Abstract
Background
Current guidelines for the diagnosis and management of patients with stable coronary artery disease (CAD) recommend functional stress testing for risk stratification prior to revascularization procedures. Cardiac magnetic resonance imaging (CMR) is a modality of choice for stress testing because of its capability to detect myocardial ischemia sensitively and specifically. Nevertheless, evidence from randomized trials evaluating a CMR-based management of stable CAD patients in comparison to a more common angiography-based approach still is limited.
Methods/design
Patients presenting themselves with symptoms indicating a stable CAD and a class I or IIa indication for diagnostic coronary angiography are prospectively screened and enrolled in the study. All subjects receive a basic cardiological work-up and guideline-directed medical therapy. A 1:1 randomization in two groups is being performed. Patients in group 1 undergo diagnostic coronary angiography and subsequent revascularization according to current guidelines. Subjects in group 2 undergo adenosine stress CMR and in case of myocardial ischemia are sent to coronary angiography. Follow-up is planned for 3 years. During this time, the number of primary endpoints (defined as cardiac death and non-fatal myocardial infarction) and unplanned invasive procedures will be documented. Furthermore, symptom burden and quality of life will be assessed by use of the Seattle Angina Questionnaire. Sample size is calculated to prove non-inferiority of the CMR-based approach.
Discussion
In case this study is able to accomplish its aim to prove non-inferiority of the CMR-based management in patients with stable CAD; the importance of this emerging modality may further increase.
Trial registration
ClinicalTrials.gov, identifier: NCT02580851. Registered on 14 October 2015. Unique Protocol ID: 237/11
Similar content being viewed by others
Background
Current guidelines for the diagnosis and management of patients with stable coronary artery disease (CAD) recommend – besides thorough history and physical examination – proper risk stratification and non-invasive detection of myocardial ischemia prior to invasive therapy [1, 2]. The detection or exclusion of moderate to severe reversible myocardial ischemia is a crucial part of the work-up process. When ischemia is present, patients are designated to a high-risk group with a high probability of having a prognostic benefit from revascularization procedures [3,4,5]. Patients without ischemia do not seem to benefit from revascularization over optimal medical therapy, at least with regard to prognosis [6]. This emphasizes the need for functional testing prior to therapeutic decisions.
Adenosine perfusion cardiac magnetic resonance imaging (CMR) is an imaging modality which is able to reliably detect reversible myocardial ischemia and thus plays an increasing role in the diagnosis and risk stratification of patients with suspected or known CAD [7,8,9,10,11]. Though CMR, therefore, is highly recommended in the diagnostic work-up of stable CAD patients, there is only one study evaluating a CMR-driven approach in patient management with regard to the occurrence of major cardiac events [12].
Invasive coronary angiography still is considered to be the “gold-standard” for the diagnosis of CAD, though it exhibits several limitations and shortcomings. Multiple studies have documented the significant interobserver variability in the grading of coronary artery stenosis, as well as the frequent occurrence of under- and overestimation of hemodynamic relevance [13, 14]. One has to conclude that coronary angiography may provide anatomical information but is not the modality of choice concerning the detection of myocardial ischemia. This is of special interest, as there is a reported frequency of complications due to diagnostic coronary angiographies of about 1.5% [15]. Nevertheless, coronary angiography remains the most often performed diagnostic test in the setting of stable CAD, with more than one half of elective percutaneous coronary interventions (PCI) done without previous stress testing [16].
The objective of our study is to show that a CMR-based conservative or invasive management of patients with suspected or known CAD is not inferior with regard to major cardiac endpoints and quality of life in comparison to a – more conventional – coronary angiography-based approach. We assume that a significant number of diagnostic coronary angiographies and PCI could be spared without decrease in patient safety and comfort. Therefore, we designed this single-center, open-label, randomized controlled trial to test for non-inferiority of the two diagnostic groups.
Methods/design
General information
This study has been approved by the local Ethics Committee of our university (Ethikkommission der Universität Ulm, Chairman Prof. Dr. Oliver Zolk, reference number 237/11, Additional file 1). It has been partially funded by Guerbet Germany, Sulzbach, Germany (see Additional file 2 for funding contract). The funder does not have any influence concerning study design, data collection, analysis and the decision to submit the report. Other financial expenses and the involved personal are provided by our own institution.
