Abstract
Background
Interleukin (IL)-18 is a marker of inflammasome activation, and high baseline plasma IL-18 is associated with increased mortality in patients with sepsis-induced ARDS. The aim of this analysis was to determine if simvastatin was associated with benefit in patients with ARDS and high plasma IL-18.
Methods
In this secondary analysis of the HARP-2 study, we compared 28-day mortality and response to simvastatin according to baseline plasma IL-18 using cox proportional hazards analysis. Separately, monocyte-derived macrophages from healthy volunteers were pre-incubated with simvastatin or rosuvastatin before stimulation with ATP and LPS, and the effect on secreted IL-18 and IL-1β compared.
Results
511 patients from HARP-2 had available data. High baseline plasma IL-18 (≥ 800 pg/ml) was associated with increased 28-day mortality (high IL-18 30.6% vs. low IL-18 17.5%; HR 1.89 [95% CI 1.30–2.73]; p = 0.001). Allocation to simvastatin in patients with high baseline plasma IL-18 was associated with a lower probability of 28-day mortality compared with placebo (24.0% vs 36.8%; p = 0.01). Finally, simvastatin, but not rosuvastatin, reduced stimulated macrophage secretion of IL-18 and IL-1β.
Conclusion
In patients with high baseline plasma IL-18, simvastatin is associated with a higher probability of survival, and this effect may be due to reduced inflammasome activation. These data suggest that baseline plasma IL-18 may allow a personalised treatment approach by identifying patients with ARDS who could benefit from simvastatin therapy.
Similar content being viewed by others
Introduction
The acute respiratory distress syndrome (ARDS) is a common clinical syndrome that is characterised by life-threatening acute hypoxaemic respiratory failure [1, 2]. ARDS results from excessive host inflammation that exacerbates the loss of alveolar-epithelial, capillary-endothelial barrier integrity [3].
The role of the inflammasome in the pathophysiology of ARDS is increasingly recognised. Activation of the NLR family pyrin domain containing 3 (NLRP3) inflammasome leads to caspase-1 activation which triggers cell death via pyroptosis and secretion of both IL-18 and IL-1β [4, 5]. In a murine model of hyperoxia-induced lung injury, mice deficient in NLRP3 had reduced lung injury compared with wild-type mice [6], whilst mice deficient in either caspase-1 or IL-18 had less alveolar neutrophilia, and lower lung injury scores, when exposed to injurious mechanical ventilation [7]. Critically ill patients with ARDS have higher plasma IL-18 than those without ARDS [7]. Plasma IL-18 also correlates with severity of hypoxaemia and mortality in patients with ARDS [8].
Simvastatin (in the HARP-2 trial) [9] and rosuvastatin (in the SAILS trial) [10] did not improve overall clinical outcomes in randomised controlled trials as therapies for ARDS. In a post hoc analysis of SAILS, baseline plasma IL-18 was positively associated with mortality and allocation to rosuvastatin was independently associated with increased odds of a rise in plasma IL-18 concentration [11], suggesting that rosuvastatin induced plasma IL-18. In a murine model of acute lung injury, it was demonstrated that pravastatin, a hydrophilic statin similar to rosuvastatin, increased pulmonary IL-1β and IL-18 in vivo and enhanced macrophage inflammasome activity in vitro [12]. This enhanced inflammasome activity was dependent on mitochondrial reactive oxygen species (mROS) generation in response to pravastatin. Although mROS generation has been reported to be differentially induced by hydrophilic and lipophilic statins [13], it is uncertain whether the pro-inflammasome activity observed is a statin class effect or specific to hydrophilic statins such as rosuvastatin and pravastatin.
In contrast to rosuvastatin, simvastatin is lipophilic and lipophilic statins have been shown to reduce NLRP3 inflammasome activation in endothelial cells [14]. Furthermore, latent class analysis of both the HARP-2 and SAILS trials demonstrated a difference in treatment effect; simvastatin improved survival in hyper-inflammatory ARDS, while rosuvastatin did not [15, 16]. This finding supports the concept that the effect of statins in ARDS may differ based on whether they are lipophilic or hydrophilic.
