Abstract
Objective
To assess the impact of treatment with steroids on the incidence and outcome of ventilator-associated pneumonia (VAP) in mechanically ventilated COVID-19 patients.
Design
Propensity-matched retrospective cohort study from February 24 to December 31, 2020, in 4 dedicated COVID-19 Intensive Care Units (ICU) in Lombardy (Italy).
Patients
Adult consecutive mechanically ventilated COVID-19 patients were subdivided into two groups: (1) treated with low-dose corticosteroids (dexamethasone 6 mg/day intravenous for 10 days) (DEXA+); (2) not treated with corticosteroids (DEXA−). A propensity score matching procedure (1:1 ratio) identified patients' cohorts based on: age, weight, PEEP Level, PaO2/FiO2 ratio, non-respiratory Sequential Organ Failure Assessment (SOFA) score, Charlson Comorbidity Index (CCI), C reactive protein plasma concentration at admission, sex and admission hospital (exact matching).
Intervention
Dexamethasone 6 mg/day intravenous for 10 days from hospital admission.
Measurements and main results
Seven hundred and thirty-nine patients were included, and the propensity-score matching identified two groups of 158 subjects each. Eighty-nine (56%) DEXA+ versus 55 (34%) DEXA− patients developed a VAP (RR 1.61 (1.26–2.098), p = 0.0001), after similar time from hospitalization, ICU admission and intubation. DEXA+ patients had higher crude VAP incidence rate (49.58 (49.26–49.91) vs. 31.65 (31.38–31.91)VAP*1000/pd), (IRR 1.57 (1.55–1.58), p < 0.0001) and risk for VAP (HR 1.81 (1.31–2.50), p = 0.0003), with longer ICU LOS and invasive mechanical ventilation but similar mortality (RR 1.17 (0.85–1.63), p = 0.3332). VAPs were similarly due to G+ bacteria (mostly Staphylococcus aureus) and G− bacteria (mostly Enterobacterales). Forty-one (28%) VAPs were due to multi-drug resistant bacteria. VAP was associated with almost doubled ICU and hospital LOS and invasive mechanical ventilation, and increased mortality (RR 1.64 [1.02–2.65], p = 0.040) with no differences among patients' groups.
Conclusions
Critically ill COVID-19 patients are at high risk for VAP, frequently caused by multidrug-resistant bacteria, and the risk is increased by corticosteroid treatment.
Trial registration: NCT04388670, retrospectively registered May 14, 2020.
Similar content being viewed by others
Introduction
Acute respiratory distress syndrome (ARDS) is a common complication of COVID-19 that frequently requires prolonged invasive mechanical ventilation [1].
Since some randomized controlled trials [2,3,4,5,6] demonstrated a mortality benefit from low-dose corticosteroid therapy, early steroids treatment has become standard in severe COVID-19 [7].
A high incidence of secondary infections, particularly ventilator-associated pneumonia (VAP), has been reported in critically ill COVID-19 patients. Still, the role of corticosteroids in the risk of infectious complications remains uncertain.
This multicenter propensity-matched retrospective cohort study aims to assess the impact of treatment with steroids on the incidence and outcome of VAP in mechanically ventilated COVID-19 patients.
Materials and methods
The local Ethical Committee approved the study (Comitato Etico Milano Area 2; #0008489).
This retrospective propensity-matched retrospective cohort was conducted in four dedicated COVID-19 ICUs in Lombardy (Italy) from February 24 to December 31, 2020. Patients' clinical management was shared between the centers (see Additional file 1).
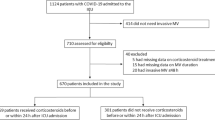
All patients admitted to ICU with laboratory-confirmed SARS-CoV-2 infection (positive Reverse-Transcription-Polymerase Chain Reaction assay of nasal swabs) were eligible for inclusion. Exclusion criteria were: (1) age < 18 years old; (2) ICU length of stay (LOS) < 48 h; (3) respiratory co-infections at ICU admission; (4) reason for ICU admission other than COVID-19; (5) treatment with immunosuppressors (i.e., tocilizumab, anakinra) and high-dose corticosteroids (> 1 mg/kg/die methylprednisolone).