As our study is an investigator-initiated, single-center trial (academic hospital, Germany) there is no coordinating center or steering committee. Patient enrollment, endpoint adjudication and data management will be carried out by the authors of this protocol independently from the sponsor. To monitor the conduction of the trial, the members of the Investigator Committee meet on a regular basis and exceptionally when concerns arise.
Participants are covered by the academic hospital in case harm should occur in the context of this trial. Provisions are not intended.
The study is registered at ClinicalTrials.gov (identifier: NCT02580851). Protocol modification will be communicated to the ethics committee and will be documented at ClinicalTrials.gov. The adapted Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) Checklist is attached as Additional file 3.
After completion of the trial, publication of the results is intended in a peer-reviewed scientific journal. Publication will only be carried by the authors of this manuscript without the help of professional writers. Granting full access to the protocol or participant-level dataset is not intended.
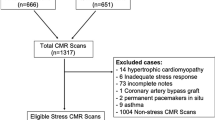
Patient recruitment
Generally, informed consent will be obtained by the investigators after personal elucidation from all participants prior to enrollment in the study. All patients presenting themselves in the outpatient clinic of our university hospital for the evaluation of symptoms indicating a stable CAD (e.g., exercise-related angina pectoris or dyspnea) will be screened prospectively. Patients at intermediate to high risk (according to recommended risk scores) and a class I or IIa indication for diagnostic coronary angiography (Additional file 4: Table S1) will be considered eligible unless they exhibit the following exclusion criteria: unstable angina pectoris, cardiac or respiratory instability, contraindication for CMR examination [17], known allergy to gadolinium-based contrast agents, impaired renal function (glomerular filtration rate <30 ml/min), contraindication or allergy to adenosine, pregnancy, age below18 years and inability to give written informed consent. It is irrelevant whether a CAD has already been diagnosed at the time of first presentation.
Protocol
All patients receive thorough history-taking, physical examination and a basic cardiological work-up including rest electrocardiogram, treadmill testing and echocardiography. Further prediagnostics (e.g., stress-echocardiography) is allowed and the respective results will be documented. According to general recommendations, risk stratification scores for each individual are calculated [18, 19]. In order to assess symptom burden and quality of life, the standardized Seattle Angina Questionnaire (SAQ) is carried out in each subject [20, 21]. All patients receive guideline-directed medical therapy (GDMT) [1].
Patients are randomized in two groups in a 1:1 fashion (blocked computer-generated random numbers). The allocation sequence is only available to a designated study nurse who will be phoned in case of an allocation. The trial is designed in an open-label fashion, i.e., there is no blinding after the initial allocation.
In group 1, patients directly undergo diagnostic coronary angiography. A PCI is performed according to current guidelines in case of ≥70% stenosis in a coronary vessel with ≥2-mm diameter [1, 2] or hemodynamically relevant stenoses in fractional flow reserve (FFR) testing.
Subjects in group 2 initially receive adenosine perfusion CMR for functional testing. The examination is conducted on a 3.0-Tesla whole-body scanner with a 32-channel phased-array cardiac receiver coil according to a well-established standard protocol [22,23,24]. In case reversible ischemia can be detected, subjects are sent to coronary angiography and PCI afterwards. Additional file 5: Figure S1 provides the study flowchart.
In case of progressive or insufficient symptom control, patients of group 2 (CMR group) are also evaluated for an invasive therapeutic approach. The following procedures will be documented.
There are no other diagnostic or therapeutic interventions planned or prohibited in the setting of this trial.
Follow-up
Adherence will be achieved by regular contact between the study personal and the participants. Follow-up information is gathered on a yearly basis after enrollment by outpatient clinic visits and by telephone interviews of patients and their general practitioners. Any reported adverse event will be reported and its significance evaluated by the investigators. At this time point, interim analyses will be performed by the investigators. The study will be stopped by the investigators if a safety concern arises that prohibits the continuation of the trial.
The primary endpoint is defined as cardiac death (defined as in [25]) and non-fatal myocardial infarction according to the current universal definition [26]. Any diagnostic or interventional coronary procedure that has not been scheduled at the time of the initial diagnostic work-up will be recorded as an unplanned procedure. Symptom burden and quality of life are assessed by SAQ each year. A follow-up period of 3 years is planned for each patient. Standardized follow-up forms have been established and are available at our institution. If consent is withdrawn by a participant, the data that has already been collected will be removed from further analysis.
Figure 1 shows the study schedule according to the populated SPIRIT figure.
