Abstract
Background
New evidence supports the use of supplemental vitamin D in the prevention of exacerbation of asthma; however, the optimal posology to sufficiently raise serum levels while maximising adherence is unclear. The objective was to ascertain the efficacy of high-dose vitamin D3 in increasing serum vitamin D in preschoolers with asthma and provide preliminary data on safety and efficacy outcomes.
Methods
We conducted a 7-month, triple-blind, randomised, placebo-controlled, pilot trial of children aged 1–5 years with viral-induced asthma. Participants were allocated to receive two oral doses of 100,000 IU vitamin D3 (intervention) or identical placebo (control) 3.5 months apart, once in the fall and once in the winter. Serum 25-hydroxyvitamin D (25OHD) was measured by tandem mass spectrometry at baseline, 10 days, 3.5 months, 3.5 months + 10 days, and 7 months. The main outcome was the change in serum 25OHD from baseline (Δ25OHD) over time and at 3.5 and 7 months; other outcomes included the proportion of children with 25OHD ≥ 75 nmol/L, safety, and adverse event rates.
Results
Children (N = 47) were randomised (intervention, 23; control, 24) in the fall. There was a significant adjusted group difference in the Δ25OHD (95% confidence interval) of 57.8 (47.3, 68.4) nmol/L, p < 0.0001), with a time (p < 0.0001) and group*time interaction effect (p < 0.0001), in favour of the intervention. A significant group difference in the Δ25OHD was observed 10 days after the first (119.3 [105.8, 132.9] nmol/L) and second (100.1 [85.7, 114.6] nmol/L) bolus; it did not reach statistical significance at 3.5 and 7 months. At 3.5 and 7 months, respectively, 63% and 56% of the intervention group were vitamin D sufficient (≥ 75 nmol/L) compared to 39% and 36% of the control group. Hypercalciuria, all without hypercalcaemia, was observed in 8.7% of intervention and 10.3% of control samples at any time point. Exacerbations requiring rescue oral corticosteroids, which appear as a promising primary outcome, occurred at a rate of 0.87/child.
Conclusion
Two oral boluses of 100,000 IU vitamin D3,once in the fall and once in the winter, rapidly, safely, and significantly raises overall serum vitamin D metabolites. However, it is sufficient to maintain 25OHD ≥ 75 nmol/L throughout 7 months in only slightly more than half of participants.
Trial registration
ClinicalTrials.gov, NCT02197702 (23 072014). Registered on 23 July 2014.
Similar content being viewed by others
Background
Asthma is the most common chronic childhood disease, affecting about 10% of children [1, 2], with preschoolers experiencing the highest rate of emergency department (ED) visits relative to other age groups [2,3,4]. Most exacerbations are triggered by viral upper respiratory tract infections (URTIs), particularly in young children [5, 6]. Circulating 25-hydroxyvitamin D (25OHD) has been inversely associated with an increased risk of viral URTIs, asthma severity, inhaled corticosteroid dose, and moderate or severe exacerbations [7,8,9], suggesting the potential role for vitamin D in viral infections and asthma. Inadequate dietary intake of vitamin D [10, 11], low use of vitamin D supplements [11, 12], dark skin pigmentation, obesity, and low sun exposure increase the risk of vitamin D insufficiency [13,14,15], affecting 40–82% of children living in high-latitude areas [11, 16, 17]. Of concern, is the higher reported rate of vitamin D insufficiency in children with versus without asthma [18,19,20]; in Canadian preschoolers with asthma, almost 75% are already vitamin D insufficient in the fall [21].
In a meta-analysis of individual patient data, Martineau and colleagues reported a significantly reduced risk of acute respiratory tract infections in participants receiving vitamin D supplementation [22]. A Cochrane systematic review of nine asthma trials (two adult and seven paediatric) [21], with variable use of inhaled corticosteroids (ICS), reported a statistically significant protective effect of vitamin D supplementation against exacerbations requiring rescue oral steroids or emergency department visits, with high-quality evidence and no heterogeneity [23]. However, the optimal posology of this promising strategy remains to be determined. We have demonstrated a rapid rise in serum vitamin D with the combination of a single bolus dose of 100,000 IU vitamin D3 and 400 IU daily for 6 months, but no significant group difference at 3 and 6 months compared to a placebo bolus and 400 IU vitamin D3 daily [21]. We surmised that the daily vitamin D supplementation in both groups attenuated group separation and that a single bolus was inadequate to maintain vitamin D sufficiency during both the fall and winter seasons.
The objective of this study was to determine if two bolus doses of vitamin D3 supplement, once in the fall and once in the winter, are associated with a rapid and sustained improvement in serum 25OHD. Second, we wish to provide pilot data on the efficacy and safety of this intervention, before formally testing in an adequately powered trial the efficacy of this strategy to improve health outcomes in preschoolers with viral-induced asthma.
