Abstract
This systematic review aimed to assess the methods used to classify mammographic breast parenchymal features in relation to the prediction of future breast cancer. The databases including Medline (Ovid) 1946-, Embase.com 1947-, CINAHL Plus 1937-, Scopus 1823-, Cochrane Library (including CENTRAL), and Clinicaltrials.gov were searched through October 2021 to extract published articles in English describing the relationship of parenchymal texture features with the risk of breast cancer. Twenty-eight articles published since 2016 were included in the final review. The identification of parenchymal texture features varied from using a predefined list to machine-driven identification. A reduction in the number of features chosen for subsequent analysis in relation to cancer incidence then varied across statistical approaches and machine learning methods. The variation in approach and number of features identified for inclusion in analysis precluded generating a quantitative summary or meta-analysis of the value of these features to improve predicting risk of future breast cancers. This updated overview of the state of the art revealed research gaps; based on these, we provide recommendations for future studies using parenchymal features for mammogram images to make use of accumulating image data, and external validation of prediction models that extend to 5 and 10 years to guide clinical risk management. Following these recommendations could enhance the applicability of models, helping improve risk classification and risk prediction for women to tailor screening and prevention strategies to the level of risk.
Similar content being viewed by others
Introduction
Evolving technology from film mammograms to digital images has changed the sources of data and ease of access to study a range of summary measures from breast mammograms and the risk of breast cancer [1, 2]. These include more extreme measures of density and also measures of breast texture features. In particular, as women have repeated mammograms as part of a regular screening program [3,4,5], access to repeated images including changing texture features has become more feasible in real time for risk estimation and classification and appropriately counseling women for their risk management [6,7,8]. Using these features may facilitate improvement in risk classification [9] and hence more fully support precision prevention for breast cancer [8, 10].
The leading measure for long-term risk categorization extracted from mammograms is breast density [11, 12]. This is now widely used and reported with many states requiring the return of mammographic breast density measures to women as part of routine screening [13]. Mammographic breast density is a strong reproducible risk factor for breast cancer across different approaches used to measure it (clinical judgment or semi/automated estimation) [11] and across regions of the world [11, 14, 15]. However, density is known to be affected by confounders such as age and body mass index [16, 17]. Texture features within mammograms have been much less frequently studied for their contribution to risk stratification and risk prediction but could potentially be less impacted by these confounders. Moreover, mammogram density only aims to measure the relative amount of fibroglandular tissue in the breast [18], which limits the ability to fully capture heterogeneity between patients in the breast tissue, while patterns of breast parenchymal complexity, formed by the x-ray attenuation of fatty, fibroglandular, and stromal tissues, are known to be associated with breast cancer [19, 20].
In 2016, Gastounioti and colleagues summarized the literature at that time to classify approaches to parenchymal texture classification: (1) gray-level features—skewness; kurtosis; entropy; and sum intensity, (2) co-occurrence features—entropy; inertia; difference moment; and coarseness, (3) run-length measures gray-level non-uniformity and run-length non-uniformity, (4) structural patterns measures lacunarity, fractal dimension, and (5) multiresolution spectral features [21]. They conclude from this review that multiparametric texture features may be more effective in predicting breast cancer than single-group features. Although this review included studies using the ipsilateral and/or contralateral breast, it did not report on their time horizon. To address this and use of more comprehensive summaries of these features since their review in 2016, we conducted a systematic review of published studies.
In current medical practice, risk prediction is viewed as an objective way to assess the risk of a patient developing a disease such as a 10-year risk of cardiovascular disease [22]. Risk prediction models are often evaluated in terms of calibrations and discrimination. For instance, the AUC (a discrimination measure) describes how well a given model separates events from non-events. On the other hand, association measures such as a significant hazard ratio for an individual risk factor do not necessarily translate to a significant increase in discrimination performance when it is added to a prediction model [23].
We aim to summarize the methods used to classify mammographic breast parenchymal features in relation to the prediction of future breast cancer, the time from mammogram to the diagnosis of breast cancer, the analysis of data from either one or both breasts (averaged or assessed individually), the study design, and the statistical methods for estimating the association between features and risk. We then identify gaps in evidence to prioritize future studies and speed us to better support the precision prevention of breast cancer.
Methods
Eligibility criteria
Population
We considered all studies of adult women (at least 18 years old) involving original data. Abstract-only papers, review articles, and conference papers were excluded.