Sample size prediction/statistics
It has been shown that the annual event rate for the defined primary endpoint is 6.3% in case of a pathological and 1.0% in case of a normal CMR examination [27]. Retrospective analysis of our data revealed a 30% rate of pathological CMR examinations during the last years, thus the expected annual event rate would be 2.59% for the whole primary CMR group. In patients primarily undergoing coronary angiography, pooled annual event rates have been shown to be about 6% [6, 28]. For the sample size prediction, a Fisher’s exact test with a power of 80% and a p value indicating significance of < .05 was used. The study was designed to prove non-inferiority with a defined non-inferiority margin of 1% within a 3-year follow-up period. This lead to a predicted sample size of 90 participants per group. Taking dropout rate and safety margin into account, we plan to enroll 100 patients into each group. Annual interim analyses will be performed to evaluate the need for further enrollment in case of insufficient event rates for an appropriate statistical analysis.
The following statistical tests will be used after completion of follow-up: to test the relationship between categorical classification factors, the chi-squared test will be applied. Continuous variables will be tested for normal distribution by the D’Agostino-Pearson test. In case of a normal distribution, variables will be reported as mean ± standard deviation and a two-tailed t test will be applied for comparison. Variables without normal distribution will be reported as median with percentiles and the Mann-Whitney rank-sum test will be used for comparison. As mentioned above, Fisher’s exact test will be applied to test for non-inferiority of the event rates of both groups. Overall, a p value ≤ .05 will be judged significant.
Data management will only be carried out by trained personal. The database is stored on protected servers of the academic hospital.
Discussion
In contrast to the recommendations given in current guidelines, diagnostic coronary angiography remains the most often applied modality in the evaluation of patients with stable CAD [1, 2]. In consequence, a high rate of angiographies without detection of obstructive CAD results [13, 15]. This is of special interest, as there is a remarkable frequency of complications associated with this procedure [15]. On the other hand, many diagnostic angiographies are followed by interventional revascularization procedures without prior functional assessment of visually detected coronary stenosis [16]. Taken together, expansion of invasive diagnostic and therapeutic procedures lead to a growing economic burden stressing health care systems without evidence for ameliorated patient care [6].
CMR is an important diagnostic modality in the growing arsenal of cardiology. Its ability to reliably and simultaneously evaluate global cardiac function and myocardial ischemia has been proven previously [11]. In particular, the high negative predictive value of a normal CMR examination with regard to the occurrence of major cardiac endpoints predisposes this modality to act as gatekeeper prior to revascularization strategies [29].
To the best of our knowledge, there is only one study prospectively randomizing patients to a CMR-driven versus an angiography-driven management strategy [12]: the MR-INFORM trial was a randomized multicenter study comparing a FFR- versus a CMR-based management approach of stable CAD patients. Non-inferiority of the CMR-based strategy could be demonstrated within a 12-month follow-up. In the present trial, a follow-up for up to 3 years is planned for every patient, thus providing information on long-term outcomes for each management strategy. Moreover, besides major clinical endpoints, symptom burden and quality of life will also be assessed. This is of special interest since clinical decision-making always should be based on patient comfort and satisfaction.
If the present study can accomplish its aim to prove non-inferiority of the CMR-based approach in the management of patients with stable CAD, its importance may further increase. This might result in a reduction of adverse events associated with coronary angiographies and revascularization procedures. This trial, therefore, aims to contribute important evidence with regard to the management of stable CAD patients.
Trial status
At the time of submission, patient recruitment is ongoing.
Abbreviations
- CAD:
-
Coronary artery disease
- CMR:
-
Cardiac magnetic resonance imaging
- FFR:
-
Fractional flow reserve
- GDMT:
-
Guideline-directed medical therapy
- PCI:
-
Percutaneous coronary intervention
References
Fihn SD, Gardin JM, Abrams J, Berra K, Blankenship JC, Dallas AP, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2012;126:e354–471.
Fihn SD, Blankenship JC, Alexander KP, Bittl JA, Byrne JG, Fletcher BJ, et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2014;130:1749–67.
Shaw LJ, Berman DS, Picard MH, Friedrich MG, Kwong RY, Stone GW, et al. Comparative definitions for moderate-severe ischemia in stress nuclear, echocardiography, and magnetic resonance imaging. JACC Cardiovasc Imaging. 2014;7:593–604.