After collection of clinical variables at admission, the patients' population was subdivided into two groups: (1) patients admitted before the publication of the RECOVERY trial, who did not receive corticosteroids (DEXA−); (2) patients admitted after June 2020, who received low-dose corticosteroids as per RECOVERY protocol (dexamethasone 6 mg/day intravenous 10 days) (DEXA+). A propensity score matching procedure (1:1 ratio, caliper of 0.2) was applied to identify two cohorts of patients matched based on the following covariates: age, weight, PEEP Level, PaO2/FiO2, non-respiratory Sequential Organ Failure Assessment (SOFA) score, Charlson Comorbidity Index (CCI), C-reactive protein concentration at ICU admission, and sex and admission hospital.
The primary outcome measure was the incidence rate and etiology of microbiologically confirmed bacterial VAP (see Additional file 1). For every VAP episode, the presence of sepsis or septic shock was recorded. Multidrug-resistant (MDR) VAP was defined according to the international guidelines [8]. The following secondary outcomes were recorded: survival at ICU and hospital discharge, ICU length of stay (LOS), and duration of mechanical ventilation.
Statistical analyses
Continuous variables were reported using median and interquartile range (IQR), while discrete variables with absolute and relative frequency.
Differences between groups were assessed using the chi-square test (or Fisher exact tests) and Student's t test (or Wilcoxon rank-sum test) as appropriate. The crude VAP incidence rate (IR) per 1000 patient-days (pd) in ICU and relative 95% confidence interval (CI) was estimated, considering only the first VAP occurrence and the days at risk between intubation and VAP, death, or ICU discharge. Risk Ratio (RR), Incidence Rate Ratio (IRR), and 95% CI were estimated as association measures between treatment and VAP occurrence.
Competing risk analysis was used to estimate the cumulative incidence of VAP in the two groups, with death as a competing event. The Grey test was applied to compare the cumulative incidence functions, and hazard ratio (95% CI) was estimated using the Fine and Gray subdistribution hazard function.
All tests were two-sided, and p < 0.05 was chosen to indicate statistical significance. SAS (SAS, Cary, NC, USA) and R, version 3.5.2 (R foundation, Wein, Austria) were used for statistical analysis.
Results
Between February 24, 2020, and December 31, 2020, 952 patients were admitted to the 4 participant centers ICUs; 739 met the study inclusion criteria (see Additional file 1: Fig. S1 and Table S1), and from them, the matching procedure identified a sample of 316 subjects (158 in each group) (see Additional file 1: Table S2). Patients were primarily male (78%), overweight (body mass index 28 [25–31]), with frequent cardiologic comorbidities (i.e., hypertension 47%, diabetes 16%, CCI 2 [1–3]). Patient suffered of a mostly respiratory critical illness (i.e., non-respiratory SOFA score 0[0–1], SOFA score 4 [3, 4], PaO2/FiO2 124 [93–180] mmHg) managed with lung-protective ventilation (PEEP 10 [10–12] cmH2O, tidal volume/predicted body weight 6.6 [6.0–7.4] mL/kg). Pronation was frequently employed (i.e., 65% of the patients), while renal replacement therapy and extracorporeal lung support were utilized in 8% and 4% of the patients. After matching, no clinically meaningful differences in admission parameters were observed between the patients' cohorts.
Eighty-nine (56%) DEXA+ patients developed a VAP, as compared to 55 (35%) DEXA− patients (RR 1.61 (1.26–2.09), p < 0.0001), after similar median time intervals from hospitalization, ICU admission and intubation (Table 1). The crude VAP incidence rate was higher for DEXA+ patients, 49.58 (49.26–49.91) versus 31.65 (31.38–31.91) VAP*1000/pd (IRR 1.57 (1.55–1.58), p < 0.0001). Competing risk analysis showed higher, statistically significant risk for VAP in the DEXA+ patients (HR 1.81 (1.31–2.50), p = 0.0003) (Fig. 1). DEXA+ patients showed longer ICU LOS and invasive mechanical ventilation but similar mortality (RR 1.17 (0.85–1.63), p = 0.3332).
