Abstract
Background
Approximately 100 common breast cancer susceptibility alleles have been identified in genome-wide association studies (GWAS). The utility of these variants in breast cancer risk prediction models has not been evaluated adequately in women of Asian ancestry.
Methods
We evaluated 88 breast cancer risk variants that were identified previously by GWAS in 11,760 cases and 11,612 controls of Asian ancestry. SNPs confirmed to be associated with breast cancer risk in Asian women were used to construct a polygenic risk score (PRS). The relative and absolute risks of breast cancer by the PRS percentiles were estimated based on the PRS distribution, and were used to stratify women into different levels of breast cancer risk.
Results
We confirmed significant associations with breast cancer risk for SNPs in 44 of the 78 previously reported loci at P < 0.05. Compared with women in the middle quintile of the PRS, women in the top 1% group had a 2.70-fold elevated risk of breast cancer (95% CI: 2.15–3.40). The risk prediction model with the PRS had an area under the receiver operating characteristic curve of 0.606. The lifetime risk of breast cancer for Shanghai Chinese women in the lowest and highest 1% of the PRS was 1.35% and 10.06%, respectively.
Conclusion
Approximately one-half of GWAS-identified breast cancer risk variants can be directly replicated in East Asian women. Collectively, common genetic variants are important predictors for breast cancer risk. Using common genetic variants for breast cancer could help identify women at high risk of breast cancer.
Similar content being viewed by others
Background
Genome-wide association studies (GWAS) to date have identified approximately 100 genetic loci associated with breast cancer risk [1–12]. Approximately 10 of these loci were initially identified in GWAS conducted in East Asian descendants [7–12]. Virtually all other loci were initially identified in studies conducted with European descendants. In a recent study, we confirmed a significant association in East Asian women for 31 of the 67 independent breast cancer susceptibility loci reported from previous GWAS conducted mostly in European descendants [13]. Previously we constructed an eight-SNP polygenic risk score (PRS) and found it to be the third strongest predictor for breast cancer risk, behind waist-to-hip ratio and previous benign breast disease. Adding the PRS to a predictive model including these two risk factors increases the area under the receiver operating characteristic curve (AUC) from 0.6178 to 0.6295 [7]. More recently, a relatively small study with 411 breast cancer cases and 1212 controls conducted in Singapore Chinese participants reported that a PRS constructed from 51 SNPs improved the classification of 6.2% of the women for their absolute risk of breast cancer in the next 5 years [14].
We have recently identified several new genetic variants associated with breast cancer risk among women of Asian ancestry [8–12]. As more breast cancer risk-related genetic variants are found, it is important to investigate the public health impact of those genetic variants to identify susceptible subgroups of individuals at elevated breast cancer risk to provide cost-efficient prevention strategies and to make appropriate healthcare decisions. In this study, we investigate the value of genetic information in predicting breast cancer risk in women of East Asian ancestry.
Methods
Study populations
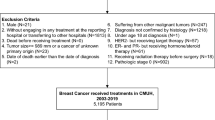
This study gathered data from 11 participating case–control studies from three sources: 12,893 women (6269 cases and 6624 controls) of East Asian origin participating in nine studies in the Breast Cancer Association Consortium (BCAC) that were conducted in China, Japan, South Korea, Thailand, and Malaysia; 5152 Chinese women (2867 cases and 2285 controls) from the Shanghai Genome-Wide Association Studies (SGWAS) who were participants in the Shanghai Breast Cancer Study (SBCS), the Shanghai Breast Cancer Survival Study (SBCSS), and the Shanghai Women’s Health Study (SWHS) (the SBCS is a population-based case–control study, and the SBCSS and SWHS are ongoing population-based, prospective cohort studies—all participants in these studies were recruited in Shanghai during the same time period from 1996 to 2005 using similar study protocols); and 5522 Chinese women (2769 cases and 2753 controls) who were participants in Stage 2 of the Shanghai breast cancer Genome-Wide Association Studies (SGWAS-stage2) [11]. In total, 23,567 women of East Asian ancestry (11,905 cases and 11,662 controls) were included in the current analysis (Additional file 1: Table S1). All participating studies obtained written, informed consent from all subjects and approval from their respective Institutional Review Boards. No participant received a stipend.
