Abstract
Background
Extracorporeal cardiopulmonary resuscitation (ECPR) may reduce mortality and improve neurological outcomes in patients with cardiac arrest. We updated our existing meta-analysis and trial sequential analysis to further evaluate ECPR compared to conventional CPR (CCPR).
Methods
We searched three international databases from 1 January 2000 through 1 November 2023, for randomised controlled trials or propensity score matched studies (PSMs) comparing ECPR to CCPR in both out-of-hospital cardiac arrest (OHCA) and in-hospital cardiac arrest (IHCA). We conducted an updated random-effects meta-analysis, with the primary outcome being in-hospital mortality. Secondary outcomes included short- and long-term favourable neurological outcome and survival (30 days–1 year). We also conducted a trial sequential analysis to evaluate the required information size in the meta-analysis to detect a clinically relevant reduction in mortality.
Results
We included 13 studies with 14 pairwise comparisons (6336 ECPR and 7712 CCPR) in our updated meta-analysis. ECPR was associated with greater precision in reducing overall in-hospital mortality (OR 0.63, 95% CI 0.50–0.79, high certainty), to which the trial sequential analysis was concordant. The addition of recent studies revealed a newly significant decrease in mortality in OHCA (OR 0.62, 95% CI 0.45–0.84). Re-analysis of relevant secondary outcomes reaffirmed our initial findings of favourable short-term neurological outcomes and survival up to 30 days. Estimates for long-term neurological outcome and 90-day–1-year survival remained unchanged.
Conclusions
We found that ECPR reduces in-hospital mortality, improves neurological outcome, and 30-day survival. We additionally found a newly significant benefit in OHCA, suggesting that ECPR may be considered in both IHCA and OHCA.
Similar content being viewed by others
Introduction
Despite advances in research, prognosis following cardiac arrest remains grim [1, 2]. Extracorporeal cardiopulmonary resuscitation (ECPR) in refractory cardiac arrest can potentially be considered, yet the utility of ECPR in out-of-hospital cardiac arrest (OHCA) remains to be seen, with three randomised controlled trials (RCTs) reporting differing outcomes [3,4,5,6]. Our group recently conducted a systematic review and meta-analysis of randomised clinical trials (RCTs) and propensity score matched studies on ECPR in cardiac arrest [7]. While we found a reduction in mortality with ECPR for in-hospital cardiac arrest (IHCA), we did not observe this same finding in OHCA, although this latter conclusion may have been impacted by ongoing imprecision. We concluded that more studies were needed assessing the role of ECPR, specifically in OHCA.
The publication of a new propensity score matched study by Okada et al. [8] evaluating ECPR in over 2000 patients with OHCA is a timely addition to the literature, along with a similar study by Choi et al. [9]. We believe that the publication of these new studies stands to enhance our understanding of this topic. As the evidence has expanded, we updated the systematic review and meta-analysis based on our previous study to evaluate the ECPR among OHCA patients.
Methods
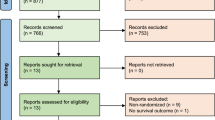
The original protocol was registered with PROSPERO (CRD42022332623). We adhered to the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) statement (Additional file 1: PRISMA Checklist) [10], and the prespecified methodology and analytical plan from our original meta-analysis. Briefly, we updated our literature search and screened the literature through 1 November 2023. We followed the prior inclusion criteria of either RCTs or propensity score matched studies comparing ECPR against conventional cardiopulmonary resuscitation (CCPR) in cardiac arrest. We did a random-effects meta-analyses (Mantel–Haenszel method) of binary outcomes using the DerSimonian–Laird model [11, 12] and present outcomes as pooled odds ratios (OR) with 95% confidence intervals (CIs). We adhered to the Grading of Recommendations, Assessment, Development, and Evaluations approach when assessing the certainty of evidence [13]. We assessed risk of bias via the Cochrane Risk of Bias 2 Tool for RCTs and Newcastle Ottawa Score for PSMs.
