Abstract
Background
Cesarean section is an important surgical procedure, when normal vaginal delivery imposes a risk to mother and/or baby. The World Health Organization states the ideal rate for Cesarean section to be between 10 and 15% of all births. In recent decades, the rate has been increased dramatically worldwide. This paper explains the protocol of a randomized controlled trial that aims to compare the effect of “motivational interviewing” and “information, motivation, and behavioral skills” counseling interventions on choosing mode of delivery in pregnant women.
Methods
A four-armed, parallel-design randomized controlled trial will be conducted on pregnant women. One hundred and twenty women will be randomly assigned to four groups including three intervention groups and one control group. The intervention groups included the following: (1) motivational interviewing; (2) face-to-face information, motivation, and behavioral skills model; and (3) information, motivation, and behavioral skills model provided using a mobile application. The inclusion criteria include being literate, being in gestational age from 24 to 32 weeks, being able to speak Persian, having no complications in the current pregnancy, having no indications for Cesarean section, and having enough time to participate in the intervention. The primary outcome of the study is the mode of delivery. The secondary outcomes are women’s intention to undergo Cesarean section and women’s self-efficacy.
Discussion
The interventions of this protocol have been programmed to reduce unnecessary Cesarean sections. Findings may contribute to a rise in normal vaginal delivery, and the effective intervention may be extended for use in national Cesarean section plans.
Trial registration
Iran Randomized Clinical Trial Center IRCT20151208025431N7. Registered on December 07, 2018.
Similar content being viewed by others
Administrative information
The order of the items has been modified to group similar items (see http://www.equator-network.org/reporting-guidelines/spirit-2013-statement-defining-standard-protocol-items-for-clinical-trials/).
Title {1} | Effect of “motivational interviewing” and “information, motivation, and behavioral skills” counseling interventions on choosing the mode of delivery in pregnant women: a study protocol for a randomized controlled trial |
Trial registration {2a and 2b}. | This study has been registered in Iran Randomized Clinical Trial Center (IRCT20151208025431N7). Registered December 07, 2018. |
Protocol version {3} | V2.0, 1st December 2019. |
Funding {4} | This study is being financially supported by Tehran University of Medical Sciences (TUMS) and Iran National Science Foundation (INSF). |
Author details {5a} | Mahboubeh Shirzad1, Elham Shakibazadeh1, Abbas Rahimi Foroushani2, Mehrandokht Abedini3, Hamid Poursharifi4, Sohrab Babaei1 1. Department of Health Education and Promotion, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran. 2. Department of Epidemiology and Biostatistics, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran. ORCID number: 0000-0002-3052-6420 3. Maternal Health Department, Ministry of Health, Tehran, Iran 4. Department of Psychology, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ORCID ID: 0000-0003-3864-9924 Correspondence: Elham Shakibazadeh, ORCID ID: 0000-0002-1320-2133 |
Name and contact information for the trial sponsor {5b} | Tehran University of Medical Sciences (TUMS); email: vcr@tums.ac.ir Iran National Science Foundation (INSF); e-mail: info@insf.org |
Role of sponsor {5c} | The role of the funders is to monitor the corresponding research planning and progression. |
Introduction
Background and rationale {6a}
Cesarean section (CS) is an important surgical procedure, when normal vaginal delivery (NVD) imposes a risk to mother and/or baby [1]. The World Health Organization (WHO) states that a rate of CS between 10 and 15% of all births is ideal; however, the rate is steadily growing in recent years [2]. The average worldwide rate of CS is 18.6%, ranging from 6.0 to 27.2% in the least and more developed countries, respectively. Countries with the highest CS rates are Brazil (55.6%) and Dominican Republic (56.4%) in Latin America and the Caribbean. Iran and Turkey (47.9% and 47.5%, respectively) have the highest rates in Asia [3]. In Iran, the rate is even higher in private hospitals (72–89%) [4,5,6,7].
CS can save the lives of mothers and infants in emergency situations. However, current rates suggest that the CS is now used for women with normal and non-complicated pregnancies and births, when it is not medically necessary [8]. Unnecessary CSs could create complications with no benefits to both mother and baby [3, 9,10,11,12]. According to an observational study conducted by the WHO in nine Asian countries, women who undergo an unplanned CS before or during labor or who have an assisted (operative) vaginal delivery are more likely to experience morbidity than those who have spontaneous vaginal delivery [13]. As with any surgery, CS is associated with short- and long-term risks that may be minor or severe [14]. CS can be associated with significant short-term risks such as asphyxia, if the uterus is hypoperfused due to anesthesia, scalpel lacerations, and neonatal respiratory morbidities [9]. Other short-term risks of CS include increased risk of infection and lower likelihood of breastfeeding [10, 11, 15]. Moreover, urinary catheterization is associated with post-CS bacteriuria and has been reported to be as high as 11% [16]. Increasing rates of CS are associated with increased maternal and perinatal morbidities [17].
In 2014, Iran’s “health sector evolution policy” was launched to improve public health. One important objective of this policy was to decrease the rate of unnecessary CSs [18]. Several strategies have been conducted such as freeing NVDs in all public hospitals, developing mother-friendly hospitals, developing standard protocols of birth and preparation classes for women, improving privacy and infrastructure of labor, promoting standards in birth facilities, promoting water birth, and determining financial incentives to doctors to encourage them to do NVDs in public hospitals [19]. There was a reduction in CS rate after implementing the policy; however, the rate is still significantly higher than the rate recommended by the WHO [19].