Genotyping methods
Samples from the nine studies in the BCAC were genotyped using a custom Illumina iSelect array (iCOGS) comprising 211,155 SNPs, as part of a large collaboration for replication and fine-mapping of promising associations selected from GWAS of multiple cancers. Detailed information about the quality control (QC) has been described previously [5, 13]. Briefly, SNPs which had a call rate < 95%, deviated from Hardy–Weinberg equilibrium in controls at P < 10−7, or had genotype discrepancies in >2% of duplicate samples were excluded across all Collaborative Oncological Gene–environment Study (COGS) consortia.
The SGWAS samples were genotyped using Affymetrix 6.0, comprising 906,602 SNPs, and Affymetrix 500 K array, comprising approximately 500,000 SNPs [7]. Genetically identical and unexpected duplicate samples were excluded, as were close relatives with a pairwise proportion of identify-by-descent estimate > 0.25. All samples with a call rate < 95% were excluded. SNPs were excluded if the minor allele frequency was <1% or the genotyping concordance rate was <95% in the QC sample.
The SGWAS-stage2 samples were genotyped using an exome chip comprising approximately 50,000 SNPs with minor allele frequency over 1%, which included most of the GWAS-identified breast cancer variants [11].
Most SNPs included in this analysis were genotyped directly, and some SNPs were imputed using IMPUTE and the 1000 Genomes data as a reference panel.
Statistical methods
A total of 88 SNPs at 78 breast cancer loci identified to date were included in this analysis. First, we evaluated associations between each SNP and breast cancer risk using logistic regression, assuming a log-additive genetic model with adjustment for age, population structure (principal components), and study sites, when applicable. We analyzed the association between each SNP and breast cancer risk separately for each data source. The final associations, combining the three sources, were derived using fixed-effect meta-analysis with inverse-variance weights. Any SNP with an association P < 0.05 (one-sided) was considered statistically significant. Tests for pairwise SNP by SNP interactions were also evaluated using logistic regression under the log-additive genetic model with the same adjustments already stated.
Second, to investigate the association between breast cancer risk and the combined effects of all significant SNPs, a PRS was derived for each study participant using the formula:
where β i is the per-allele log odds ratio (OR) for breast cancer associated with the risk allele for SNP i , which is the number of risk alleles (0, 1, or 2) for the SNP, and n is the total number of significant SNPs. Thus, the PRS summarizes the combined effect of SNPs having significant association with breast cancer risk.
Under the multiplicative polygenic model, and given a large number of unlinked loci, each conferring a small effect, the population distribution of the PRS is normal (F = N(μ, σ 2)), with mean value μ and variance σ 2 [15, 16]:
where p i is the effect allele frequency of the SNP i , q i = 1 − p i , and β i is the log OR.
The distribution of the PRS in breast cancer cases is also normal (G = N(μ', σ'2)), with the parameters μ' = μ + σ 2 and σ'2 = σ 2 [15, 16].