Methods
Design
We conducted a 7-month randomised, parallel-group, triple-blind, placebo-controlled trial at the Sainte-Justine University Health Centre (SJUHC), Montreal Canada, in accordance with Helsinki Good Clinical Practice Guidelines [24]. The Institutional Research Ethics Board (#2015–786, 4004) and Health Canada approved the study (#187438). Euro-Pharm (Montreal, Canada) donated the drug, but had no input into the study design, conduct, analysis, or writing of the study. Parents provided written informed consent for their child’s study participation and for the release of medical and pharmacy data. Parents received small monetary reimbursement for parking or transportation. The study is reported according to recommended standards (Additional file 1).
Participants
Children aged 1–5 years were eligible if they had: (i) physician-diagnosed asthma, based on clinical signs of airflow obstruction and reversibility [25]; (ii) URTI reported by parents as the main asthma trigger; (iii) ≥ 4 URTIs in the preceding year; and (iv) ≥ 1 exacerbation requiring rescue oral corticosteroids (OCS) in the preceding 6 months (or ≥ 2 in the past 12 months), confirmed by pharmacy and/or medical records. Patients were excluded due to intake of or intention to use > 400 IU/day of vitamin D supplement; extreme prematurity (< 28 weeks’ gestation); high risk of vitamin D deficiency (e.g., vegan diet); condition(s) (e.g., rickets) or drug(s) altering calcium or vitamin D absorption or metabolism (e.g., anti-epileptic, diuretic, antacid, or anti-fungal medications); anticipated difficult follow up.
Randomisation and blinding
We randomised children to receive vitamin D or placebo supplement in a 1:1 ratio, using computer-generated random numbers with variable permuted blocks. No daily supplement was provided or recommended. The active (50,000 IU/mL of cholecalciferol) and placebo preparations were identical in appearance and taste. The Central Pharmacy (SJUHC) held the allocation codes, prepared the study supplements in sequentially coded syringes, and dispensed as per randomisation 2 mL of vitamin D3 (100,000 IU of cholecalciferol) or identical placebo, administered by the nurse at baseline and 3.5 months. At the end of follow up, parents, nurse, and physician independently guessed the child’s group assignment.
Protocol
Children were randomised between 1 September and 30 November in 2014 and 2015 and were followed for 7 ± 0.5 months. Baseline characteristics included demographics, atopy [26], and recent morbidity. As per national recommendations physicians reviewed the management plan at randomisation to include daily ICS with/without adjunct therapy, or episodic high-dose ICS, with rescue salbutamol during exacerbations, delivered by metered dose inhalers with a holding chamber [25]. After randomisation, two medical visits at 3.5 ± 0.5 and 7 ± 0.5 months, with monthly phone contacts, served to review asthma control, vitamin D and calcium intake according to a validated food frequency questionnaire [27], URTIs, exacerbations, healthcare utilisation, and adverse health events. Non-fasting urine and blood samples were obtained at each visit (Additional file 2). At randomisation, the urine calcium:creatinine ratio (Ca:Cr) and serum calcium, phosphorus and alkaline phosphatase were systematically analysed. At each subsequent clinic and home visit, only urinary Ca:Cr was routinely analysed for safety monitoring; if abnormal, the aforementioned serum markers were analysed. Additional serum aliquots were stored at − 80 °C for total 25OHD vitamin D, which was analysed using tandem mass spectrometry only at the end of the study [28, 29].
Outcomes
After premature trial cessation due partial funding enabling only a 2-year single-centre pilot trial, rather than an adequately powered multicentre study of 865 children, the primary outcome was modified post hoc to the overall change (∆) from baseline in total serum 25OHD and at 3.5 and 7 months, similar to our previous pilot study [21]. Post hoc secondary outcomes included group difference in the proportion of children with total 25OHD ≥ 75 nmol/L at 3.5 and 7 months, and the rate of OCS courses per child. Other outcomes specified a priori included the proportion of children with hypercalciuria (Ca:Cr) > 1.25 (1–2 years)or > 1 (2–5 years) nmol/nmol at any point in time; proportion of children with ≥ 1 exacerbation requiring rescue OCS (former primary outcome); number of emergency department (ED) visits; intensity and duration of asthma symptoms and cumulative use of rescue ß2-agonist use, documented on the Asthma Flare-up Diary for Young Children (ADYC) [30]; parental functional status during exacerbations ascertained on the Effect of a child’s asthma flare-up on parents (ECAP) [31]; and URTI duration.
Statistical methods
An intention-to-treat (ITT) analysis was carried out whereby all randomised children were included in the analysis, wherever possible. The group difference in within-patient ∆25OHD level overall, and specifically at 3.5 and at 7 months, was examined using a generalised linear mixed model, after adjustment for variables with a potential for effect modification (vitamin D intake, ethnicity) or baseline group imbalance (sex, ethnicity, environmental tobacco exposure, school-day missed, asthma management strategy). Modified multivariable logistic regression (to deal with lack of convergence) [32] served to estimate the relative risk of children experiencing at least one event (OCS and emergency department (ED) visits), with 95% confidence interval. We computed the incidence rate ratio to compare the event rate per child, namely, the mean number of OCS and URTI occurring during the 7-month follow up, with an offset variable for variations in person-time, where relevant. The severity and duration of asthma symptoms, use of rescue β2-agonists, and functional outcomes during episodes were compared across groups using a generalised linear regression model, adjusting for the clustering of events in individual children. In all efficacy models, covariates considered a priori for inclusion in the model were those with a potential for effect modification: vitamin D intake, asthma phenotype (episodic versus persistent), skin colour (Fitzpatrick scale) [33], or baseline group imbalance (sex, ethnicity, environmental tobacco exposure, school-day missed, management strategy (episodic ICS versus daily ICS monotherapy versus daily ICS with adjunct therapy)). Of note, to avoid multicollinearity due to the strong correlation (r = 0.95) between ethnicity and skin colour, ethnicity was selected, because complete data were available. Continuous values were displayed as mean (95% CI). All tests were two-sided with estimates presented with 95% CI, with no adjustment for multiple outcomes. All analyses were carried out using SAS software version 9.3.
