Abstract
Background
Breast density and microcalcifications are strongly associated with the risk of breast cancer. However, few studies have evaluated the combined association between these two factors and breast cancer risk. We investigated the association between breast density, microcalcifications, and risk of breast cancer.
Methods
This cohort study included 3,910,815 women aged 40–74 years who were screened for breast cancer between 2009 and 2010 and followed up until 2020. The National Health Insurance Service database includes national health-screening results from the national breast cancer screening program, which is an organized screening program provided every 2 years for all women aged 40 years or older. Breast density was assessed based on the Breast Imaging Reporting and Data System (BI-RADS) 4th edition, mostly through visual assessment by radiologists. The presence or absence of microcalcifications was obtained from the mammographic results. Cox proportional hazard regression for breast cancer risk was used to estimate hazard ratios (aHRs) adjusted for breast cancer risk factors.
Results
A total of 58,315 women developed breast cancer during a median follow-up of 10.8 years. Women with breast cancer had a higher proportion of microcalcifications than women without breast cancer (0.9% vs. 0.3%). After adjusting for breast density, women with microcalcification had a 3.07-fold (95% confidence interval [CI] 2.82–3.35) increased risk of breast cancer compared to women without microcalcification. The combined association between microcalcification and breast density dramatically increased the risk of breast cancer, corresponding to a higher level of breast density. Among postmenopausal women, the highest risk group was women with BI-RADS 4 and microcalcification. These women had more than a sevenfold higher risk than women with BI-RADS 1 and non-microcalcification (aHR, 7.26; 95% CI 5.01–10.53).
Conclusion
Microcalcification is an independent risk factor for breast cancer, and its risk is elevated when combined with breast density.
Similar content being viewed by others
Background
Breast cancer is the most common cancer and the fifth leading cause of cancer-related deaths, ranking first for incidence in 159 countries and mortality in 110 countries [1]. A population-based mammographic breast cancer screening program is cost-effective for reducing breast cancer mortality through early detection and appropriate treatment at an early stage [1]. The World Health Organization recommends organized mammographic screening every 2 years for women aged 50–69 years with an average risk in well-resourced settings [2]. In Korea, the national breast cancer screening program provides mammography screening for women aged 40 years or older every two years [3]. Mammographic breast cancer screening reduces mortality [4, 5]. It may reveal breast features that characterize benign breast disease and those that suggest an increased breast cancer risk, such as high breast density and an aberrant texture [4,5,6,7]. Studies have suggested that breast density and structural features identified through mammography increase breast cancer independently or jointly, suggesting personalized screening strategies using routine screening information [4,5,6,7].
Microcalcifications are deposits of calcium oxalate or calcium phosphate with a diameter of < 1 mm that can be identified on mammography as small bright dots [8]. Breast microcalcifications are not breast cancers themselves but represent approximately one-third of malignant breast lesions and are a well-recognized risk factor for breast cancer [9, 10]. In addition, women with dense breasts have an increased breast cancer risk compared to women with non-dense breasts [11]. A recent study suggested that a combination of mammographic features, including density, microcalcification, and mass, enables the identification of high-risk groups [12]. Although breast density and microcalcifications are well-recognized as strong independent risk factors for breast cancer, few studies have investigated the combined association of these two factors with breast cancer risk [9].
This study aimed to investigate the independent association between microcalcification and the risk of subsequent breast cancer, considering the effect of mammographic density, by using data from a retrospective cohort of East Asian women with normal mammographic breast cancer screening results. In addition, joint associations between breast density, microcalcifications, and breast cancer risk were assessed.
Methods
Settings and study population
This retrospective cohort study used claims data obtained from the National Health Information Database of the National Health Insurance Service, a compulsory health insurance system covering the entire Korean population. The database includes information on demographics, healthcare utilization, vital statistics, and national health-screening results [13]. In addition, mammographic screening information was obtained from breast cancer screening program data, which were provided every two years for all women aged 40 years or older [14].