Third, the discriminative accuracy of using the PRS to predict breast cancer risk was evaluated with the AUC, which was calculated theoretically [17, 18] given that the PRS distributions (F, G) are known:
Additionally, the AUC was also evaluated using logistic regression models and a nonparametric approach [19]. The AUC does not measure risk concentration, which was evaluated with the proportion of cases followed (PCF), as the proportion of cases that would be followed in a program that followed the proportion q of the population at highest risk. The proportion q is the complementary measure, the proportion needed to follow-up (PNF) [17, 18]. Given PNF and the PRS distributions (F, G):
Finally, we used an approach similar to that described previously for the Gail model [20] to estimate the absolute risk of breast cancer according to percentile of the PRS. Specifically, we predicted the probability of developing breast cancer between ages α and α + τ for a woman who is in PRS percentile j as:
where subscript 1 refers to the incidence of breast cancer and subscript 2 refers to all other causes of death. In Eq. (6), h 1(t) is the baseline hazard rate of developing breast cancer at age t in the reference group, h 1(t) = h *(t)(1 – PAR), where PAR is the population attributable risk (PAR) related to the PRS and the theoretical prediction of the OR j for individuals in the PRS interval j between two percentiles (u, v) versus the 40th–60th percentiles:
and h *(t) is the age-specific breast cancer incidence rate in a composite population, in urban Shanghai during 2002 and 2003 [21] or in Korean women in the Korean risk assessment model for breast cancer risk prediction [22]; and h 2 (t) is the mortality rate at age t from all causes of death, except breast cancer, in the population, estimated using age-specific nonbreast cancer mortality in Shanghai in 2002 and 2003 [21] or in Korean women [22].
Results
The association between the 88 selected SNPs at the 78 genetic loci and breast cancer risk in East Asian women are presented in Additional file 2: Table S2, Additional file 3: Table S3, and Additional file 4: Table S4. Of those 78 loci, we observed 44 independent genetic loci that were significantly associated with breast cancer risk at P < 0.05 (one-sided, Additional file 2: Table S2, Additional file 3: Table S3, and Additional file 4: Table S4). We did not observe significant heterogeneity (data not shown) of the association across participating studies. No significant association with breast cancer risk was observed for the other 34 loci.
The PRS was derived based on the effect (β) and the number of risk alleles of a SNP carried by a woman. Some loci had multiple SNPs. In three of these loci (near C6orf97, ZNF365, and ANKLE1 genes), the most significant SNPs in Asian women (rs2046210, rs10822013, and rs2363956) were different from the most significant SNPs in European women (rs3757318, rs10995190, and rs8170). Only the SNP with the most significant association with breast cancer risk in each locus was selected for the PRS. The PRS for Asian women therefore included 44 SNPs.
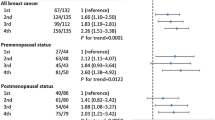
Under the multiplicative polygenic model, we observed a standard deviation (SD) of 0.38 for the PRS distribution in East Asian women (Eq. (3)). The theoretically predicted ORs from Eq. (4) and the observed ORs from logistic regression models for different percentiles of the PRS were compared with women in the 40th–60th percentiles (Table 1). The predicted and the observed estimates for ORs were similar, which provides support for the multiplicative polygenic model. Compared with Asian women in the middle quintile, for Asian women in the highest 1% of the PRS the theoretically predicted OR was 2.77 and the observed OR was 2.70 (95% CI: 2.15–3.40); for Asian women in the lowest 1% of the PRS, the theoretically predicted OR was 0.37 and the observed OR was 0.39 (95% CI: 0.27–0.57). The OR for the increment per decile of PRS was 1.13.
As mentioned earlier, the PCF measures the proportion of cases (p) which are included in the proportion q of individuals in the population at highest risk, while PNF assesses the proportion of the general population at highest risk (q) that one needs to follow in order that a proportion p of those destined to become cases will be followed. Given the SD of 0.38 for the PRS distribution, we estimated that approximately 2.6% of breast cancer cases in the general population would be found among those who were in the top 1% of PRS (PCF = 2.6% when PNF = 1%) (Table 2 and Fig. 1). In other words, to detect 80% of cases, 67.8% of the population needs to be screened (PNF = 67.8% when PCF = 80%). Given SD = 0.38, we estimated the AUC = 0.606, which is similar to the value of 0.602 estimated from logistic models using the data for 5152 Chinese women from the SGWAS. Figure 1 shows the AUC, which is also the area under a plot of PCF versus PNF as the risk threshold varies [18]. Based on the logistic models, the improvement in the AUC for the 44-SNP PRS to the breast cancer prediction model was 0.0386 (Table 1). This is greater than the AUC improvement (0.0328) for all of the traditional breast cancer risk factors combined from the same data (results not shown).