Results
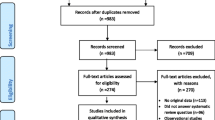
We screened 274 children: 102 were ineligible, primarily due to an insufficient number of URTI (33%), no asthma diagnosis (20%), anticipated difficult follow up (18%), and no recent rescue OCS use (10%). Of the 172 potentially eligible children, 125 declined participation mainly because of the number of blood tests, lack of time to comply to other procedures, and lack of interest. Participants were comparable to non-participants in age and sex (data not shown). There were 47 children randomised to the intervention (N = 23) or control group (N = 24) (Fig. 1).
Patient selection. The flow of patients is depicted from screening to analysis; 274 children were screened, 102 were not eligible (non-mutually exclusive reasons for ineligibility are listed). Of the 172 provisionally eligible children, 77 could not be reached to confirm eligibility and 48 were not interested in study participation. Of the 47 randomised children, 23 were allocated to receive vitamin D and 24 to receive placebo supplementation. With one child in each group with no measurement of serum 25-hydroxyvitamin D (25OHD) after baseline, 22 and 23 children in the vitamin D and placebo groups were analysed for the main outcome. URTI, Upper respiratory tract infection
Most baseline characteristics were similar between groups but some appeared slightly imbalanced, with a greater proportion of male participants, environmental tobacco exposure, use of combination therapy, more school days missed, fewer Caucasians and lower vitamin D dietary intake in the intervention compared to the placebo group (Table 1). With a mean age of 2.9 years, most participants were male, Caucasian, and had persistent asthma and URTI as one of multiple asthma triggers; half were atopic. Participants had experienced significant morbidity in the preceding year and at randomisation, most were prescribed daily ICS with or without adjunct therapy. Barely 13% were taking supplemental vitamin D at baseline at a daily dose of 50–400 UI. The median dietary intake of vitamin D (< 250 IU) was markedly below the recommended 600 IU [34] and did not change significantly throughout the study. Most participants had vitamin D insufficiency (< 75 nmol/L) at randomisation, but none had deficiency (< 25 nmol/L) [35].
The median (25%, 75%) follow up was 7 (6.5, 7.4) months, with 89% retention: one participant from the intervention group withdrew at visit 1, two participants (one each from the intervention and placebo group[s) withdrew at visit 2, before the first and second bolus, respectively (due to fear/inconvenience of blood tests), and two participants from the intervention group withdrew before visit 3 (due to the inconvenience of medical visits). After excluding doses not given due to study withdrawals, full-bolus retention was documented in 94% (85/90) of administered boluses: four patients (two each from the intervention and placebo groups) partially spit five doses. There was no evidence of unblinding among participants, nurses, or physicians (Additional file 3).
There was an overall statistically significant group difference in total serum ∆25OHD over time (57.8 (47.3, 68.2) nmol/L, p < 0.0001), with a significant time (p < 0.0001) and group*time interaction (p < 0.0001) effect (Fig. 2). Ten days following the first and second bolus, the group difference in the adjusted within-patient mean ∆25OHD from baseline was 119.3 (95% CI 105.8, 132.9) nmol/L and 100.1 (95% CI 85.7, 114.6) nmol/L, respectively, whereas the mean ∆25OHD at 3.5 months (6.4 (− 6.9, 19.7) nmol/L) and 7 months (5.3 (− 8.2, 18.9) nmol/L) was not statistically significant. The same held true when comparing crude or adjusted 25OHD serum values at various time points between groups (Fig. 3). All patients in the intervention group became vitamin D sufficient (≥ 75 nmol/L) 10 days after the first and second bolus compared to 48% (p = 0.0003) and 35% (p < 0.0001) of patients in the control group, respectively. Vitamin D sufficiency was maintained at 3.5 months in 63% vs. 39% (p = 0.12) and at 7 months in 56% vs. 36% (p = 0.22) in the intervention versus the control groups, respectively.