Intervention
We included studies measuring at least one non-density mammographic feature. A study had to explicitly define the mammographic features included. Studies that did not do this, such as those which used a deep model, were excluded because we would be unable to determine the characteristics of features used and compare these to other studies.
Comparison
We compared models using parenchymal texture features to those that did not.
Outcomes
Our primary outcome of interest was the risk of breast cancer, including both invasive and in situ cancers. The risk of breast cancer was required to be dichotomized (yes/no). Analysis of other risks (e.g., risk of interval vs. screen-detected cancer) and studies examining the association between mammographic features and other risk factors were excluded to narrow the scope of our paper.
Only studies available in English were included. Additionally, only studies published from 2016 onward were included to avoid overlap with previous reviews.
Information sources
The published literature was searched using strategies designed by a medical librarian for the concepts of breast density, mammography, and related synonyms. These strategies were created using a combination of controlled vocabulary terms and keywords, and were executed in Medline (Ovid) 1946-, Embase.com 1947-, CINAHL Plus 1937-, Scopus 1823-, Cochrane Library (including CENTRAL), and Clinicaltrials.gov. Results were limited to English using database-supplied filters. Letters, comments, notes, and editorials were also excluded from the results using publication type filters and limits.
Search strategy
An example search is provided below (for Embase).
('breast density'/exp OR ((breast NEAR/3 densit*):ti,ab,kw OR (mammary NEAR/3 densit*):ti,ab,kw OR (mammographic NEAR/3 densit*):ti,ab,kw)) AND ('mammography'/deOR mammograph*:ti,ab,kwOR mammogram*:ti,ab,kwOR mastrography:ti,ab,kwOR ‘digital breast tomosynthesis’:ti,ab,kwOR ‘x-ray breast tomosynthesis’:ti,ab,kw)NOT('editorial'/it OR 'letter'/it OR 'note'/it) AND [english]/lim
The search was completed for the first time on September 9, 2020, and was run again on October 14, 2021, to retrieve citations that were published since the original search. The second search was dated limited to 2020-present (October 2021). Full search strategies are provided in the Additional file 1: appendix.
Selection process
Two reviewers (AA, CS) worked independently to review the titles and abstracts of the records. Next, the two reviewers independently screened the full text of the articles that they did not reject to determine which were eligible for inclusion. Any disagreements about which articles to include were resolved by consensus. Two reviewers (AA, YC) then went through this subset independently and excluded the ones without explicitly defined features.
Data collection process
We created a data extraction sheet that two reviewers (AA, YC) used to independently extract data from the included studies. Disagreements were resolved by a third reviewer. If included studies were missing any desired information, any additional papers from the works cited, such as previous reports, methods papers, or protocols, were reviewed for this information.
Data items
Any estimate of the risk of breast cancer was eligible to be included. Risk models could combine multiple texture features or examine texture features individually. The predictive ability could be evaluated using an area under the curve, odds ratio, matched concordance index, hazard ratio, or p value. No restrictions on follow-up time were placed. For studies that reported multiple risk estimates, we prioritized the area under the curve with the most non-mammogram covariates included from the validation study if applicable. If the study did not report an area under the curve, we listed the primary models which were discussed in the Results section of the paper.
We collected data on:
-
the report: author, publication year
-
the study: location/institution, number of cases, number of controls, study design
-
the research design and features: lapsed time from mammogram to diagnosis
-
the mammogram: machine type, mammogram view(s), breast(s) used for analysis
-
the model: how density was measured, number of texture features extracted, types of texture features extracted, whether feature extraction was machine or human, whether all features were used in the analysis, how features for analysis were chosen, non-mammogram covariates included, established confounders for density, prediction horizon, statistical methods for assessing risk association
Risk of bias
The quality of the included studies was assessed using the Quality in Prognostic Studies (QUIPS) tool [24]. Risk of bias was rated as high, moderate, low, or unclear by two reviewers (AA and CS) across six domains including study participation, study attrition, prognostic factor measurement, outcome measurement, study confounding, and statistical analysis and reporting. Raters independently recorded supporting information and justification for judgments of risk of bias for each domain. Any disagreements were resolved by consensus.
Human subjects
This study did not involve human subjects, and therefore oversight from an Institutional Review Board was not required.
Registration and protocol
This review was not registered and a protocol was not prepared.