Several studies have been conducted on reasons behind the high rate of CS in Iran [20,21,22,23]. Studies have shown that the main reason is the willingness of women to undergo CS due to fear of pain during labor and childbirth [21, 24, 25], concerns about genital modifications after vaginal delivery [26,27,28], belief that CS is safer for the baby [29,30,31], and the convenience for women and their families [18]. Studies show that women can play a major role in the decision-making process about their birth [32,33,34,35,36].
In recent years, different interventions intended to reduce the CS rate in Iran [37,38,39,40]. Although these interventions have been effective in the short term, they have not been effective in the long term. To further reduce the rate of CS, it is necessary not only to address the health system, health facility, and health professional factors, but also to change women’s choice behaviors [19]. The WHO has provided recommendations on non-clinical interventions to reduce unnecessary CSs. The recommendations are grouped according to the target of intervention: (a) interventions targeted at women, (b) interventions targeted at healthcare professionals, and (c) interventions targeted at health organizations, facilities, or systems [41].
Regarding non-clinical interventions on reducing unnecessary CS targeted at women, the WHO has recommended implementing psycho-education interventions for women [8, 42]. A Cochrane review conducted by Chen et al. on non-clinical interventions for reducing unnecessary CS reported that psycho-education interventions were effective in reducing unnecessary CSs [43]. The educational interventions included psycho-education on fear of childbirth [44], intensive group therapy (cognitive-behavioral therapy and childbirth psycho-therapy) [45], psycho-education by telephone [46], role-play education versus standard education using lectures [47], and nurse-led applied relaxation training program [44].
Several psycho-educational models and methods/strategies have been introduced to change behaviors effectively. Motivational interviewing (MI) is a patient-centered counseling approach to motivate individuals to change their behaviors [48], and it is specifically designed to enhance motivation to change among patients not ready to change [49]. It highlights the importance of motivation in personal behavior change. Research on MI has demonstrated positive effects of helping patients clarify goals, explore obstacles to treatment, and make commitments to change [49]. MI is a relatively new cognitive-behavioral technique that aims to help patients identify and change behaviors that may be placing them at risk of developing health problems or may be preventing optimal management of a chronic condition.
In the Information-Motivation-Behavioral skills (IMB) model, preventive behavioral skills represent a final common pathway for predicting complex preventive behaviors [50]. The IMB model is a generalizable and simple model to guide thinking about complex health behaviors. The IMB constructs, and how they pertain to patient adherence, are outlined below: (1) Information is the basic knowledge about a medical condition that might include how the disease develops, its expected course, and effective strategies for its management; (2) Motivation encompasses personal attitudes towards the adherence behavior, the perceived social support for such behavior, and the patients’ subjective norms or perceptions of how others with this medical condition might behave; and (3) Behavioral skills include ensuring that the patient has specific behavioral tools or strategies necessary to perform the adherence behavior such as enlisting social support and other self-regulation strategies.
In recent years, mobile applications play an important role in delivering educational content. People carry their mobile phones with themselves wherever they go, so educational interventions can be delivered at any time to anyone with extra support upon request wherever and whenever it is needed. This opportunity provides simple and non-expensive interventions to various ranges of individuals. Motivational messages, monitoring, and behavior change tools can be modified for delivery via mobile phones [51]. The effectiveness of this type of intervention is affirmed in several studies such as smoking cessation [52], adherence to prescribed medication [53], and blood pressure management [54]. This paper explains our study protocol aiming at comparing the effect of MI and IMB, and IMB based on mobile application (IMB-App) on choosing the mode of delivery in pregnant women.
Objectives {7}
This is the protocol of our study that aims at comparing the effect of IM, IMB, and IMB-App counseling interventions on choosing the mode of delivery in pregnant women.
Trial design {8}
This study is a randomized controlled, parallel-design trial.
Methods: participants, interventions, and outcomes
Study setting {9}
Pregnant women will be chosen from private hospitals located in Tehran. We have chosen private hospitals, because they support elective CS by providing high-quality facilities for women. Only in private hospitals, women are able to choose CS as a mode of delivery (maternal request) [18].
Eligibility criteria {10}
Inclusion criteria
The criteria for entering women are being literate, being in gestational age 24 to 32 weeks, being able to speak Persian, having no complications in the current pregnancy, having no indications for CS, and having enough time to participate in the interventions.
Exclusion criteria
We exclude women who show complications during the study, have preterm labor, and are reluctant to continue to participate in this study.
Who will take informed consent? {26a}
Written informed consent will be obtained from all the participants by the principal investigator or sub-investigators prior to enrollment.
Additional consent provisions for collection and use of participant data and biological specimens {26b}
This is not applicable. No biological specimens will be collected for research purposes; hence, no additional consent will be sought from the participants.
Interventions
Explanation for the choice of comparators {6b}
This is not applicable.
Intervention description {11a}
-
1
The content of interventions will be designed based on a qualitative evidence synthesis and a quantitative systematic review and meta-analysis in Iran [55]. Also, we will design the interventions tailored to the participants’ needs. The interventions are expected to take around 2 months to be completed, and women will be followed up until their delivery time.
-
2
Motivational interviewing (MI)
In this intervention group, pregnant women will be trained face-to-face based on the MI. During three 45–60-min sessions, MI techniques will be provided to the participants. MI is a directive, client-centered counseling style for eliciting behavior change by helping clients to explore and resolve ambivalence. It is most centrally defined not by technique but by its spirit as a facilitative style for interpersonal relationships. MI is a relatively simple, transparent, and supportive talk therapy based on the principles of cognitive-behavior therapy. In this group, we will help women to explore and resolve ambivalence about the mode of delivery and build their intrinsic motivation.
