Abstract
Background
Management of bleeding trauma patients is still a difficult challenge. Massive transfusion (MT) requires resources to ensure the safety and timely delivery of blood products. Early prediction of MT need may be useful to shorten the time process of blood product preparation. The primary aim of this study was to assess the accuracy of shock index to predict the need for MT in adult patients with trauma. For the same population, we also assessed the accuracy of SI to predict mortality.
Methods
This systematic review and meta-analysis was performed in accordance with the PRISMA guidelines. We performed a systematic search on MEDLINE, Scopus, and Web of Science from inception to March 2022. Studies were included if they reported MT or mortality with SI recorded at arrival in the field or the emergency department. The risk of bias was assessed using the QUADAS-2.
Results
Thirty-five studies were included in the systematic review and meta-analysis, for a total of 670,728 patients. For MT the overall sensibility was 0.68 [0.57; 0.76], the overall specificity was 0.84 [0.79; 0.88] and the AUC was 0.85 [0.81; 0.88]. Positive and Negative Likelihood Ratio (LR+; LR−) were 4.24 [3.18–5.65] and 0.39 [0.29–0.52], respectively. For mortality the overall sensibility was 0.358 [0.238; 0.498] the overall specificity 0.742 [0.656; 0.813] and the AUC 0.553 (confidence region for sensitivity given specificity: [0.4014; 0.6759]; confidence region for specificity given sensitivity: [0.4799; 0.6332]). LR+ and LR− were 1.39 [1.36–1.42] and 0.87 [0.85–0.89], respectively.
Conclusions
Our study demonstrated that SI may have a limited role as the sole tool to predict the need for MT in adult trauma patients. SI is not accurate to predict mortality but may have a role to identify patients with a low risk of mortality.
Similar content being viewed by others
Background
Injuries are responsible for about 8% of all deaths worldwide [1]. Hemorrhage is often preventable death and early hemorrhage control pathway including time-critical transfusion is crucial to reduce this preventable mortality. The early recognition and management of bleeding patients is the major challenge because rapid intervention aiming to stop the bleeding is fundamental to reducing mortality and morbidity. Prediction of the need for a hemorrhage control pathway should be easy, quick and reliable to anticipate and mobilize resources. Massive transfusion (MT) requires resources to ensure the safety and timely delivery of blood products [2]. Early prediction of MT is useful to anticipate the process of blood product preparation [2]. Thus, MT protocols improve patients’ outcome and minimized blood product wastage [3, 4]. Several scores to predict MT have been proposed [5], but they may not be always simple to be calculated in the field. The Shock Index (SI) is a simple mathematical equation based on the ratio between heart rate (HR) and systolic blood pressure (SBP), it is easy to calculate in pre-hospital settings and those vital signs are frequently communicated to the trauma center directly from the scene. Normal values in adults range from 0.5 to 0.7. A hypovolemic shock classification based on this score has been proposed (SI < 0.6: no shock; SI 0.6–1: mild shock; SI 1–1.4: moderate shock; SI ≥ 1.4: severe shock) [6]. The current European guidelines on the management of major bleeding and coagulopathy following trauma suggest using SI to assess the severity of hypovolemic shock [7].
We performed a systematic review and meta-analysis to investigate the role of SI to predict the need for MT in adult trauma patients. The secondary aim was to assess the role of SI to predict mortality in patients with trauma.
Methods
Protocol and guidance for conducting and reporting
The Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) guidelines [8] have been followed to write the protocol while the methodology for conducting and reporting the systematic review was based on the Preferred Reporting Items for Systematic Reviews and Meta-analyses of diagnostic test accuracy studies (PRISMA-DTA) guidelines [9]. The protocol (Additional file 1) has been registered on International Prospective Register of Systematic Reviews (PROSPERO) (CRD42021270285).
Review questions and hypothesis
The primary review question was if SI could predict the need for MT in adult patients with trauma, while the secondary review question was if SI could predict the mortality of adult patients with trauma.
We hypothesized that SI was significantly higher in adult trauma patients that need MT and in those that did not survive to trauma.
Primary and secondary outcomes
The primary outcome of the study was to assess the accuracy of SI to detect the need for MT in adult patients with trauma.
The secondary outcome was to assess the accuracy of SI to detect mortality in adult patients with trauma.
Eligibility criteria
We considered patients with trauma, and ≥ 14 years old. No further exclusion criteria different from pediatric age (< 14 years) have been considered. We selected papers that reported pre-hospital and/or hospital SI and the need for MT. MT is classically defined as a transfusion of > 10 red blood cells (RBC) units in 24 h. However, because of MT definition is evolving [10], we did not restrict it to a specific definition, but we considered MT as defined by the single study. For the secondary outcome, mortality (as defined in the study) was recorded when available.
Randomized controlled trials and observational studies (prospective and retrospective) were included. Conference proceedings, abstracts, case reports, and studies not involving humans were excluded. No language restrictions were applied.
Studies with data from the field and the hospital are included.
Search strategy
We searched the Medline, Scopus, and Web of Science databases from their inception to September 2022. The search strategy can be found in the Additional file 1. Reference lists of eligible studies and review articles have been assessed. Before paper submission, the research was repeated (1 December 2022) to identify further papers published in the meantime, and the analysis was updated.