Therefore, we hypothesised that compared with rosuvastatin, simvastatin may have a different effect on outcomes in patients with ARDS who have higher baseline plasma IL-18 concentration. To address this, we performed a secondary analysis of the HARP-2 trial [9] and performed an in vitro study evaluating the effect of rosuvastatin and simvastatin in monocyte-derived macrophages.
Materials and methods
This was a secondary analysis of the previously reported HARP-2 clinical trial [9]. In brief, 540 patients from 40 intensive care units across the UK and Ireland who fulfilled the American-European Consensus Conference definition for acute lung injury or ARDS [17] within the previous 48 h, were randomised to receive either simvastatin (80 mg once per day) or placebo for up to 28 days. Where available, baseline plasma samples were obtained from patients following trial enrolment, and this secondary analysis includes all patients from the HARP-2 trial with available baseline plasma samples. Ethical approval was granted by Queen’s University Belfast School Research Ethics Committee (ref. 14/06). During the consent process for HARP-2, written informed consent was obtained for storage and future analysis of samples. The primary outcome was 28-day mortality. Although ventilator-free days (VFDs) up to day 28 was the primary outcome in HARP-2 [9], we used 28-day mortality as the primary outcome for the purposes of this secondary analysis as it is a more patient-centred outcome to inform future trials.
Monocytes were isolated from the peripheral blood of healthy volunteers using density gradient centrifugation across a Ficoll-Paque gradient followed by adherence [18, 19], and were differentiated into macrophages (monocyte-derived macrophages (MDM)) by incubating in GM-CSF for 7 days [20]. Following a 24-h period of rest in fresh medium, macrophages were pre-treated for 4 h with 50 µM of either simvastatin or rosuvastatin calcium (Sigma-Aldrich, Germany). Cells were then treated with 100 ng/ml Escherichia coli 026:B6 lipopolysaccharide (LPS) for 3 h, before treatment with 2 mM adenosine triphosphate (ATP) (Sigma-Aldrich, Germany) for 30 min [21, 22]. An unstimulated control and a stimulated control (LPS + ATP) were also assessed. Cell culture supernatants were collected and processed for later analysis. MDMs from each patient were studied in each condition.
Total IL-18 and IL1β concentrations were measured in plasma or cell supernatants in duplicate by enzyme-linked immunosorbent assay (Duoset, R&D systems, Bio-Techne LTD, UK). If the coefficient of variation was > 10%, sample measurement was repeated in duplicate.
Statistical methods
Descriptive statistics included calculation of proportions for categorical variables and mean (standard deviation (SD)) for continuous variables. The population of included patients was grouped by 28-day survivor status, and the statistical difference between these groups was calculated using chi-square test (or Fisher exact test) for discrete variables and by t test for continuous variables.
We used the previously reported threshold of IL-18 ≥ 800 pg/ml, demonstrated to be associated with increased mortality in patients with sepsis-associated ARDS, to define a high baseline plasma IL-18 [11]. The relationship between 28-day mortality and high baseline IL-18 was tested by proportional hazards regression using the actual time of death, censored at 28 days. Age, baseline APACHE II score, pre-randomisation partial pressure of oxygen to fraction of inspired oxygen (P/F) ratio, vasopressor use and having sepsis were pre-specified as clinically important variables to include in the models. These variables were selected to minimise the potential for confounding caused by increased plasma IL-18 with increasing age [23], the potential effect of baseline organ dysfunction and illness severity on plasma IL-18 concentration, and that there may be a difference in outcomes between patients with ARDS due to sepsis compared with ARDS from other causes [24]. SOFA score, baseline plasma C-reactive protein (CRP), plateau pressure and tidal volume were evaluated in an expanded univariate analysis to evaluate for an effect of baseline organ dysfunction, inflammation, pulmonary compliance and volutrauma. APACHE and SOFA were not both included in the multivariable models because the severity of illness variables from which they are calculated are broadly the same. The joint effect of simvastatin treatment and elevated IL-18 was studied by including the interaction term in the model and by subgroup analysis. As secondary analyses, area under the curve (AUC) for IL-18 and 28-day mortality was calculated, univariate and multivariable analysis was performed to assess the effect of this threshold on 28-day mortality, and correlation between baseline IL-18 and SOFA score at baseline, days 3 and 7 was calculated using Pearson’s r test.