Change from baseline in serum 25-hydroxyvitamin D (25OHD) levels over 7 months. The adjusted mean change from baseline in 25OHD is presented with 95% confidence interval at each time point, in the vitamin D (filled circles) and placebo (open squares) groups over the 7-month study period; values were adjusted for vitamin D intake, ethnicity, sex, environmental tobacco exposure, school-days missed, and asthma management strategy. In the lower panel, the adjusted mean changes from baseline (95% CI) for each group and the adjusted mean group difference in the change from baseline (95% CI) are recorded at 10 days (d) (after 1st bolus), 3.5 months (mo), 3.5 months + 10 days (after 2nd bolus) and 7 months
Serum 25-hydroxyvitamin D (25OHD) levels over 7 months. The 25OHD values are presented by group at various time points. a Crude total serum 25OHD in the vitamin D (filled boxes) and control (open boxes) groups over the 7-month study period. The median is depicted by the horizontal bar, with the lower and upper limits of each box representing the 25% and 75%; these numerical values are also recorded in the lower panel as median (25%, 75%) at each time point. Error bars represent the minimum and maximum of the distribution. b Adjusted marginal means for the total serum 25OHD are presented in the vitamin D (filled circles) and control (open squares) groups over the 7-month study period, after adjustment for asthma phenotype, sex, ethnicity, environmental tobacco exposure, school-days missed, baseline vitamin D intake, baseline serum 25OHD, and asthma management strategy. Error bars represent the 95% confidence interval of the mean. In the lower panel, their numerical values are recorded by group at each point in time along with the adjusted mean group difference (95% CI). Using a generalised linear mixed model, a statistically significant overall group (p < 0.0001), time (p < 0.0001), and group*time (p < 0.0001) interaction was documented. In both graphs, the dotted line represents the 75 nmol/ L on the y-axis. Total 25OHD was comprised overwhelmingly of 25-hydroxyvitamin D3, with 3-epimer-25-hydroxyvitamin D3 and 25-hydroxyvitamin D2
Over the 7-month study period, patients experienced an average of 4 URTIs and 2–3 viral-induced asthma exacerbations, with no significant group difference in incidence. URTIs were more frequently reported verbally during monthly contact than documented on diaries. Participants experienced 41 exacerbations requiring rescue OCS (mean: 0.87/patient); more than half of participants made an ED visit and received OCS for asthma. No significant group difference was observed in healthcare utilisation, severity and average duration of asthma episodes, use of β2-agonists, or lost workdays or functional status of caregivers; observations were consistent across data sources (verbal report versus diaries) (Table 2).
Urinary Ca:Cr was normal in all but 9/104 (8.7%) intervention samples (N = 4 patients) and 12/117 (10.3%) placebo samples (N = 8 patients) at baseline or after randomisation, all with borderline abnormal values; no episode of hypercalciuria was associated with hypercalcaemia, decrease in alkaline phosphatase, or elevated (> 225 nmol/L) 25OHD, with one exception where the 25OHD was 231 nmol/L. Six patients in the intervention group had a 25OHD value > 225 nmol/L 10 days after the initial (N = 5 patients: 231–293 nmol/L) or the second (N = 1 patient: 237 nmol/L) bolus; only one episode was associated with borderline hypercalciuria (Ca:Cr 1.02) and none was associated with hypercalcaemia. Overall, 227 adverse health events were reported using MedDRA [36] (intervention, 96; control, 131), the most frequent being infections (N = 88, 39%) and general disorders (N = 47, 21%) (Additional file 4); one serious adverse health event, hospitalisation for pneumonia, occurred in the placebo group.
Discussion
In this group of high-morbidity preschool children with recurrent viral-induced exacerbation of asthma, two boluses of 100,000 IU vitamin D3 given once in the fall and once in the winter rapidly raised serum 25OHD and increased overall 25OHD compared to a placebo. However, at 3.5 months and 7 months the residual change from baseline in serum 25OHD was only modest and in both cases was not significantly different from that in the placebo group. This supplemental approach permitted the majority of, but not all, patients in the intervention group to achieve and maintain vitamin D above 75 nmol/L throughout the study.
Children living in countries at high latitude are recommended to take vitamin D supplementation during the fall and winter to maintain serum 25OHD at or above 75 nmol/L for bone health [35]. Despite the recommended average dietary requirement of 600 IU in children ≥ 1 year of age as set by the Institute of Medicine [37], our participants’ dietary intake was less than half the recommended intake, with barely 13% taking a vitamin D supplement, a finding concordant with that of our prior pilot study [21]. The majority of children were already vitamin D insufficient at baseline in the fall, probably as a result of a combination of factors, including low intake, sun protection practices, and skin colour [11, 38]. The lower dietary intake and lower serum 25OHD observed in participants contrasts with that of healthy and population-based Canadian preschoolers [39]. Perhaps the avoidance of milk due to the widespread belief that dairy products increase mucus production [40, 41] or less time spent outdoors because of respiratory symptoms triggered by physical activities or environmental allergies contribute to these findings in our young population in whom half were atopic. Nonetheless, our results indicate that preschoolers with asthma are at high risk of vitamin D insufficiency.
