1–174. https://doi.org/10.3310/hta24160.
Lamb SE, Williams MA, Williamson EM, Gates S, Withers EJ, Mt-Isa S, et al. Managing injuries of the neck trial (mint): a randomised controlled trial of treatments for whiplash injuries. Health Technol Assess. 2012;16(49):1–141. https://doi.org/10.3310/hta16490.
Iliffe S, Kendrick D, Morris R, Masud T, Gage H, Skelton D, et al. Multicentre cluster randomised trial comparing a community group exercise programme and home-based exercise with usual care for people aged 65 years and over in primary care. Health Technol Assess. 2014;18(49):1–105. https://doi.org/10.3310/hta18490.
Snooks HA, Anthony R, Chatters R, Dale J, Fothergill R, Gaze S, et al. Support and assessment for fall emergency referrals (SAFER) 2: a cluster randomised trial and systematic review of clinical effectiveness and cost-effectiveness of new protocols for emergency ambulance paramedics to assess older people following a fall wi. Health Technol Assess. 2017;21(13):1–218. https://doi.org/10.3310/hta21130.
Heller S, White D, Lee E, Lawton J, Pollard D, Waugh N, et al. A cluster randomised trial, cost-effectiveness analysis and psychosocial evaluation of insulin pump therapy compared with multiple injections during flexible intensive insulin therapy for type 1 diabetes: The REPOSE Trial. Health Technol Assess. 2017;21(20):1–277. https://doi.org/10.3310/hta21200.
Ring H, Howlett J, Pennington M, et al. Training nurses in a competency framework to support adults with epilepsy and intellectual disability: the EpAID cluster RCT. Health Technol Assess. 2018;22(10). https://doi.org/10.3310/hta22100.
Humphrey N, Hennessey A, Lendrum A, Wigelsworth M, Turner A, Panayiotou M, et al. The PATHS curriculum for promoting social and emotional well-being among children aged 7–9 years: a cluster RCT. Public Health Res. 2018;6(10):1–116. https://doi.org/10.3310/phr06100.
Gulliford MC, Juszczyk D, Prevost AT, Soames J, McDermott L, Sultana K, et al. Electronically delivered interventions to reduce antibiotic prescribing for respiratory infections in primary care: cluster RCT using electronic health records and cohort study. Health Technol Assess. 2019;23(11):11–70. https://doi.org/10.3310/hta23110.
Harris T, Kerry S, Victor C, Iliffe S, Ussher M, Fox-Rushby J, et al. A pedometer-based walking intervention in 45- to 75-year-olds, with and without practice nurse support: The PACE-UP three-arm cluster RCT. Health Technol Assess. 2018;22(37):1–273. https://doi.org/10.3310/hta22370.
Morrell CJ, Warner R, Slade P, et al. Psychological interventions for postnatal depression: cluster randomised trial and economic evaluation. The PoNDER trial. Health Technol Assess. 2009;13(30). https://doi.org/10.3310/hta13300.
Dormandy E, Bryan S, Gulliford MC, Roberts TE, Ades AE, Calnan M, et al. Antenatal screening for haemoglobinopathies in primary care: a cohort study and cluster randomised trial to inform a simulation model. The screening for haemoglobinopathies in first trimester (SHIFT) trial. Health Technol Assess. 2010;14(20):1–160. https://doi.org/10.3310/hta14200.
Harrington DM, Davies MJ, Bodicoat D, Charles JM, Chudasama YV, Gorely T, et al. A school-based intervention (‘Girls Active’) to increase physical activity levels among 11- to 14-year-old girls: cluster RCT. Public Health Res. 2019;7(5):1–162. https://doi.org/10.3310/phr07050.
Fiero MH, Huang S, Oren E, Bell ML. Statistical analysis and handling of missing data in cluster randomized trials: a systematic review. Trials. 2016;17(1):1–10. https://doi.org/10.1186/s13063-016-1201-z.
Turner EL, Li F, Gallis JA, Prague M, Murray DM. Review of recent methodological developments in group-randomized trials: Part 1 - Design. Am J Public Health. 2017;107(6):907–15. https://doi.org/10.2105/AJPH.2017.303706.
Arnup SJ, Forbes AB, Kahan BC, Morgan KE, McKenzie JE. Appropriate statistical methods were infrequently used in cluster-randomized crossover trials. J Clin Epidemiol. 2016;74:40–50. https://doi.org/10.1016/j.jclinepi.2015.11.013.
Campbell MK, Grimshaw JM, Elbourne DR. Intracluster correlation coefficients in cluster randomized trials: empirical insights into how should they be reported. BMC Med Res Methodol. 2004;5(1):1–5. https://doi.org/10.1186/1471-2288-4-9.
Funding
Offorha is sponsored by the Nigerian Tertiary Education Trust Fund (TETFund). Prof. Walters, and Dr. Jacques, received funding across various projects by NIHR. Prof. Walters is a National Institute for Health Research (NIHR) Senior Investigator (NF-SI-0617-10012) supported by the NIHR for this research project. The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR, NHS or the UK Department of Health and Social Care. These organisations had no role in the study design; in the collection, analysis, and interpretation of the data; in the writing of the report; or in the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
BCO conceptualised the idea for this review, prepared the data collection form, carried out the search and data extraction, analysed the data, wrote the first draft of the manuscript and revised and edited the manuscript. SJW and RMJ conceptualised the idea for this review, prepared the data collection tool, supervised and validated the search and extraction of the data, and critically revised and edited the manuscript. The authors read and approved the final manuscript.
Authors’ information
BCO is a PhD candidate in Medical Statistics. SJW is a Professor of Medical Statistics. RMJ is a Senior lecturer in Medical Statistics.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The information extracted in this review is based on published NIHR trials where ethics approvals were obtained by the original trial teams. This review does not involve recruiting new participants or analysing individual participants, and the original participants cannot be identified from this review.
Consent for publication
This review does not involve recruiting new participants or analysing individual participants’ data. Individual informed consent was obtained to take part in the original trials by primary investigators.
Competing interests
The PhD study of Offorha is financially sponsored by the Nigerian Tertiary Education Trust Fund (TETFund) (Grant No. TETF/ES/UNIV/UTURU/TSA/2019). Prof. Walters and Dr. Jacques received funding across various projects by NIHR. Prof. Walters is a National Institute for Health Research (NIHR) Senior Investigator (NF-SI-0617-10012) supported by the NIHR for this research project. The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR, NHS or the UK Department of Health and Social Care. These organisations had no role in the study design; in the collection, analysis, and interpretation of the data; in the writing of the report; or in the decision to submit the paper for publication.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Data collection tool (NIHR).
Additional file 2.
PRISMA 2020 checklist.
Additional file 3.
List of included reports.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Offorha, B.C., Walters, S.J. & Jacques, R.M. Statistical analysis of publicly funded cluster randomised controlled trials: a review of the National Institute for Health Research Journals Library. Trials 23, 115 (2022). https://doi.org/10.1186/s13063-022-06025-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-022-06025-1