Abstract
The obesity paradox has been observed in short-term outcomes from critical illness. However, little is known regarding the impact of obesity on long-term outcomes for survivors of critically ill patients. We aimed to evaluate the influence of obesity on long-term mortality outcomes after discharge alive from ICU. The adult patients who were discharged alive from the last ICU admission were extracted. After exclusion, a total of 7619 adult patients discharged alive from ICU were included, with 4-year mortality of 32%. The median body mass index (BMI) was 27.2 (IQR 24–31.4) kg/m2, and 2490 (31.5%) patients were classified as obese or morbidly obese. The morbidly obese patients had the highest ICU and hospital length of stay. However, higher BMI was associated with lower hazard ratio for 4-year mortality. The results showed the obesity paradox may be also suitable for survivors of critically ill patients.
Similar content being viewed by others
Background
Survivors of critically ill patients are at risk of experiencing significant physical, cognitive, and mental health issues, which were associated with an increased mortality following discharge from intensive care unit (ICU) [1,2,3,4]. However, factors associated with mortality for survivors of critical illness are not well understood, which may be important when counseling patients and families.
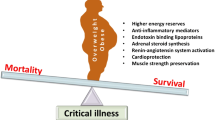
The obesity paradox, which is the phenomenon that obesity increases the risk of obesity-related diseases but paradoxically is associated with survival benefits, has been observed in short-term outcomes from critical illness [5,6,7]. Nonetheless, little is known regarding the impact of obesity on long-term outcomes after discharge from intensive care unit (ICU).
We, therefore, aimed to evaluate the influence of obesity on 4-year mortality outcome for survivors of critically illness.
Methods
Data were extracted from the online database Medical Information Mart for Intensive Care (MIMIC III) [8]. We included adult patients who were discharged alive from the last ICU admission. The exclusion criteria were: (1) No weight and height data available, (2) body mass index (BMI) < 10 kg/m2 or > 70 kg/m2, (3) No follow-up survival data available.
We abstracted the height and weight data from the Electronic Medical Records (EMR) when admitted to ICU. The BMI was calculated using the equation: BMI (kg/m2) = weight (kg)/height2 (m2). BMI was examined as both a categorical and continuous variable. According to the international standards [9], obesity was assessed as a categorical variable according to BMI (BMI less than 10.0 or greater than 70.0 kg/m2 was excluded): underweight, BMI < 18.5 k kg/m2; normal weight, 18.5 ≤ BMI < 25 kg/m2; overweight, 25 ≤ BMI < 30 kg/m2; obese, 30 ≤ BMI < 40 kg/m2; morbidly obese, BMI ≥ 40 kg/m2.
The primary endpoint was 4-year mortality which was extracted from the social security database and was considered as a time-to-event variable.
Baseline and clinical characteristics were compared among different BMI categories. Multiple imputation was used to deal with the missing data with the mice package [10]. We used Cox proportional hazards regression model to produce adjusted hazard ratios (HRs) for the association between BMI and 4-year mortality with normal weight as reference. To better understand the effect of BMI on 4-year mortality as a continuous covariate in multivariable Cox model, the splines-based HR curve was expressed with smoothHR package [11]. The PostgreSQL (version 10, www.postgresql.org) was used for data extraction, and R software (version 3.5.1, www.r-project.org) was used to conduct all the statistical analysis.
Results
After exclusion, 7619 adult patients discharged alive from ICU were included, with 4-year mortality of 32% (Table 1). The median BMI was 27.2 (IQR 24–31.4) kg/m2. 2490 (31.5%) patients were classified as obese or morbidly obese. As expected, higher BMI patients had a higher percentage of comorbidities of hypertension and diabetes mellitus. The morbidly obese patients had the highest ICU and hospital length of stay. The underweight patients had the highest 4-year mortality (62%). The higher BMI was associated with lower HR for 4-year mortality.
Underweight and normal-weight patients had a lower probability of 4-year survival (Fig. 1B). When considering normal-weight patients as the reference, underweight patients had higher adjusted HR for mortality, while overweight and obese patients had lower adjusted HRs (Fig. 1C). When using BMI as a continuous variable, the pointwise estimation of the adjusted HR curve showed a nonlinear relationship between BMI and long-term mortality outcome, with a BMI of 28.9 kg/m2 the lowest HR (Fig. 1D).