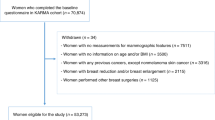
The initial cohort included 4,873,325 women aged 40–74 who underwent breast cancer screening between 2009 and 2010 and were followed up until the date of breast cancer diagnosis, date of death, or December 31, 2020, whichever came first (Fig. 1). If participants underwent mammographic screening more than once during the study period, we used data from the first screening. The following exclusion criteria were applied to select women included in the analysis: (1) participants who were diagnosed with any cancer or died within 3 months of screening to avoid the possibility of including screening-detected cancer; (2) participants whose mammographic screening results were suspicious abnormalities, highly suggestive of malignancy, or incomplete; and (3) participants whose main exposure information was missing (breast density or microcalcification). In total, 3,910,815 women who underwent negative screening were included in the analysis.
The study was approved by the Institutional Review Board (approval no. HYUIRB-202106-003-1). The requirement for informed consent was waived because the database was constructed after anonymization of individual identities. This work was supported by a National Research Foundation of Korea grant funded by the Korean government (MSIT) (grant no. 2021R1A2C1011958). This work was partly supported by Institute of Information & Communications Technology Planning & Evaluation (IITP) grant funded by the Korea government (MSIT) (No.2020-0-01,373, Artificial Intelligence Graduate School Program (Hanyang University)) and the research fund of Hanyang University (HY- 202,100,000,670,061).
Mammographic breast density and microcalcification
Information on mammographic breast density and microcalcification was extracted from the mammography screening results, which were read by trained radiologists at each screening center. The results of the Korean national breast cancer screening were recorded based on the BI-RADS 4th edition since 2009. Each breast’s density was assessed according to the BI-RADS 4th edition guidelines (< 25% glandular tissue, BI-RADS 1; 25–50% glandular tissue, BI-RADS 2; 50–75% glandular tissue, BI-RADS 3; > 75% glandular tissue, BI-RADS 4) and the presence and location of a mass, typically benign calcification, microcalcification, asymmetry, architectural distortion, and associated features, were recorded. Based on these findings, the final assessment of the BI-RADS category was recorded. Microcalcification was defined as a record of microcalcification in the mammography results.
Breast cancer cases
In Korea, the national health insurance policy has set a cost-sharing rate from 0 to 10% of the total medical expenditures for patients with high medical expenses, including severe diseases such as cancer, rare diseases, and incurable diseases [15]. Thus, patients with cancer have a special payment reduction program. Incident cancer cases are registered in this system, and special codes are given to cancer patients in the NHID. The ascertainment of cancer cases in our study was obtained from the healthcare utilization database using a combination of ICD-10 codes for breast cancer and catastrophic illness codes. The primary outcome was a breast cancer event, which was defined as a combination of the International Classification of Disease-10 code of invasive breast cancer (C50) or ductal carcinoma in situ (D05), in combination with the catastrophic illness code. This definition of cancer has a sensitivity of 98.1% compared with that of the Korean Central Cancer Registry, which contains a register of 90% of cancer cases nationwide [16].
Covariates
We considered the following variables for adjustment in the analysis: age at screening, the cut-off for BMI was applied according to the WHO Asia–Pacific recommendation, which defines overweight as BMI ≥ 23 kg/m2 and obesity as BMI ≥ 25 kg/m2 [17, 18], family history of breast cancer among first-degree relatives, number of delivered children, smoking (experience of smoking), alcohol consumption (drinking even once a week), physical activity (high-or moderate-intensity, or walking at least once a week), age at menarche, history of breastfeeding, and use of oral contraceptives. For postmenopausal women, the age at menopause, menopausal status, and history of hormone replacement therapy were also included as adjustment factors. Except for BMI, information on the above-mentioned covariates was collected using standardized questionnaires and self-reported by the participants at each screening center during health examinations and cancer screening.