Hachamovitch R, Rozanski A, Hayes SW, Thomson LE, Germano G, Friedman JD, et al. Predicting therapeutic benefit from myocardial revascularization procedures: are measurements of both resting left ventricular ejection fraction and stress-induced myocardial ischemia necessary? J Nucl Cardiol. 2006;13:768–78.
Hachamovitch R, Rozanski A, Shaw LJ, Stone HW, Thomson LE, Friedman JD, et al. Impact of ischaemia and scar on the therapeutic benefit derived from myocardial revascularization vs. medical therapy among patients undergoing stress-rest myocardial perfusion scintigraphy. Eur Heart J. 2011;32:1012–24.
Boden WE, O’Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356:1503–16.
Groothuis JG, Beek AM, Brinckman SL, Meijerink MR, van den Oever ML, Hofman MB, et al. Combined non-invasive functional and anatomical diagnostic work-up in clinical practice: the magnetic resonance and computed tomography in suspected coronary artery disease (MARCC) study. Eur Heart J. 2013;34:1990–8.
Buckert D, Dewes P, Walcher T, Rottbauer W, Bernhardt P. Intermediate-term prognostic value of reversible perfusion deficit diagnosed by adenosine CMR: a prospective follow-up study in a consecutive patient population. JACC Cardiovasc Imaging. 2013;6:56–63.
Bruder O, Wagner A, Lombardi M, Schwitter J, van Rossum A, Pilz G, et al. European Cardiovascular Magnetic Resonance (EuroCMR) registry—multi-national results from 57 centers in 15 countries. J Cardiovasc Magn Reson. 2013;15:9.
Coelho-Filho OR, Seabra LF, Mongeon FP, Abdullah SM, Francis SA, Blankstein R, et al. Stress myocardial perfusion imaging by CMR provides strong prognostic value to cardiac events regardless of patient’s sex. JACC Cardiovasc Imaging. 2011;4:850–61.
Bingham SE, Hachamovitch R. Incremental prognostic significance of combined cardiac magnetic resonance imaging, adenosine stress perfusion, delayed enhancement, and left ventricular function over preimaging information for the prediction of adverse events. Circulation. 2011;123:1509–18.
Hussain ST, Paul M, Plein S, McCann GP, Shah AM, Marber MS, et al. Design and rationale of the MR-INFORM study: stress perfusion cardiovascular magnetic resonance imaging to guide the management of patients with stable coronary artery disease. J Cardiovasc Magn Reson. 2012;14:65.
Nallamothu BK, Spertus JA, Lansky AJ, Cohen DJ, Jones PG, Kureshi F, et al. Comparison of clinical interpretation with visual assessment and quantitative angiography in patients undergoing percutaneous coronary intervention in contemporary practice: the Assessing Angiography (A2) project. Circulation. 2013;127:1793–800.
Kern MJ, Samady H. Current concepts of integrated coronary physiology in the catheterization laboratory. J Am Coll Cardiol. 2010;55:173–85.
Dehmer GJ, Weaver D, Roe MT, Milford-Beland S, Fitzgerald S, Hermann A, et al. A contemporary view of diagnostic cardiac catheterization and percutaneous coronary intervention in the United States: a report from the CathPCI Registry of the National Cardiovascular Data Registry, 2010 through 2011. J Am Coll Cardiol. 2012;60:2017–31.
Lin GA, Dudley RA, Lucas FL, Malenka DJ, Vittinghoff E, Redberg R. Frequency of stress testing to document ischemia prior to elective percutaneous coronary intervention. JAMA. 2008;300:1765–73.
Prasad SK, Pennell DJ. Safety of cardiovascular magnetic resonance in patients with cardiovascular implants and devices. Heart. 2004;90:1241–4.
D’Agostino Sr RB, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743–53.
Assmann G, Cullen P, Schulte H. Simple scoring scheme for calculating the risk of coronary events based on the 10-year follow-up of the prospective cardiovascular Münster (PROCAM) study. Circulation. 2002;105:30–5.
Spertus JA, Winder JA, Dewhurst TA, Deya RA, Prodzinski J, McDonell M, et al. Development and evaluation of the Seattle Angina Questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995;25:333–41.
Dougherty CM, Dewhurst T, Nichol WP, Spertus J. Comparison of three quality of life instruments in stable angina pectoris: Seattle Angina Questionnaire, Short Form Health Survey (SF-36), and Quality of Life Index-Cardiac Version III. J Clin Epidemiol. 1998;51:569–75.