We will not force women to choose a specific mode of delivery. We will ask open-ended questions (for example, “Tell me what you think about CS?” or “What do encourage you to choose this type of delivery (CS or NVD)?”). Open-ended questions can help us to understand how they are thinking about the mode of delivery. Affirming is one of the fundamental MI skills. We will use it to support engagement, encourage the women to further explore change processes, and build confidence. We will find an opinion the client is making or a strength she will notice and reflect it to her (for example, “So how did you manage to control your fear after attending our training sessions?”). We will use reflective listening as a simple method to reduce resistance in MI. The last step of this technique is to summarize what the pregnant women have said.
-
3
Information, motivation, and behavioral skills model through a face-to-face approach (IMB)
During three 45–60-min sessions, the model’s strategies will be provided to the participants. Participants will receive information and behavioral skills related to the choice of mode of delivery as well as internal and external motivational factors related to the choice of delivery. The strategy includes the following: (1) Information—the intervention will begin with information on the prevalence of CS and CS-related complications in women, and outcome of unnecessary CS; (2) Motivation—the interventionist will perform this technique to motivate pregnant women, providing personal feedback, asking open-ended questions, affirming desirable behavior, reflective listening, working at the women’s pace, and negotiating goals that will be realistic and attainable; and (3) Behavioral skills—women will be given behavioral skills training on how to control the obstacle of NVD. To build skills for choosing the mode of delivery, training will be given on how to reduce these barriers.
-
4
Information, motivation, and behavioral skills model through mobile app (IMB-App)
The mobile application (M-health) has been designed based on the IMB model. The software will be installed on mobile phones of participants in the group, and its operation will be taught individually. Women will work with the application in the presence of the research team, and any existing problems will be resolved. The strategies foreseen for adherence improvement include reminders set at defined intervals in the form of pop-up messages. To monitor adherence, the data collected on the server will be used. In addition to the application, a server will be designed in which the users’ activities will be collected. Items such as the duration of application usage and the sections used by the user (in addition to registering their time and duration) will be registered. Every time the user’s mobile is connected to the Internet, the data will be uploaded and saved on to the server. These data can be used as a proxy of adherence to the intervention.
Control group: without any intervention
Criteria for discontinuing or modifying allocated interventions {11b}
The intervention will be discontinued based on the participant’s request, or if a woman undergoes birth.
Strategies to improve adherence to interventions {11c}
This is not applicable.
Relevant concomitant care permitted or prohibited during the trial {11d}
Usual prenatal care will be provided in all study groups.
Provisions for post-trial care {30}
This is not applicable.
Outcomes {12}
-
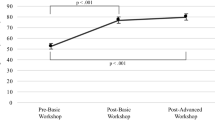
Determining and comparing the effects of MI, IMB, and IMB-App on mode of delivery in the target and control groups before and after the interventions.
-
Determining and comparing the effects of MI, IMB, and IMB-App on the intention of performing CS in women in the target and control groups before and after the interventions.
-
Determining and comparing the effect of MI, IMB, and IMB-App on women’s self-efficacy in target and control groups before and after the interventions.
Participant timeline {13}
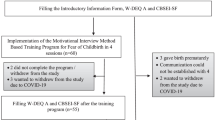
The recruitment of participants for this study started in December 2019 and is still ongoing. The recruitment is expected to be completed in April 2020; the data analysis, writing of scientific manuscripts, and submissions to peer-reviewed scientific journals will occur from 2020 to 2021.
Sample size {14}
The sample size is 120 pregnant women (30 in each group) with a power of 80% to detect a minimum difference.
Recruitment {15}
We will be present in the research setting during the intervention period to recruit all eligible women. The study will be available to all pregnant women interested in participating and speaking Persian. Individuals who fulfill the inclusion criteria will receive a description of the study, indicating the follow-up schedule and assurance of confidentiality, and they will be directed to complete a consent form. Included participants will be randomly allocated in three intervention groups and one control group.
Assignment of interventions: allocation
Sequence generation {16a}
The participants will be randomly assigned to four groups after the initial assessment and upon completing the baseline data form. We will recruit the participants based on the registration order of women with the clinic, and no other factor will contribute to participants’ order on the list. Each participant on the list will be assigned a consecutive research identification number according to the order by which they will be registered with the clinic. The first participant on the list will be randomly assigned to the MI intervention group, and the next two participants will be assigned to the IMB and IMB-App interventions, respectively. The fourth participant will be assigned to the control group.
Concealment mechanism {16b}
Randomization will be performed by a person who will not be engaged in the study and will be blinded to the identity of the participants.
Implementation {16c}
There will be four arms. The abovementioned interventions will be implemented among the three intervention groups. The control group will only receive usual care.
Assignment of interventions: blinding
This is not applicable. It is not possible to mask this study because of its nature. To avoid bias in the outcome assessment, research assistants concerned with data collection and/or preparation will be blinded to the allocation of the participants.
Who will be blinded {17a}
As the RCT is an educational intervention study, blinding of participants and researchers is not possible. To minimize selection bias, we will use randomization.
Procedure for unblinding if needed {17b}
This is not applicable.
Data collection and management
Plans for assessment and collection of outcomes {18a}
The primary outcome of the intervention (mode of delivery) will be measured using a checklist after the childbirth.