The primary outcome was in-hospital mortality. We also re-analysed relevant secondary outcomes where reported by any of the newly included studies. These were favourable short-term (discharge to 30 days) neurological outcome (defined by a cerebral performance category (CPC) score of 1–2), as well as post-discharge survival of 30 days. We repeated the prespecified subgroup analyses and the trial sequential analysis.
Further details on the original methodology, along with their references, can be found in Additional file 1: Original Methods and References for Original Methods. As both shockable and non-shockable cohorts in Okada et al. [8] were matched separately, we have included these cohorts separately in this updated analysis. We used p-values of less than 0.05 as the threshold for statistical significance. We did all meta-analyses analyses using R (version 4.0.5) and trial sequential analyses using TSA v0.9.5.10 (www.ctu.dk/tsa).
Results
Updated primary outcomes
We updated our search until 1 November 2023, including 13 studies (three RCTs and 10 PSMs) with 14 pairwise comparisons comprising 14,048 patients (6336 ECPR and 7712 CCPR, references in Additional file 1: PRISMA Flowchart and References for Included Studies). Study characteristics for individual studies are noted in Table 1. All RCTs were noted to be either at ‘low risk’ or ‘some concerns’ for bias, while all PSMs were noted to be of ‘high quality’ (Additional file 1: Table S1a and S1b). ECPR was associated with lower mortality (OR 0.63, 95% CI 0.50–0.79), with high certainty based on GRADE (Additional file 1: Table S2). Due to concerns regarding possible overlaps in Korean OHCA data [14], we conducted sensitivity analysis excluding Choi et al. [9]; the pooled estimate did not substantially change.
Subgroup analysis examining mortality based on type of study, geographical region, location of arrest (OHCA vs in-hospital cardiac arrest [IHCA]), and study quality did not demonstrate significant differences (pinteraction > 0.05 for all subgroup comparisons). As compared to the previous analysis, the overall findings were very similar. However, for patients with OHCA, while ECPR previously had no association with mortality reduction, the updated analysis, including these two new studies, now demonstrated a reduction in mortality with ECPR (OR 0.67, 95% CI 0.51–0.88, Fig. 1). Trial sequential analysis for mortality found that the cumulative Z-curve passed the required information size and TSA-adjusted boundary for benefit affirmed our results.
Updated secondary outcomes
Updated analysis of relevant secondary outcomes found that ECPR was associated with favourable neurological outcomes at short-term follow-up (OR 1.57, 95% CI 1.14–2.15, high certainty) and survival up to 30 days (OR 1.70, 95% CI 1.29–2.26, high certainty), for which trial sequential analyses demonstrated that required information size was met, and TSA-adjusted boundaries were consistent. These findings were both similar to what we had previously demonstrated.
Additional file 1: Table S3 summarises these updated findings for all updated analyses, including subgroup analysis. While reported in our previously published meta-analysis, there were no new data evaluating long-term (3 months, 6 months, and 1 year) survival and long-term neurological outcomes in the newly included studies. As such, these outcomes were not updated and presented in this paper. These outcomes can be found in the initial report [7]. We have also indicated the result of post hoc sensitivity analysis in Additional file 1: Table S4.
Discussion
The most pertinent change in findings from this updated analysis were improvements in mortality when using ECPR for patients with OHCA, which represents a change from our previously published results [7]. This change in findings is likely a result of improvements in precision achieved with including additional studies and therefore larger number of patients and events.
Although both new studies had large sample sizes, it was Okada et al. [8] which included both shockable and non-shockable cohorts that primarily led to improvements in precision and generalisability of results, and an improved estimate in the OHCA cohort. The other new study, Choi et al. [9], did not see any significant differences in mortality with ECPR, with results being imprecise.