Study selection and data extraction
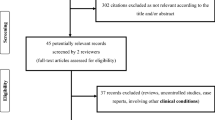
Two researchers (A.C. and R.A.) independently screened titles and abstracts of all papers resulting from the database search. Subsequently, they independently assessed the full text of the papers selected from titles and abstracts screening. The same investigators independently performed data extraction. Any discrepancies that arose during the selection process and data extraction were solved by consensus or by the decision of a third independent researcher (A.D.). CADIMA software vers. 2.2.3 (JKI—Julius Kühn-Institut) has been used for screening and papers assessment.
Assessment of risk of bias and quality of the evidence
Two trained investigators (A.C. and A.R.) independently rated the quality of the selected studies. As per the Cochrane DTA handbook [11], the quality assessment of diagnostic accuracy studies (QUADAS-2) tool was used to assess for risk of bias and applicability concerns in patients’ selection, index test, reference standard, and flow and timing. Each item was evaluated as low, unclear, or high risk of bias [12]. The highest risk of bias shown for any item was used to determine the overall risk of bias for the study. The overall quality of the evidence for the primary and secondary outcomes has been assessed according to Grading of Recommendations Assessment, Development and Evaluation (GRADE) guidelines [13, 14].
Statistical analysis
The statistical analysis has been performed using diagmeta package in R (R version 4.2.0 (2022-04-22)), and metandi and midas in STATA (StataCorp 2021; Stata Statistical Software: Release 17; StataCorp LLC). The bivariate model proposed by Reitsma et al. has been used to assess the accuracy of SI to predict MT and mortality and for summary receiver operating characteristic (SROC) curve calculation [15]. When appropriate, SROC will be drawn with confidence and prediction contour. They are both graphical representations that describe the uncertainty in the SROC estimate. The confidence contour describes the uncertainty in the SROC estimate and shows the 95% confidence interval for the SROC at a given point. The prediction contour, on the other hand, describes the uncertainty in predicting the SROC for future tests that might be performed. It shows a 95% prediction interval for the SROC, based on the distribution of SROCs estimated from different tests. This is useful for predicting future test performance and assessing the effect of any future tests. In case of multiple cut-offs for SI, the model of multiple thresholds proposed by Steinhuser has been used if appropriate [16]. This model is able to calculate the optimal cut-off.
Quantitative SROC analysis has been performed if five or more studies reported data for the primary/secondary outcome. In the presence of an appropriate number of studies, subgroup analysis considering pre-hospital SI (PH-SI) and SI recorded at hospital admission (H-SI) has been performed. Further subgroup analysis has been considered to investigate the potential sources of heterogeneity.
Results
Study selection and study characteristics
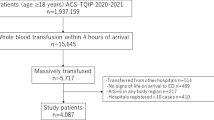
2652 titles were retrieved from the literature search. After removing duplicates (n = 463) and papers that focused on non-trauma patients (n = 325), we screened the titles/abstracts of 1864 records. 529 papers have been excluded because they examined outcomes other than MT and/or mortality. Of the remaining 1335 papers, 1246 considered different tests (such as Age Shock Index and Reverse Shock Index) and were also excluded. After assessing 89 studies for eligibility, we were unable to retrieve 54 of them because they focused on a pediatric population. Finally, 35 studies were included, considering 670,728 patients (Fig. 1). Studies were published from 1996 to 2022. The main characteristics of the selected studies are described in Additional file 1: Tables S1 and S2.
All studies considered patients ≥ 14 years old involved in trauma. Twenty-two studies considered H-SI [6, 17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37] while 10 studies considered PH-SI [38,39,40,41,42,43,44,45,46,47]. Three studies reported both PH- and H-SI [48,49,50]. Two studies involved the geriatric population [33, 35], while Montoya et al. [36] considered only patients younger than 50 years old. Seven studies excluded patients with traumatic brain injuries (TBI) [17, 21, 32, 33, 35, 37, 41]. Some variability was observed regarding the definition of MT and mortality. Almost all studies defined MT as 10 red blood cells (RBC units within 24 h [19, 21, 22, 28, 38, 40, 42, 44, 47, 51, 52] and mortality as in-hospital mortality [18, 22, 25,26,27,28,29, 31, 33,34,35, 38, 41]. Different definitions are a further source of potential heterogeneity.
Risk of bias and quality of evidence
The quality assessment of the studies is summarized in Figs. 2 and 3. Almost all studies clearly stated the age of the population. The overall quality of evidence was very low/low mainly due to the high heterogeneity between studies.
Primary outcome
Fifteen studies have been considered for quantitative analysis of SROC [18, 19, 21, 22, 28, 38, 40,41,42, 44,45,46,47,48, 50].
SI showed an overall sensibility of 0.68 [0.57; 0.76] and an overall specificity of 0.84 [0.79; 0.88] to predict MT. The AUC was 0.85 [0.81; 0.88] (Fig. 4). Positive and Negative Likelihood Ratio (LR+ ; LR−) were 4.24 [3.18–5.65] and 0.39 [0.29–0.52], respectively.
Considering PH-SI, the sensitivity was 0.67 [0.50; 0.81], the specificity was 0.83 [0.75; 0.89] and the AUC was 0.84 [0.81; 0.87] (Additional file 1: Figure S1). LR+ and LR− were 3.97 [2.52–6.25] and 0.40 [0.24–0.64], respectively.