A bolus dose of 100,000 IU vitamin D, once in the fall and once in the winter, is recommended by the French Society of Paediatrics for healthy preschoolers [42] and has been shown to rapidly and safely raise blood 25OHD levels. With recent meta-analyses suggesting a beneficial effect of supplemental vitamin D on reducing the incidence of viral infections [22] and asthma exacerbations [23], a rapid increase in circulating 25OHD may be ideal to efficiently prevent the well-documented paediatric “September epidemic” of viral-induced asthma exacerbations in the Northern hemisphere [43]. Although the optimal posology to prevent asthma exacerbations is unknown, bolus doses previously appeared less protective against respiratory infections than daily doses in children; however, this approach was primarily tested in undernourished children as a means to prevent pneumonia [44, 45]. In contrast, a 2015 meta-analysis of paediatric trials strongly recommended the use of a bolus dose (< 300,000 IU), concluding that daily doses as high as 4000 IU were insufficient to rapidly raise serum 25OHD in vitamin D deficient children [46]. The present trial confirms that each loading dose of 100,000 IU rapidly raises serum 25OHD in predominantly vitamin D insufficient children, but is inadequate to maintain sufficiency in about 40% of children; indeed, only a nominal change from baseline of approximatively 5–6 nmol/L was maintained 3.5 months after each bolus. Our findings of an acute rise in 25OHD following each bolus is concordant with the prior literature [21, 47], as is the return to near baseline levels approximately 3.5 months post bolus [48, 49]. Despite our hope to avoid the need for daily supplementation, two boluses proved suboptimal in many young asthmatic children.
The combination of bolus and daily supplementation would appear more promising. Indeed, in our prior pilot study of asthmatic preschoolers [21], the control group, receiving only 400 IU daily vitamin D (with no bolus), had a slow but steady increase from baseline of 20 nmol/L at 3 months, with no further improvement despite ongoing supplementation; yet, only 55% reached 75 nmol/L after 3 months of supplementation, confirming this approach as suboptimal. In contrast, the intervention group in the same trial, receiving a single 100,000 IU bolus combined with 400 IU daily vitamin D3, displayed a rapid rise of 132 nmol/L in serum 25OHD within 10 days, with a clinically meaningful change from baseline of 27.1 nmol/L at 3 months, but little additional increase to 6 months. Whereas all patients in the intervention group had maintained serum 25OHD at ≥ 75 nmol/L at 3 months, it dropped to 88% by 6 months, suggesting the need for a second bolus. Admittedly, the target serum level for the immune and anti-inflammatory effect observed with vitamin D supplementation by Martineau and colleagues [22, 23] remains to be established. Collectively, the findings of our two pilot studies would support two loading doses of 100,000 IU spaced 3.5 months apart, combined with a daily dose of 400 IU throughout the fall and winter, as an optimal intervention to achieve a rapid and sustained increase in serum vitamin D in preschoolers with asthma.
No significant group difference was observed in the severity of asthma exacerbations or healthcare utilisation. The non-significant trend observed in several outcomes, which was not in favour of vitamin D, is likely random, but may also be explained by baseline group imbalances (despite adjustment); more children in the intervention group displayed several baseline characteristics associated with more severe asthma and lower vitamin D exposure (skin colour and dietary intake) compared to the control group.
The study contributes to accumulating evidence on the safety profile of 100,000 IU vitamin D boluses. Although several participants displayed elevated urinary Ca:Cr, blood calcium levels were normal in all cases, suggesting that hypercalciuria was perhaps due to an unbalanced diet or a non-fasting state. Moreover, all participants with elevated serum 25OHD had normocalcaemia. To date, only five published paediatric trials have tested an oral dose of 100,000 IU vitamin D, with just two reporting circulating 25OHD: two cases (0.3%) with 25OHD > 375 nmol/L occurred in one trial of malnourished Afghan infants [44] and two children (18%) with 25OHD > 250 nmol/L but no associated hypercalciuria or hypercalcaemia were reported in our prior pilot study [21]. In the three small trials reporting serum bone metabolism biomarkers in the paediatric population, no episodes of hypercalcaemia occurred [47, 49, 50]. Yet, additional safety data in larger samples are required.
We acknowledge several trial limitations and lessons learned. Due to its small sample size, this study resulted in baseline group imbalances and provided only preliminary process and efficacy data. However, in line with our prior trials using similar criteria [21, 50], the high morbidity of enrolled patients, evidenced by the frequency of exacerbations requiring rescue OCS in the preceding 12 months (≥ 2/child) and during the study period (0.87/child), confirmed the appropriateness of eligibility criteria and the ongoing health burden, despite ICS therapy. With two thirds of participants already vitamin D insufficient at baseline and the expected further decline during the winter, the pragmatic recruitment without pre-screening for vitamin D status appears justified. Whereas greater efficacy had been suggested in asthmatic patients with the lowest baseline 25OHD [23], randomising children irrespective of baseline vitamin D would provide the opportunity to explore the dose-response association with, and identify the optimal target for, immune and anti-inflammatory effect. The absence of clinically important change in dietary vitamin D intake over the study period suggests no evidence of Hawthorne bias. Tolerance of the 2-mL bolus was excellent with 94% of administered doses completely retained. Importantly, we documented the main outcome in all participants, despite an 11% dropout, with pre-approved consent to obtain drug and medical information at study endpoint. The twofold higher number of URTI and asthma exacerbations documented by monthly verbal versus diary report, suggests the need to facilitate diary completion, perhaps by offering electronic diaries, shown to improve veracity and adherence [51, 52]. Conducted in a single centre with multi-ethnic Canadian preschoolers with asthma, most of whom were vitamin D insufficient at baseline, the observed serum 25OHD response to two boluses of 100,000 IU may not apply to healthy children, other ethnic groups, or those with significantly higher (or lower) baseline vitamin D status or exposure. These lessons learned have been implemented in the ongoing, funded, large, multicenter, triple-blind, placebo-controlled trial testing two boluses of 100,000 IU with daily 400 IU of vitamin D in the same population (NCT 03365687).