In our previously published report, we discussed differing conclusions between the three RCTs examining this topic and proposed that varying times to cannulation between these studies might explain their differing results, with the RCT having the shortest time to cannulation having the greatest benefit seen in ECPR. We posit that this same variable may also explain the shift in these updated results, particularly with reference to the inclusion of Okada et al. [8]. Okada and colleagues were able to achieve extremely fast time to ECPR cannulation, with a median time of under 30 min in both shockable and non-shockable cohorts, which corroborates with the findings from our prior meta-regression that mortality increases with low-flow time (HR [hazard ratio] per min: 1.01, 95% CI 1.00–1.01). In Japan, ECPR is often initiated at the emergency department, without the need to involve inpatient services, unlike in other regions [21]. This would result in faster cannulation than if the patient had to be transported to the operating theatre or other procedural rooms in order to achieve cannulation. This decrease in low-flow time likely reduces multiorgan failure and brain injury after cardiac arrest, thereby augmenting the survival benefits of ECPR [3, 22].
These studies supplement our prior analysis, with the addition of additional OHCA cohorts now demonstrating the benefit of ECPR in both OHCA and IHCA. Nevertheless, factors such as the preparedness of pre-hospital ECMO programmes and the speed at which ECMO cannulation is achieved affect outcomes, and it remains a highly labour- and resource-intense intervention. ECPR can only be as effective as the team that is providing it, with effectiveness likely only seen in high-volume centres able to achieve expeditious cannulation.
This study has limitations that should be considered. Importantly, residual confounding remains an issue in PSMs, with factors outside the propensity model not accounted for and potentially confounding the analysis. Furthermore, there are no clear, unified eligibility criteria for ECPR. Each study in this meta-analysis reported variable selection criteria, which necessitates a cautious interpretation of the results. Furthermore, it is noted that among the RCTs included in this analysis, two were terminated early and did not reach the pre-defined sample size [5, 6], one had a number of post-randomisation exclusions [4], and others had protocolised features that may have impacted maintenance of blinding [4, 5]. Also, there is some variability in our risk of bias assessments and those of previously published systematic reviews, and while we are confident in our assessments (Additional file 1: Table S1a and S1b), this highlights the subjectivity that can be associated with these ratings [25]. Additionally, we used mortality as the primary outcome, which although patient important, does not provide information related to quality of life. This was prespecified in our protocol, and based on the fact that we thought more of the included studies would report on this endpoint, that being said, we have included survival with favourable neurological outcome as a secondary outcome in the analysis.
Conclusion
In conclusion, we found that ECPR was associated with significant reductions in mortality for patients with cardiac arrest, with a significant reduction in patients with OHCA upon addition of new studies. Compared with CCPR, ECPR also improves short-term neurological outcomes and 30-day survival, affirming our prior analysis.
Availability of data and materials
All data generated or analysed in this study were extracted from published studies and their supplementary information files.
References
Peberdy MA, Kaye W, Ornato JP, Larkin GL, Nadkarni V, Mancini ME, Berg RA, Nichol G, Lane-Trultt T. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National registry of cardiopulmonary resuscitation. Resuscitation. 2003;58(3):297–308.
Yan S, Gan Y, Jiang N, Wang R, Chen Y, Luo Z, Zong Q, Chen S, Lv C. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit Care. 2020;24(1):61.
Twohig CJ, Singer B, Grier G, Finney SJ. A systematic literature review and meta-analysis of the effectiveness of extracorporeal-CPR versus conventional-CPR for adult patients in cardiac arrest. J Intensiv Care Soc. 2019;20(4):347–57.
Suverein MM, Delnoij TSR, Lorusso R, Brandon Bravo Bruinsma GJ, Otterspoor L, Elzo Kraemer CV, Vlaar APJ, van der Heijden JJ, Scholten E, den Uil C, et al. Early extracorporeal CPR for refractory out-of-hospital cardiac arrest. N Engl J Med. 2023;388(4):299–309.
