Abstract
Background
The treatment of depression remains a challenge since at least 40% of patients do not respond to initial antidepressant therapy and 20% present chronic symptoms (more than 2 years despite standard treatment administered correctly). Repetitive transcranial magnetic stimulation (rTMS) is an effective adjuvant therapy but still not ideal. Intermittent Theta Burst Stimulation (iTBS), which has only been used recently in clinical practice, could have a faster and more intense effect compared to conventional protocols, including 10-Hz high-frequency rTMS (HF-rTMS). However, no controlled study has so far highlighted the superiority of iTBS in resistant unipolar depression.
Methods/design
This paper focuses on the design of a randomised, controlled, double-blind, single-centre study with two parallel arms, carried out in France, in an attempt to assess the efficacy of an iTBS protocol versus a standard HF- rTMS protocol. Sixty patients aged between 18 and 75 years of age will be enrolled. They must be diagnosed with major depressive disorder persisting despite treatment with two antidepressants at an effective dose over a period of 6 weeks during the current episode. The study will consist of two phases: a treatment phase comprising 20 sessions of rTMS to the left dorsolateral prefrontal cortex, localised via a neuronavigation system and a 6-month longitudinal follow-up. The primary endpoint will be the number of responders per group, defined by a decrease of at least 50% in the initial score on the Montgomery and Asberg Rating Scale (MADRS) at the end of rTMS sessions. The secondary endpoints will be: response rate 1 month after rTMS sessions; number of remissions defined by a MADRS score of <8 at the endpoint and 1 month after; the number of responses and remissions maintained over the next 6 months; quality of life; and the presence of predictive markers of the therapeutic response: clinical (dimensional scales), neuropsychological (evaluation of cognitive functions), motor (objective motor testing) and neurophysiological (cortical excitability measurements).
Discussion
The purpose of our study is to check the assumption of iTBS superiority in the management of unipolar depression and we will discuss its effect over time. In case of a significant increase in the number of therapeutic responses with a prolonged effect, the iTBS protocol could be considered a first-line protocol in resistant unipolar depression.
Trial registration
ClinicalTrials.gov, Identifier NCT02376491. Registered on 17 February 2015 at http://clinicaltrials.gov.
Similar content being viewed by others
Background
Depression is a real public health problem. In 2020, according to the World Health Organisation (WHO), depression will be the second major cause of handicap and premature death in the world after coronary diseases. Standard treatment comprises support therapy combined with medication. However, at least 40% of patients do not respond to the initial treatment and 20% present with persistent resistance to conventional pharmacological treatments [1]. It is, therefore, essential to find efficient treatment alternatives for resistant depression. The reference treatment in this case is still electroconvulsive therapy (ECT) with a 48% response rate in the event of severe resistance to pharmacological therapies [2]. Repetitive transcranial magnetic stimulation (rTMS) is a non-invasive, focal, cortical stimulation technique involving modulation of cortical excitability. It is an upstream alternative to ECT and could close to match comparable efficacy in the absence of psychotic symptoms with a satisfactory duration and number of stimuli [3, 4]. Its interest in the treatment of resistant unipolar depression has clearly been established in conjunction with antidepressant chemotherapy.
The efficacy of rTMS depends on its parameters (stimulation site, orientation of the magnetic field, number of stimuli delivered as well as the frequency, intensity and duration of stimulation) [5]. The two types of dorsolateral prefrontal cortex (DLPFC) stimulation used in the treatment of depression – high frequency to the left (L-HF) and low frequency to the right (R-LF) – have proved to be equi-effective [6–9]. Response rates on average vary from 30 to 40% depending on the series [10, 11], with a 58% response rate maintained at 3 months, then 33% at 6 months [12, 13].
Although these various parameters currently have yet to be optimised, a new rTMS technique known as Theta Burst Stimulation (TBS) has recently emerged. This displays faster, more robust action compared to conventional protocols [14], with excellent tolerability [15], provided that safety recommendations are followed [16]. Two different methods have been described: intermittent (iTBS) and continuous Theta Burst Stimulation (cTBS) with facilitating and inhibitory effects, respectively. iTBS involves the application of bursts of three pulses at a frequency of 50 Hz every 200 ms; therefore, at 5 Hz, delivery is over 2 s and repeated every 10 s, 20 times in succession. An uncontrolled study on a small sample generated 70% of responses and 42% of remissions in resistant unipolar depression following a course of iTBS [17]. These shorter sessions would be an additional source of comfort for the patient not to mention the lower cost of the session. It should be noted that a very recent study highlighted the superiority of iTBS over cTBS and placebo in the management of resistant depression [18]. In 2014, Bakker et al. demonstrated similar efficacy with iTBS prefrontal dorsomedial bilateral stimulation (6 min) and a 10-Hz protocol (30 min) in an uncontrolled retrospective study [19]. With regard to recent scientific literature, various points must be specifically investigated: controlled comparison of protocols with the enrolment of a homogeneous population in terms of treatment and clinical form of the condition (most studies combine both bipolar and unipolar disorder); duration of the effect with longitudinal follow-up; and predictive response factors [20]. The main predictive therapeutic response factors identified to date are age, duration of the episode, degree of therapeutic resistance, clinical profile and, in particular, cognitive impairment and psychomotor retardation [21, 22]. A study of cortical excitability, which reflects the gabaergic and glutamatergic transmission of cortical interneurones (IN), could also prove promising in distinguishing neurostimulation responder profiles. No controlled study comparing the efficacy of iTBS versus conventional rTMS protocols in unipolar resistant depression has been published to date.