An estimate of 30% of the heritability of breast cancer, the total variability of propensity for breast cancer explained by genetic factors, was reported [23, 24], which corresponds to SD = 0.55 for the genetic variation. We present the AUC, PCF, and PNF for SD = 0.55 in Table 2 for comparison purposes. We estimated the AUC = 0.652 when SD = 0.55.
The absolute risk estimates for Shanghai Chinese and Korean women were compared (Table 3). Using the predicted OR estimates in Eq. (7), the estimated PAR (Eq. (8)) for breast cancer is 6.8% for the 44-SNP PRS. According to this PRS value, and using Eq. (6) and the age-specific breast cancer incidence and age-specific nonbreast cancer mortality for women in Shanghai in 2002 and 2003 [21] or in Korean women [22], the lifetime risk (age 20–80) of developing breast cancer by age 80 for the lowest 1% of the PRS was 1.35% for Chinese women in Shanghai and 1.31% for Korean women. The estimated risk for the highest 1% of the PRS was 10.06% for Chinese women and 9.81% for Korean women. For a 50-year-old woman with an average PRS value (40th–60th percentiles), the projected 10-year absolute risk of breast cancer is 1.03% for Chinese women and 1.05% for Korean women.
As reported previously [13], we observed significant heterogeneity (P < 0.05) of the SNP–breast cancer association by breast cancer estrogen receptor (ER) status in multiple loci (Additional file 3: Table S3 and Additional file 4: Table S4). As a whole, for the PRS distribution under the multiplicative polygenic model (Eq. (3)), we observed an SD of the PRS of 0.39 for ER-positive breast cancer and 0.38 for ER-negative breast cancer.
Finally, we evaluated the interaction between the PRS and age and pairwise multiplicative SNP by SNP interaction; no significant results were observed.
Discussion
In this study, we demonstrated the value of using common breast cancer variants, summarized as a 44-SNP PRS, to discriminate the breast cancer risk for women of East Asian ancestry. Compared with the recent report for women of European ancestry [15], we found that the PRS of common genetic variants had a smaller discriminative ability to identify high breast cancer risk in Asian women. The SD of the PRS distribution was 0.45 in European women, while the SD in this report among East Asian women is 0.38. There were 34 breast cancer loci identified previously in populations of European ancestry that were not associated with breast cancer risk in Asian women. In addition, previous studies found that the association of the PRS with ER-positive breast cancer was substantially stronger than the association with ER-negative breast cancer in women of European ancestry [25]. Mavaddat et al. [15] observed a striking difference in the SD of the PRS distribution by ER status (SD of 0.50 for ER-positive breast cancer and 0.38 for ER-negative breast cancer) in women of European ancestry. By comparison, a much less striking difference in the SD of the PRS distribution by ER status was observed (SD of 0.39 for ER-positive breast cancer and 0.38 for ER-negative breast cancer) in women of Asian ancestry (Additional file 3: Table S3 and Additional file 4: Table S4).
We reported previously the contribution of a genetic risk score derived from eight breast cancer-related SNPs in the prediction of breast cancer risk [21]. The 44-SNP PRS had greater discriminative ability than the eight-SNP PRS reported previously [21]. The AUC improvement of 0.0386 and SD = 0.38 for the 44-SNP PRS were substantially greater than the AUC improvement of 0.0117 and SD = 0.21 for the previous eight-SNP PRS. Previously we estimated that 37.7% of breast cancer cases in the general population would be found among women in the top 30% of the eight-SNP PRS values. Based on the 44-SNP PRS, we would expect to find 44.3% of breast cancer cases among those women, a moderate improvement for targeting women with a high risk of breast cancer for screening. If all genetic effects, estimated according to 30% of heritability of breast cancer [23, 24], were taken into account, we would find 51% of breast cancer cases among women in the top 30% of genetic risk (Table 2).