Considering H-SI, the sensitivity was 0.771 [0.584; 0.890], the specificity was 0.775 [0.674; 0.852], and the AUC was 0.841 (confidence region for sensitivity given specificity: [0.4566; 0.9393]; confidence region for specificity given sensitivity: [0.7762; 0.9036]) (Additional file 1: Figure S2). LR+ and LR− were 3.43 [3.07–3.83] and 0.30 [0.27–0.34], respectively. We found an optimal cut-off value of 0.796 at hospital admission to discriminate between patients with low vs. high risk of MT.
The quality of the evidence table for SI to predict MT in adult patients with trauma is shown in Additional file 1: Table S3.
Secondary outcome
Twenty-six studies have been considered for secondary outcome [6, 17,18,19,20, 23, 24, 26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43, 49].
SI showed an overall sensibility of 0.358 [0.238; 0.498] and an overall specificity of 0.742 [0.656; 0.813] to predict mortality. The AUC was 0.553 (confidence region for sensitivity given specificity: [0.4014; 0.6759]; confidence region for specificity given sensitivity: [0.4799; 0.6332]) (Fig. 5). LR+ and LR− were 1.39 [1.36–1.42] and 0.87 [0.85–0.89], respectively. The optimal cut-off of SI to predict mortality was 0.804.
Considering pre-hospital data, the overall sensibility was 0.886 [0.064; 0.998] and the overall specificity was 0.389 [0.072; 0.837]. The AUC was 0.590 (confidence region for sensitivity given specificity: [0.0632; 0.7517]; confidence region for specificity given sensitivity: [0.3237; 0.8588]) (Additional file 1: Figure S3). LR+ and LR− were 1.45 [1.38–1.52] and 0.29 [0.28–0.3], respectively. The optimal cut-off of PH-SI to predict mortality was 0.569.
Considering hospital data, the overall sensitivity was 0.462 [0.349; 0.580] and the overall specificity was 0.780 [0.699; 0.855]. The AUC was 0.638 (confidence region for sensitivity given specificity: [0.5220; 0.7333]; confidence region for specificity given sensitivity: [0.5741; 0.7037]) (Additional file 1: Figure S4). LR+ and LR− were 2.1 [2–2.18] and 0.69 [0.66–0.72], respectively. The optimal cut-off of H-SI to predict mortality was 0.836.
To reduce the potential source of heterogeneity due to different timepoint for mortality definition, we performed a subgroup analysis considering 12 studies reporting hospital mortality [18, 26,27,28,29, 31, 33,34,35, 38, 41, 42], as this was the most frequently reported timepoint for mortality assessment. For an optimal cut-off of 0.795, SI showed a sensitivity of 0.325 [0.161; 0.547] and a specificity of 0.736 [0.600; 0.838] to predict hospital mortality. The AUC was 0.5315 (confidence region for sensitivity given specificity [0.2712; 0.7154]; confidence region for specificity given sensitivity: [0.4157; 0.6660]) (Additional file 1: Figure S5). LR+ and LR− were 1.23 [1.19–1.27] and 0.92 [0.89–0.95], respectively.
The quality of the evidence table for SI to predict mortality in adult patients with trauma is shown in Additional file 1: Table S4.
Discussion
Even if deaths following trauma and MT need are decreasing in the last years [53], management of massive hemorrhage is still a challenge in trauma patients. Transfusion protocols drawn up to overcome this problem improved survival [54, 55]. SI is probably one of the most useful indices that measure the severity of hypovolemia, especially when patients still present with systolic pressure in the normal range despite having suffered significant blood loss [56].
Our study showed that SI may have a role in trauma patients. It showed a high AUC of SROC curve for MT prediction. However, LR+ and LR− showed a weak ability of SI to detect whether patients needed MT or not, as a positive or negative SI reveal about 25% increased or reduced risk of MT, respectively. Both pre-hospital and hospital recordings may have approximately the same role. AUC is approximately the same for PH- and H-SI, with the PH-SI being less sensitive and more specific than H-SI. However, considering the confidence interval, this difference does not seem significant. The cut-off of 0.8 may be considered reasonable to discriminate a risk for MT.
SI values can vary in a range from 0 to infinity and increasing its value higher is the risk for transfusion. The values are therefore correlated with the degree of shock and impaired tissue perfusion [37, 57]. For this reason, SI is a better indicator of hemodynamic instability than HR or blood pressure considered individually [56]. Furthermore, an increase in SI indicates a higher probability of negative outcome and the need for more resources for treatment [49] such as surgery, mechanical ventilation, prolonged hospitalization in intensive care, and a longer hospital stay [52].
Olaussen et al. [2] support the usefulness of measuring the SI before arrival at the hospital because it could warn the physician, avoiding the preparation of unnecessary blood. According to Vandromme et al. [38], a patient who has a SI = 0.91 in the field has more than 1.5 times increased risk for receiving MT compared to a patient with normal SI, and for a SI = 1.14 in the pre-hospital setting the risk of MT is 5 times higher.