Statistical analysis
The distribution of breast cancer events in our cohort was described with respect to the presence of microcalcifications (Additional file 1: Appendix 1). Descriptive statistics of baseline characteristics at the screening examination of study participants who developed breast cancer were compared using the chi-square test or Student’s t-test. The 5-year risk of developing breast cancer was calculated according to the BI-RADS density category for those with and without microcalcification, and menopausal status among all participants. The 5-year breast cancer risk was estimated as the number of cases diagnosed with breast cancer within 5 years of screening. Additionally, the Gray test was used to identify the equality of the cumulative incidence functions between the two groups. To quantify the association between microcalcification and the risk of breast cancer, Cox proportional hazard regression (HR) analysis was used to model the time from screening to breast cancer diagnosis with adjustment for other covariates. The assumption of proportional hazards was examined using Kaplan–Meier curves, and parallel lines of the log–log survival distribution function were identified. In the Cox regression model, breast cancer events were the primary outcomes. All participants were followed up until the date of any cancer diagnosis, including breast cancer diagnosis, date of death, or December 31, 2020, which ever came first. The censored cases were those who did not develop breast cancer (including other types of cancer development or death) or were alive until December 31, 2020. To quantify the independent association between microcalcification and breast cancer risk, analyses were performed with and without adjustments for breast density together with adjustment for other covariates. The analysis was conducted on the total population and further stratified by menopausal status. Finally, to quantify the joint associations between breast density, microcalcification, and breast cancer risk, the participants were classified into a combination of BI-RADS category and the presence of microcalcification, and the HR was presented with women with BI-RADS density category 1 and no microcalcification as the reference group. In addition, we assessed the effect of microcalcification on breast cancer risk by breast density category and then assessed the significant interaction of these two factors on breast cancer risk using the extra-sum of square F test. Additionally, to evaluate the trend of breast density categories across the development of breast cancer and the comparison by the presence of microcalcification, we obtained the p-value for trend from the asymptotic test to evaluate the trend between the exposure and the outcome. All reported p-values were two-sided with a type I error (α < 0.05) and were considered statistically significant. Statistical analyses were performed using the SAS statistical software (version 9.4; SAS Institute, Cary, NC, USA).
Results
Among the 3,910,815 women included in the analysis (Fig. 1), 58,315 were diagnosed with breast cancer during a median follow-up of 10.8 years. After screening, average time of breast cancer diagnosis was 8.2 ± 1.8 years in all women. In women with microcalcifications, the average time of breast cancer diagnosis was 7.9 ± 1.8 years, whereas in women without microcalcifications, the average time of breast cancer diagnosis was 8.5 ± 1.8 years. Baseline characteristics of the women included in this study are shown in Table 1. The mean age of the women at screening was 54.69 ± 9.6 years. The proportion of women with microcalcifications was 0.3%, and that of women with dense breasts (BI-RADS density classifications 3 and 4) was 38.4%. Women with a breast cancer development had a higher proportion of microcalcifications and dense breasts than women without a breast cancer development (0.9% vs. 0.3% for microcalcifications and 38.4% vs. 55.4% for BI-RADS breast density, respectively).
Overall, women with microcalcifications had a higher 5-year risk of breast cancer than those without microcalcifications in all the BI-RADS density categories (Table 2). In the total study population, the 5-year breast cancer risk was 0.60% (95% confidence interval [CI] 0.60–0.61). As the BI-RADS density category increased, the 5-year breast cancer risk increased, irrespective of the presence of microcalcifications. Overall, in women with microcalcification, the 5-year risk increased from 1.69% (95% CI 1.15–2.40) in BI-RADS 1 to 3.93% (95% CI 3.10–4.91) in BI-RADS 4. Women with microcalcification had a higher 5-year breast cancer risk, regardless of menopausal status and BI-RADS density categories. Overall, and in most categories, higher 5-year breast cancer risk were observed in premenopausal women than in postmenopausal women. However, postmenopausal women with microcalcification had a higher 5-year breast cancer risk than premenopausal women in BI-RADS density category 2, (2.11% [95% CI 1.32–3.21] vs. 2.77% [95% CI 2.09–3.60]), as well as category 4 (4.41% [95% CI 2.75–6.65] vs. 3.85% [95% CI 2.91–4.98]). Additional file 2: Appendix 2 shows the cumulative incidence over time since mammography was based on the presence/absence of microcalcifications. Overall, in all breast density groups, women with microcalcifications had a higher risk than those without microcalcifications. In BI-RADS 4, the 5-year risk of women without microcalcifications was 2.77% (95% CI 2.73–2.82) but that of women with microcalcifications was 8.39% (95% CI 7.80–9.00).
The associations between microcalcification and the risk of subsequent breast cancer, with and without adjustment for breast density, are presented in Table 3. In the model without adjustment for density, microcalcification was associated with a more than threefold increase in the risk of breast cancer in premenopausal and postmenopausal women. After adjusting for breast density, despite a slight decrease in the strength of the association, hazard ratios were all greater than threefold (3.09 [95% CI 2.83–3.36] in all women, 3.07 [95% CI 2.74–3.44] in premenopausal women, and 3.09 [95% CI 2.70–3.53] in postmenopausal women. Additionally, women with microcalcification were at increased risk of DCIS by fourfold (4.02 [95% CI 3.44–4.69]) and IBC risk by threefold (2.99 [95% CI 2.72–3.27]) after adjusting for breast density.