The secondary outcomes will be measured by a questionnaire 1 month after the interventions.
Questionnaire
The questionnaire contains the women’s demographic and obstetrics history information, self-efficacy [56] in CS, and intention [57]. Demographic and obstetrics history items include age, income, educational level (pregnant women and their spouses), employment status (pregnant women and their spouses), number of births, number of pregnancies, current gestational age, number of live children, history of infertility, history of illness, date of birth, and participating in birth classes.
The questionnaire also consists of 17 items about self-efficacy and one item about intention of the women. To measure women’s self-efficacy, we used the Iranian version of the Childbirth Self-Efficacy Inventory (CBSEI) [56]. The instrument was originally developed by Lowe to measure maternal confidence in coping abilities during labor [58]. Khorsandi et al. examined the psychometric properties of the Iranian version and reported that this version was acceptable, reliable, and valid to measure women’s self-efficacy. Items were Likert-type questions, ranging from 1 to 10. Intention was measured using a single item questionnaire [57]. Several studies have found that single item questionnaires would be sufficient to measure some constructs [59].
Plans to promote participant retention and complete follow-up {18b}
We will follow the participants until the time of delivery. The pregnant women will be participated in this study after ensuring that they have met the study criteria. They will complete informed consent forms. In the first visit, the baseline measurement will be completed by the researcher. During the second visit, the application will be installed on cell phones of the IMB-App group and its operation will be taught to them.
Data management {19}
To ensure that the data is correctly entered, a double entry of data will be performed by two different individuals. Pregnant women who refer to the hospital will be registered, by chronological order of selection, and they will be allocated randomly in each group. All data obtained from women will be entered to SPSS software. A code will be defined to identify missing data. After screening the data and preparing the data for statistical analysis, first using descriptive statistics such as frequency tables, means and standard deviation, and bar chart and histogram, the distribution of variables will be checked. The obtained data will be kept strictly confidential and will be stored with secured and restricted access; also, the signed consent will be kept locked. Follow-up data are received using the same questionnaires as used at baseline.
Confidentiality {27}
Only researchers will have access to the personal data in the trial. These data will not be published, and they will be discarded after the publication of results.
Plans for collection, laboratory evaluation, and storage of biological specimens for genetic or molecular analysis in this trial/future use {33}
This is not applicable. Researchers confirm that there are no laboratory and storage of biological specimens for genetic or molecular analysis in this study.
Statistical methods
Statistical methods for primary and secondary outcomes {20a}
Data will be analyzed using descriptive statistics (mean, frequency, and standard deviation); inferential statistics including independent t test, paired t test, chi-squared, and one-way ANOVA tests; and logistic regression modeling to examine the factors affecting the women’s choice on the mode of delivery to examine the simultaneous effect of variables on the chances of choosing CS. The significance level of the tests will be considered as less than 0.05.
Interim analyses {21b}
This is not applicable.
Methods for additional analyses (e.g., subgroup analyses) {20b}
This is not applicable.
Methods in analysis to handle protocol non-adherence and any statistical methods to handle missing data {20c}
This is not applicable.
Plans to give access to the full protocol, participant-level data, and statistical code {31c}
Information from the full protocol will be published in a peer-reviewed journal. The relevant data analyzed during the development of this study protocol are available upon request from the corresponding author.
Oversight and monitoring
A team from Tehran University of Medical Sciences and a peer reviewer (audit) from Iran National Science Foundation (INSF) will regularly monitor the study implementation and datasets and make recommendations on necessary protocol modifications or termination of all or part of the study.
Composition of the coordinating center and trial steering committee {5d}
This is not applicable.
Composition of the data monitoring committee, its role and reporting structure {21a}
Data monitoring will be coordinated by INSF. The auditors will follow a monitoring plan to verify that the clinical trial is conducted and that data are generated, documented, and reported in compliance with the protocol and the applicable regulatory requirements.
Adverse event reporting and harms {22}
Due to the nature of the intervention, there is no adverse event and no harm in this study. Based on our knowledge, the study will not have any negative consequences.
Frequency and plans for auditing trial conduct {23}
Every 6 months, we will send a report to the auditor.
Plans for communicating important protocol amendments to relevant parties (e.g., trial participants, ethical committees) {25}
This is not applicable.
Dissemination plans {31a}
We will share the results of this study with key stakeholders via presenting in related seminars and publishing in peer-reviewed journals. We will also provide and share monographs with related departments in the Ministry of Health, Iran.
Discussion
This study aims to assess the effect of IM, IMB, and IMB-App on choosing the mode of delivery in pregnant women. Iran has one of the highest CS rates in the region and the world [60]. In line with increasing unnecessary CS, Iran’s healthcare system was reformed and NVD was on the agenda [19]. Many policy interventions have been performed to reduce unnecessary CS rate [39, 40, 61]; however, they were not sustained for a long time. These experiences indicate that the interventions have not been effective enough. Designing appropriate interventions for promoting NVD and decreasing the use of unnecessary CS is one of the most important WHO recommendations on non-clinical interventions on CS [41].