Specific aims
The aim of this randomised controlled trial is to investigate the efficacy of iTBS versus 10-Hz high-frequency transcranial magnetic stimulation (HF-rTMS) in a population of patients suffering from unipolar depression (Montgomery and Asberg Rating Scale (MADRS) score of >20) despite the use of two antidepressant agents during the current episode. Moreover, this trial will evaluate whether certain specific clinical or neuropsychological dimensions, objective measurements of psychomotor retardation or even distinct cortical excitability profiles could predict the efficacy of iTBS and HF-rTMS, respectively.
Methods/design
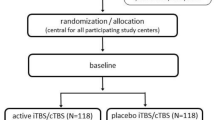
Study design, setting and recruitment
This is a randomised, controlled, double-blind, single-centre study. It is carried out at the Centre Hospitalier Universitaire (University Hospital Centre) of Nantes, France. The patients are randomly assigned to the iTBS or the HF-rTMS group as shown in Fig. 1 (Flow Chart). More specifically, the two parallel arms compare an iTBS protocol to a so-called conventional protocol at 10 Hz [23]. The stimulation target is identical in the left dorsolateral prefrontal cortex (Brodmann areas 9 and 46), localised via Nextim® (software Eximia®) neuronavigation. Participants are randomised to one of the treatment groups using a computer programme included in the electronic Case Report Form (e-CRF). This study has been approved by the local Nantes Ouest IV Ethics Committee (reference: ID RCB N°2014-AO1918-39) and compiled in accordance with the principles of the Declaration of Helsinki (final version 2004) as well as French legislation (article L1121-160 and L1126-7 of the Public Health Code). Additional quality standards are detailed in Additional file 1 according to SPIRIT Check-list requirements. All of the patients are given written and verbal information about the study aim and procedures. They sign a written Consent Form in order to take part in the study. The aim is to enrol 60 patients who have been put forward either by private or hospital psychiatrists in the region, previously informed in writing of the study.
Inclusion criteria
The 60 patients between 18 and 75 years old must present with a current depressive episode considered major (defined by Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-V) diagnostic criteria [24] and a MADRS score of >20 [25]) and resistant (failure to respond to two sequences of different antidepressants at an effective dose level over a period of 6 weeks during the current episode). The current antidepressant is continued at a stable dose throughout the study.
Each subject must be able to: understand the information; take a decision; volunteer to participate; complete the required questionnaires; take orally administered treatment independently or have the necessary assistance to do so throughout the study; and return to the research centre for successive visits.
Noninclusion criteria
Patients presenting with at least one of the following criteria are not be enrolled in the study: diagnosis of a bipolar disorder; schizophrenia; addiction; neurodegenerative disease; use of benzodiazepines (unless prescribed over 3 months earlier at a stable dosage); use of mood-modifying treatments (thyroid extracts, interferon, corticosteroids); previous failure of ECT therapy; anticonvulsant treatment; contraindication to magnetic resonance imaging (MRI); contraindication to the practice of rTMS: history of convulsions, progressive neurological and neurosurgical disorders; any prosthetic material or foreign body in situ (pacemaker, implantable defibrillator); minors or persons deprived of liberty following a legal or administrative decision or hospitalised without consent, in guardianship; or pregnant women or women of child-bearing age who are not using contraception because of no available data about iTBS and pregnancy (these women could receive, if absolutely necessary, from case to case, conventional rTMS treatment, outside the study). The same applies for subjects unable to guarantee longitudinal follow-up.
In case of a serious adverse event or exacerbated symptoms of depression, blind status will be lifted and patients will receive appropriate care and retained in the follow-up.
Study process
The screening visit V1 (D − 21 to D42) includes the Patient Information Leaflet, collection of the Consent Form and checking of inclusion/exclusion criteria. The medical research team will be in charge of enrolment and assignation of participants to the intervention. The study manager and psychiatrist investigators can generate the allocation sequence. Treatment is adjusted in line with the course of therapy. A clinical examination is also carried out and MRI prescribed to rule out any neurological disorder and mark the neuronavigation target during the baseline visit. The procedure is conducted using a Siemens 1.5 T machine with the following sequences: diffusion, T1 3D, FLAIR 2D and T2 rapid and SWI.
Randomisation
During the baseline inclusion visit, the inclusion/exclusion criteria are checked and participants randomised into two groups by a computerised random number generator with a permuted block design (ratio 1:1) without stratification or minimisation. Block size and type of variation (fixed or randomly) are not yet known by the investigators to maintain adequate blinding. Randomisation occurs in a recorded delay of maximum 72 h before first rTMS session.
Blinding
Research nurses, who perform rTMS sessions, are the only persons to know the allocated sequence. Just after the randomisation, they will receive an automatic e-mail on their individual professional mail box. The session will take place in a dedicated room with appropriate noise control and a signal on the door during the session to prevent accidental entry of investigators. Patients are not told the group they belong to, will not have precise description of rTMS parameters and duration and will not be able to speak to each other. Both treatments will be equally presented as efficient and superior to placebo.
Follow-up
Investigators will meet participants 1, 3 and 6 months after the last rTMS session.
A patient who fails to respond to therapy (no decrease of over 50% in the MADRS score) despite 4 weeks of treatment will continue longitudinal follow-up in order to avoid selection bias. A telephone call is made in the second, fourth and fifth month outside the follow-up consultations to keep in contact with patients and remind them of the next appointment in order to avoid their being lost to follow-up.