Results
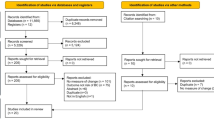
The search and study selection process is shown in Fig. 1. A total of 11,111 results were retrieved from the initial database literature search and imported into Endnote. Eleven citations from ClinicalTrials.gov were retrieved and added to an Excel file library. After removing duplicates, 4863 unique citations remained for analysis. The search was run again in October 2021 to retrieve citations that were published since the original search. A total of 1633 results were retrieved and imported to Endnote. After removing duplicates, including duplicates from the original search, 466 unique citations were added to the pool of results for screening. Between the two searches, a total of 11,577 results were retrieved, and there were 5329 unique citations.
Of the 5329 unique citations, 5124 were excluded based on the review of the title and abstract. Two hundred and five full-text reports were retrieved and assessed for eligibility by two readers. Of these, 177 were excluded for reasons such as not measuring a non-density feature, not reporting risk of breast cancer as an outcome, being an abstract or a duplicate paper, or not being published in English.
We identified 28 studies published since 2016 that met eligibility criteria as set out in the selection flowchart [25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52].
Of the 28 studies, only 7 were based on digitized analog film images [26, 38, 40, 47,48,49], 2 did not provide details [34, 37], and the others used full-field digital mammograms from Hologic, GE, or other manufacturers, or did not report details (see Table 1). The number of cases included in studies ranged from 20 up to 1900. Of the 28 studies, 8 included fewer than 100 cases [30, 35, 37, 41, 42, 46, 50, 51]. Most studies used a case–control design, although there were a few prospective and retrospective cohort studies.
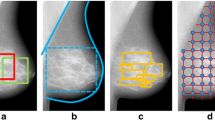
Tables 2 and 3 summarize how the texture features were identified in the mammographic images in studies not using the contralateral breast and those which did, respectively. These methods included defined masses or calcifications [29], or a predefined list of texture features such as 34 [31] or 44 [32] or even 112 [45] or 944 [44] initial features. Machine-driven identification of features was also reported. After machine identification, the features were reduced for analysis often based on statistical rules.
The approach to the assessment of breast parenchymal texture and side of body (ipsilateral or contralateral breast) varied across studies. Almost half of the studies (13 out of 28) used BIRADs as the baseline measure of density [28,29,30,31,32, 34,35,36, 41, 42, 48,49,50]. Others used Volpara and machine-derived density or Cumulus-like approaches. Time from mammogram to diagnosis of breast cancer ranged from under 24 months on average up to 82 months.
We next assessed the value added from the addition of texture features to prediction models for breast cancer. As noted in Tables 2 and 3, there was a substantial variation in the number of texture features included and the method of their identification for inclusion (human-defined or machine-identified). Many papers only reported on the association of texture with the risk of breast cancer using an odds ratio or relative risk. These were often contemporaneous with diagnosis (measured on contralateral breast) [26, 39, 44, 45, 52]. Model building details and results were not routinely reported. Tables 4 and 5 give the AUC for a baseline model without texture and then the value for the model with texture added when these were reported separately. Studies were not comparable across time horizon and baseline models. Hence, we did not proceed to a numerical quantitative summary such as meta-analysis of AUC values. However, within studies we saw that those that reported concordance statistics for models primarily reported results of models with MD and then MD plus texture features. In these studies, we saw an increase in reported concordance when texture features were added. The addition of parenchymal features often increased the AUC by 0.05 in studies not using the contralateral breast as presented in Table 6. Several studies using the contralateral breast at the time of cancer diagnosis noted even greater increases, such as Pertuz with a change in AUC from 0.609 to 0.786 when using texture features (Table 5) [52].
Reporting on established confounders for mammographic density varied across studies, with some accounting for age, body mass index, hormone therapy, and menopausal status while others considered fewer or even none in analyses. The prediction horizon, or how far ahead a model predicts breast cancer, was only defined for 3 of the studies [29, 30, 32] and was usually the time to the next routine screening mammogram, but less than 3 years on average. Examples are summarized to give more context to the details in the tables. Eriksson et al. [29] evaluated data from the KARMA cohort that followed 70,877 women for up to 3 years after baseline mammograms. The median time from the screening mammogram to breast cancer diagnosis was 1.74 years and 433 breast cancers were diagnosed. In their analysis, they used both 2- and 3-year horizons. The AUC improved from 0.64 for the model that included age, MD, and BMI to 0.71 after adding calcifications. Heidari 2018 [32] chose 4 features associated with the asymmetry of mammogram images from a pool of 44 machine-identified features. The time horizon was 12 to 18 months, defined as the time to the next screening mammogram. A machine learning classifier was built to predict breast cancer on the subsequent mammogram, reducing the features to a vector with 4 features. The AUC improved from 0.62 to 0.68.