The joint associations between microcalcification, breast density, and risk of breast cancer are shown in Table 4. Among women with BI-RADS density category 1, those with microcalcifications had a 3.42-fold (95% CI 2.60–4.50) increased risk of breast cancer. Compared to women with BI-RADS 1 but without microcalcification, women with BI-RADS category 4 had a 2.30-fold (95% CI 2.22–2.37) increased risk of breast cancer. Women with BI-RADS 4 breast density and microcalcification had a 6.65-fold (adjusted hazard ratio [aHR], 6.65; 95% CI 5.59–7.72). Among premenopausal women, the hazard ratios increased corresponding to a higher level of breast density, reaching a value of 5.95 (95% CI 4.87–7.28, p for trend = 0.004) in women with microcalcification and BI-RADS 4 compared with women with BI-RADS 1 but without microcalcification. In postmenopausal women, participants with BI-RADS 4 and microcalcification had a more than sevenfold higher risk of breast cancer (aHR, 7.26; 95% CI 5.01–10.53) compared with women with BI-RADS1 and without microcalcification. Additionally, the joint associations between microcalcification, breast density, and risk of breast cancer are shown with respect to breast cancer subtype. Women with BI-RADS 4 and microcalcification had a sixfold higher risk of invasive breast cancer (aHR, 6.27; 95% CI 5.19–7.57) than women with BI-RADS 1 and without microcalcification. However, women with BI-RADS 4 and microcalcification had an eightfold higher risk of DCIS (aHR, 8.30; 95% CI 3.95–17.47) than women with BI-RADS 1 and without microcalcification which indicates that there was an interaction effect between breast density and the presence of microcalcification on the risk of breast cancer (p < 0.001).
Discussion
In this large population-based cohort, we found that women with microcalcification detected during mammographic screening had an approximately threefold increased risk of breast cancer relative to women without microcalcification, regardless of menopausal status. The association between microcalcification and breast cancer risk did not change significantly after adjusting for breast density, suggesting an independent association that was not confounded by breast density. Both microcalcification and higher breast density categories increased breast cancer risk, suggesting a joint association of microcalcification and higher breast density with breast cancer risk. Women with microcalcification and BI-RADS density category 4 had an approximately sixfold higher risk of breast cancer than women without microcalcification and BI-RADS category 1.
Previous studies have shown an association between microcalcification identified during mammographic screening and an increased risk of breast cancer [9, 19], as we found in this study. Other studies suggested that as the number of microcalcification clusters increases, the risk of breast cancer and ductal carcinoma in situ likewise increases [8, 12, 20, 21]. When subjects were stratified by menopausal status, Azam et al. showed that the presence of three or more microcalcification clusters had a higher association with premenopausal breast cancer risk than postmenopausal breast cancer risk [9]. In this study, the overall association between microcalcification and breast cancer risk was observed in both premenopausal and postmenopausal women, with similar HRs in both groups. However, in women with BI-RADS density category 1, the association between microcalcification and breast cancer risk was stronger in premenopausal women than in postmenopausal women. In women with BI-RADS density categories 2–4, the association of microcalcification was higher in postmenopausal women than in premenopausal women or similar in both groups.
Microcalcification is more prevalent in older patients [9] and is affected by epithelial-mesenchymal transition [22], cell necrosis, and debris [19]. A previous study showed that age, breast density, genetic predictors of breast cancer, having more than two children, and long breastfeeding periods are associated with an increased risk of microcalcification clusters [9]. Other studies have revealed that body mass index, smoking, and alcohol consumption could be negatively associated with microcalcification clusters because of the protective effect of estrogen [23, 24]. Although breast density and breast microcalcification are independently associated with breast cancer, the relationship between these two factors and age is the opposite. While breast density decreases with increasing age [25], the number of microcalcification clusters increases with age increases [9]. The age-dependent prevalence of the microcalcification clusters could be explained by the effect of normal aging due to epithelial-mesenchymal transition over age [26]. A recent Swedish population study indicated that microcalcification clusters can be observed as a complementary risk indicator of breast cancer [20], whereas mammographic density is a strong risk factor for breast cancer [27].