In addition to the SI, several scores would equally allow making these considerations, but the SI is the most easily accessible and calculable since it is obtained from only two parameters [38, 48]. Schroll et al. [21] have shown that SI > 1 has a greater sensitivity than the ABC score in predicting the need for MT even if it has a weaker specificity. Both Demuro et al. [58] and El-Menyar et al. [28] argue that SI > 0.8 is the better cut-off to predict the need for MT. The rationale for this choice is that it decreases the possibility of underestimating patients who may need urgent intervention during triage. However, cut-off = 1 is more specific and can be easily interpreted by pre-hospital staff since it is sufficient to consider the SBP numerically lower than the HR as a warning condition [2]. This facilitates the identification of high-risk patients without requiring other additional tools and SI > 1 could be useful criteria to suspect hemorrhagic shock [46, 48, 59,60,61]. The early activation of the MT protocol and its strict adherence has been shown to improve the outcome in the most serious patients and decrease the number of plasma transfusions [3]. A delay in the activation of the transfusion protocol (> 15 min from the patient's arrival) has been found in 50% of cases and it was the only cause of non-compliance with the protocol [62]. MT protocol activation based on information coming from the field could decrease delays and improve compliance.
The predictive strength of SI could be compromised in patients with chronic hypertension, diabetes mellitus, or coronary heart disease, conditions in which the dynamic response of pressure and HR—and therefore of SI—could differ from healthy patients and thus hinder its application in predicting MT [22]. Hypertension alters basal systolic blood pressure and drugs, such as beta-blockers or calcium channel blockers, limit tachycardia in response to hypovolemia [63]. Heart failure can also limit the physiological response to shock. Some authors suggest that both vital signs and SI are more difficult to interpret in the elderly because they tend to have a lower sympathetic system response in regulating HR and blood pressure. This leads to an increase in the false negative rate [32, 64, 65]. Thus, the usefulness of the SI may be limited in these subpopulations as they do not have substantial changes in HR in response to hemodynamic stress [66]. TBI has also been associated with an alteration in the autonomic response to bleeding with consequent uncoupling of the autonomic and cardiovascular systems [67, 68]. However, even if the accuracy of SI has been previously questioned by an experimental model of TBI and hemorrhage [69], a retrospective study based on a large database has confirmed the validity of SI to identify patients at risk of transfusion independently of the presence of an associated TBI [31].
Regarding the predictive capacity of SI on mortality, the selected studies have shown a low sensitivity and a higher specificity, indicating that a normal SI may be useful to identify patients with a low risk of mortality. On the other hand, an abnormal value may have limited significance. Bruijns et al. [32] analyzed the variation of some scores (SI, Age-SI, minpulse [MP], pulse max index [PMI], and blood pressure-age index [BPAI]) with mortality and they were able to show an association. Some scores consider the patient's age as a variable for calculation. Whatever the exact age, there is a broad agreement that the older the patient, the higher the probability of death, even if the patient has less severe injuries [70, 71]. A retrospective study considered 111,019 patients on beta blockers or calcium channel blockers, hypertension, diabetes and aged > 65 years to understand if these comorbidities weaken the ability of SI to predict mortality [72]. The authors have shown that patients > 65 years with SI > 1 had an increased risk of mortality at 30 days but elderly age, hypertension, and the use of beta-blockers or calcium antagonists weaken the correlation between SI and mortality [72]. Kim et al. [35] considering only an elderly population (age > 65 years), underline the utility of the Age-SI (SI multiplied by the age) to have a more precise relationship with mortality. In this case, values greater than 50 are indicative of hemodynamic instability. Pandit et al. [33] agree on the greater accuracy of the Age-SI but point out the greater difficulty in calculating this score which would make it less applicable in emergencies. Similarly, the Shock Index Pediatric Adjusted (SIPA) has been developed for the pediatric population and is more reliable for this subgroup of patients [73, 74]. The SI is the only score among those considered by Bruijns et al. [32] which has a relationship with mortality (sensitivity 0.37, specificity 0.95) without including age in its equation. According to El-Menyar et al. [28], as the SI values increase, regardless of the patient's condition, the prognosis will be worse. Higher values reflect a higher incidence of multi-organ dysfunction and sepsis, all factors affecting mortality [6, 28]. Moreover, an increase of SI > 0.3 between the pre-hospital and in-hospital recording is associated with increased mortality by 5 times [49]. Thus, considering the limitations of SI to predict mortality shown by our results, other scores should be considered. Trauma and injury severity score (TRISS) and the Revised Injury Severity Classification II (RISC II) are two more sophisticated tools specially designed for this purpose.
Recently, Need For Trauma Intervention (NFTI) has been proposed as an alternative measure to Injury Severity Score (ISS) and Revised Trauma Score (RTS) to better define major trauma [75, 76]. The NFTI criteria are: (1) receiving packed red blood within 4 h of arrival; (2) emergency department (ED) discharge to operating room within 90 min; (3) ED discharge to interventional radiology; (4) ED discharge to intensive care unit (ICU) with ICU length of stay ≥ 3 calendar days; (5) nonprocedural mechanical ventilation within 72 h of arrival; and (6) mortality within 60 h of arrival [75]. NFTI seems a better indicator of major trauma. Thus, the ability of SI to identify severe trauma could be also assessed considering this definition. Current literature is lacking about this.