Not all studies reported concordance statistics for their analysis, a metric to evaluate the predictions made by an algorithm defined as the proportion of concordant pairs divided by the total number of possible evaluation pairs. We summarized six studies in Table 6 that reported association measures for texture features with breast cancer [27, 28, 37, 41, 46, 47].
Results from the assessment of the risk of bias are shown in Additional file 1: Table S1. While many studies demonstrated similar risk of bias within specific domains, there was some variability, especially for study confounding. For study confounding, studies that adjusted for age, body mass index, menopausal status, and hormone therapy were considered to have a lower risk of bias.
Study reporting impacted our ability to rate the risk of bias. None of the studies reported information to judge study attrition risk of bias, leaving all with an unclear risk of bias. Likewise, for the study population, most studies did not report on the characteristics of the source population making it difficult to determine whether the population of interest was adequately represented.
Discussion
This review examined studies that evaluated the value of adding texture features to predict future breast cancer incidence or reported the association between these features and risk, of which we identified 28. Our findings suggest that risk prediction model performance increases when breast texture measures are added to mammographic breast density. The majority of studies evaluating future risk were limited to less than 3 years. Evidence using a longer interval from mammogram to diagnosis is necessary to be sufficient to guide breast cancer risk management or prevention [6, 53,54,55,56]. Results also demonstrate the need for a uniform approach to assess texture to enable comparison between studies.
The use of machine learning approaches to overcome variability in the assessment of BD has been reviewed recently [57]. The challenges of developing consistent approaches to the assessment of texture extend on that work. There is substantial variation in the methods used for defining and summarizing the measures of texture. No consistent approach is used to reduce the large number of predefined features, or machine-identified features, to a subset or summary for analysis. Studies also varied in their design. While most studies used a case–control design, some of these were nested in prospective cohorts, and other studies were retrospective cohort studies. Given this variation, we did not combine data across studies but note that comparison within studies shows that texture features are related to breast cancer incidence and improved concordance or AUC. Texture features are important contributors to breast cancer risk beyond mammographic breast density.
There have been some efforts on validating the texture features included in the studies in the literature. For example, the Tabár classification of parenchymal patterns has been shown to be highly reproducible [58] and several studies used a separate validation cohort. However, there is a need for more evidence evaluating these features, including external validation using different population characteristics.
There are several limitations to the studies included in this review. There was a large amount of variability in reporting established confounders of density, raising the issue of study confounding among studies that did not account for these established risk factors for density measures. Methods used may be nongeneralizable due to study specificities such as using different types of mammograms and different racial/ethnic populations. With short time periods between mammography and diagnosis of cancer, it is difficult to know whether studies using the ipsilateral breast are predicting breast cancer or merely detecting it. Some studies only provided evidence of an association rather than assessing the prediction performance of future risk, limiting their clinical translation. Large sample sizes are needed to validate associations, and a few studies had a small number of cases. Variation in the risk of bias observed in these studies reflects the variation in methods particularly in consideration of confounding. Level of reporting impacted our ability to fully assess the risk of bias in these studies.
We observed 5 studies using measures of texture that were measured or defined at the time of cancer diagnosis and from the contralateral breast [26, 39, 44, 45, 52]. Density was first evaluated as a risk factor for breast cancer using the contralateral breast at the time of diagnosis, and case–control studies have used an approach like this for decades in cancer epidemiology [59]. However, for assessing risk, examining features in the unaffected breast prior to diagnosis is a superior approach. Considering this previous work, we chose to include studies using the contralateral breast, but stratified tables in light of their limitations. We found that studies using the contralateral breast at the time of cancer diagnosis tended to report greater increases in AUC when adding parenchymal texture features.
To more effectively improve risk classification and prediction, we note the need for a harmonized strategy for assessing features across studies. The measurement challenge is a resource providing common mammogram images to identify the best method to measure mammographic density and predict breast cancer risk [60]. A similar project extends explorations to digital breast tomosynthesis and breast architecture distortions for use in screening and prediction model development [61].