A limitation of this study is that this analysis included original studies that identified several new genetic variants among women of Asian ancestry [8–12], which raised an overfitting concern for the prediction model. If those SNPs were excluded from the PRS, then the SD of the PRS would be slightly decreased to 0.37 from 0.38, and the AUC would be slightly decreased to 0.603 from 0.606. On the contrary, it can be anticipated that the discriminative ability of breast cancer risk prediction based on genetic factors will further increase as more studies are conducted and more genetic variants, common or rare, are identified in East Asian women. In this report, there were several loci whose association with breast cancer risk in Asian women were not significant but were within the 95% CI of the association for European populations (Additional file 2: Tables S2). If those loci were included in the PRS, then the SD of the PRS would be slightly increased to 0.39 from 0.38, and the AUC would be slightly increased to 0.609 from 0.606. However, even when all genetic factors are taken into account (AUC = 0.652), the improvement in discrimination quality would still not be sufficient to be considered meaningful for clinical application. In order to increase discriminatory accuracy, other strong predictors, such as mammographic density and biopsy features, need to be included.
Conclusions
We have shown that known common genetic variants are important predictors for breast cancer risk, and using a 44-SNP PRS could help discriminate breast cancer risk in women of East Asian ancestry, although the discriminatory ability is not sufficient for clinical application.
Abbreviations
- AUC:
-
Area under the receiver operating characteristic curve
- BCAC:
-
Breast Cancer Association Consortium
- CI:
-
Confidence interval
- COGS:
-
Collaborative Oncological Gene–environment Study
- ER:
-
Estrogen receptor
- GWAS:
-
Genome-wide association study
- OR:
-
Odds ratio
- PAR:
-
Population attributable risk
- PCF:
-
Proportion of cases followed
- PNF:
-
Proportion needed to follow-up
- PRS:
-
Polygenic risk score
- QC:
-
Quality control
- SBCS:
-
Shanghai Breast Cancer Study
- SBCSS:
-
Shanghai Breast Cancer Survival Study
- SD:
-
Standard deviation
- SGWAS:
-
Shanghai Genome-wide Association Studies
- SNP:
-
Single nucleotide polymorphism
- SWHS:
-
Shanghai Women’s Health Study
References
Ghoussaini M, Pharoah PD, Easton DF. Inherited genetic susceptibility to breast cancer: the beginning of the end or the end of the beginning? Am J Pathol. 2013;183(1525–2191 (Electronic)):1038–51.
Stacey SN, Manolescu A, Sulem P, Rafnar T, Gudmundsson J, Gudjonsson SA, et al. Common variants on chromosomes 2q35 and 16q12 confer susceptibility to estrogen receptor-positive breast cancer. Nat Genet. 2007;39(7):865–9.
Thomas G, Jacobs KB, Kraft P, Yeager M, Wacholder S, Cox DG, et al. A multistage genome-wide association study in breast cancer identifies two new risk alleles at 1p11.2 and 14q24.1 (RAD51L1). Nat Genet. 2009;41(5):579–84.
Turnbull C, Ahmed S, Morrison J, Pernet D, Renwick A, Maranian M, et al. Genome-wide association study identifies five new breast cancer susceptibility loci. Nat Genet. 2010;42(6):504–7.
Michailidou K, Hall P, Gonzalez-Neira A, Ghoussaini M, Dennis J, Milne RL, et al. Large-scale genotyping identifies 41 new loci associated with breast cancer risk. Nat Genet. 2013;45(1546–1718 (Electronic)):353–61.
Michailidou K, Beesley J, Lindstrom S, Canisius S, Dennis J, Lush MJ, et al. Genome-wide association analysis of more than 120,000 individuals identifies 15 new susceptibility loci for breast cancer. Nat Genet. 2015;47(4):373–80.
Zheng W, Long J, Gao YT, Li C, Zheng Y, Xiang YB, et al. Genome-wide association study identifies a new breast cancer susceptibility locus at 6q25.1. Nat Genet. 2009;41(1546–1718 (Electronic)):324–8.