VAP was associated with increased overall mortality (i.e., 38% vs. 27%, OR 1.64 [1.02–2.65], p = 0.040). with almost doubled mechanical ventilation (i.e., 22 [14–42] vs. 12 [6–18] days, p < 0.001 in DEXA+ patients, and 23 [14–37] vs. 11 [5–15] days, p < 0.001 in DEXA− patients), and ICU LOS (i.e., 25 [14–37] vs. 11 [7–20] days, p < 0.001 in DEXA+ patients, and 24 [15–38] vs. 12 [6–16] days, p < 0.001, in DEXA− patients), with no differences among patients' groups (see Additional file 1: Tables S3, S4 and S5).
The etiology of VAP was not different between groups (see Additional file 1: Table S6). VAPs were due to G+ bacteria (mostly Staphylococcus aureus, i.e., 83% of the G+ VAPs) and G− bacteria (mostly Enterobacterales, i.e., 45% of G- VAPs) in 33% and 67% of the cases. Forty-one (28%) VAPs were due to MDR microorganisms: 26 (29%) in DEXA+ patients, and 15 (27%) (p = 0.802). Considering patients with VAP, DEXA+ had a higher incidence rate of MDR VAP compare to DEXA− (31.48 vs. 27.83 VAP*1000/pd), with an IRR equal to 1.13 (95% CI: 1.11–1.15; p < 0.0001). No significant difference between groups was detected at competing risk analysis (sHR 1.09, 95% CI: 0.58–2.04, p = 0.800) (see Additional file 1: Fig. S2).
Discussion
In this study, we documented a high risk of VAP in mechanically ventilated COVID-19 patients, which was further increased by using corticosteroids.
We previously documented [1] that critically ill COVID-19 patients are at high risk for hospital-acquired infections, especially VAP and bloodstream infections, frequently caused by MDR bacteria. Several studies [9] showed similar results, with an apparent increased risk of infection in COVID-19 vs. non-COVID-19 patients [10].
Since the publication of the RECOVERY and subsequent randomized controlled studies [2,3,4,5,6], corticosteroids were introduced as standard clinical practice for severe COVID-19 patients. Only the CoDEX trial specifically assessed the incidence of infections [6]. However, the study was terminated early after the dissemination of the results of the RECOVERY study, and the impact of corticosteroids on infection risk could not be evaluated. A retrospective analysis [11] on the effect of corticosteroid treatment in invasively ventilated COVID-19 patients failed to show an increased risk of infections. Still, this study did not focus on VAP and included a limited number of non-matched patients (i.e., 151). Moreover, 30% of the cases received concomitant treatment with other immunosuppressants (e.g., tocilizumab), and 10% of the subjects had a secondary co-infection at admission.
To control the effect of potential confounders and of eventual selection bias in the use of steroids, in the present study we: (1) excluded all patients treated with rescue immunosuppressants (i.e., high-dose corticosteroids, tocilizumab); (2) excluded all patients with co-infections; (3) performed a rigorous matching approach—comprising the basal inflammatory status by the CRP at admission—that allowed to compare two "identical" groups of patients except for their exposure status; (4) focused only on microbiologically confirmed VAP; (5) performed a complete follow-up, until death or hospital discharge (and thus excluding the possibility for a late protective effect of steroids on VAP risk).
Our study has several limitations. First, it is a retrospective analysis. Second, there was no standard antibiotic strategy across different centers and periods. Third, since we included only microbiologically confirmed VAP, we may have underestimated the incidence of low-yield cultures (e.g., cultures obtained while the patients were receiving an antibiotic treatment) infections. Fourth, the study was conducted in a single Western European country with a high incidence of MDR infection, limiting the generalizability of our findings. Lastly, unmeasurable, and unavailable confounders (e.g., evolutionary patterns of microbiological epidemiology, different period of enrollment) may have influenced our results.
Conclusions
Critically ill COVID-19 patients are at high risk for VAP, frequently caused by multidrug-resistant bacteria, and the risk is increased by corticosteroid treatment. Clinicians should make every effort to implement protocols for the surveillance and prevention of infectious complications. Further longitudinal studies could focus on benefits and costs of DEXA connected to VAP incidence and survival.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- CCI:
-
Charlson Comorbidity Index
- CI:
-
Confidence interval
- COVID-19:
-
Coronavirus disease 2019
- DEXA:
-
Dexamethasone
- FiO2 :
-
Inspired fraction of oxygen
- HR:
-
Hazard ratio
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- IR:
-
Incidence rate
- IRR:
-
Incidence rate ratio
- LOS:
-
Length of stay
- MDR:
-
Multidrug-resistant
- OR:
-
Odds ratio
- PaO2 :
-
Partial pressure of oxygen
- PEEP:
-
Positive end-expiratory pressure
- RR:
-
Risk ratio
- SOFA:
-
Sequential organ failure assessment
- VAP:
-
Ventilator-associated pneumonia
References
Grasselli G, Scaravilli V, Mangioni D, et al. Hospital-acquired infections in critically Ill patients with COVID-19. Chest. 2021;160(2):454–65.