Yannopoulos D, Bartos J, Raveendran G, Walser E, Connett J, Murray TA, Collins G, Zhang L, Kalra R, Kosmopoulos M, et al. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open-label, randomised controlled trial. Lancet. 2020;396(10265):1807–16.
Belohlavek J, Smalcova J, Rob D, Franek O, Smid O, Pokorna M, Horák J, Mrazek V, Kovarnik T, Zemanek D, et al. Effect of intra-arrest transport, extracorporeal cardiopulmonary resuscitation, and immediate invasive assessment and treatment on functional neurologic outcome in refractory out-of-hospital cardiac arrest: a randomized clinical trial. JAMA. 2022;327(8):737–47.
Low CJW, Ramanathan K, Ling RR, Ho MJC, Chen Y, Lorusso R, MacLaren G, Shekar K, Brodie D. Extracorporeal cardiopulmonary resuscitation versus conventional cardiopulmonary resuscitation in adults with cardiac arrest: a comparative meta-analysis and trial sequential analysis. Lancet Respir Med. 2023;11(10):883–93.
Okada Y, Komukai S, Irisawa T, Yamada T, Yoshiya K, Park C, Nishimura T, Ishibe T, Kobata H, Kiguchi T, et al. In-hospital extracorporeal cardiopulmonary resuscitation for patients with out-of-hospital cardiac arrest: an analysis by time-dependent propensity score matching using a nationwide database in Japan. Crit Care. 2023;27(1):442.
Choi Y, Park JH, Jeong J, Kim YJ, Song KJ, Shin SD. Extracorporeal cardiopulmonary resuscitation for adult out-of-hospital cardiac arrest patients: time-dependent propensity score-sequential matching analysis from a nationwide population-based registry. Crit Care. 2023;27(1):87.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22(4):153–60.
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, DeBeer H, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–94.
Kim SJ, Han KS, Lee EJ, Lee SJ, Lee JS, Lee SW. Association between extracorporeal membrane oxygenation (ECMO) and mortality in the patients with cardiac arrest: a nation-wide population-based study with propensity score matched analysis. J Clin Med. 2020;9(11):3703.
Blumenstein J, Leick J, Liebetrau C, Kempfert J, Gaede L, Groß S, Krug M, Berkowitsch A, Nef H, Rolf A, et al. Extracorporeal life support in cardiovascular patients with observed refractory in-hospital cardiac arrest is associated with favourable short and long-term outcomes: A propensity-matched analysis. Euro Heart J Acute Cardiovas Care. 2016;5(7):13–22.
Chen Y-S, Lin J-W, Yu H-Y, Ko W-J, Jerng J-S, Chang W-T, Chen W-J, Huang S-C, Chi N-H, Wang C-H. Cardiopulmonary resuscitation with assisted extracorporeal life-support versus conventional cardiopulmonary resuscitation in adults with in-hospital cardiac arrest: an observational study and propensity analysis. Lancet. 2008;372(9638):554–61.
Daun JG, Tak LJ, Eun P, Hansol C, Taerim KW, Chul C, Hee YS, Yeon HT, Gun SM, Sub S, IkJoon J, Seung-Hwa LS, Do S, Jin-Ho C. Extracorporeal Life-support for Out-of-hospital Cardiac Arrest: A Nationwide Multicenter Study. Shock. 2022;57(5):680–6.
Lin JW, Wang MJ, Yu HY, Wang CH, Chang WT, Jerng JS, Huang SC, Chou NK, Chi NH, Ko WJ, et al. Comparing the survival between extracorporeal rescue and conventional resuscitation in adult in-hospital cardiac arrests: propensity analysis of three-year data. Resuscitation. 2010;81(7):796–803.
Maekawa K, Tanno K, Hase M, Mori K, Asai Y. Extracorporeal cardiopulmonary resuscitation for patients with out-of-hospital cardiac arrest of cardiac origin. Critical Care Med. 2013;41(5):1186–96.