It is unclear whether microcalcification is a risk factor for benign breast diseases, breast cancer, or an early detection marker for these diseases [28]. Microcalcification is not only a risk factor for breast cancer, but also a potential surrogate for breast cancer recurrence [32] and a prognostic marker for residual disease after excision [29]. Microcalcification can be used to indicate where breast cancer develops and when it appears [19]. However, in this study, by excluding those with mammographic screening results of suspected breast cancer cases or incomplete and developed breast cancer within three months of screening, microcalcifications with malignancy potential (surrogate marker of breast cancer) could be excluded at baseline. Thus, the results of this study suggest that microcalcifications, but not microcalcifications with malignant potential, are a risk factor for breast cancer.
Our study had several limitations, mainly because the definition of microcalcification was solely based on mammography results as information regarding biopsy results was unavailable in the National Health Insurance Service database. Despite the absence of biopsy results to explain the pathological information in detail, our results suggest a normal screening process that can be directly applied in screening settings. In the Korean National Breast Cancer Screening setting, it is not mandatory for at least two radiologists to interpret screening mammograms according to European guidelines [30]. Therefore, the breast density, presence of microcalcification, and BI-RADS classification were read by a single radiologist at each screening center. Although the BI-RADS classification has been extensively assessed, the results may vary depending on the skill and ability of the radiologist. However, in Korea, there is a standardized mammography education program that can increase the quality of interpretation [31]. In addition, inter-radiologist variability was assessed in randomly selected films from the Korean National Breast Cancer Screening Program, and the results showed an inter-radiologist variability of 0.83, which suggests high agreement in performance [32]. Another point should be noted that in proportion of women with family history of breast cancer in our study is relative lower than reported among western population [1]. A previous study on women from the western countries showed that approximately 15% of the women had a family history of breast cancer within their first-degree relatives [33]. Differences in the proportion of family history of breast cancer in women from the West and Korea might be related to different baseline breast cancer incidences in the population by race (lower breast cancer incidence in women from Asia compared with women from the West) [1]. A study conducted in women from Korea showed a similar proportion of family history of breast cancer as our result [34].
Despite these limitations, this study included approximately 4 million women from a population-based national breast cancer screening, which represents the demographic composition of women in Korea and other East Asian populations. Another point worth mentioning is that even though the association between microcalcification and increased breast cancer risk has been studied in published works [9, 19, 27], few studies have considered the combination of microcalcification, breast density, and breast cancer risk with additional stratification by menopausal status. To the best of our knowledge, this study is the largest cohort study to provide evidence of an increased risk of breast cancer in women with microcalcifications, with additional consideration of breast density. Hence, this large national cohort study with prospective ascertainment of breast cancer cases provides new evidence for the combined association of microcalcification and breast density at the population level, advancing existing interventions for the early detection of cancer among women with microcalcification and dense breasts who have a higher breast cancer risk.
Conclusions
We found that microcalcification was an independent risk factor for breast cancer and that the risk increased when combined with breast density. To the best of our knowledge, our study is the first comprehensive study to use national breast cancer screening to study microcalcification and shed light on the risk of breast cancer associated with the presence of microcalcification.
Availability of data and materials
The data that support the findings of this study are available from the NHIS, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. However, the data are available from the authors upon reasonable request and with permission from the NHIS.
Abbreviations
- BI-RADS:
-
The breast imaging reporting and data systems
- aHRs:
-
Adjusted hazard ratios
- CI:
-
Confidence interval
- HR:
-
The hazard ratio
- BMI:
-
Body mass index
- SD:
-
Standard deviation
- NA:
-
Not applicable
- NO:
-
Number
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F: Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: Cancer J Clinic 2021, 71(3):209–249.
Yaffe MJ. Mammographic density. Measurement of mammographic density. Breast Cancer Res. 2008;10(3):1.
Lee EH, Park B, Kim N-S, Seo H-J, Ko KL, Min JW, Shin M-H, Lee K, Lee S, Choi N, et al. The Korean guideline for breast cancer screening. J Korean Med Assoc. 2015;58(5):569.
Warner ET, Rice MS, Zeleznik OA, Fowler EE, Murthy D, Vachon CM, Bertrand KA, Rosner BA, Heine J, Tamimi RM. Automated percent mammographic density, mammographic texture variation, and risk of breast cancer: a nested case-control study. NPJ Breast Cancer. 2021;7(1):68.