A large portion of increased unnecessary CS rates in Iran is related to women [26, 31, 34, 35, 62,63,64,65]. Several studies have reported women’s important role in increasing CS. Women have some problems when they want to choose the mode of delivery. Several studies have shown that the most common reasons underlying the preference for CS in Iran were deep-rooted fear of labor pain and vaginal birth [26, 34, 66,67,68,69,70], irreversible damage to the body and sexual function [23, 28, 35, 36, 70, 71], safety (mother/ baby) and comfort [20, 28, 33, 34, 63, 72], social convenience of birthing to time (time scheduling) [26, 34, 68,69,70, 73], religious beliefs [28, 34, 70, 72], and cultural beliefs (having role models; modernity, the capability to do vaginal birth) [20, 63, 72, 74, 75]. We realized that most of the reasons come from their beliefs. Therefore, we need to conduct cognitive intervention to decrease the rate. According to the WHO recommendation, psycho-education interventions may be useful to decrease this trend [41].
Due to the target group and their problems with long-term intervention or attendance at classes, we will use brief intervention. The brief intervention is efficacious in mechanisms of change [76,77,78]. Among different models and techniques, we supposed MI and IMB models can be an effective method of facilitating behavioral changes in CS. The effectiveness of these models has already been confirmed. There are several examples of successful interventions about this technique in health. Rubak et al.’s review has shown that MI is a scientific setting that effectively helps clients change their behavior [79]. The review has shown that MI can be effective even in brief encounters of only 15 min [79]. Another review indicates the potential strength of the IMB model as a theoretical framework to develop behavioral interventions [80]. In this study, we will use both techniques as our study framework for face-to-face education. In recent years, massive smartphone applications have been used widely and effectively in education [81]. We have created a mobile app based on the IMB model to use in a group of interventions. The content has been designed according to the constructs of IMB model.
Limitations and strengths
We understand that women may be inclined to respond in certain ways because they come to receive certain services. However, we will ensure that their responses will not affect the service they will receive and ensure confidentiality. The self-report nature of the questionnaire and necessity of owning a smartphone are another limitation.
Diverse interventions will allow the researchers to obtain different perspectives from the outcome. We have designed evidence-based non-clinical interventions to reduce unnecessary CSs targeted at women. Causes of increasing CS rates are various and different between and within countries. Before implementing any intervention on the issue, we should recognize the reasons behind this increase, as well as locally relevant determinants of CS, and the views and cultural norms of women and healthcare providers. Our study is supported by evidence-based (qualitative synthesis and meta-analysis in Iran) (unpublished paper) information. We will also use a mobile app, a technology that is ubiquitous and has no limitations. Another strength is the simple and non-expensive nature of the interventions.
Conclusion
To the best of our knowledge, this paper is the first published paper that describes the protocol of CS with this design (face-to-face and M-health) in Iran. We believe that our study will lead to decrease unnecessary CS in the health system of Iran, and conducting this intervention can increase NVD. To achieve this goal, a systematic review study is done to assess the reason of CS in Iran.
Trial status
The recruitment of participants for this study started in December 2019 and is still ongoing. The recruitment is expected to be completed in March 2020.
Current protocol version and date: V2.0, 1 December 2019.
Abbreviations
- CS:
-
Cesarean section
- NVD:
-
Normal vaginal delivery
- WHO:
-
World Health Organization
- TUMS:
-
Tehran University of Medical Sciences
- INSF:
-
Iran National Science Foundation
References
Ahmad Nia S, Delavar B, Eini Zinab H, Kazemipour S, Mehryar A, Naghavi M. Caesarean section in the Islamic Republic of Iran: prevalence and some sociodemographic correlates; 2009..
Betran AP, Torloni MR, Zhang JJ, Gülmezoglu AM; WHO Working Group on Caesarean Section. WHO Statement on Caesarean Section Rates. BJOG. 2016;123(5):667–670. https://doi.org/10.1111/1471-0528.13526.
Betrán AP, Ye J, Moller A-B, Zhang J, Gülmezoglu AM, Torloni MR. The increasing trend in caesarean section rates: global, regional and national estimates: 1990-2014. PLoS One. 2016;11(2):e0148343.
Yavangi M, Sohrabi M-R, Alishahi TA. Effect of Iranian ministry of health protocols on cesarean section rate: a quasi-experimental study. J Res Health Sci. 2013;13(1):48–52.
Azami-Aghdash S, Ghojazadeh M, Dehdilani N, Mohammadi M. Prevalence and causes of cesarean section in Iran: systematic review and meta-analysis. Iran J Public Health. 2014;43(5):545.
Omani-Samani R, Mohammadi M, Almasi-Hashiani A, Maroufizadeh S. Cesarean section and socioeconomic status in Tehran. Iran J Res Health Sci. 2017;17(4):e00394.
Mohamadbeigi A, Tabatabaee SH, Mohammad Salehi N, Yazdani M. Factors influencing cesarean delivery method in Shiraz hospitals. Iran J Nurs. 2009;21(56):37–45.
Kingdon C, Downe S, Betran AP. Women’s and communities’ views of targeted educational interventions to reduce unnecessary caesarean section: a qualitative evidence synthesis. Reprod Health. 2018;15(1):130.
Gregory KD, Jackson S, Korst L, Fridman M. Cesarean versus vaginal delivery: whose risks? Whose benefits? Am J Perinatol. 2012;29(01):07–18.
Creasy R, Resnik R, Iams J. Clinical aspects of normal and abnormal labor. Matern Fetal Med. 1984;5:543–9.
Guise J-M, Eden K, Emeis C, Denman MA, Marshall N, Fu RR, et al. Vaginal birth after cesarean: new insights. Evid Rep Technol Assess. 2010;191:1.
Souza JP, Gülmezoglu A, Lumbiganon P, Laopaiboon M, Carroli G, Fawole B, et al. Caesarean section without medical indications is associated with an increased risk of adverse short-term maternal outcomes: the 2004-2008 WHO Global Survey on Maternal and Perinatal Health. BMC Med. 2010;8(1):71.