Patricio D, Peluso L, Brasseur A, Lheureux O, Belliato M, Vincent J-L, Creteur J, Taccone FS. Comparison of extracorporeal and conventional cardiopulmonary resuscitation: a retrospective propensity score matched study. Critical Care. 2019;23(1).
Inoue A, Hifumi T, Sakamoto T, Okamoto H, Kunikata J, Yokoi H, Sawano H, Egawa Y, Kato S, Sugiyama K, et al. Extracorporeal cardiopulmonary resuscitation in adult patients with out-of-hospital cardiac arrest: a retrospective large cohort multicenter study in Japan. Crit Care. 2022;26(1):129.
Sandroni C, Cronberg T, Sekhon M. Brain injury after cardiac arrest: pathophysiology, treatment, and prognosis. Intensiv Care Med. 2021;47(12):1393–414.
Shin TG, Choi J-H, Jo IJ, Sim MS, Song HG, Jeong YK, Song Y-B, Hahn J-Y, Choi SH, Gwon H-C, et al. Extracorporeal cardiopulmonary resuscitation in patients with inhospital cardiac arrest: a comparison with conventional cardiopulmonary resuscitation*. Crit Care Med. 2011;39(1):1–7.
Shin TG, Jo IJ, Sim MS, Song YB, Yang JH, Hahn JY, Choi SH, Gwon HC, Jeon ES, Sung K, et al. Two-year survival and neurological outcome of in-hospital cardiac arrest patients rescued by extracorporeal cardiopulmonary resuscitation. Int J Cardiol. 2013;168(4):3424–30.
Holmberg MJ, Granfeldt A, Guerguerian A-M, Sandroni C, Hsu CH, Gardner RM, et al. Extracorporeal cardiopulmonary resuscitation for cardiac arrest: An updated systematic review. Resuscitation. 2023;182:109665.
Acknowledgements
We thank Suei Nee Wong for her assistance with the search strategy, in both original and updated meta-analyses.
Funding
This study was supported by a scientific research grant from the JSPS KAKENHI (JP23K16253 to YO) and the ZOLL Foundation (YO).
Author information
Authors and Affiliations
Contributions
CJWL, RRL, and YO helped in conception and design of this study, CJWL and RRL helped in data acquisition, CJWL, RRL, YC, and BR helped in analysis, CJWL and RRL contributed to writing original draft, KR, TK, TI, MEHO, and YO helped in review and revision of the draft, and KR and YO worked in supervision. All authors have approved the final manuscript and have agreed both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones, in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
RRL acknowledges research support from the Clinician Scientist Development Unit, Yong Loo Lin School of Medicine, National University of Singapore. KR serves on the steering committee of the Extracorporeal Life Support Organisation. He is the current chair of the Publications Committee and is the past co-chair of the Scientific Oversight Committee. YO has received a research grant from the ZOLL Foundation and an overseas scholarship from the FUKUDA Foundation for Medical Technology and the International Medical Research Foundation. MEHO reports grants from the Laerdal Foundation, Laerdal Medical, and Ramsey Social Justice Foundation for funding of the Pan-Asian Resuscitation Outcomes Study an advisory relationship with Global Healthcare SG, a commercial entity that manufactures cooling devices; and funding from Laerdal Medical on an observation programme to their Community CPR Training Centre Research Program in Norway. MEHO is a Scientific Advisor to TIIM Healthcare SG and Global Healthcare SG. These organisations have no role in conducting this research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. PRISMA Checklist. Original Methods and References for Original Method. PRISMA Flowchart and References for Included Studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Low, C.J.W., Ling, R.R., Ramanathan, K. et al. Extracorporeal cardiopulmonary resuscitation versus conventional CPR in cardiac arrest: an updated meta-analysis and trial sequential analysis. Crit Care 28, 57 (2024). https://doi.org/10.1186/s13054-024-04830-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-024-04830-5