The study will last 33 months in total with 24 months being the enrolment period. Patients are followed up over a period of approximately 34 weeks in total (Table 1).
Assessments
The following variables are documented during the baseline visit: sociodemographic (age, gender, laterality, professional and marital status); medical history (length of illness, duration of current episode; psychiatric and addictive comorbidities; somatic history; treatments prescribed; degree of prior therapeutic resistance according to the Maudsley Staging Model (MSM) [29]; basal personality according to Cloninger’s Temperament and Character Inventory (TCI) [30]).
The following variables are evaluated at the beginning and end of treatment, as shown in Table 1: intensity of the depression according to the MADRS [25]; the Beck Depression Inventory 13 items (BDI 13) [26] and Clinical Global Impression – Severity (CGI-S) [27]; and quality of life with the Short-Form 36 Health Survey (SF-36) [28]. Response will be defined by a 50% reduction of MADRS or BDI score, and remission by a MADRS score of <8 and a BDI score of <10.
Potential explanatory variables to predict treatment response in addition to sociodemographic and anamnestic data are: clinical dimensions according to the Echelle de Ralentissement Dépressif (ERD) (Depression Retardation Scale) [31], the lack of pleasure Snaith-Hamilton Pleasure Scale (SHAPS) [32] and Starkstein’s Apathy Scale (SAS) [33]; cognitive functions according to the Montreal Cognitive Assessment (MoCA) [34], the Verbal Fluency Test [35] [36], the Modified Card Sorting Test (MCST) [37], the digit span, the Wechsler Adult Intelligence Scale (WAIS IV) [38] and the Trail Making Test [39]; psychomotor retardation using specific tests such as the Finger Taping Test (FTT) [40, 41], the prehensile motor strength test [42], a test to measure information processing speed (currently being validated by our team [43]); and neurophysiological measurements of cortical excitability, namely the cortical motor threshold, short intracortical inhibition (SICI) and intracortical facilitation (ICF) expressed as a percentage compared to the base value, and similarly for the cortical silent period (CSP), which is carried out in both hemispheres [44–46]. All these scales are validated scales. Concerning the motor retardation assessment, we recently showed that administering a battery of psychomotor tests during rTMS sessions is feasible, free of adverse effects and well-tolerated by that population [43]. Cortical excitability is used in daily practice for patients with neurodegenerative troubles with an excellent tolerance and feasibility. Those measures are not performed the same day (interval maximum 72 h) to avoid participant overstimulation. An incentive of €80 is planned for cortical excitability ancillatory measures.
The following scales are evaluated on a weekly basis: the MADRS, the BDI and the CGI to investigate the response kinetics and 1 month, 3 months and 6 months after the endpoint as well as quality of life (SF-36). Data collected directly from participants themselves will be the BDI, the SAS, the SHAPS, the TCI and the SF-36. Adherence to study quality standards is carried out by an independent research associate. All significant adverse events will be reported in the e-CRF by the research team.
Interventions
For the rTMS, an eight-shaped coil (Cool B65) and a Magpro Stimulator X100 (Dantec Company, Copenhagen, Denmark) are used. The resting motor threshold (RMT) is recorded daily by a Natus Keypoint® (Natus, Middleton, WI, USA). This is defined as the intensity required to elicit at least five motor-evoked potentials (MEPs) with a 50-μV peak-to-peak amplitude out of ten consecutive stimulations when the coil is placed over the left primary cortex (site for maximal stimulation of the abductor pollicis brevis muscle). The parameters used for HF-rTMS delivery are: 110% of RMT; 10 Hz; 20 min; 4 s per train; 28 s intertrain interval; 1600 pulses per day (40 trains of 40 pulses each). The iTBS protocol will be: 80% of RMT; 50 Hz; 6 min; 600 pulses a day.
The target is left DLPFC corresponding to the junction between Brodmann areas 9 and 46 according to an individual’s 3D-MRI. During rTMS sessions, participants are instructed to keep their eyes open and to be relaxed. All subjects are evaluated before, once a week during the rTMS course, at the endpoint and then at 1, 3 and 6 months.
Primary outcome measures
The primary endpoint in our study will be the number of responders per group, defined by a decrease of at least 50% in the initial MADRS score at the end of rTMS sessions.
Secondary outcome measures
The secondary endpoints will be: therapeutic response rate corresponding to a MADRS score improvement of >50% in each group 1 month after rTMS sessions; number of remissions defined by a MADRS score of <8 at the endpoint and 1 month after; number of therapeutic responses and remissions maintained in the 6 months following rTMS treatment; changes in quality of life; and clinical, motor, neuropsychological and neurophysiological (cortical excitability) therapeutic response markers.
Statistical analysis
A descriptive analysis of the data collected during each patient evaluation will be carried out up until the final evaluation. Specific time points for analysis are: end of rTMS sessions and, 1, 3 and 6 months after the treatment course. Continuous variables will be described using median and range; and qualitative variables using frequencies and percentages.
The final analysis will be conducted according to the intent-to-treat (ITT) principle. The starting hypothesis is a 25% response rate in the 10-Hz group in accordance with 10-Hz HF-rTMS trials of reference [5] and 60% in the iTBS group based on pilot studies [17]. Assuming a 5% (bilateral) type I error and a power of 80%, a total of 60 subjects is required (calculated using SAS software).
The therapeutic response rates (proportion of responders) in each group will be compared using a chi-squared test (or Fisher’s exact test, if appropriate). Estimates of absolute and relative differences (via the odds ratio or relative risk) in terms of efficacy will be provided with their corresponding 95% confidence intervals. The format of the outcome data used for each participant for analysis will be changes from baseline.