In the 2016 review, Gastounioti et al. reviewed features of automated parenchymal texture analysis in relation to breast cancer risk [21]. This included details of methods to classify texture in mammographic images and its contribution to discrimination in case–control studies. Based on the review, they concluded that further research including large prospective studies is needed to establish the predictive value of parenchymal texture for ultimate inclusion in breast cancer risk prediction models. Such prediction models that extend to 5 and 10 years then require external validation to support clinical risk management. While we have a stronger base of evidence with more prospective studies in our review, our overall conclusions remain the same, though we emphasize the need for a coordinated strategy to enable greater comparisons and applicability of studies as well as studies using a longer prediction horizon.
Regarding our methods for this updated systematic review, we used the QUIPS tool [24] to assess the risk of bias. There are several limitations to the current review. The heterogeneity of the data did not allow for a meta-analysis. Additionally, systematic reviews are always subject to possible publication bias if all relevant studies have not been published. We used several strategies to reduce the risk of this including using a thorough search strategy designed by a medical librarian with expertise in searching for systematic reviews and searching clinicaltrials.gov for any ongoing studies.
For clinical use to guide precision prevention, we must identify both high-risk women for a range of risk reduction strategies [6] and low-risk women to consider the frequency of screening [62]. From this systematic literature review, we identify gaps in evidence to prioritize future studies. They include: (1) details on the prediction horizon for the risk of breast cancer; (2) other statistical approaches might also be used to assess the risk of breast cancer from the time of image acquisition that includes the texture features to the diagnosis of breast cancer such as survival analysis.
Conclusion
The addition of parenchymal texture features to risk prediction models generally resulted in improved performance beyond mammographic density. Despite current limitations in the literature, the more widespread use of digital mammography and availability of digital images including parenchymal features offer a growing opportunity to more uniformly assess image texture features. Incorporating these features into risk prediction models can improve risk classification and risk prediction, leading to improved breast cancer risk management such as tailoring screening interval and prevention strategies to the level of risk.
Availability of data and materials
Data are available upon reasonable request by contacting the corresponding author. All data relevant to the study are included in the article.
References
van Ravesteyn NT, van Lier L, Schechter CB, Ekwueme DU, Royalty J, Miller JW, et al. Transition from film to digital mammography: impact for breast cancer screening through the national breast and cervical cancer early detection program. Am J Prev Med. 2015;48(5):535–42.
Hopper JL, Nguyen TL, Schmidt DF, Makalic E, Song YM, Sung J, et al. Going beyond conventional mammographic density to discover novel mammogram-based predictors of breast cancer risk. J Clin Med. 2020;9(3):627.
Oeffinger KC, Fontham ET, Etzioni R, Herzig A, Michaelson JS, Shih YC, et al. Breast cancer screening for women at average risk: 2015 guideline update from the American Cancer Society. JAMA. 2015;314(15):1599–614.
Siu AL, Force USPST. Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2016;164(4):279–96.
Qaseem A, Lin JS, Mustafa RA, Horwitch CA, Wilt TJ, Clinical Guidelines Committee of the American College of P, et al. Screening for breast cancer in average-risk women: a guidance statement from the American College of Physicians. Ann Intern Med. 2019;170(8):547–60.
Bevers TB, Ward JH, Arun BK, Colditz GA, Cowan KH, Daly MB, et al. Breast cancer risk reduction, Version 2.2015. J Natl Compr Cancer Netw. 2015;13(7):880–915.
Louro J, Posso M, Hilton Boon M, Roman M, Domingo L, Castells X, et al. A systematic review and quality assessment of individualised breast cancer risk prediction models. Br J Cancer. 2019;121(1):76–85.
Brooks JD, Nabi HH, Andrulis IL, Antoniou AC, Chiquette J, Despres P, et al. Personalized risk assessment for prevention and early detection of breast cancer: integration and implementation (PERSPECTIVE I&I). J Pers Med. 2021;11(6):511.
Jiang S, Cao J, Rosner B, Colditz G. Supervised two-dimensional functional principal component analysis with time-to-event outcomes and mammogram imaging data. Biometrics. 2021. https://doi.org/10.1111/biom.13611
Pashayan N, Antoniou AC, Ivanus U, Esserman LJ, Easton DF, French D, et al. Personalized early detection and prevention of breast cancer: ENVISION consensus statement. Nat Rev Clin Oncol. 2020;17(11):687–705.