Conclusion
The administration of an oral bolus of 100,000 IU vitamin-D3 in the fall, with a repeat dose in the winter, rapidly and significantly raises overall serum 25OHD in Canadian preschoolers with high-morbidity asthma, despite suboptimal dietary and sun exposure. While sufficient in slightly more than half of children, this strategy appears inadequate to maintain vitamin D sufficiency over 7 months in a notable proportion of this population.
Abbreviations
- 25OHD:
-
25-Hydroxyvitamin D
- ED:
-
Emergency department
- ICS:
-
Inhaled corticosteroids
- OCS:
-
Oral corticosteroids
- URTI:
-
Upper respiratory tract infection
References
Gershon AS, Guan J, Wang C, To T. Trends in asthma prevalence and incidence in Ontario, Canada, 1996-2005: a population study. Am J Epidemiol. 2010;172(6):728–36.
Moorman JE, Akinbami LJ, Bailey CM, Zahran HS, King ME, Johnson CA, Liu X. National surveillance of asthma: United States, 2001-2010. Vital Health Stat. 2012;3(35):1–58.
Rosychuk RJ, Voaklander DC, Klassen TP, Senthilselvan A, Marrie TJ, Rowe BH. Asthma presentations by children to emergency departments in a Canadian province: a population-based study. Pediatr Pulmonol. 2010;45(10):985–92.
Lougheed MD, Garvey N, Chapman KR, Cicutto L, Dales R, Day AG, Hopman WM, Lam M, Sears MR, Szpiro K, et al. The Ontario asthma regional variation study: emergency department visit rates and the relation to hospitalization rates. Chest. 2006;129(4):909–17.
Xepapadaki P, Papadopoulos NG. Childhood asthma and infection: virus-induced exacerbations as determinants and modifiers. Eur Respir J. 2010;36(2):438–45.
Ducharme FM, Zemek R, Chauhan BF, Gravel J, Chalut D, Poonai N, Guertin MC, Quach C, Blondeau L, Laberge S. Determinants of emergency department treatment failure in children with acute moderate or severe asthma: a cohort study. Lancet Respir Med. 2016;4(12):990–8.
Science M, Maguire JL, Russell ML, Smieja M, Walter SD, Loeb M. Low serum 25-hydroxyvitamin D level and risk of upper respiratory tract infection in children and adolescents. Clin Inf Dis. 2013;57(3):392–7.
Brehm JM, Schuemann B, Fuhlbrigge AL, Hollis BW, Strunk RC, Zeiger RS, Weiss ST, Litonjua AA. Serum vitamin D levels and severe asthma exacerbations in the childhood asthma management program study. J Allergy Clin Immunol. 2010;126(1):52–8 e55.
Searing DA, Zhang Y, Murphy JR, Hauk PJ, Goleva E, Leung DYM. Decreased serum vitamin D levels in children with asthma are associated with increased corticosteroid use. J Allergy Clin Immunol. 2010;125(5):995–1000.
Stoian CA, Lyon M, Cox RG, Stephure DK, Mah JK. Vitamin D concentrations among healthy children in Calgary, Alberta. Paediatr Child Health. 2011;16(2):82–6.
El Hayek J, Pham TT, Finch S, Hazell TJ, Jean-Philippe S, Vanstone CA, Agellon S, Rodd C, Rauch F, Weiler HA. Vitamin D status in Montreal preschoolers is satisfactory despite low vitamin D intake. J Nutr. 2013;143(2):154–60.
Whiting SJ, Langlois KA, Vatanparast H, Greene-Finestone LS. The vitamin D status of Canadians relative to the 2011 dietary reference intakes: an examination in children and adults with and without supplement use. Am J Clin Nutr. 2011;94(1):128–35.
Holick MF. Vitamin D: a D-Lightful health perspective. Nutr Rev. 2008;66(10 Suppl 2):S182–94.
Roth DE, Martz P, Yeo R, Prosser C, Bell M, Jones AB. Are national vitamin D guidelines sufficient to maintain adequate blood levels in children? Can J Public Health. 2005;96(6):443–9.
Turer CB, Lin H, Flores G. Prevalence of Vitamin D deficiency among overweight and obese US children. Pediatrics. 2013;131(1):e152–61.
Maguire JL, Birken CS, O’Connor DL, Macarthur C, Thorpe KE, Mamdani M, Parkin PC. Prevalence and predictors of low vitamin D concentrations in urban Canadian toddlers. Paediatr Child Health. 2011;16(2):e11–5.
Spiro A, Buttriss JL. Vitamin D: an overview of vitamin D status and intake in Europe. Nutr Bull. 2014;39(4):322–50.
Gupta A, Sjoukes A, Richards D, Banya W, Hawrylowicz C, Bush A, Saglani S. Relationship between serum vitamin D, disease severity, and airway remodeling in children with asthma. Am J Respir Crit Care Med. 2011;184(12):1342–9.