Changes in quantitative variables over time (evaluation of the therapeutic effect of rTMS (iTBS) on variations in the MADRS, BDI and CGI scores) will be analysed using random effect models allowing to take into account the repeated measurements. Time (baseline, after 5, 10, 15, and 20 sessions, +1 month, +3 months and +6 months) and group (iTBS or standard) effects will be estimated and tested as well as an interaction with group. Changes in other quantitative variables over time will be investigated according to the same strategy.
The analysis and comparison between groups of the onset of relapse of depression in the 6 months will be carried out using a logistic regression model and testing factors linked to the therapeutic response (neuropsychological and motor tests, dimensional scales, initial measurements of cortical excitability).
Concerning the risk of missing data, a very low attrition rate is expected, below 5% [47] because of the well-known high tolerance to rTMS and iTBS [48]. In case of withdrawal of consent, patients will not be included in final analysis – they will be replaced.
Missing data will be described in terms of frequencies and percentage for each group. Imbalances will be evaluated by the chi-squared test (or Fisher’s exact test). Comparison of missing data onset during follow-up will be realised with a log-rank test for longitudinal data. Each dropout will be described as follows: arm, exit date, exit reason, characteristics at inclusion and last data collected. In case of missing data, despite every effort to prevent it, a multiple imputation analysis will be performed.
Discussion
Depression is known as a difficult-to-treat disorder. By 2013, unipolar depression is expected to rank second out of the 15 most common disorders after AIDS and before ischemic heart disease [49]. The advantages of rTMS are numerous: it is painless, well-tolerated in terms of memory, cardiac, hepatic and renal functions as well as libido. There is no need for general anaesthesia with curarisation. Since the early 1990s, an increasing number of studies has focused on the therapeutic potential of rTMS in psychiatry [50].
This technique has a compliance rate of 97% (versus 60% traditionally recorded for medication). In fact, several meta-analyses based on randomised, controlled, double-blind studies refer to the therapeutic efficacy of rTMS in the management of resistant depression. The use of rTMS devices was also validated for this indication by the US Food and Drug Administration (FDA) in 2008 and by the European Union (EU) in 2012. By way of example, one of the most recent analyses highlighted a three-fold greater response and remission rate for left prefrontal cortex stimulation at high frequency versus placebo [10].
Furthermore, once antidepressants have failed, rTMS would be less expensive and would allow a better quality of life and greater function compared to conventional treatment strategies [51]. Its mechanisms of action are manifold: improvement in prefrontal hypometabolism [52] and neuromodulation of remote cerebral areas (especially the subgenual region) [53], regulation of the hypothalamo-hypophyseal axis [53], modulation of cortical excitability and synaptic plasticity [54–56] and dopaminergic secretion [57, 58].
The optimisation of alternative treatments for refractory or chronic depression is, therefore, a public health issue. The Theta Burst paradigm seems promising since 3 min of iTBS are essentially more effective and have a longer lasting effect than 20 min of conventional rTMS stimulation at 5 Hz (as evidenced in MEPs) [59]. In fact, iTBS tends to mimic the physiological rhythm of the human neocortex and involves the cerebral plasticity mechanisms responsible for positive and presumably longer-lasting effects [60], with a shorter, less intense stimulation mechanism [61]. Duprat et al., (2016) recently found a 30% remission rate (HDRS <7) after 2 weeks of accelerated (20 sessions/2 weeks) iTBS in a cross-over, sham-controlled design [48]. These facts suggest additional patient comfort, lower session costs and greater prevention of relapse. In the case of a prolonged effect, it could be an alternative to potentiating medicinal treatment (combinations of antidepressant, mood stabilising or adjuvant antipsychotic agents) with fewer compliance problems. The efficacy of Theta Burst was investigated in the management of resistant depression in two studies, which confirmed its superiority compared to placebo (Li et al., [18] with 30 subjects; Plewnia et al., [62] involving 60 subjects). Recently, in a larger sample but under natural conditions (retrospective study), iTBS was as clinically effective as HF-rTMS at 10 Hz but five times longer (6 versus 30 min, respectively) [19]. The authors concluded that these data should be confirmed by randomised controlled trials. Better targeting of the responder profile leads to better use of human and material resources in medical-economic terms. In cognitive terms, the planning assessed in the TMT, mental flexibility assessed using the MCST, or verbal fluency are influenced by rTMS treatment [63–67] and are, therefore, potential response markers. Psychomotor retardation has a predictive value in assessing the response for most biological treatments of depression [68]. Unlike cognitive functions, its pure motor component has not been assessed objectively to date in the context of the cerebral stimulation techniques used in the management of depression, for instance, with tasks such as the FTT or the prehensile motor strength test. The three main parameters affecting the motor cortex excitability are the CSP partly reflecting the activity of the gamma-aminobutyric acid (GABA)-B inhibitory circuits and double-pulse measurements including: SICI partly reflecting the activity of GABA-A IN inhibitors; and ICF partly reflecting the activity of glutamatergic IN activators. Two recent meta-analyses have highlighted changes in motor cortical excitability in an entire series of psychiatric disorders compared to healthy subjects [69, 70], with essentially an alteration in SICI and CSP during the depressive episode. In recent years, a few authors have focused on their potential as response markers, especially during noninvasive brain stimulation. In 2008, for instance, Lefaucheur et al., highlighted interhemispheric asymmetry of cortical excitability in depressed subjects: CSP and SICI were altered in the left hemisphere compared to the right and contrary to findings in healthy subjects [71]. Following cerebral stimulation (ECT and rTMS), Bajbouj et al. showed that CSP and SICI improved in responders and not in nonresponders [72].