Winkel RR, von Euler-Chelpin M, Nielsen M, Petersen K, Lillholm M, Nielsen MB, Lynge E, Uldall WY, Vejborg I. Mammographic density and structural features can individually and jointly contribute to breast cancer risk assessment in mammography screening: a case–control study. BMC Cancer. 2016;16(1):414.
Kim S, Tran TXM, Song H, Ryu S, Chang Y, Park B. Mammographic breast density, benign breast disease, and subsequent breast cancer risk in 3.9 million Korean women. Radiology. 2022;304(3):212727.
Tran TXM, Kim S, Song H, Park B. Mammographic breast density, body mass index and risk of breast cancer in Korean women aged 75 years and older. Int J Cancer. 2022;151(6):869.
Henrot P, Leroux A, Barlier C, Genin P. Breast microcalcifications: the lesions in anatomical pathology. Diagn Interv Imaging. 2014;95(2):141–52.
Azam S, Eriksson M, Sjölander A, Gabrielson M, Hellgren R, Czene K, Hall P. Mammographic microcalcifications and risk of breast cancer. Br J Cancer. 2021;125(5):759–65.
Holowko N, Eriksson M, Kuja-Halkola R, Azam S, He W, Hall P, Czene K. Heritability of mammographic breast density, density change, microcalcifications, and masses. Cancer Res. 2020;80(7):1590–600.
Kim S, Park B. Association between changes in mammographic density category and the risk of breast cancer: a nationwide cohort study in East-Asian women. Int J Cancer. 2021;148(11):2674–84.
Eriksson M, Czene K, Pawitan Y, Leifland K, Darabi H, Hall P. A clinical model for identifying the short-term risk of breast cancer. Breast Cancer Res: BCR. 2017;19(1):29.
Bahk J, Kim YY, Kang HY, Lee J, Kim I, Lee J, Yun SC, Park JH, Shin SA, Khang YH. Using the national health information database of the national health insurance service in Korea for monitoring mortality and life expectancy at national and local levels. J Korean Med Sci. 2017;32(11):1764–70.
Cheol Seong S, Kim YY, Khang YH, Heon Park J, Kang HJ, Lee H, Do CH, Song JS, Hyon Bang J, Ha S, et al. Data resource profile: the national health information database of the national health insurance service in South Korea. Int J Epidemiol. 2017;46(3):799–800.
Kim S, Kwon S. Impact of the policy of expanding benefit coverage for cancer patients on catastrophic health expenditure across different income groups in South Korea. Soc Sci Med. 2015;138:241–7.
Yang MS, Park M, Back JH, Lee GH, Shin JH, Kim K, Seo HJ, Kim YA. Validation of cancer diagnosis based on the national health insurance service database versus the national cancer registry database in Korea. Cancer Res Treat. 2021;54(2):352.
Organization WH: The Asia-Pacific perspective: redefining obesity and its treatment. 2000.
Kim MK, Lee WY, Kang JH, Kang JH, Kim BT, Kim SM, Kim EM, Suh SH, Shin HJ, Lee KR, Lee KY. 2014 clinical practice guidelines for overweight and obesity in Korea. Endocrinol Metabol. 2014;29(4):405–9.
Ali MA, Czene K, Hall P, Humphreys K. Association of microcalcification clusters with short-term invasive breast cancer risk and breast cancer risk factors. Sci Rep. 2019;9(1):1–8.
Hofvind S, Iversen BF, Eriksen L, Styr BM, Kjellevold K, Kurz KD. Mammographic morphology and distribution of calcifications in ductal carcinoma in situ diagnosed in organized screening. Acta Radiol. 2011;52(5):481–7.
Castells X, Domingo L, Corominas JM, Tora-Rocamora I, Quintana MJ, Bare M, Vidal C, Natal C, Sanchez M, Saladie F, et al. Breast cancer risk after diagnosis by screening mammography of nonproliferative or proliferative benign breast disease: a study from a population-based screening program. Breast Cancer Res Treat. 2015;149(1):237–44.
Stomper PC, Geradts J, Edge SB, Levine EG. Mammographic predictors of the presence and size of invasive carcinomas associated with malignant microcalcification lesions without a mass. Am J Roentgenol. 2003;181(6):1679–84.
Lochner DM, Brubaker KL. Incidence of malignancy in hormone therapy users with indeterminate calcifications on mammogram. Am J Obstet Gynecol. 2006;194(1):82–5.