Long J, Cai Q, Shu XO, Qu S, Li C, Zheng Y, et al. Identification of a functional genetic variant at 16q12.1 for breast cancer risk: results from the Asia Breast Cancer Consortium. PLoS Genet. 2010;6(1553–7404 (Electronic)):e1001002.
Cai Q, Long J, Lu W, Qu S, Wen W, Kang D, et al. Genome-wide association study identifies breast cancer risk variant at 10q21.2: results from the Asia Breast Cancer Consortium. Hum Mol Genet. 2011;20(1460–2083 (Electronic)):4991–9.
Long J, Cai Q, Sung H, Shi J, Zhang B, Choi JY, et al. Genome-wide association study in east Asians identifies novel susceptibility loci for breast cancer. PLoS Genet. 2012;8(1553–7404 (Electronic)):e1002532.
Cai Q, Zhang B, Sung H, Low SK, Kweon SS, Lu W, et al. Genome-wide association analysis in East Asians identifies breast cancer susceptibility loci at 1q32.1, 5q14.3 and 15q26.1. Nat Genet. 2014;46(1546–1718 (Electronic)):886–90.
Long J, Delahanty RJ, Li G, Gao YT, Lu W, Cai Q, et al. A common deletion in the APOBEC3 genes and breast cancer risk. J Natl Cancer Inst. 2013;105(8):573–9.
Zheng W, Zhang B, Cai Q, Sung H, Michailidou K, Shi J, et al. Common genetic determinants of breast-cancer risk in East Asian women: a collaborative study of 23 637 breast cancer cases and 25 579 controls. Hum Mol Genet. 2013;22(1460–2083 (Electronic)):2539–50.
Lee CP, Irwanto A, Salim A, Yuan JM, Liu J, Koh WP, et al. Breast cancer risk assessment using genetic variants and risk factors in a Singapore Chinese population. Breast Cancer Res. 2014;16(1465-542X (Electronic)):R64.
Mavaddat N, Pharoah P, Michailidou K. Prediction of breast cancer risk based on profiling with common genetic variants. J Natl Cancer Inst. 2015;107(5):djv036.
Pharoah PD, Antoniou A, Bobrow M, Zimmern RL, Easton DF, Ponder BA. Polygenic susceptibility to breast cancer and implications for prevention. Nat Genet. 2002;31(1061–4036 (Print)):33–6.
Pfeiffer RM, Gail MH. Two criteria for evaluating risk prediction models. Biometrics. 2011;67(3):1057–65.
Gail MH. Personalized estimates of breast cancer risk in clinical practice and public health. Stat Med. 2011;30(10):1090–104.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44(3):837–45.
Gail MH, Brinton LA, Byar DP, Corle DK, Green SB, Schairer C, et al. Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst. 1989;81(0027–8874 (Print)):1879–86.
Zheng W, Wen W, Gao YT, Shyr Y, Zheng Y, Long J, et al. Genetic and clinical predictors for breast cancer risk assessment and stratification among Chinese women. J Natl Cancer Inst. 2010;102(1460–2105 (Electronic)):972–81.
Park B, Ma SH, Shin A, Chang MC, Choi JY, Kim S, et al. Korean risk assessment model for breast cancer risk prediction. PLoS One. 2013;8(10):e76736.
Collins A, Politopoulos I. The genetics of breast cancer: risk factors for disease. Appl Clin Genet. 2011;4:11–9.
Locatelli I, Lichtenstein P, Yashin AI. The heritability of breast cancer: a Bayesian correlated frailty model applied to Swedish twins data. Twin Res Off J Int Soc Twin Stud. 2004;7(2):182–91.
Husing A, Canzian F, Beckmann L, Garcia-Closas M, Diver WR, Thun MJ, et al. Prediction of breast cancer risk by genetic risk factors, overall and by hormone receptor status. J Med Genet. 2012;49(1468–6244 (Electronic)):601–8.