Patients with incomplete data fields (e.g., missing APACHE II score) were excluded from the regression analyses. Results of logistic regression models are shown as odds ratios (OR) with 95% confidence intervals (CI) and p-value, and for proportional hazards regression as hazard ratios with 95% confidence intervals (CI) and p-value. Data were assumed missing completely at random, and this was confirmed using Little’s MCAR test (p = 0.85). These analyses were performed using the R statistical package (version 3.6.2).
In vitro data were normalised to the stimulated control and assessed using Kruskal–Wallis test with Dunn’s multiple comparison test to compare differences between the simvastatin and rosuvastatin groups, and between the statin groups and both the stimulated and unstimulated controls. The statistical analyses for the in vitro data were performed, and all the manuscript figures produced, using GraphPad Prism version 5.03.
Results
Of the 540 patients recruited to the HARP-2 trial, 511 patients (95% of the enrolled trial population) were included in this analysis [9]. 28 patients had no baseline plasma sample available, and outcome data were unavailable for one patient. Of the included patients, 124 (24.3%) did not survive to day 28. Baseline characteristics are shown in Table 1. Non-survivors had a higher baseline plasma IL-18, a higher baseline APACHE II score, a lower pre-randomisation P/F ratio, were older, and more frequently receiving vasopressors.
Of the 511 patients included in this analysis, 453 had a complete dataset and were included in regression analyses. There was no difference in baseline characteristics between these patients and the 86 patients recruited to HARP-2 with available data that were not included (Additional file 1: Table E1, supplementary appendix). Similarly, there was no difference in 28-day mortality between patients included and excluded in regression analyses (24% vs. 27%; p = 0.69).
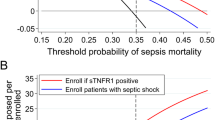
High baseline plasma IL-18 is associated with increased 28-day mortality
265 patients (51.9%) were categorised as having high baseline plasma IL-18, based on a previously defined threshold of ≥ 800 pg/ml [11], and 28-day mortality was higher in these patients than in patients with low baseline plasma IL-18 (high 30.6% vs. low 17.5%). The hazard ratio (HR) for death by day 28 associated with a high baseline plasma IL-18 was 1.89 (95% CI 1.30–2.73; cox proportional hazards p = 0.001) (Fig. 1). When adjusted for age, baseline APACHE II score, pre-randomisation P/F ratio, sepsis and vasopressor use, the hazard ratio for death by day 28 remained elevated for high baseline plasma IL-18 (1.61 [1.08–2.40]; p = 0.02) (Additional file 1: Table E2). Similarly, there were fewer ventilator-free days in patients with high baseline plasma IL-18 compared with those with low baseline plasma IL-18 (10.1 (10.1) vs. 14.1 (9.9); p < 0.001).
When analysing IL-18 as a (log-transformed) continuous variable, the association with 28-day mortality was maintained in univariate (HR 1.35 [1.15–1.58; p < 0.001) and multivariable analysis (1.30 [1.08–1.57]; p = 0.01), after adjustment for randomisation to simvastatin and baseline characteristics (Additional file 1: Table E3).