Schnatz PF, Rotter MA, Hadley S, Currier AA, O’Sullivan DM. Hormonal therapy is associated with a lower prevalence of breast arterial calcification on mammography. Maturitas. 2007;57(2):154–60.
Liao Y-S, Zhang J-Y, Hsu Y-C, Hong M-X, Lee L-W. Age-specific breast density changes in Taiwanese women: a cross-sectional study. Int J Environ Res Public Health. 2020;17(9):3186.
Santos F, Moreira C, Nóbrega-Pereira S. Bernardes de Jesus B: new insights into the role of epithelial-mesenchymal transition during aging. Int J Mol Sci. 2019;20(4):891.
Boyd NF, Martin LJ, Yaffe MJ, Minkin S. Mammographic density and breast cancer risk: current understanding and future prospects. Breast cancer research : BCR. 2011;13(6):223.
Tot T, Gere M, Hofmeyer S, Bauer A, Pellas U: The clinical value of detecting microcalcifications on a mammogram. In: Seminars in cancer biology: Elsevier; 2021: 165–174.
Koca B, Kuru B, Yuruker S, Gokgul B, Ozen N. Factors affecting surgical margin positivity in invasive ductal breast cancer patients who underwent breast-conserving surgery after preoperative core biopsy diagnosis. J Korean Surg Soc. 2013;84(3):154–9.
Perry N, Broeders M, de Wolf C, Törnberg S, Holland R, von Karsa L. European guidelines for quality assurance in breast cancer screening and diagnosis -summary document. Oncol Clinic Prac. 2008;4(2):74–86.
Lee EH, Jun JK, Jung SE, Kim YM, Choi N. The efficacy of mammography boot camp to improve the performance of radiologists. Korean J Radiol. 2014;15(5):578–85.
Jo H-M, Song S, Lee EH, Ko K, Kang BJ, Cha JH, Yi A, Jung HK, Jun JK. Interpretive volume and inter-radiologist agreement on assessing breast density. J Korean Soc Breast Screening. 2018;15:15–22.
Brewer HR, Jones ME, Schoemaker MJ, Ashworth A, Swerdlow AJ. Family history and risk of breast cancer: an analysis accounting for family structure. Breast Cancer Res Treat. 2017;165(1):193–200.
Choi HG, Park JH, Choi YJ, Suh YJ. Association of family history with the development of breast cancer: a cohort study of 129,374 women in KoGES data. Int J Environ Res Publ Health. 2021;18(12):6409.
Acknowledgements
This work was supported by a National Research Foundation of Korea grant funded by the Korean government (MSIT) (grant no. 2021R1A2C1011958). This work was partly supported by Institute of Information & communications Technology Planning & Evaluation (IITP) grant funded by the Korea government (MSIT) (No.2020-0-01373, Artificial Intelligence Graduate School Program (Hanyang University)) and the research fund of Hanyang University (HY- 202100000670061)
Author information
Authors and Affiliations
Contributions
SK analyzed and drafted the manuscript. MT designed the study and drafted the manuscript. HS analyzed and revised the manuscript substantively. BP substantially contributed to the conception and revised the manuscript. All authors read and approved by the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of Hanyang University College of Medicine (approval no. HYUIRB-202106–003-1). The National Health Insurance Service (NHIS) granted permission to use the NHIS database. Informed consent was waived because all screened populations agreed to transfer their screening results to the NHIS, and the NHIS database was constructed after anonymization of individual identities.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Histogram of the time distribution from study enrollment (date of mammographic breast cancer screening) to breast cancer diagnosis in incident breast cancer cases. A Total breast cancer. B Total breast cancer cases without microcalcifications. C Total breast cancer cases with microcalcifications.
Additional file 2:
Cumulative incidence over time since mammography was based on the presence/absence of microcalcifications and mammographic breast density. P-values were calculated using the Gray test. A BI-RADS 1; B BI-RADS 2; C BI-RADS 3; D BI-RADS 4. BI-RADS: Breast Imaging Reporting and Data System.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kim, S., Tran, T.X.M., Song, H. et al. Microcalcifications, mammographic breast density, and risk of breast cancer: a cohort study. Breast Cancer Res 24, 96 (2022). https://doi.org/10.1186/s13058-022-01594-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13058-022-01594-0