Horby P, Lim WS, Emberson JR, et al. Dexamethasone in Hospitalized Patients with Covid-19 - Preliminary Report. N Engl J Med 2020. Published online July 2020.
Sterne JACC, Murthy S, Diaz JV, et al. Association between administration of systemic corticosteroids and mortality among critically Ill patients with COVID-19: a meta-analysis. JAMA. 2020;324(13):1330–41.
Jeronimo CMP, Farias MEL, Val FFA, et al. Methylprednisolone as adjunctive therapy for patients hospitalized with coronavirus disease 2019 (COVID-19; metcovid): a randomized, double-blind, phase IIb, Placebo-controlled Trial. Clin Infect Dis. 2021;72(9):e373–81.
Angus DC, Derde L, Al-Beidh F, et al. Effect of hydrocortisone on mortality and organ support in patients with severe COVID-19: the REMAP-CAP COVID-19 corticosteroid domain randomized clinical trial. JAMA. 2020;324(13):1317–29. https://doi.org/10.1001/jama.2020.17022.
Tomazini BM, Maia IS, Cavalcanti AB, et al. Effect of dexamethasone on days alive and ventilator-free in patients with moderate or severe acute respiratory distress syndrome and COVID-19: the CoDEX randomized clinical trial. JAMA. 2020;324(13):1307–16.
Alhazzani W, Møller MH, Arabi YM, et al. Surviving sepsis campaign: guidelines on the management of critically Ill adults with Coronavirus Disease 2019 (COVID-19). Crit Care Med. 2020;48(6):e440–69.
Magiorakos A, Srinivasan A, Carey RB, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Microbiology. 2011;18(3):268–81.
Buetti N, Ruckly S, de Montmollin E, et al. COVID-19 increased the risk of ICU-acquired bloodstream infections: a case-cohort study from the multicentric OUTCOMEREA network. Intensive Care Med. 2021;47(2):180–7. https://doi.org/10.1007/s00134-021-06346-w.
Rouzé A, Martin-Loeches I, Povoa P, et al. Relationship between SARS-CoV-2 infection and the incidence of ventilator-associated lower respiratory tract infections: a European multicenter cohort study. Intensive Care Med. 2021;47(2):188–98. https://doi.org/10.1007/s00134-020-06323-9.
Gragueb-Chatti I, Lopez A, Hamidi D, et al. Impact of dexamethasone on the incidence of ventilator-associated pneumonia and blood stream infections in COVID-19 patients requiring invasive mechanical ventilation: a multicenter retrospective study. Ann Intensive Care. 2021. https://doi.org/10.1186/s13613-021-00876-8.
Acknowledgements
Not applicable.
Funding
This work was partly funded by the Italian Ministry of Health—Current research IRCCS.
Author information
Authors and Affiliations
Contributions
VS and GG conceived and designed the study; AG performed data management; FB analyzed the data alongside AG and VS; VB, GB, GM, and MG collected the data; VS, AG, and VB contributed to data analysis and interpretation. AP and GG supervised the study. All authors: drafting the manuscript and approving the manuscript for submission. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethical Committees of all participating centers (Promoting Centre’s Ethical Committee: Comitato Etico Milano Area 2; protocol: 0008489; date of approval: March 20, 2020). The need for informed consent from individual patients was waived owing to the retrospective nature of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Additional methods and results.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Scaravilli, V., Guzzardella, A., Madotto, F. et al. Impact of dexamethasone on the incidence of ventilator-associated pneumonia in mechanically ventilated COVID-19 patients: a propensity-matched cohort study. Crit Care 26, 176 (2022). https://doi.org/10.1186/s13054-022-04049-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-022-04049-2