Acknowledgements
The ACP wishes to thank the participants in the Thai Breast Cancer study. Special thanks also go to the Thai Ministry of Public Health (MOPH), and doctors and nurses who helped with the data collection process. Finally, the study would like to thank Dr Prat Boonyawongviroj, the former Permanent Secretary of MOPH, and Dr Pornthep Siriwanarungsan, the Department Director-General of Disease Control, who have supported the study throughout. The BCAC thanks all individuals who took part in these studies and all of the researchers, clinicians, technicians, and administrative staff who have enabled this work to be carried out. This study would not have been possible without the contributions of the following: Per Hall (COGS); Douglas F. Easton, Paul Pharoah, Kyriaki Michailidou, Manjeet K. Bolla, and Qin Wang (BCAC); Andrew Berchuck (OCAC); Rosalind A. Eeles, Douglas F. Easton, Ali Amin Al Olama, Zsofia Kote-Jarai, and Sara Benlloch (PRACTICAL); Georgia Chenevix-Trench, Antonis Antoniou, Lesley McGuffog, Fergus Couch, and Ken Offit (CIMBA); Joe Dennis, Alison M. Dunning, Andrew Lee, and Ed Dicks; Craig Luccarini and the staff of the Centre for Genetic Epidemiology Laboratory; Javier Benitez, Anna Gonzalez-Neira and the staff of the CNIO genotyping unit; Jacques Simard, Daniel C. Tessier, Francois Bacot, Daniel Vincent, Sylvie LaBoissière and Frederic Robidoux and the staff of the McGill University and Génome Québec Innovation Centre; Stig E. Bojesen, Sune F. Nielsen, Borge G. Nordestgaard and the staff of the Copenhagen DNA laboratory; and Julie M. Cunningham, Sharon A. Windebank, Christopher A. Hilker, Jeffrey Meyer and the staff of Mayo Clinic Genotyping Core Facility. The HERPACC appreciates all of the study participants in the HERPACC study. The authors also thank the support from the Biobank at Aichi Cancer Center. The LAABC thanks all of the study participants and the entire data collection team, especially Annie Fung and June Yashiki. The MYBRCA thanks Phuah Sze Yee, Peter Kang, Kang In Nee, Kavitta Sivanandan, Shivaani Mariapun, Yoon Sook-Yee, Daphne Lee, Teh Yew Ching, and Nur Aishah Mohd Taib for DNA Extraction and patient recruitment. The SBCGS, SGWAS, SGWAS_stage2, SEBCS, TBCS, and TWBCS thank the study participants and research staff for their contributions and commitment to this project. The SGBCS thanks the participants and research coordinator Kimberley Chua.
Funding
The work conducted for this project at Vanderbilt University (SBCGS, SGWAS, SGWAS_stage2) was supported in part by US National Institutes of Health grants (R01CA124558, R01CA148667, R37CA070867, R01CA118229, R01CA092585, R01CA064277, R01CA122756, R01CA137013), US Department of Defense Idea Awards (BC011118, BC050791), and Ingram Professorship and Research Reward funds. The BCAC was funded by Cancer Research UK (C1287/A10118, C1287/A12014) and by the European Community’s Seventh Framework Programme under grant agreement number 223175 (grant number HEALTH-F2-2009-223175) (COGS). Funding for the iCOGS infrastructure came from: the European Community's Seventh Framework Programme under grant agreement n° 223175 (HEALTH-F2-2009-223175) (COGS), Cancer Research UK (C1287/A10118, C1287/A 10710, C12292/A11174, C1281/A12014, C5047/A8384, C5047/A15007, C5047/A10692, C8197/A16565), the National Institutes of Health (CA128978) and Post-Cancer GWAS initiative (1U19 CA148537, 1U19 CA148065, 1U19 CA148112—the GAME-ON initiative), the Department of Defence (W81XWH-10-1-0341), the Canadian Institutes of Health Research (CIHR) for the CIHR Team in Familial Risks of Breast Cancer, Komen Foundation for the Cure, the Breast Cancer Research Foundation, and the Ovarian Cancer Research Fund. The ACP study was funded by the Breast Cancer Research Trust, UK. The HERPACC was supported by a Grant-in-Aid for Scientific Research on Priority Areas from the Ministry of Education, Science, Sports, Culture and Technology of Japan, by the Practical Research for Innovative Cancer Control (15ck0106177h0001) from Japan Agency