Kramer CM, Barkhausen J, Flamm SD, Kim RJ, Nagel E, Society for Cardiovascular Magnetic Resonance Board of Trustees Task Force on Standardized Protocols. Standardized cardiovascular magnetic resonance (CMR) protocols 2013 update. J Cardiovasc Magn Reson. 2013;15:91.
Schulz-Menger J, Bluemke DA, Bremerich J, Flamm SD, Fogel MA, Friedrich MG, et al. Standardized image interpretation and post processing in cardiovascular magnetic resonance: Society for Cardiovascular Magnetic Resonance (SCMR) board of trustees task force on standardized post processing. J Cardiovasc Magn Reson. 2013;15:35.
Bernhardt P, Walcher T, Rottbauer W, Wöhrle J. Quantification of myocardial perfusion reserve at 1.5 and 3.0 Tesla: a comparison to fractional flow reserve. Int J Cardiovasc Imaging. 2012;28:2049–56.
Hicks KA, Tcheng JE, Bozkurt B, Chaitman BR, Cutlip DE, Farb A, et al. 2014 ACC/AHA key data elements and definitions for cardiovascular endpoint events in clinical trials: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Data Standards (Writing Committee to Develop Cardiovascular Endpoints Data Standards). J Am Coll Cardiol. 2015;66:403–69.
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Writing Group on behalf of the Joint ESC/ACCF/AHA/WHF Task Force for the Universal Definition of Myocardial Infarction. Third universal definition of myocardial infarction. Glob Heart. 2012;7:275–95.
Steel K, Broderick R, Gandla V, Larose E, Resnic F, Jerosch-Herold M, et al. Complementary prognostic values of stress myocardial perfusion and late gadolinium enhancement imaging by cardiac magnetic resonance in patients with known or suspected coronary artery disease. Circulation. 2009;120:1390–400.
Hemingway H, Chen R, Junghans C, Timmis A, Eldrigde S, Black N, et al. Appropriateness criteria for coronary angiography in angina: reliability and validity. Ann Intern Med. 2008;149:221–31.
Pilz G, Jeske A, Klos M, Ali E, Hoefling B, et al. Prognostic value of normal adenosine-stress cardiac magnetic resonance imaging. Am J Cardiol. 2008;101:1408–12.
Acknowledgements
Not applicable.
Funding
This trial has been partially funded by Guerbet Germany, Sulzbach, Germany (see Additional file 2 for funding contract). The funder does not have any influence concerning study design, data collection, analysis or the decision to submit the report. Other financial expenses and the involved personal are provided by our own institution.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
DB participated in the design of the study, carried out patient enrollment, performed the statistical analysis and drafted the manuscript. SW carried out patient enrollment and follow-up and helped to perform the statistical analysis. MC participated in patient enrollment and helped to draft the manuscript. RT participated in patient enrollment and helped to draft the manuscript. WR participated in the design of the study and its coordination. PB conceived of the study and participated in its design and coordination, carried out patient enrollment and helped to draft the manuscript. All authors read and approved the manuscript. Only the abovementioned persons will have access to the final dataset.
Corresponding author
Ethics declarations
Authors’ information
The authors have provided an additional personal cover letter to highlight the changes made to the manuscript since the first submission (Fig. 1).
Ethics approval and consent to participate
This study has been approved by the local Ethics Committee of our university (Ethikkommission der Universität Ulm, Chairman Prof. Dr. Oliver Zolk, reference number 237/11, Additional file 1). Informed consent will be obtained from all participants by the named investigators after personal elucidation.
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Ethics approval document. (JPG 766 kb)
Additional file 2:
Funding contract. (PDF 1 mb)
Additional file 3:
SPIRIT Checklist. (DOC 118 kb)
Additional file 4:
Table S1. Indications for coronary angiography. (DOCX 11 kb)
Additional file 5:
Figure S1. Flowchart depicting study protocol. GDMT – guideline-directed medical therapy. (DOCX 31 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Buckert, D., Witzel, S., Cieslik, M. et al. Magnetic resonance Adenosine perfusion imaging as Gatekeeper of invasive coronary intervention (MAGnet): study protocol for a randomized controlled trial. Trials 18, 358 (2017). https://doi.org/10.1186/s13063-017-2101-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-017-2101-6