To date and to our knowledge, this is the first trial aiming to investigate the comparative influence of iTBS and HF-rTMS on psychomotor retardation, executive functions and cortical motor excitability in depressed subjects. Psychomotor retardation could be corrected by the pro-dopaminergic effect of rTMS. Furthermore, executive functions may be a marker of the effect of DLPFC stimulation [73]. Given the data available on the effect of rTMS on magnetic resonance spectroscopy measurements, which indicate an increase in GABA and glutamate levels after rTMS [74, 75], neuromodulation can be assumed to manifest in the form of changes in cortical excitability measurements tending towards normalisation with 10-Hz protocols and iTBS, the greatest change being apparent in the case of the latter. The intensity of the gabaergic and/or glutamatergic deficit(s) and the degree of interhemispherical asymmetry in cortical excitability tests could identify responder patient profiles for both treatments. Moreover, measuring the difference in neurophysiological effect in both protocols would enhance the neurobiological understanding of this disease.
This sample is probably not entirely representative of a population often combining comorbidities with considerable treatment heterogeneity. However, we opted to limit the inclusion criteria in order to facilitate comparison with fewer confusing variables and interpret cortical excitability measurements.
Trial status
Patient recruitment is still ongoing.
Abbreviations
- BDI:
-
Beck Depression Inventory
- CGI:
-
Clinical Global Impression
- CSP:
-
Cortical Silent Period
- cTBS:
-
Continuous Theta Burst Stimulation
- DLPFC:
-
Dorsolateral Prefrontal Cortex
- e-CRF:
-
Electronic Case Report Form
- ECT:
-
ElectroConvulsive Therapy
- ERD:
-
Echelle de Ralentissement Dépressif
- EU:
-
European Union
- FDA:
-
Food and Drug Administration
- FTT:
-
Finger Tapping Test
- GABA:
-
Gamma-AminoButyric Acid
- HARD scale:
-
Humeur, Anxiété, Ralentissement, Danger
- ICF:
-
Intracortical Facilitation
- IN:
-
InterNeurons
- iTBS:
-
Intermittent Theta Burst Stimulation
- ITT:
-
Intention-To-Treat
- L-HF:
-
Left-High Frequency
- MADRS:
-
Montgomery and Adsberg Rating Scale
- MCST:
-
Modified Card Sorting Test
- MEP:
-
Motor-Evoked Potential
- MoCA:
-
Montreal Cognitive Assessment
- MRI:
-
Magnetic Resonance Imaging
- MSM:
-
Maudsley Staging Model
- R-LF:
-
Right-Low Frequency
- RMT:
-
Resting Motor Threshold
- rTMS:
-
repeated Transcranial Magnetic Stimulation
- SAS:
-
Starkstein’s Apathy Scale
- SF-36:
-
Short-Form 36
- SHAPS:
-
Snaith-Hamilton Pleasure Scale
- SICI:
-
Short Intracortical Inhibition
- TCI:
-
Temperament and Character Inventory
- TMT:
-
Trail Making Test
- WAIS IV:
-
Wechsler Adult Intelligence Scale
- WHO:
-
World Health Organisation
References
Fava M. Diagnosis and definition of treatment-resistant depression. Biol Psychiatry. 2003;53(8):649–59.
Heijnen WT, Birkenhäger TK, Wierdsma AI, van den Broek WW. Antidepressant pharmacotherapy failure and response to subsequent electroconvulsive therapy: a meta-analysis. J Clin Psychopharmacol. 2010;30(5):616–9.
Xie J, Chen J, Wei Q. Repetitive transcranial magnetic stimulation versus electroconvulsive therapy for major depression: a meta-analysis of stimulus parameter effects. Neurol Res. 2013;35(10):1084–91.
Ren J, Li H, Palaniyappan L, Liu H, Wang J, Li C, et al. Repetitive transcranial magnetic stimulation versus electroconvulsive therapy for major depression: a systematic review and meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2014;51:181–9.
O’Reardon JP, Solvason HB, Janicak PG, Sampson S, Isenberg KE, Nahas Z, et al. Efficacy and safety of transcranial magnetic stimulation in the acute treatment of major depression: a multisite randomized controlled trial. Biol Psychiatry. 2007;62(11):1208–16.
Schulz M, Irmisch G, Mau R, Schläfke D, Richter J. Antidepressant efficacy of two different rTMS procedures. High frequency over left versus low frequency over right prefrontal cortex compared with sham stimulation. Eur Arch Psychiatry Clin Neurosci. 2003;253(2):103–9.
Fitzgerald PB, Huntsman S, Gunewardene R, Kulkarni J, Daskalakis ZJ. A randomized trial of low-frequency right-prefrontal-cortex transcranial magnetic stimulation as augmentation in treatment-resistant major depression. Int J Neuropsychopharmacol. 2006;9(6):655–66.
Fitzgerald PB, Hoy K, Daskalakis ZJ, Kulkarni J. A randomized trial of the anti-depressant effects of low- and high-frequency transcranial magnetic stimulation in treatment-resistant depression. Depress Anxiety. 2009;26(3):229–34.
Pallanti S, Bernardi S, Di Rollo A, Antonini S, Quercioli L. Unilateral low frequency versus sequential bilateral repetitive transcranial magnetic stimulation: is simpler better for treatment of resistant depression? Neuroscience. 2010;167(2):323–8.