AUC analysis identified that plasma IL-18 concentration of 1014 pg/ml had the optimal specificity for 28-day mortality in this cohort (Additional file 1: Table E4). 216 (42.2%) of patients had a baseline plasma IL-18 ≥ 1014 pg/ml, and of these patients 70 (32%) did not survive to 28-day days. In both univariable and multivariable analysis, a plasma IL-18 threshold ≥ 1014 pg/ml remained associated with 28-day mortality (adjusted odds ratio (OR) 2.08 (1.30–3.33; p = 0.002) (Additional file 1: Table E5).
Finally, there was no relationship between baseline plasma CRP, plateau pressure or tidal volume with 28-day mortality, whilst SOFA score demonstrated a similar effect to that observed with APACHE-II score (Additional file 1: Table E6).
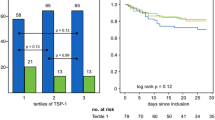
Simvastatin is associated with reduced mortality in patients with high baseline plasma IL-18
Of the patients with high baseline IL-18, 129 (48.7%) were randomised to receive simvastatin in HARP-2. In patients with high baseline IL-18, survival to day 28 was higher in patients randomised to simvastatin compared with placebo (24.0% vs 36.8% 28-day mortality; p = 0.01). In contrast, 118 (48.0%) patients with low baseline IL-18 were randomised to receive simvastatin, and there was no difference in 28-day survival between these patients and those randomised to receive placebo (17.8% vs. 17.2% 28-day mortality; p = 0.75) (Fig. 2).
28-day survival stratified by baseline IL-18 and treatment simvastatin vs. placebo). Kaplan–Meier curve of survival from enrolment to day 28. Overall p value < 0.001. Patients with high baseline IL-18 (≥ 800 pg/ml) treated with simvastatin vs placebo p = 0.01; patients with low baseline IL-18 (< 800 pg/ml) treated with simvastatin vs. placebo p = 0.75. Interaction of simvastatin and high baseline IL-18 p = 0.19
In multivariable logistic regression analysis, in patients with high baseline plasma IL-18, allocation to simvastatin was associated with reduced odds of 28-day mortality (adjusted OR 0.39 (0.20–0.73; p = 0.004) (Additional file 1: Table E7). However, formal statistical testing for an interaction between simvastatin and baseline plasma IL-18 was not significant (p = 0.19). The results were similar when a plasma IL-18 threshold of ≥ 1014 pg/ml was used (p = 0.49).
Baseline plasma IL-18 is positively correlated with SOFA score during the first 7 days of ARDS
To understand whether baseline plasma IL-18 may be related to systemic organ dysfunction in the first 7 days of ARDS, correlation between baseline plasma IL-18 and SOFA score at baseline, days 3 and 7 was calculated. At each timepoint there was a positive correlation between baseline plasma IL-18 and SOFA score (baseline (Pearson r 0.28 [0.19, 0.6]; p < 0.0001); day 3 (0.26 [0.17, 0.34]; p < 0.0001); day 7 0.20 [0.09, 0.30]; p = 0.001) (Additional file 1: Figure S1).
Simvastatin, but not rosuvastatin, reduces inflammasome activation in MDMs
To understand the potential mechanism for the disparate findings between rosuvastatin (reported in SAILS [11]) and simvastatin (in HARP-2 that are reported here), the effects of statin therapy on inflammasome activation in macrophages, as measured by IL-18 and IL-1β release, was assessed. Macrophages were pre-treated with either rosuvastatin or simvastatin prior to stimulation with LPS and ATP to induce inflammasome activation. Simvastatin, but not rosuvastatin, significantly reduced secretion of IL-1β and IL-18 in response to LPS and ATP. Furthermore, macrophage secretion of IL-1β was significantly higher in the rosuvastatin pre-treatment group compared to the unstimulated control, whilst there was no difference between the simvastatin pre-treatment group and the unstimulated control (Fig. 3).