A Histogram and density distribution of body mass index (BMI); B Kaplan–Meier survival curves by BMI category (log-rank p < 0.001); C Adjusted hazards ratio (HR) for 4-year mortality according to BMI categories, with normal weight as reference. The HRs and 95% confidence intervals (error bars) for each categories were calculated using COX proportional hazard model after adjusting for age, sex, ethnicity, marital status, insurance type, comorbidities (hypertension, diabetes mellitus, tumor, respiratory disease, chronic heart failure, liver disease, and renal failure), ICU type, disease severity score of simplified acute physiology score (SAPS) II, and hospital discharge locations; D Smoothed HR (log transformation) curve with pointwise nonparametric estimation of association between BMI and 4-year mortality after adjusting for confounders (same with the confounders in C)
Discussion
In the present study, a significant proportion of patients discharging from ICU survive less than 4 years. Among survivors of critical illness, obesity was associated with lower 4-year mortality.
The high mortality of survivors discharging from ICU was in line with previous studies [12, 13]. In the study of Brinkman et al. [12], the mortality risk at 3 years after hospital discharge was 27.5%; and the 5 years mortality was 26.9% in the study of Doherty et.al, which was higher than the general age-matched population [13]. In view of the prevalence of obesity continuing to rise among the ICU population [6], efforts to understand the impact of obesity long-term outcomes after critical illness should also be important [14]. The present study showed the mortality was high for ICU survivors and obesity was associated with reduced mortality; However, the underlying mechanisms were unknown. Several pathophysiologic mechanisms including higher energy reserves, anti-inflammatory immune profile, role of adipose tissue, and prevention of muscle wasting may contribute to explain this phenomenon [5]. Interestingly, according to the recent study of Drago et al. [15], the relationship of increasing BMI and lower risk of hypoglycemia might contribute to decreased mortality.
The concept of obesity paradox has also been challenged. Martino et.al found that extreme obesity was not associated with a worse survival advantage after adjusted for confounders as well as had a longer duration of mechanical ventilation and ICU length of stay [16]. On the other hand, the BMI as a composite variable is intrinsically problematic, which is not an appropriate measure of fat and skeletal muscle mass and its distribution [17]. In the studies of Jaitovich et al. [18, 19], ICU admission pectoralis muscle area or erector spinae muscle mass was associated with survival outcomes, not was the subcutaneous adipose tissue mass. Similar studies were sparse for ICU survivors. As for survivors of critically ill patients, it is unclear whether it reflects a protective effect or limitations inherent to observational research for obesity paradox, which warrants further research.
There were several limitations to our study. First, the retrospective design in nature was subjected to the inherent limitations even though adjusted for potential confounders. The other confounding factors including smoking status, alcohol consumption, income, education, physical activity, and dietary pattern may be involved, which were not extracted from the database. Second, the ICU admission height and weight data were extracted from the EMR with a higher missing rate. The method (estimation or measurement) for recording the height and weight was unknown. Third, the weight was a variable parameter relying on fluid balance, which could cause perturbation for calculation of BMI. As a result of these limitations, the present findings warrant a cautious interpretation, and more prospective cohort studies are needed to further elucidate this phenomenon.
Conclusions
In conclusion, our results suggest that the obesity paradox may be also suitable for survivors of critically ill patients.
Availability of data and materials
Data analyzed during the present study are currently stored in the Medical Information Mart for Intensive Care (MIMIC III) (mimic.mit.edu).
Abbreviations
- BMI:
-
Body mass index
- EMR:
-
Electronic medical records
- HR:
-
Hazard ratio
- ICU:
-
Intensive care unit
- MIMIC:
-
Medical Information Mart for Intensive Care
References
Hatch R, Young D, Barber V, Griffiths J, Harrison DA, Watkinson P. Anxiety, depression and post traumatic stress disorder after critical illness: a UK-wide prospective cohort study. Crit Care. 2018;22(1):310.
de Lima V, Bierrenbach AL, Alencar GP, Andrade AL, Azevedo LCP. Increased risk of death and readmission after hospital discharge of critically ill patients in a developing country: a retrospective multicenter cohort study. Intensive Care Med. 2018;44(7):1090–6.
Wilcox ME, Girard TD, Hough CL. Delirium and long term cognition in critically ill patients. BMJ. 2021;373:n1007.
Hashem MD, Nallagangula A, Nalamalapu S, Nunna K, Nausran U, Robinson KA, Dinglas VD, Needham DM, Eakin MN. Patient outcomes after critical illness: a systematic review of qualitative studies following hospital discharge. Crit Care. 2016;20(1):345.