Berlim MT, van den Eynde F, Tovar-Perdomo S, Daskalakis ZJ. Response, remission and drop-out rates following high-frequency repetitive transcranial magnetic stimulation (rTMS) for treating major depression: a systematic review and meta-analysis of randomized, double-blind and sham-controlled trials. Psychol Med. 2014;44(2):225–39.
Berlim MT, Van den Eynde F, Daskalakis ZJ. Efficacy and acceptability of high frequency repetitive transcranial magnetic stimulation (rTMS) versus electroconvulsive therapy (ECT) for major depression: a systematic review and meta-analysis of randomized trials. Depress Anxiety. 2013;30(7):614–23.
George MS, Taylor JJ, Short EB. The expanding evidence base for rTMS treatment of depression. Curr Opin Psychiatry. 2013;26(1):13–8.
Cohen RB, Boggio PS, Fregni F. Risk factors for relapse after remission with repetitive transcranial magnetic stimulation for the treatment of depression. Depress Anxiety. 2009;26(7):682–8.
Huang Y-Z, Edwards MJ, Rounis E, Bhatia KP, Rothwell JC. Theta burst stimulation of the human motor cortex. Neuron. 2005;45(2):201–6.
Grossheinrich N, Rau A, Pogarell O, Hennig-Fast K, Reinl M, Karch S, et al. Theta burst stimulation of the prefrontal cortex: safety and impact on cognition, mood, and resting electroencephalogram. Biol Psychiatry. 2009;65(9):778–84.
Rossi S, Hallett M, Rossini PM, Pascual-Leone A, Safety of TMS Consensus Group. Safety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research. Clin Neurophysiol. 2009;120(12):2008–39.
Holzer M, Padberg F. Intermittent theta burst stimulation (iTBS) ameliorates therapy-resistant depression: a case series. Brain Stimul. 2010;3(3):181–3.
Li C-T, Chen M-H, Juan C-H, Huang H-H, Chen L-F, Hsieh J-C, et al. Efficacy of prefrontal theta-burst stimulation in refractory depression: a randomized sham-controlled study. Brain. 2014;137(Pt 7):2088–98.
Bakker N, Shahab S, Giacobbe P, Blumberger DM, Daskalakis ZJ, Kennedy SH, et al. rTMS of the dorsomedial prefrontal cortex for major depression: safety, tolerability, effectiveness, and outcome predictors for 10 Hz versus intermittent theta-burst stimulation. Brain Stimul. 2015;8(2):208–15.
Dell’osso B, Camuri G, Castellano F, Vecchi V, Benedetti M, Bortolussi S, et al. Meta-review of metanalytic studies with repetitive Transcranial Magnetic Stimulation (rTMS) for the treatment of major depression. Clin Pract Epidemiol Ment Health. 2011;7:167–77.
Lisanby SH, Husain MM, Rosenquist PB, Maixner D, Gutierrez R, Krystal A, et al. Daily left prefrontal repetitive transcranial magnetic stimulation in the acute treatment of major depression: clinical predictors of outcome in a multisite, randomized controlled clinical trial. Neuropsychopharmacology. 2009;34(2):522–34.
Dumas R, Padovani R, Richieri R, Lançon C. Repetitive transcranial magnetic stimulation in major depression: response factor. Encéphale. 2012;38(4):360–8.
Avery DH, Holtzheimer PE, Fawaz W, Russo J, Neumaier J, Dunner DL, et al. A controlled study of repetitive transcranial magnetic stimulation in medication-resistant major depression. Biol Psychiatry. 2006;59(2):187–94.
American Psychiatric Association. DSM-5: diagnostic and statistical manual of mental disorders. 5th ed. Washington: American Psychiatric Association; 2013.
Montgomery A. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–9.
Beck AT, Beamesderfer A. Assessment of depression: the Depression Inventory. Psychological measurements in psychopharmacology. Mod. Probl. in Pharmacopsychiatry. Mod Probl Pharmacopsychiatry. 1974;7:151–9.
Guy W. ECDEU Assessment Manual for Psychopharmacology —Revised Edition. Rockville: NIMH Publication; 1976; 218–222.
McHorney CA, Ware JE, Lu JF, The SCD, MOS. 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32(1):40–66.
Fekadu A, Wooderson S, Donaldson C, Markopoulou K, Masterson B, Poon L, et al. A multidimensional tool to quantify treatment resistance in depression: the Maudsley staging method. J Clin Psychiatry. 2009;70(2):177–84.
Cloninger CR, Svrakic DM. Integrative psychobiological approach to psychiatric assessment and treatment. Psychiatry. 1997;60(2):120–41.
Widlöcher DJ. Psychomotor retardation: clinical, theoretical, and psychometric aspects. Psychiatr Clin North Am. 1983;6(1):27–40.
Snaith RP, Hamilton M, Morley S, Humayan A, Hargreaves D, Trigwell P. A scale for the assessment of hedonic tone the Snaith-Hamilton Pleasure Scale. Br J Psychiatry. 1995;167(1):99–103.
Pedersen KF, Alves G, Larsen JP, Tysnes O-B, Møller SG, Brønnick K. Psychometric properties of the Starkstein Apathy Scale in patients with early untreated Parkinson disease. Am J Geriatr Psychiatry. 2012;20(2):142–8.
Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–9.
Cardebat D, Doyon B, Puel M, Goulet P, Joanette Y. Formal and semantic lexical evocation in normal subjects. Performance and dynamics of production as a function of sex, age and educational level. Acta Neurol Belg. 1990;90(4):207–17.