Boyd NF, Guo H, Martin LJ, Sun L, Stone J, Fishell E, et al. Mammographic density and the risk and detection of breast cancer. N Engl J Med. 2007;356(3):227–36.
Boyd NF, Rommens JM, Vogt K, Lee V, Hopper JL, Yaffe MJ, et al. Mammographic breast density as an intermediate phenotype for breast cancer. Lancet Oncol. 2005;6(10):798–808.
Ray KM, Price ER, Joe BN. Breast density legislation: mandatory disclosure to patients, alternative screening, billing, reimbursement. AJR Am J Roentgenol. 2015;204(2):257–60.
Bae JM, Kim EH. Breast density and risk of breast cancer in asian women: a meta-analysis of observational studies. J Prev Med Public Health. 2016;49(6):367–75.
Chiu SY, Duffy S, Yen AM, Tabar L, Smith RA, Chen HH. Effect of baseline breast density on breast cancer incidence, stage, mortality, and screening parameters: 25-year follow-up of a Swedish mammographic screening. Cancer Epidemiol Biomark Prev. 2010;19(5):1219–28.
Burton A, Maskarinec G, Perez-Gomez B, Vachon C, Miao H, Lajous M, et al. Mammographic density and ageing: a collaborative pooled analysis of cross-sectional data from 22 countries worldwide. PLoS Med. 2017;14(6):e1002335.
Soguel L, Diorio C. Anthropometric factors, adult weight gain, and mammographic features. Cancer Causes Control. 2016;27(3):333–40.
Yaffe MJ. Mammographic density. Measurement of mammographic density. Breast Cancer Res. 2008;10(3):209.
Kaufhold J, Thomas J, Eberhard J, Galbo C, Trotter DG. A calibration approach to glandular tissue composition estimation in digital mammography. Med Phys. 2002;29(8):1867–80.
Wolfe JN. Breast patterns as an index of risk for developing breast cancer. Am J Roentgenol. 1976;126(6):1130–7.
Gastounioti A, Conant EF, Kontos D. Beyond breast density: a review on the advancing role of parenchymal texture analysis in breast cancer risk assessment. Breast Cancer Res. 2016;18(1):91.
Lloyd-Jones DM. Cardiovascular risk prediction: basic concepts, current status, and future directions. Circulation. 2010;121(15):1768–77.
Lloyd-Jones DM, Liu K, Tian L, Greenland P. Narrative review: assessment of C-reactive protein in risk prediction for cardiovascular disease. Ann Intern Med. 2006;145(1):35–42.
Hayden JA, van der Windt DA, Cartwright JL, Cote P, Bombardier C. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158(4):280–6.
Abdolell M, Payne JI, Caines J, Tsuruda K, Barnes PJ, Talbot PJ, et al. Assessing breast cancer risk within the general screening population: developing a breast cancer risk model to identify higher risk women at mammographic screening. Eur Radiol. 2020;30(10):5417–26.
Ali MA, Czene K, Eriksson L, Hall P, Humphreys K. Breast tissue organisation and its association with breast cancer risk. Breast Cancer Res. 2017;19(1):103.
Azam S, Eriksson M, Sjolander A, Gabrielson M, Hellgren R, Czene K, et al. Mammographic microcalcifications and risk of breast cancer. Br J Cancer. 2021;125:759–65.
Choi WJ, Cha JH, Kim HH, Shin HJ, Chae EY. Analysis of prior mammography with negative result in women with interval breast cancer. Breast Cancer. 2016;23(4):583–9.
Eriksson M, Czene K, Pawitan Y, Leifland K, Darabi H, Hall P. A clinical model for identifying the short-term risk of breast cancer. Breast Cancer Res. 2017;19(1):29.
Evans KK, Culpan AM, Wolfe JM. Detecting the “gist” of breast cancer in mammograms three years before localized signs of cancer are visible. Br J Radiol. 2019;92(1099):20190136.
Gastounioti A, Hsieh MK, Cohen E, Pantalone L, Conant EF, Kontos D. Incorporating breast anatomy in computational phenotyping of mammographic parenchymal patterns for breast cancer risk estimation. Sci Rep. 2018;8(1):17489.
Heidari M, Khuzani AZ, Hollingsworth AB, Danala G, Mirniaharikandehei S, Qiu Y, et al. Prediction of breast cancer risk using a machine learning approach embedded with a locality preserving projection algorithm. Phys Med Biol. 2018;63(3):035020.