The strength of our study is the high number of patients considered in the analysis. A previous systematic review has been conducted to investigate the role of SI to predict MT in trauma patients in 2014 [2]. Since that, other 26 studies have been considered. However, we are also aware of some limitations. Retrospective studies have been included in the analysis (only 1 prospective study) and this may be responsible for bias. Most of the included studies considered the classic definition of MT (> 10 RBC units/24 h). This is currently less and less frequent [53] and actually a sort of failure of an integrated hemorrhage control pathway. However, correlating SI with the quality of the hemorrhage control pathway is difficult, and the literature still widely considers MT as evidence of severe hemorrhagic shock. The definition of MT, however, is currently moving from the concept of the number of RBC transfused over a defined time interval to the time-critical character of transfusion management in bleeding trauma patients, which is not limited to RBC but considers early transfusion of any kind of blood product (fibrinogen, plasma, and platelets) [10].
Furthermore, considering the whole adult population, we faced different trauma mechanisms. Statistically, young people are more involved in penetrating traumas than the elderly. Some studies excluded patients with traumatic brain injuries as clinical parameters may be altered independently from hemorrhagic shock while other studies also included this subpopulation. It should also be specified that the elderly population may frequently present other comorbidities that can influence the outcome. For this reason, several authors propose adapting SI to age [35]. All these aspects may contribute to increasing heterogeneity and results should be interpreted with caution.
The records of all the studies considered do not contain information regarding any therapies made by the patient: beta-blockers and anti-hypertensive drugs, analgesics, drugs for the treatment of anxiety, and others that can affect the HR response to hemorrhage and alter other vital signs.
Regarding mortality, the main limitation of our study is represented by the heterogeneity of the different studies in reporting this outcome. There is no uniformity as regards the time in which the patient's mortality was recorded (hospital mortality, at 24 h, 48 h, or 28 days).
Conclusions
Our study demonstrates that SI may have a weak role to detect the risk for MT in adult trauma patients. On the other hand, regarding mortality, SI may be useful only to identify patients with a low risk of mortality, as for its low sensitivity and high specificity. However, the low/very low quality of evidence due to the retrospective design of the included studies and some sources of heterogeneity does not allow to recommend SI as the sole parameter to consider in predicting MT and mortality in trauma patients. The role of SI adjusted for age for special populations (pediatric and elderly) needs to be further assessed.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AgeSI:
-
Age shock index
- AUC:
-
Area under the curve
- BPAI:
-
Blood pressure-age index
- ED:
-
Emergency department
- GRADE:
-
Grading of Recommendations Assessment, Development and Evaluation
- HR:
-
Heart rate
- H-SI:
-
Hospital shock index
- ICU:
-
Intensive care unit
- ISS:
-
Injury Severity Score
- LR+:
-
Positive likelihood ratio
- LR−:
-
Negative likelihood ratio
- MP:
-
Minpulse
- MT:
-
Massive blood transfusion
- NFTI:
-
Need For Trauma Intervention
- PH-SI:
-
Pre-hospital shock index
- PMI:
-
Pulse max index
- PRISMA-DTA:
-
Preferred Reporting Items for Systematic Reviews and Meta-analyses of diagnostic test accuracy studies
- PRISMA-P:
-
Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols
- QUADAS-2:
-
Quality assessment of diagnostic accuracy studies
- RBC:
-
Red blood cells
- RISC II:
-
Revised injury severity classification II
- RTS:
-
Revised Trauma Score
- SBP:
-
Systolic blood pressure
- SI:
-
Shock index
- SIPA:
-
Shock index pediatric adjusted
- SROC:
-
Summary receiver operating characteristic
- TBI:
-
Traumatic brain injury
- TRISS:
-
Trauma and injury severity score
References
World Health Organization. Injuries and violence [Internet]. 2021 [cited 2023 Feb 11]. Available from: https://www.who.int/news-room/fact-sheets/detail/injuries-and-violence
Olaussen A, Blackburn T, Mitra B, Fitzgerald M. Review article: shock index for prediction of critical bleeding post-trauma: a systematic review. Emerg Med Australas. 2014;26:223–8.
Vogt KN, Van Koughnett JA, Dubois L, Gray DK, Parry NG. The use of trauma transfusion pathways for blood component transfusion in the civilian population: a systematic review and meta-analysis. Transfus Med. 2012;22:156–66.
Holcomb JB, Del Junco DJ, Fox EE, Wade CE, Cohen MJ, Schreiber MA, et al. The prospective, observational, multicenter, major trauma transfusion (PROMMTT) study: comparative effectiveness of a time-varying treatment with competing risks. JAMA Surg. 2013;148:127–36.
Burman S, Cotton BA. Trauma patients at risk for massive transfusion: the role of scoring systems and the impact of early identification on patient outcomes. Expert Rev Hematol. 2012;5:211–8.
Mutschler M, Nienaber U, Münzberg M, Wölfl C, Schoechl H, Paffrath T, et al. The Shock Index revisited - a fast guide to transfusion requirement? A retrospective analysis on 21,853 patients derived from the TraumaRegister DGU®. Crit Care. 2013;17:R172.
Spahn D, Bouillon B, Cerny V, Duranteau J, Filipescu D, Hunt B, et al. The European guideline on management of major bleeding and coagulopathy following trauma: fifth edition. Crit Care. 2019;23:98.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350: g7647.
Salameh JP, Bossuyt PM, McGrath TA, Thombs BD, Hyde CJ, MacAskill P, et al. Preferred reporting items for systematic review and meta-analysis of diagnostic test accuracy studies (PRISMA-DTA): explanation, elaboration, and checklist. BMJ. 2020;370: m2632.
Gauss T, Moyer JD, Bouzat P. Massive transfusion in trauma: an evolving paradigm. Minerva Anestesiol. 2022;88:184–91.