Troyer AK, Moscovitch M, Winocur G. Clustering and switching as two components of verbal fluency: evidence from younger and older healthy adults. Neuropsychology. 1997;11(1):136–48.
Nelson HE. A Modified Card Sorting Test sensitive to frontal lobe defects. Cortex. 1976;12(4):313–24.
Benson N, Hulac DM, Kranzler JH. Independent examination of the Wechsler Adult Intelligence Scale-Fourth Edition (WAIS-IV): what does the WAIS-IV measure? Psychol Assess. 2010;22(1):121–30.
Tombaugh TN. Making Test A and B: normative data stratified by age and education. Arch Clin Neuropsychol. 2004;19(2):203–14.
Reitan RM, Wolfson D. Can neuropsychological testing produce unequivocal evidence of brain damage? II. Testing for right vs. left differences. Appl Neuropsychol. 2008;15(1):39–43.
Reitan RM, Wolfson D. The Halstead-Reitan Neuropsychological Test Battery: theory and clinical interpretation. Tucson: Neuropsychology Press; 1993. incomplète.
Calancie B, Nordin M, Wallin U, Hagbarth KE. Motor-unit responses in human wrist flexor and extensor muscles to transcranial cortical stimuli. J Neurophysiol. 1987;58(5):1168–85.
Thomas-Ollivier V, Deschamps T, Bulteau S, Le Gall F, Pichot A, Valriviere P, et al. Effect of repetitive transcranial magnetic stimulation on psychomotor retardation in major depression: a pilot feasibility study. J Neuropsychiatry Clin Neurosci. 2016;28(1):62–5.
Kujirai T, Caramia MD, Rothwell JC, Day BL, Thompson PD, Ferbert A, et al. Corticocortical inhibition in human motor cortex. J Physiol. 1993;471:501–19.
Maeda F, Pascual-Leone A. Transcranial magnetic stimulation: studying motor neurophysiology of psychiatric disorders. Psychopharmacology (Berl). 2003;168(4):359–76.
Ziemann U. TMS measures of motor cortical and corticospinal excitability: physiology, function and plasticity. The Oxford handbook of transcranial stimulation. Oxford: University Press; 2008.
Liu B, Zhang Y, Zhang L, Li L. Repetitive transcranial magnetic stimulation as an augmentative strategy for treatment-resistant depression, a meta-analysis of randomized, double-blind and sham-controlled study. BMC Psychiatry. 2014;14:342.
Duprat R, Desmyter S, de Rudi R, van Heeringen K, Van den Abbeele D, Tandt H, et al. Accelerated intermittent theta burst stimulation treatment in medication-resistant major depression: a fast road to remission? J Affect Disord. 2016;200:6–14.
Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442.
Lefaucheur J-P, André-Obadia N, Antal A, Ayache SS, Baeken C, Benninger DH, et al. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS). Clin Neurophysiol. 2014;125(11):2150–206.
Simpson KN, Welch MJ, Kozel FA, Demitrack MA, Nahas Z. Cost-effectiveness of transcranial magnetic stimulation in the treatment of major depression: a health economics analysis. Adv Ther. 2009;26(3):346–68.
Bestmann S, Baudewig J, Siebner HR, Rothwell JC, Frahm J. BOLD MRI responses to repetitive TMS over human dorsal premotor cortex. Neuroimage. 2005;28(1):22–9.
Baeken C, Marinazzo D, Everaert H, Wu G-R, Van Hove C, Audenaert K, et al. The impact of accelerated HF-rTMS on the subgenual anterior cingulate cortex in refractory unipolar major depression: insights from (18)FDG PET brain imaging. Brain Stimul. 2015;8(4):808–15.
Baeken C, De Raedt R. Neurobiological mechanisms of repetitive transcranial magnetic stimulation on the underlying neurocircuitry in unipolar depression. Dialogues Clin Neurosci. 2011;13(1):139–45.
Pell GS, Roth Y, Zangen A. Modulation of cortical excitability induced by repetitive transcranial magnetic stimulation: influence of timing and geometrical parameters and underlying mechanisms. Prog Neurobiol. 2011;93(1):59–98.
Hoogendam JM, Ramakers GMJ, Di Lazzaro V. Physiology of repetitive transcranial magnetic stimulation of the human brain. Brain Stimul. 2010;3(2):95–118.
Strafella AP, Paus T, Fraraccio M, Dagher A. Striatal dopamine release induced by repetitive transcranial magnetic stimulation of the human motor cortex. Brain. 2003;126(Pt 12):2609–15.
Shaul U, Ben-Shachar D, Karry R, Klein E. Modulation of frequency and duration of repetitive magnetic stimulation affects catecholamine levels and tyrosine hydroxylase activity in human neuroblastoma cells: implication for the antidepressant effect of rTMS. Int J Neuropsychopharmacol. 2003;6(3):233–41.
Gamboa OL, Antal A, Laczo B, Moliadze V, Nitsche MA, Paulus W. Impact of repetitive theta burst stimulation on motor cortex excitability. Brain Stimul. 2011;4(3):145–51.
Thut G, Pascual-Leone A. A review of combined TMS-EEG studies to characterize lasting effects of repetitive TMS and assess their usefulness in cognitive and clinical neuroscience. Brain Topogr. 2010;22(4):219–32.
Hinder MR, Goss EL, Fujiyama H, Canty AJ, Garry MI, Rodger J, et al. Inter- and intra-individual variability following intermittent theta burst stimulation: implications for rehabilitation and recovery. Brain Stimul. 2014;7(3):365–71.