Heine J, Fowler E, Scott CG, Jensen MR, Shepherd J, Hruska CB, et al. Mammographic variation measures, breast density, and breast cancer risk. AJR Am J Roentgenol. 2021;217(2):326–35.
Hsu W, Zhou X, Petruse A, Chau N, Lee-Felker S, Hoyt A, et al. Role of clinical and imaging risk factors in predicting breast cancer diagnosis among BI-RADS 4 cases. Clin Breast Cancer. 2019;19(1):e142–51.
Kontos D, Winham SJ, Oustimov A, Pantalone L, Hsieh MK, Gastounioti A, et al. Radiomic phenotypes of mammographic parenchymal complexity: toward augmenting breast density in breast cancer risk assessment. Radiology. 2019;290(1):41–9.
Ma L, Cai Y, Lin X, He Z, Zeng H, Chen W, Qin G. Association of the differences in average glandular dose with breast cancer risk. BioMed Res Int. 2020;2020:8943659.
Li T, Tang L, Gandomkar Z, Heard R, Mello-Thoms C, Shao Z, et al. Mammographic density and other risk factors for breast cancer among women in China. Breast J. 2018;24(3):426–8.
Malkov S, Shepherd JA, Scott CG, Tamimi RM, Ma L, Bertrand KA, et al. Mammographic texture and risk of breast cancer by tumor type and estrogen receptor status. Breast Cancer Res. 2016;18(1):122.
Perez-Benito FJ, Signol F, Perez-Cortes JC, Pollan M, Perez-Gomez B, Salas-Trejo D, et al. Global parenchymal texture features based on histograms of oriented gradients improve cancer development risk estimation from healthy breasts. Comput Methods Programs Biomed. 2019;177:123–32.
Schmidt DF, Makalic E, Goudey B, Dite GS, Stone J, Nguyen TL, et al. Cirrus: an automated mammography-based measure of breast cancer risk based on textural features. JNCI Cancer Spectr. 2018;2(4):pky057.
Sorin V, Yagil Y, Shalmon A, Gotlieb M, Faermann R, Halshtok-Neiman O, et al. Background parenchymal enhancement at contrast-enhanced spectral mammography (CESM) as a breast cancer risk factor. Acad Radiol. 2020;27(9):1234–40.
Tagliafico AS, Valdora F, Mariscotti G, Durando M, Nori J, La Forgia D, et al. An exploratory radiomics analysis on digital breast tomosynthesis in women with mammographically negative dense breasts. Breast. 2018;40:92–6.
Tan M, Zheng B, Leader JK, Gur D. Association Between changes in mammographic image features and risk for near-term breast cancer development. IEEE Trans Med Imaging. 2016;35(7):1719–28.
Tan M, Mariapun S, Yip CH, Ng KH, Teo SH. A novel method of determining breast cancer risk using parenchymal textural analysis of mammography images on an Asian cohort. Phys Med Biol. 2019;64(3):035016.
Wang C, Brentnall AR, Cuzick J, Harkness EF, Evans DG, Astley S. A novel and fully automated mammographic texture analysis for risk prediction: results from two case–control studies. Breast Cancer Res. 2017;19(1):114.
Ward L, Heller S, Hudson S, Wilkinson L. Parenchymal pattern in women with dense breasts. Variation with age and impact on screening outcomes: observations from a UK screening programme. Eur Radiol. 2018;28(11):4717–24.
Warner ET, Rice MS, Zeleznik OA, Fowler EE, Murthy D, Vachon CM, et al. Automated percent mammographic density, mammographic texture variation, and risk of breast cancer: a nested case–control study. NPJ Breast Cancer. 2021;7(1):68.
Winkel RR, Euler-Chelpin MV, Lynge E, Diao P, Lillholm M, Kallenberg M, et al. Risk stratification of women with false-positive test results in mammography screening based on mammographic morphology and density: a case control study. Cancer Epidemiol. 2017;49:53–60.
Winkel RR, von Euler-Chelpin M, Nielsen M, Petersen K, Lillholm M, Nielsen MB, et al. Mammographic density and structural features can individually and jointly contribute to breast cancer risk assessment in mammography screening: a case–control study. BMC Cancer. 2016;16(1):414.