Maalmi H, Berraies A, Tangour E, Ammar J, Abid H, Hamzaoui K, Hamzaoui A. The impact of vitamin D deficiency on immune T cells in asthmatic children: a case-control study. J Asthma Allergy. 2012;5:11–9.
Bener A, Ehlayel MS, Tlulic MK, Hamid Q. Vitamin D deficiency as a strong predictor of asthma in children. Int Arch Allergy Immunol. 2012;157:168–75.
Jensen ME, Mailhot G, Alos N, Rousseau E, White JH, Khamessan A, Ducharme FM. Vitamin D intervention in preschoolers with viral-induced asthma (DIVA): a pilot randomised controlled trial. Trials. 2016;17(1):353.
Martineau AR, Jolliffe DA, Hooper RL, Greenberg L, Aloia JF, Bergman P, Dubnov-Raz G, Esposito S, Ganmaa D, Ginde AA, et al. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. Br Med J. 2017;356:i6583.
Jolliffe DA, Greenberg L, Hooper RL, Griffiths CJ, Camargo CA Jr, Kerley CP, Jensen ME, Mauger D, Stelmach I, Urashima M, et al. Vitamin D supplementation to prevent asthma exacerbations: a systematic review and meta-analysis of individual participant data. Lancet Respir Med. 2017;5(11):881–90.
World Medical A. World medical association declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–4.
Ducharme FM, Dell SD, Radhakrishnan D, Grad RM, Watson WT, Yang CL, Zelman M. Diagnosis and management of asthma in preschoolers: a Canadian Thoracic Society and Canadian Paediatric Society position paper. Can Respir J. 2015;22(3):135–43.
23Asher MI, Keil U, Anderson HR, Beasley R, Crane J, Martinez F, Mitchell EA, Pearce N, Sibbald B, Stewart AW, et al. International Study of Asthma and Allergies in Childhood (ISAAC): rationale and methods. Eur Respir J. 1995;8(3):483–91.
Pritchard JM, Seechurn T, Atkinson SA. A food frequency questionnaire for the assessment of calcium, vitamin D and vitamin K: a pilot validation study. Nutrients. 2010;2(8):805–19.
van den Ouweland JM, Vogeser M, Bacher S. Vitamin D and metabolites measurement by tandem mass spectrometry. Rev Endocr Metab Disord. 2013;14(2):159–84.
Jensen ME, Ducharme FM, Theoret Y, Belanger AS, Delvin E. Assessing vitamin D nutritional status: is capillary blood adequate? Clin Chim Acta. 2016;457:59–62.
Ducharme FM, Jensen ME, Mendelson MJ, Parkin PC, Desplats E, Zhang X, Platt R. Asthma flare-up diary for young children to monitor the severity of exacerbations. J Allergy Clin Immunol. 2016;137(3):744–9 e746.
Jensen ME, Mendelson MJ, Desplats E, Zhang X, Platt R, Ducharme FM. Caregiver's functional status during a young child's asthma exacerbation: A validated instrument. J Allergy Clin Immunol 2016:782-8.
Diaz-Quijano FA. A simple method for estimating relative risk using logistic regression. BMC Med Res Methodol 2012;12:14
Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol. 1988;124(6):869–71.
IOM (Institute of Medicine). Dietary reference intakes for calcium and vitamin D. Washington DC: The National Academies Press; 2011.
Holick MF. Vitamin D deficiency. New Engl J Med. 2007;357(3):266–81.
International Federation of Pharmaceutical Manufacturers and Associations. Preferred terms. In: MedDRA introductory guide version 140. Chantilly: Harmonisation for better health; 2011. p. 9.
Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK, Durazo-Arvizu RA, Gallagher JC, Gallo RL, Jones G, et al. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab. 2011;96(1):53–8.
Aglipay M, Birken CS, Parkin PC, Loeb MB, Thorpe K, Chen Y, Laupacis A, Mamdani M, Macarthur C, Hoch JS, et al. Effect of high-dose vs standard-dose wintertime vitamin D supplementation on viral upper respiratory tract infections in young healthy children. JAMA. 2017;318(3):245–54.
Munasinghe LL, Yuan Y, Willows ND, Faught EL, Ekwaru JP, Veugelers PJ. Vitamin D deficiency and sufficiency among Canadian children residing at high latitude following the revision of the RDA of vitamin D intake in 2010. Br J Nutr. 2017;117(3):457–65.
Thiara G, Goldman RD. Milk consumption and mucus production in children with asthma. Can Fam Physician. 2012;58(2):165–6.
Lee C, Dozor AJ. Do you believe milk makes mucus? Arch Pediatr Adolesc Med. 2004;158(6):601–3.
Vidailhet M, Mallet E, Bocquet A, Bresson JL, Briend A, Chouraqui JP, Darmaun D, Dupont C, Frelut ML, Ghisolfi J, et al. Vitamin D: still a topical matter in children and adolescents. A position paper by the Committee on Nutrition of the French Society of Paediatrics. Arch Pediatr. 2012;19(3):316–28.