Reitsma JB, Rutjes AWS, Whiting P, Vlassov VV, Leeflang MMG, Deeks JJ. Chapter 9: assessing methodological quality. In: Deeks JJ, Bossuyt PM, Gatsonis C, editors. Cochrane handbook for systematic reviews of diagnostic test accuracy version 1.0.0. London: The Cochrane Collaboration; 2009.
Whiting PF, Rutjes AWS, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. Quadas-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529–36.
Schünemann HJ, Mustafa RA, Brozek J, Steingart KR, Leeflang M, Murad MH, et al. GRADE guidelines: 21 part 1. Study design, risk of bias, and indirectness in rating the certainty across a body of evidence for test accuracy. J Clin Epidemiol. 2020;122:129–41.
Schünemann HJ, Mustafa RA, Brozek J, Steingart KR, Leeflang M, Murad MH, et al. GRADE guidelines: 21 part 2. Test accuracy: inconsistency, imprecision, publication bias, and other domains for rating the certainty of evidence and presenting it in evidence profiles and summary of findings tables. J Clin Epidemiol. 2020;122:142–52.
Reitsma JB, Glas AS, Rutjes AWS, Scholten RJPM, Bossuyt PM, Zwinderman AH. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol. 2005;58:982–90.
Steinhauser S, Schumacher M, Rücker G. Modelling multiple thresholds in meta-analysis of diagnostic test accuracy studies. BMC Med Res Methodol. 2016;16:97.
Zarzaur BL, Croce MA, Fischer PE, Magnotti LJ, Fabian TC. New vitals after injury: shock index for the young and age × shock index for the old. J Surg Res. 2008;147:229–36.
El-Menyar A, Jabbour G, Asim M, Abdelrahman H, Mahmood I, Al-Thani H. Shock index in patients with traumatic solid organ injury as a predictor of massive blood transfusion protocol activation. Inj Epidemiol. 2019;6:41.
Marenco CW, Lammers DT, Morte KR, Bingham JR, Martin MJ, Eckert MJ. Shock index as a predictor of massive transfusion and emergent surgery on the modern battlefield. J Surg Res. 2020;256:112–8.
Jouini S, Jebali A, Hedhli H, Kaddour RB, Mrabet A, Hebaieb F. Predictive value of shock index ≥ 1 in severe trauma patients in emergency. Tunis Med. 2019;97:802–7.
Schroll R, Swift D, Tatum D, Couch S, Heaney JB, Llado-Farrulla M, et al. Accuracy of shock index versus ABC score to predict need for massive transfusion in trauma patients. Injury. 2018;49:15–9.
Rau CS, Wu SC, Kuo SCH, Kuo PJ, Hsu SY, Chen YC, et al. Prediction of massive transfusion in trauma patients with shock index, modified shock index, and age shock index. Int J Environ Res Public Health. 2016;13:683.
Bhandarkar P, Munivenkatappa A, Roy N, Kumar V, Moscote-Salazar LR, Agrawal A. Pattern and distribution of shock index and age shock index score among trauma patients in towards improved trauma care outcomes (TITCO) dataset. Bull Emerg Trauma. 2018;6:313–7.
Ono Y, Yokoyama H, Matsumoto A, Kumada Y, Shinohara K, Tase C. Is preoperative period associated with severity and unexpected death of injured patients needing emergency trauma surgery? J Anesth. 2014;28:381–9.
Torabi M, Mirafzal A, Rastegari A, Sadeghkhani N. Association of triage time shock index, modified shock index, and age shock index with mortality in emergency severity index level 2 patients. Am J Emerg Med. 2016;34:63–8.
Asim M, El-Menyar A, Chughtai T, Al-Hassani A, Abdelrahman H, Rizoli S, et al. Shock index for the prediction of interventions and mortality in patients with blunt thoracic trauma. J Surg Res. 2023;283:438–48.
Kakimoto K, Shibahashi K, Oishio M, Sugiyama K, Hamabe Y. Mortality of hospital walk-in trauma patients: a multicenter retrospective cohort study. Acute Med Surg. 2022;9: e784.
El-Menyar A, Goyal P, Tilley E, Latifi R. The clinical utility of shock index to predict the need for blood transfusion and outcomes in trauma. J Surg Res. 2018;227:52–9.
Chowdhury S, Parameaswari P, Leenen L. Outcomes of trauma patients present to the emergency department with a Shock Index of ≥1.0. J Emerg Trauma Shock. 2022;15:17–22.
Turan E, Şahin A. Role of glucose/potassium ratio and shock index in predicting mortality in patients with isolated thoracoabdominal blunt trauma. Ulus Travma Acil Cerrahi Derg. 2022;28:1442–8.
Fröhlich M, Driessen A, Böhmer A, Nienaber U, Igressa A, Probst C, et al. Is the shock index based classification of hypovolemic shock applicable in multiple injured patients with severe traumatic brain injury?-an analysis of the TraumaRegister DGU®. Scand J Trauma Resusc Emerg Med. 2016;24:148.
Bruijns SR, Guly HR, Bouamra O, Lecky F, Lee WA. The value of traditional vital signs, shock index, and age-based markers in predicting trauma mortality. J Trauma Acute Care Surg. 2013;74:1432–7.