for Medical Research and development (AMED), by a Grant-in-Aid for the Third Term Comprehensive 10-Year Strategy for Cancer Control from Ministry Health, Labour and Welfare of Japan, by Health and Labour Sciences Research Grants for Research on Applying Health Technology from Ministry Health, Labour and Welfare of Japan, and National Cancer Center Research and Development Fund. The LAABC was supported by grants (1RB-0287, 3 PB-0102, 5 PB-0018, 10 PB-0098) from the California Breast Cancer Research Program. Incident breast cancer cases were collected by the USC Cancer Surveillance Program (CSP) which is supported under subcontract by the California Department of Health. The CSP is also part of the National Cancer Institute's Division of Cancer Prevention and Control Surveillance, Epidemiology, and End Results Program, under contract number N01CN25403. The MYBRCA was funded by research grants from the Malaysian Ministry of Science, Technology and Innovation (MOSTI), Malaysian Ministry of Higher Education (UM.C/HlR/MOHE/06), and Cancer Research Initiatives Foundation (CARIF). Additional controls were recruited by the Singapore Eye Research Institute, which was supported by a grant from the Biomedical Research Council (BMRC08/1/35/19/550), Singapore and the National Medical Research Council, Singapore (NMRC/CG/SERI/2010). The SEBCS was supported by the BRL (Basic Research Laboratory) program through the National Research Foundation of Korea funded by the Ministry of Education, Science and Technology (2012–0000347). The SGBCS was funded by the NUS start-up Grant, the National University Cancer Institute Singapore (NCIS) Centre Grant, and the NMRC Clinician Scientist Award. Additional controls were recruited by the Singapore Consortium of Cohort Studies-Multi-ethnic cohort (SCCS-MEC), which was funded by the Biomedical Research Council (grant number: 05/1/21/19/425). The TBCS was funded by The National Cancer Institute Thailand. The TWBCS was supported by the Taiwan Biobank project of the Institute of Biomedical Sciences, Academia Sinica, Taiwan. No funder had a role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article (and its Additional file 1: Table S1, Additional file 2: Table S2, Additional file 3: Table S3, Additional file 4: Table S4, and Additional file 5: Table S5.
Authors’ contributions
WW conducted the statistical analysis and wrote the manuscript. WZ conceived and directed the study. DFE led the BCAC and COGS. KM, MKB, QW, JD, and PDPP contributed significantly to the BCAC and COGS. All authors contributed to collection of the data and biological samples in the original studies, and data preparation for collaboration in BCAC. All authors reviewed the manuscript and approved its submission for publication. WZ had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
All participating studies obtained written, informed consent from all subjects and approval from their respective Institutional Review Boards (Additional file 5: Table S5).
Author information
Authors and Affiliations
Corresponding author
Additional files
Additional file 1:
is Table S1 presenting participating studies in this analysis. (PDF 79 kb)
Additional file 2:
is Table S2 presenting the association between selected SNPs and breast cancer risk in East Asian women. (PDF 146 kb)
Additional file 3:
is Table S3 presenting the association between selected SNPs and ER-positive breast cancer risk in East Asian women. (PDF 134 kb)
Additional file 4:
is Table S4 presenting the association between selected SNPs and ER-negative breast cancer risk in East Asian women. (PDF 137 kb)
Additional file 5:
is Table S5 presenting ethics committees that approved participating studies. (PDF 59 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Wen, W., Shu, Xo., Guo, X. et al. Prediction of breast cancer risk based on common genetic variants in women of East Asian ancestry. Breast Cancer Res 18, 124 (2016). https://doi.org/10.1186/s13058-016-0786-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13058-016-0786-1