Johnston NW, Johnston SL, Duncan JM, Greene JM, Kebadze T, Keith PK, Roy M, Waserman S, Sears MR. The September epidemic of asthma exacerbations in children: a search for etiology. J Allergy Clin Immunol. 2005;115(1):132–8.
Manaseki-Holland S, Qader G, Isaq Masher M, Bruce J, Zulf Mughal M, Chandramohan D, Walraven G. Effects of vitamin D supplementation to children diagnosed with pneumonia in Kabul: a randomised controlled trial. Tropical Med Int Health. 2010;15(10):1148–55.
Manaseki-Holland S, Maroof Z, Bruce J, Mughal MZ, Masher MI, Bhutta ZA, Walraven G, Chandramohan D. Effect on the incidence of pneumonia of vitamin D supplementation by quarterly bolus dose to infants in Kabul: a randomised controlled superiority trial. Lancet. 2012;379(9824):1419–27.
McNally JD, Iliriani K, Pojsupap S, Sampson M, O’Hearn K, McIntyre L, Fergusson D, Menon K. Rapid normalization of vitamin D levels: a meta-analysis. Pediatrics. 2015;135(1):e152–66.
Tau C, Ciriani V, Scaiola E, Acuna M. Twice single doses of 100,000 IU of vitamin D in winter is adequate and safe for prevention of vitamin D deficiency in healthy children from Ushuaia, Tierra Del Fuego, Argentina. J Steroid Biochem Mol Biol. 2007;103(3–5):651–4.
Ilahi M, Armas LA, Heaney RP. Pharmacokinetics of a single, large dose of cholecalciferol. Am J Clin Nutr. 2008;87(3):688–91.
Arpadi SM, McMahon D, Abrams EJ, Bamji M, Purswani M, Engelson ES, Horlick M, Shane E. Effect of bimonthly supplementation with oral cholecalciferol on serum 25-hydroxyvitamin D concentrations in HIV-infected children and adolescents. Pediatrics. 2009;123(1):e121–6.
Ducharme FM, Lemire C, Noya FJ, Davis GM, Alos N, Leblond H, Savdie C, Collet JP, Khomenko L, Rivard G, et al. Preemptive use of high-dose fluticasone for virus-induced wheezing in young children. New Engl J Med. 2009;360(4):339–53.
Hufford MR, Stone AA, Shiffman S, Schwartz JE, Broderick JE. Paper vs. electronic diaries: compliance and subject evaluations. Appl Clin Trials. 2002;11(8):38–43.
Voorend-van Bergen S, Vaessen-Verberne AA, Landstra AM, Brackel HJ, van den Berg NJ, Caudri D, de Jongste JC, Merkus PJ, Pijnenburg MW. Monitoring childhood asthma: Web-based diaries and the asthma control test. J Allergy Clin Immunol. 2014;133(6):1599–605 e1592.
Acknowledgements
This work was funded through two research bridge-funding grants (# 313322 and 142741) of the Canadian Institutes of Health Research (CIHR). The Sainte-Justine Research Centre is supported by the Fonds de la recherche en Santé au Québec. We acknowledge the support given by Euro-Pharm International Canada for developing and donating the active and placebo bolus vitamin-D3 supplementation. We sincerely thank Christine Lord and Suzanne Taillefer for their contribution to coordination and overall support of the project; the research nurses, Christine Massicotte and Caroline Champagne for patient recruitment and follow-up; and Viet Anh Tran for statistical support. We thank the staff and physicians of the asthma and respiratory clinics, emergency department, and hospital wards for their collaboration; and sincerely thank the parents and children for their participation and feedback on the study.
Funding
This work was funded through two research bridge-funding grants (# 313322 and 142741) of the CIHR. The funders had no role in the design, collection, analysis and interpretation of data, or in the writing of the manuscript.
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
FMD designed the study, obtained funding, oversaw the project, supervised the analysis, and interpreted and wrote the manuscript. MJ and GM were involved in study design and were responsible for the dietary assessment. NA was responsible for overseeing safety aspects of the study. JW and ER provided intellectual input into the design and interpretation of the vitamin D results. SMT assisted in the conduct of the study. AK designed the study drug formulation. BV conducted the statistical analyses. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Parents provided written informed consent for their child’s study participation and for the release of medical and pharmacy data. The Institutional Research Ethics Board of the Sainte-Justine University Health Centre (#2015–786, 4004) and Health Canada approved the study (#187438).
Consent for publication
Not applicable.
Competing interests
Euro-Pharm (Montreal, Canada) elaborated and donated the study drug formulation, but had no input in the study design, conduct, analysis, and writing of the study. The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Consolidated Standards of Reporting Trials (CONSORT) 2010 checklist of information to include when reporting a randomised trial. (DOC 217 kb)
Additional file 2:
Study intervention and procedures. (xlsx 14 kb)
Additional file 3:
Study mechanics. (xlsx 15 kb)
Additional file 4:
Adverse health events. (xlsx 13 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Ducharme, F.M., Jensen, M., Mailhot, G. et al. Impact of two oral doses of 100,000 IU of vitamin D3 in preschoolers with viral-induced asthma: a pilot randomised controlled trial. Trials 20, 138 (2019). https://doi.org/10.1186/s13063-019-3184-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-019-3184-z