Pandit V, Rhee P, Hashmi A, Kulvatunyou N, Tang A, Khalil M, et al. Shock index predicts mortality in geriatric trauma patients: an analysis of the National Trauma Data Bank. J Trauma Acute Care Surg. 2014;76:1111–5.
Wu SC, Rau CS, Kuo SCH, Chien PC, Hsieh HY, Hsieh CH. The reverse shock index multiplied by glasgow coma scale score (Rsig) and prediction of mortality outcome in adult trauma patients: a cross-sectional analysis based on registered trauma data. Int J Environ Res Public Health. 2018;15:2346.
Kim SY, Hong KJ, Do Shin S, Ro YS, Ahn KO, Kim YJ, et al. Validation of the shock index, modified shock index, and age shock index for predicting mortality of geriatric trauma patients in emergency departments. J Korean Med Sci. 2016;31:2026–32.
Montoya KF, Charry JD, Calle-Toro JS, Núñez LR, Poveda G. Shock index as a mortality predictor in patients with acute polytrauma. J Acute Dis. 2015;4:202–4.
King RW, Plewa MC, Buderer NMF, Knotts FB. Shock index as a marker for significant injury in trauma patients. Acad Emerg Med. 1996;3:1041–5.
Vandromme MJ, Griffin RL, Kerby JD, McGwin G, Rue LW, Weinberg JA. Identifying risk for massive transfusion in the relatively normotensive patient: Utility of the prehospital shock index. J Trauma. 2011;70:384–90.
Yang S, Hu PF, Anazodo A, Gao C, Chen H, Wade C, et al. Trends of hemoglobin oximetry: do they help predict blood transfusion during trauma patient resuscitation? Anesth Analg. 2016;122:115–25.
Wang IJ, Bae BK, Park SW, Cho YM, Lee DS, Min MK, et al. Pre-hospital modified shock index for prediction of massive transfusion and mortality in trauma patients. Am J Emerg Med. 2019;38:187–90.
Kim DK, Jeong J, Do Shin S, Song KJ, Hong KJ, Ro YS, et al. Association between prehospital field to emergency department delta shock index and in-hospital mortality in patients with torso and extremity trauma: a multinational, observational study. PLoS ONE. 2021;16:e0258811.
Jehan F, Con J, McIntyre M, Khan M, Azim A, Prabhakaran K, et al. Pre-hospital shock index correlates with transfusion, resource utilization and mortality; The role of patient first vitals. Am J Surg. 2019;218:1169–74.
Kheirbek T, Martin TJ, Cao J, Hall BM, Lueckel S, Adams CA. Prehospital shock index outperforms hypotension alone in predicting significant injury in trauma patients. Trauma Surg Acute Care Open. 2021;6: e000712.
Pottecher J, Ageron FX, Fauché C, Chemla D, Noll E, Duranteau J, et al. Prehospital shock index and pulse pressure/heart rate ratio to predict massive transfusion after severe trauma: retrospective analysis of a large regional trauma database. J Trauma Acute Care Surg. 2016;81:713–22.
Meyer DE, Vincent LE, Fox EE, O’Keeffe T, Inaba K, Bulger E, et al. Every minute counts: time to delivery of initial massive transfusion cooler and its impact on mortality. J Trauma Acute Care Surg. 2017;83:19–24.
Mitra B, Fitzgerald M, Chan J. The utility of a shock index ≥ 1 as an indication for pre-hospital oxygen carrier administration in major trauma. Injury. 2014;45:61–5.
Zhu CS, Cobb D, Jonas RB, Pokorny D, Rani M, Cotner-Pouncy T, et al. Shock index and pulse pressure as triggers for massive transfusion. J Trauma Acute Care Surg. 2019;87:S159–64.
Olaussen A, Peterson EL, Mitra B, O’Reilly G, Jennings PA, Fitzgerald M. Massive transfusion prediction with inclusion of the pre-hospital Shock Index. Injury. 2015;46:822–6.
Cannon CM, Braxton CC, Kling-Smith M, Mahnken JD, Carlton E, Moncure M. Utility of the shock index in predicting mortality in traumatically injured patients. J Trauma. 2009;67:1426–30.
Figueiredo S, Taconet C, Harrois A, Hamada S, Gauss T, Raux M, et al. How useful are hemoglobin concentration and its variations to predict significant hemorrhage in the early phase of trauma? A multicentric cohort study. Ann Intensive Care. 2018;8:76.
David JS, Voiglio EJ, Cesareo E, Vassal O, Decullier E, Gueugniaud PY, et al. Prehospital parameters can help to predict coagulopathy and massive transfusion in trauma patients. Vox Sang. 2017;112:557–66.
McNab A, Burns B, Bhullar I, Chesire D, Kerwin A. A prehospital shock index for trauma correlates with measures of hospital resource use and mortality. Surgery. 2012;152:473–6.
Cole E, Weaver A, Gall L, West A, Nevin D, Tallach R, et al. A decade of damage control resuscitation: new transfusion practice, new survivors. New Directions Ann Surg. 2021;273:1215–20.
Malone DL, Hess JR, Fingerhut A. Massive transfusion practices around the globe and a suggestion for a common massive transfusion protocol. J Trauma. 2006;60:S91–6.
Cotton BA, Gunter OL, Isbell J, Au BK, Robertson AM, Morris JA, et al. Damage control hematology: the impact of a trauma exsanguination protocol on survival and blood product utilization. J Trauma. 2008;64:1177–82.