Ramashwar S. In Asia, cesarean section associated with increased risk of neonatal mortality. Int Perspect Sex Reprod Health. 2010;36(2):116.
Rothenberg KH. National Institutes of Health State-of-the-Science Conference Statement: cesarean delivery on maternal request. Obstetrics Gynecol. 2006;107:1386.
Menacker F, Hamilton BE. Recent trends in cesarean delivery in the United States; 2010.
Buchholz N-P, Daly-Grandeau E, Huber-Buchholz M-M. Urological complications associated with caesarean section. Eur J Obstetrics Gynecol Reprod Biol. 1994;56(3):161–3.
Organization WH. WHO statement on caesarean section rates; 2018. p. 12.
Shirzad M, Shakibazadeh E, Betran AP, Bohren MA, Abedini M. Women’s perspectives on health facility and system levels factors influencing mode of delivery in Tehran: a qualitative study. Reprod Health. 2019;16(1):15.
Rashidian A, Moradi G, Takian A, Sakha MA, Salavati S, Faraji O, et al. Effects of the Health Transformation Plan on caesarean section rate in the Islamic Republic of Iran: an interrupted time series. 2018.
Yazdizadeh B, Nedjat S, Mohammad K, Rashidian A, Changizi N, Majdzadeh R. Cesarean section rate in Iran, multidimensional approaches for behavioral change of providers: a qualitative study. BMC Health Serv Res. 2011;11(1):159.
Bagheri A, Masoodi-Alavi N, Abbaszade F. Effective factors for choosing the delivery method among the pregnant women in Kashan. KAUMS J (FEYZ). 2012;16(2):146–53.
Lotfi R, Ramezani TF, Torkestani F, Rostami DM, Abedini M, Sajedinejad S. Health system management and strategies to decrease elective cesarean section: a qualitative study; 2015.
Shams M, Mousavizadeh A, Parhizkar S, Maleki M, Angha P. Development a tailored intervention to promote normal vaginal delivery among primigravida women: a formative research. Iran J Obstetrics Gynecol Infertil. 2016;19(30):9–25.
Shahoei R, Rostami F, Khosravi F, Ranayi F, Hasheminasab L, Hesami K, et al. Women lived experience of choice of cesarean delivery: a phenomenology study. Iran J Obstetrics Gynecol Infertil. 2014;17(104):1–10.
Abbaspour Z, Moghaddam BI, Ahmadi F, Kazemnejad A. Women’s fear of childbirth and its impact on selection of birth method: a qualitative study; 2014.
Rahnama P, Mohammadi K, Montazeri A. Salient beliefs towards vaginal delivery in pregnant women: a qualitative study from Iran. Reprod Health. 2015;13(1):7.
Javaheri F, Hashemikhah Z. Voluntary cesarean the study on female existential experiences based on a sample from Tehran; 2016.
Hajian S, Shariati M, Najmabadi KM, Yunesian M, Ajami ME. Psychological predictors of intention to deliver vaginally through the extended parallel process model: a mixed-method approach in pregnant Iranian women. Oman Med J. 2013;28(6):395.
Hajian S, Vakilian K, Shariati M, Esmaeel AM. Attitude of pregnant women, midwives, obstetricians and anesthesiologists toward mode of delivery: a qualitative study; 2011.
Tohid S, St EN. How do women's decisions process to elective cesarean?: a qualitative study. Aust J Basic Appl Sci. 2011;5(6):210–5.
Shahoei R, Rezaei M, Ranaei F, Khosravy F, Zaheri F. Kurdish women’s preference for mode of birth: a qualitative study. Int J Nurs Pract. 2014;20(3):302–9.
Latifnejad-Roudsari R, Zakerihamidi M, Merghati-Khoei E, Kazemnejad A. Cultural perceptions and preferences of Iranian women regarding cesarean delivery. Iran J Nurs Midwifery Res. 2014;19(7 Suppl1):S28.
Bayrami R, Valizadeh L, Zaheri F. Nulliparous women’s childbirth experiences: a phenomenological study; 2011.
Mobarakabadi SS, Najmabadi KM, Tabatabaie MG. Ambivalence towards childbirth in a medicalized context: a qualitative inquiry among Iranian mothers. Irani Red Crescent Med J. 2015;17(3):e24262. https://doi.org/10.5812/ircmj.24262.
Faisal I, Matinnia N, Hejar A, Khodakarami Z. Why do primigravidae request caesarean section in a normal pregnancy? A qualitative study in Iran. Midwifery. 2014;30(2):227–33.
Abbaspoor Z, Moghaddam-Banaem L, Ahmadi F, Kazemnejad LA. Postnatal sexual concerns regarding the selection of delivery mode among Iranian women: a qualitative content analysis. J Midwifery Reprod Health. 2016;4(2):613–21.
Besharati F, Hazavehei S, Moeini B, Moghimbeigi A. Effect of educational interventions based on theory of planned behavior (TPB) in selecting delivery mode among pregnant women referred to Rasht health centers. J Zanjan Univ Med Sci Health Serv. 2011;19(77):10.
Soltani F, Eskandari Z, Khodakarami B, Parsa P, Roshanaei G. The effect of self-efficacy oriented counselling on controlling the fear of natural delivery in primigravida women. J Pharm Sci Res. 2017;9(10):1757–61.