Karampela I, Chrysanthopoulou E, Christodoulatos GS, Dalamaga M. Is there an obesity paradox in critical illness? Epidemiologic and metabolic considerations. Curr Obes Rep. 2020;9(3):231–44.
Schetz M, De Jong A, Deane AM, Druml W, Hemelaar P, Pelosi P, Pickkers P, Reintam-Blaser A, Roberts J, Sakr Y, et al. Obesity in the critically ill: a narrative review. Intensive Care Med. 2019;45(6):757–69.
Pepper DJ, Sun J, Welsh J, Cui X, Suffredini AF, Eichacker PQ. Increased body mass index and adjusted mortality in ICU patients with sepsis or septic shock: a systematic review and meta-analysis. Crit Care. 2016;20(1):181.
Johnson AE, Pollard TJ, Shen L, Lehman LW, Feng M, Ghassemi M, Moody B, Szolovits P, Celi LA, Mark RG. MIMIC-III, a freely accessible Critical Care database. Scientific data. 2016;3:160035.
Pi-Sunyer FXBD, Bouchard C, Carleton RA, Colditz GA, Dietz WH, et al. Executive summary of the clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. Arch Intern Med. 1998;158(17):1855–67.
Zhang Z. Multiple imputation with multivariate imputation by chained equation (MICE) package. Ann Transl Med. 2016;4(2):30.
Meira-Machado L, Cadarso-Suárez C, Gude F, Araújo A. smoothHR: an R package for pointwise nonparametric estimation of hazard ratio curves of continuous predictors. Comput Math Methods Med. 2013;2013:745742.
Brinkman S, de Jonge E, Abu-Hanna A, Arbous MS, de Lange DW, de Keizer NF. Mortality after hospital discharge in ICU patients. Crit Care Med. 2013;41(5):1229–36.
Doherty Z, Kippen R, Bevan D, Duke G, Williams S, Wilson A, Pilcher D. Long-term outcomes of hospital survivors following an ICU stay: A multi-centre retrospective cohort study. PLoS ONE. 2022;17(3):e0266038.
Tremblay A, Bandi V. Impact of body mass index on outcomes following critical care. Chest. 2003;123(4):1202–7.
Plečko D, Bennett N, Mårtensson J, Bellomo R. The obesity paradox and hypoglycemia in critically ill patients. Crit Care. 2021;25(1):378.
Martino JL, Stapleton RD, Wang M, Day AG, Cahill NE, Dixon AE, Suratt BT, Heyland DK. Extreme obesity and outcomes in critically ill patients. Chest. 2011;140(5):1198–206.
Weig T, Irlbeck T, Frey L, Paprottka P, Irlbeck M. Above and beyond BMI : Alternative methods of measuring body fat and muscle mass in critically ill patients and their clinical significance. Anaesthesist. 2016;65(9):655–62.
Jaitovich A, Khan M, Itty R, Chieng HC, Dumas CL, Nadendla P, Fantauzzi JP, Yucel RM, Feustel PJ, Judson MA. ICU admission muscle and fat mass, survival, and disability at discharge: a prospective cohort study. Chest. 2019;155(2):322–30.
Jaitovich A, Dumas CL, Itty R, Chieng HC, Khan M, Naqvi A, Fantauzzi J, Hall JB, Feustel PJ, Judson MA. ICU admission body composition: skeletal muscle, bone, and fat effects on mortality and disability at hospital discharge-a prospective, cohort study. Crit Care. 2020;24(1):566.
Acknowledgements
None.
Funding
This study was supported by Foundation of Beijing Tongren Hospital, Capital Medical University (No. 2021-YJJ-ZZL-026).
Author information
Authors and Affiliations
Contributions
DW Z and T L conceived this study. DW Z extracted the data. T L, DW Z, and C W designed and performed the statistical analyses. DW Z and Q L wrote the first draft of the manuscript. DW Z and T L reviewed and modified the final manuscript. All authors read, critically reviewed, and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All information was obtained from the MIMIC III database and was anonymized. Due to the HIPAA compliant de-identification in this database, our IRB requirement was waived.
Consent for publication
Not applicable.
Competing interest
None of the authors has declared a conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhou, D., Wang, C., Lin, Q. et al. The obesity paradox for survivors of critically ill patients. Crit Care 26, 198 (2022). https://doi.org/10.1186/s13054-022-04074-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-022-04074-1