Birkhahn RH, Gaeta TJ, Terry D, Bove JJ, Tloczkowski J. Shock index in diagnosing early acute hypovolemia. Am J Emerg Med. 2005;23:323–6.
Rady MY, Nightingale P, Little RA, Edwards JD. Shock index: a re-evaluation in acute circulatory failure. Resuscitation. 1992;23:227–34.
Demuro JP, Simmons S, Jax J, Gianelli SM. Application of the shock index to the prediction of need for hemostasis intervention. Am J Emerg Med. 2013;31:1260–3.
Chuang J-F, Rau C-S, Wu S-C, Liu H-T, Hsu S-Y, Hsieh H-Y, et al. Use of the reverse shock index for identifying high-risk patients in a five-level triage system. Scand J Trauma Resusc Emerg Med. 2016;24:12.
Lai W-H, Wu S-C, Rau C-S, Kuo P-J, Hsu S-Y, Chen Y-C, et al. Systolic blood pressure lower than heart rate upon arrival at and departure from the emergency department indicates a poor outcome for adult trauma patients. Int J Environ Res Public Health. 2016;13:528.
Lai W-H, Rau C-S, Hsu S-Y, Wu S-C, Kuo P-J, Hsieh H-Y, et al. Using the reverse shock index at the injury scene and in the emergency department to identify high-risk patients: a cross-sectional retrospective study. Int J Environ Res Public Health. 2016;13:357.
Bawazeer M, Ahmed N, Izadi H, McFarlan A, Nathens A, Pavenski K. Compliance with a massive transfusion protocol (MTP) impacts patient outcome. Injury. 2015;46:21–8.
McNab A, Burns B, Bhullar I, Chesire D, Kerwin A. An analysis of shock index as a correlate for outcomes in trauma by age group. Surgery. 2013;154:384–7.
Foëx BA. Systemic responses to trauma. Br Med Bull. 1999;55:726–43.
Kannel WB. Blood pressure as a cardiovascular risk factor: Prevention and treatment. J Am Med Assoc. 1996;275:1571–6.
Koch E, Lovett S, Nghiem T, Riggs R, Rech MA. Shock index in the emergency department: utility and limitations. Open Access Emerg Med. 2019;11:179–99.
Goldstein B, Toweill D, Lai S, Sonnenthal K, Kimberly B. Uncoupling of the autonomic and cardiovascular systems in acute brain injury. Am J Physiol. 1998;275:R1287–92.
McMahon CG, Kenny R, Bennett K, Kirkman E. Modification of acute cardiovascular homeostatic responses to hemorrhage following mild to moderate traumatic brain injury. Crit Care Med. 2008;36:216–24.
McMahon CG, Kenny R, Bennett K, Little R, Kirkman E. The effect of acute traumatic brain injury on the performance of shock index. J Trauma. 2010;69:1169–75.
Caterino JM, Valasek T, Werman HA. Identification of an age cutoff for increased mortality in patients with elderly trauma. Am J Emerg Med. 2010;28:151–8.
Clement ND, Tennant C, Muwanga C. Polytrauma in the elderly: predictors of the cause and time of death. Scand J Trauma Resusc Emerg Med. 2010;18:26.
Kristensen AKB, Holler JG, Hallas J, Lassen A, Shapiro NI. is shock index a valid predictor of mortality in emergency department patients with hypertension, diabetes, high age, or receipt of β- or calcium channel blockers? Ann Emerg Med. 2016;67:106-113.e6.
Linnaus ME, Notrica DM, Langlais CS, St. Peter SD, Leys CM, Ostlie DJ, et al. Prospective validation of the shock index pediatric-adjusted (SIPA) in blunt liver and spleen trauma: an ATOMAC + study. J Pediatr Surg. 2017;52:340–4.
Acker SN, Ross JT, Partrick DA, Tong S, Bensard DD. Pediatric specific shock index accurately identifies severely injured children. J Pediatr Surg. 2015;50:331–4.
Roden-Foreman JW, Rapier NR, Yelverton L, Foreman ML. Asking a better question: development and evaluation of the need for trauma intervention (NFTI) metric as a novel indicator of major trauma. J Trauma Nurs. 2017;24:150–7.
Roden-Foreman JW, Rapier NR, Foreman ML, Zagel AL, Sexton KW, Beck WC, et al. Rethinking the definition of major trauma: the need for trauma intervention outperforms Injury Severity Score and Revised Trauma Score in 38 adult and pediatric trauma centers. J Trauma Acute Care Surg. 2019;87:658–65.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
AC has conceived the paper, drew the protocol, selected the studies, revised the analysis and the manuscript; RC has performed literature search, selected the studies, performed the analysis, and draft the manuscript; EC has contributed to the analysis of results; ED has substantially contributed to manuscript revision; FG has substantially contributed to manuscript revision; BM has substantially contributed to manuscript revision; EA has substantially contributed to manuscript revision; AD has contributed to studies selection and substantially contributed to manuscript revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Study protocol, supplemental tables and figures.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Carsetti, A., Antolini, R., Casarotta, E. et al. Shock index as predictor of massive transfusion and mortality in patients with trauma: a systematic review and meta-analysis. Crit Care 27, 85 (2023). https://doi.org/10.1186/s13054-023-04386-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-023-04386-w