Sharifirad G, Rezaeian M, Soltani R, Javaheri S, Mazaheri MA. A survey on the effects of husbands education of pregnant women on knowledge, attitude, and reducing elective cesarean section. Health Serv Res. 2010;6(1):7–12.
Rasouli M, Mousavi SA, Khosravi A, Keramat A, Fooladi E, Atashsokhan G. The impact of motivational interviewing on behavior stages of nulliparous pregnant women preparing for childbirth: a randomized clinical trial. J Psychosom Obstet Gynecol. 2018;39(3):237–45.
Organization WH. WHO recommendations non-clinical interventions to reduce unnecessary caesarean sections: World Health Organization; 2018.
Walker R, Turnbull D, Wilkinson C. Strategies to address global cesarean section rates: a review of the evidence. Birth. 2002;29(1):28–39.
Chen I, Opiyo N, Tavender E, Mortazhejri S, Rader T, Petkovic J, Yogasingam S, Taljaard M, Agarwal S, Laopaiboon M, Wasiak J, Khunpradit S, Lumbiganon P, Gruen RL, Betran AP. Non-clinical interventions for reducing unnecessary caesarean section. Cochrane Database Syst Rev. 2018;9(9):CD005528. https://doi.org/10.1002/14651858.CD005528.
Bastani F, Hidarnia A, Montgomery KS, Aguilar-Vafaei ME, Kazemnejad A. Does relaxation education in anxious primigravid Iranian women influence adverse pregnancy outcomes?: a randomized controlled trial. J Perinat Neonatal Nurs. 2006;20(2):138–46.
Saisto T, Salmela-Aro K, Nurmi J-E, Könönen T, Halmesmäki E. A randomized controlled trial of intervention in fear of childbirth. Obstet Gynecol. 2001;98(5):820–6.
Rouhe H, Salmela-Aro K, Toivanen R, Tokola M, Halmesmäki E, Saisto T. Obstetric outcome after intervention for severe fear of childbirth in nulliparous women–randomised trial. BJOG Int J Obstet Gynaecol. 2013;120(1):75–84.
Navaee M, Abedian Z. Effect of role play education on primiparous women’s fear of natural delivery and their decision on the mode of delivery. Iran J Nurs Midwifery Res. 2015;20(1):40.
Miller WR. Motivational interviewing: research, practice, and puzzles. Addict Behav. 1996;21(6):835–42.
Hoseini Haji SZ, Firoozi M, Asghari Pour N, Taghi SM. Impact of motivational interviewing on women’s knowledge, attitude and intention to choose vaginal birth after caesarean section: a randomized clinical trial. J Midwifery Reprod Health. 2019;8(1):1–11.
Fisher WA, Fisher JD, Harman J. The information-motivation-behavioral skills model: a general social psychological approach to understanding and promoting health behavior. Soc Psychol Foundations Health Illn. 2003;82:106.
Free C, Phillips G, Galli L, Watson L, Felix L, Edwards P, et al. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Med. 2013;10(1):e1001362.
Whittaker R, McRobbie H, Bullen C, Rodgers A, Gu Y. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst Rev. 2016;4(4):CD006611. https://doi.org/10.1002/14651858.CD006611.
Dayer L, Heldenbrand S, Anderson P, Gubbins PO, Martin BC. Smartphone medication adherence apps: potential benefits to patients and providers. J Am Pharm Assoc. 2013;53(2):172–81.
Price M, Yuen EK, Goetter EM, Herbert JD, Forman EM, Acierno R, et al. mHealth: a mechanism to deliver more accessible, more effective mental health care. Clin Psychol Psychother. 2014;21(5):427–36.
Shirzad M, Shakibazadeh E, Hajimiri KH, Betran AP, Jahanfar S, Meghan A, Bohren ON, Long Q, Kingdon C, Colomar M, Abedini M. Prevalence of and reasons for women’s, family members’, and health professionals’ preferences for cesarean section in Iran: a mixed-methods systematic review; 2019.
Khorsandi M, Ghofranipour F, Faghihzadeh S, Hidarnia A, Akbarzadeh Bagheban A, Aguilar-Vafaie ME. Iranian version of childbirth self-efficacy inventory. J Clin Nurs. 2008;17(21):2846–55.
ShahrakiSanavi F, Navidian A, Rakhshani F, Ansari-Moghaddam A. The effect of education on base the Theory of Planned Behavior toward normal delivery in pregnant women with intention elective cesarean. Hormozgan Med J. 2014;17(6):531–9.
Lowe NK. Maternal confidence for labor: development of the childbirth self-efficacy inventory. Res Nurs Health. 1993;16(2):141–9.
Wanous JP, Hudy MJ. Single-item reliability: a replication and extension. Organ Res Methods. 2001;4(4):361–75.
Gibbons L, Belizán JM, Lauer JA, Betrán AP, Merialdi M, Althabe F. The global numbers and costs of additionally needed and unnecessary caesarean sections performed per year: overuse as a barrier to universal coverage. World Health Rep. 2010;30:1–31.
Arefi Z, Hekamatpou D, Ali Orouji M, Shaahmadi Z, Khushemehri G, Shaahmadi F. The effect of educational intervention based on BASNEF model on decreasing the cesarean section rate among pregnant women in Khomain country. J Fami Reprod Health. 2015;9(3):101.
Moffat M, Bell JS, Porter MA, Lawton S, Hundley V, Danielian P, et al. Decision making about mode of delivery among pregnant women who have previously had a caesarean section: a qualitative study. BJOG Int J Obstet Gynaecol. 2007;114(1):86–93.