Yan S, Wang Y, Aghaei F, Qiu Y, Zheng B. Improving performance of breast cancer risk prediction by incorporating optical density image feature analysis: an assessment. Acad Radiol. 2022;29(Suppl 1):S199–210.
Yan S, Wang Y, Aghaei F, Qiu Y, Zheng B. Applying a new bilateral mammographic density segmentation method to improve accuracy of breast cancer risk prediction. Int J Comput Assist Radiol Surg. 2017;12(10):1819–28.
Pertuz S, Sassi A, Holli-Helenius K, Kämäräinen J, Rinta-Kiikka I, Lääperi AL, Arponen O. Clinical evaluation of a fully-automated parenchymal analysis software for breast cancer risk assessment: A pilot study in a Finnish sample. Eur J Radiol. 2019;121:108710.
Brentnall AR, Cuzick J, Buist DS, Bowles EJA. Long-term accuracy of breast cancer risk assessment combining classic risk factors and breast density. JAMA Oncol. 2018;4(9):e180174.
Evans DGR, Donnelly LS, Harkness EF, Astley SM, Stavrinos P, Dawe S, et al. Breast cancer risk feedback to women in the UK NHS breast screening population. Br J Cancer. 2016;114(9):1045–52.
Brentnall AR, Harkness EF, Astley SM, Donnelly LS, Stavrinos P, Sampson S, et al. Mammographic density adds accuracy to both the Tyrer-Cuzick and Gail breast cancer risk models in a prospective UK screening cohort. Breast Cancer Res. 2015;17(1):147.
Visvanathan K, Fabian CJ, Bantug E, Brewster AM, Davidson NE, DeCensi A, et al. Use of endocrine therapy for breast cancer risk reduction: ASCO clinical practice guideline update. J Clin Oncol. 2019;37(33):3152–65.
Gastounioti A, Desai S, Ahluwalia VS, Conant EF, Kontos D. Artificial intelligence in mammographic phenotyping of breast cancer risk: a narrative review. Breast Cancer Res. 2022;24(1):14.
Gao J, Warren R, Warren-Forward H, Forbes JF. Reproducibility of visual assessment on mammographic density. Breast Cancer Res Treat. 2008;108(1):121–7.
Pettersson A, Graff RE, Ursin G, Santos Silva ID, McCormack V, Baglietto L, et al. Mammographic density phenotypes and risk of breast cancer: a meta-analysis. J Natl Cancer Inst. 2014;106(5):dju078.
Dench E, Bond-Smith D, Darcey E, Lee G, Aung YK, Chan A, et al. Measurement challenge: protocol for international case–control comparison of mammographic measures that predict breast cancer risk. BMJ Open. 2019;9(12):e031041.
Buda M, Saha A, Walsh R, Ghate S, Li N, Swiecicki A, et al. A data set and deep learning algorithm for the detection of masses and architectural distortions in digital breast tomosynthesis images. JAMA Netw Open. 2021;4(8):e2119100.
Pace LE, Keating NL. Should women at lower-than-average risk of breast cancer undergo less frequent screening? J Natl Cancer Inst. 2021;113(8):953–4.
Pertuz S, Sassi A, Karivaara-Mäkelä M, Holli-Helenius K, Lääperi A-L, Rinta-Kiikka I, et al. Micro-parenchymal patterns for breast cancer risk assessment. Biomed Phys Eng Express. 2019;5(6):065008.
Funding
This work was supported by Breast Cancer Research Foundation grant number (BCRF 21-028) and in part by NCI (R37 CA256810).
Author information
Authors and Affiliations
Contributions
SJ and GAC planned the study. AA, CS, AH, SJ, and GAC drafted the manuscript. AA and YC extracted the data with CS resolving any discrepancies. AH searched the literature. AA and CS screened the studies and assessed the risk of bias. All authors reviewed and approved the final version of the manuscript. GAC is responsible for the overall content as guarantor. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study did not involve human subjects, and therefore oversight from an Institutional Review Board was not required.
Consent for publication
All authors have agreed to the final manuscript content and publication.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Risk of bias assessments for 28 included studies using QUIPS (sorted by year). Complete search strategy. PRISMA checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Anandarajah, A., Chen, Y., Colditz, G.A. et al. Studies of parenchymal texture added to mammographic breast density and risk of breast cancer: a systematic review of the methods used in the literature. Breast Cancer Res 24, 101 (2022). https://doi.org/10.1186/s13058-022-01600-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13058-022-01600-5