Plewnia C, Pasqualetti P, Große S, Schlipf S, Wasserka B, Zwissler B, et al. Treatment of major depression with bilateral theta burst stimulation: a randomized controlled pilot trial. J Affect Disord. 2014;156:219–23.
Furukawa T, Izumi S-I, Toyokura M, Masakado Y. Effects of low-frequency repetitive transcranial magnetic stimulation in Parkinson’s disease. Tokai J Exp Clin Med. 2009;34(3):63–71.
Huang M, Luo B, Hu J, Wang S-S, Zhou W, Wei N, et al. Repetitive transcranial magnetic stimulation in combination with citalopram in young patients with first-episode major depressive disorder: a double-blind, randomized, sham-controlled trial. Aust N Z J Psychiatry. 2012;46(3):257–64.
Noda Y, Nakamura M, Saeki T, Inoue M, Iwanari H, Kasai K. Potentiation of quantitative electroencephalograms following prefrontal repetitive transcranial magnetic stimulation in patients with major depression. Neurosci Res. 2013;77(1–2):70–7.
Zheng H, Jia F, Guo G, Quan D, Li G, Wu H, et al. Abnormal anterior cingulate N-acetylaspartate and executive functioning in treatment-resistant depression after rTMS therapy. Int J Neuropsychopharmacol. 2015;18(11): pyv059.
Pallanti S, Di Rollo A, Antonini S, Cauli G, Hollander E, Quercioli L. Low-frequency rTMS over right dorsolateral prefrontal cortex in the treatment of resistant depression: cognitive improvement is independent from clinical response, resting motor threshold is related to clinical response. Neuropsychobiology. 2012;65(4):227–35.
Schrijvers D, Hulstijn W, Sabbe BGC. Psychomotor symptoms in depression: a diagnostic, pathophysiological and therapeutic tool. J Affect Disord. 2008;109(1–2):1–20.
Bunse T, Wobrock T, Strube W, Padberg F, Palm U, Falkai P, et al. Motor cortical excitability assessed by transcranial magnetic stimulation in psychiatric disorders: a systematic review. Brain Stimul. 2014;7(2):158–69.
Radhu N, de Jesus DR, Ravindran LN, Zanjani A, Fitzgerald PB, Daskalakis ZJ. A meta-analysis of cortical inhibition and excitability using transcranial magnetic stimulation in psychiatric disorders. Clin Neurophysiol. 2013;124(7):1309–20.
Lefaucheur JP, Lucas B, Andraud F, Hogrel JY, Bellivier F, Del Cul A, et al. Inter-hemispheric asymmetry of motor corticospinal excitability in major depression studied by transcranial magnetic stimulation. J Psychiatr Res. 2008;42(5):389–98.
Bajbouj M, Luborzewski A, Danker-Hopfe H, Lang UE. Motor cortical excitability in depressive patients after electroconvulsive therapy and repetitive transcranial magnetic stimulation. J ECT. 2005;21(4):243–5.
Guse B, Falkai P, Wobrock T. Cognitive effects of high-frequency repetitive transcranial magnetic stimulation: a systematic review. J Neural Transm (Vienna). 2010;117(1):105–22.
Luborzewski A, Schubert F, Seifert F, Danker-Hopfe H, Brakemeier E-L, Schlattmann P, et al. Metabolic alterations in the dorsolateral prefrontal cortex after treatment with high-frequency repetitive transcranial magnetic stimulation in patients with unipolar major depression. J Psychiatr Res. 2007;41(7):606–15.
Yue L, Xiao-lin H, Tao S. The effects of chronic repetitive transcranial magnetic stimulation on glutamate and gamma-aminobutyric acid in rat brain. Brain Res. 2009;1260:94–9.
Acknowledgments
We thank Aurelie Grateau and Christelle Volteau for e-CRF and randomisation process preparation.
Funding
CHU de Nantes, call of birds 2014; Reference RC14-0375; Eudract number 2014-A01918-39. Protocol current version 19 June 2014. Insurance company SHAM (N°135964).
Availability of data and materials
All supporting data can be available.
Authors’ contributions
SB conceived the study and designed the study protocol and is the coordinator of the study. SB and AS wrote the manuscript. SB, AS, EL and J-MV are investigators and responsible for enrolment, indications for treatment, and data collection. JF is the project manager, helped with general organisation and sought ethical and regulatory approval. AP and PV contributed to deliver the technique and treatment planning. VS is responsible for statistical power calculation and analysis. TD and VTO are responsible for designing and assessing neuropsychological status and psychomotor retardation. EA-C is responsible for MRI data. SB, GF and YP are responsible for cortical excitability assessment. AB is responsible for planning, randomisation and e-CRF completion. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
ANSM approval (registration number DMDPT-BLOC/MM/2014-AO1918-39/MS 1).
Nantes Ouest IV Ethics Committee approval 1 December 2015 (reference 05/15, TLT/BB CPP N°738/2015).
Information letter and consent form approved: version n°2 (12 January 2015).
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1:
SPIRIT 2013 Checklist. recommended items to address in a clinical trial protocol and related documents. (DOCX 52 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Bulteau, S., Sébille, V., Fayet, G. et al. Efficacy of intermittent Theta Burst Stimulation (iTBS) and 10-Hz high-frequency repetitive transcranial magnetic stimulation (rTMS) in treatment-resistant unipolar depression: study protocol for a randomised controlled trial. Trials 18, 17 (2017). https://doi.org/10.1186/s13063-016-1764-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-016-1764-8