Roudsari RL, Zakerihamidi M, Khoei EM. Socio-cultural beliefs, values and traditions regarding women’s preferred mode of birth in the North of Iran. Int J Commun Based Nurs Midwifery. 2015;3(3):165–76.
Zakerihamidi M, Roudsari RL, Khoei EM. Vaginal delivery vs. cesarean section: a focused ethnographic study of women’s perceptions in the north of Iran. Int J Commun Based Nurs Midwifery. 2015;3(1):39.
Sadat Z. Reasons for elective cesarean section in Iranian women. Nurs Midwifery Stud. 2014;3(3):e22502.
Ahmad SHirvani M, Bagheri-Nesami M, Tayebi T. Exploration of women birth experiences role in decisiding the type of next delivery. J Nurs Midwifery Urmia Univ Med Sci. 2014;12(4):286–96.
Borghei NS, Taghipour A, Latifnejad RR. The concern of fetal health: women’s experiences of worries during pregnancy. Iran J Obstetrics Gynecol Infertil. 2016;19(28):10–21.
Sanavi FS, Rakhshani F, Ansari-Moghaddam A, Edalatian M. Reasons for elective cesarean section amongst pregnant women; a qualitative study. J Reprod Infertil. 2012;13(4):237–40.
Darvishi E, Mortazavi S, Nedjat S, Holakouie NK. Experiences of women and gynecologists on the choice of delivery method: a qualitative research. J Health Sys Res. 2012;8:59–68.
Javaheri F, Hashemikhah Z. Voluntary cesarean the study on female existential experiences based on a sample from Tehran. Women’s strategic studies (ketabe zanan). Spring. 2016;18:7–28.
Mansoureh Jamshidi Manesh LJ, Oskouie SF, Sanagoo A. How do women’s decisions process to elective cesarean?: a qualitative study. Aust J Basic Appl Sci. 2011;5(6):210–5.
Hajian S, Vakilian K, Shariati M, Ajami ME. Attitude of pregnant women, midwives, obstetricians and anesthesiologists toward mode of delivery: a qualitative study. Health Monit J Iran Inst Health Sci Res. 2011;10(1):39–48.
Rahnama P, Mohammadi K. Behavioral beliefs about cesarean section according to the theory of planned behavior in pregnant women. J Mazandaran Univ Med Sci. 2015;24(122):169–78.
Abbaspoor Z, Moghaddam-Banaem L, Ahmadi F, Kazemnejad A. Iranian mothers’ selection of a birth method in the context of perceived norms: a content analysis study. Midwifery. 2014;30(7):804–9.
AbouAli Vedadhir FH, Sadati SMH. Childbearing as a socio-cultural issue: constructionism contemplation of Caesarean section in Tabriz, Iran. Iran J Anthropol Res. 2011;1(2):111–35.
Borsari B, Carey KB. Effects of a brief motivational intervention with college student drinkers. J Consult Clin Psychol. 2000;68(4):728.
Walton GM, Cohen GL. A brief social-belonging intervention improves academic and health outcomes of minority students. Science. 2011;331(6023):1447–51.
McCambridge J, Saitz R. Rethinking brief interventions for alcohol in general practice. Bmj. 2017;356:j116.
Rubak S, Sandbæk A, Lauritzen T, Christensen B. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract. 2005;55(513):305–12.
Chang SJ, Choi S, Kim S-A, Song M. Intervention strategies based on information-motivation-behavioral skills model for health behavior change: a systematic review. Asian Nurs Res. 2014;8(3):172–81.
Boulos MNK, Wheeler S, Tavares C, Jones R. How smartphones are changing the face of mobile and participatory healthcare: an overview, with example from eCAALYX. Biomed Eng Online. 2011;10(1):24.
Acknowledgements
We are grateful to the women who are participating in our study. Also, we are grateful for the excellent support provided by the Ebnesina Hospital.
Authors’ contributions {31b}
ESh, MSh, MA, ARF, and HP have conceptualized the study. ESh, MSh, and MA have developed the study design and data collection plans. MSh and ESh will collect and analyze the data. ESh, MSh, and SB drafted this manuscript. All authors provided critical input on an earlier version of the manuscript and read and approved the final manuscript.
Competing interests {28}
The authors declare that they have no competing interests.
Funding {4}
This study is being financially supported by the Tehran University of Medical Sciences (TUMS) and Iran National Science Foundation (INSF) (Project code: 97014281). The role of the funders is to monitor the corresponding research planning and progression.
Availability of data and materials {29}
Not applicable. This manuscript does not contain any data, as this is a study design manuscript.
Consent for publication {32}
Not applicable.
Ethics approval and consent to participate {24}
This was conducted as part of a Ph.D. thesis project at the Tehran University of Medical Sciences (TUMS). This study was approved by the School of Public Health and Allied Medical Sciences Ethics Committee; Tehran University of Medical Sciences (Ethics code: IR.TUMS.SPH.REC 1397-130). All participants will be informed about the study and purposes and will be ensured that all collected information will remain confidential. Every participant will be signed an informed consent form.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shirzad, M., Shakibazadeh, E., Rahimi Foroushani, A. et al. Effect of “motivational interviewing” and “information, motivation, and behavioral skills” counseling interventions on choosing the mode of delivery in pregnant women: a study protocol for a randomized controlled trial. Trials 21, 970 (2020). https://doi.org/10.1186/s13063-020-04865-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-020-04865-3