Effect of statin pre-treatment on monocyte-derived macrophage inflammasome activation. Monocyte-derived macrophages were pre-treated with either 50 µM simvastatin or 50 µM rosuvastatin for 4 h before stimulation with 100 ng/ml LPS and 2 mM ATP. In contrast to rosuvastatin, simvastatin significantly reduced the production of both (A) IL-18 and (B) IL-1β by MDMs (p < 0.05). When compared to the unstimulated control, rosuvastatin pre-treatment was associated with significantly higher IL-1β production (p < 0.05). Data analysed using Kruskal–Wallis test with Dunn’s multiple comparison test for between group differences. * = p < 0.05. N = 6 for all groups
Discussion
In this secondary analysis of the HARP-2 clinical trial [9], we confirmed that baseline plasma IL-18 (≥ 800 pg/ml) is associated with mortality in a broad population of patients with ARDS, and present the novel finding that simvastatin may be associated with reduced mortality in patients with ARDS who have high baseline plasma IL-18 (≥ 800 pg/ml). Furthermore, we performed mechanistic studies that may explain the disparate effects of rosuvastatin and simvastatin, showing that in contrast to rosuvastatin, simvastatin pre-treatment reduced MDM inflammasome activity in human macrophages.
In addition to the findings from SAILS [11], enhanced inflammasome activity has been previously been identified in patients with ARDS when compared with patients with sepsis, systemic inflammatory response syndrome, and healthy controls [7]. Our data support the theory that early plasma IL-18 concentration is a prognostic marker in ARDS, which is also consistent with previous data demonstrating that elevated serum IL-18 in the early phase of ARDS is associated with increased mortality at 90 days [8]. Furthermore, we demonstrate that there is a positive correlation between baseline plasma IL-18 and SOFA score at baseline, days 3 and 7. Although the correlation was weak, these data support further investigation as a component of further study of IL-18 as a prognostic marker for ARDS.
Simvastatin has been studied as a therapy for ARDS because of its pleiotropic effects [25]. Whilst pre-clinical and early phase clinical trial data supported an anti-inflammatory effect in healthy subjects with experimental lung injury [19], and patients with ARDS [26], when studied in a large randomised clinical trial, there was no significant effect on clinical outcomes in patients with ARDS [9]. Heterogeneity in ARDS biology is increasingly recognized, with numerous ARDS cohorts best described by 2 phenotypes rather than one [27,28,29]. We have previously shown that the hyperinflammatory sub-phenotype (identified as part of latent class analysis) may benefit from simvastatin therapy [15], suggesting that a personalised approach to therapy is likely to be required in patients with ARDS. In this secondary analysis of the HARP-2 clinical trial, we present the novel finding that in patients with high baseline plasma IL-18, not measured as part of latent class analysis, randomisation to simvastatin was associated with reduced mortality at 28-days. Compared with latent class analysis, this single biomarker approach may be simpler for enrichment of future clinical trials for patients who may benefit from simvastatin. However, there was no significant interaction between simvastatin and high baseline plasma IL-18, and further studies are required to evaluate this relationship and the efficacy of using baseline plasma IL-18 as part of a personalised medicine approach to treatment.
Our in vitro data suggest there is a different effect on inflammasome activation between rosuvastatin and simvastatin, as we demonstrate that macrophages pre-treated with simvastatin, but not those pre-treated with rosuvastatin, had reduced inflammasome activation, as measured by IL-18 and IL-1β release, in response to LPS. Differences in the treatment effect between these statins have previously been demonstrated. For example, in the SAILS trial there was no treatment interaction between rosuvastatin and the hyper-inflammatory sub-phenotype [16], whilst there was a signal for benefit of simvastatin in patients with a hyper-inflammatory sub-phenotype in HARP-2 [15]. These data may reflect pharmacological differences between hydrophilic and lipophilic statins [12, 13]. Obesity can upregulate inflammasome activity [30], and although data on body mass index were not presented for patients recruited to SAILS [11] it is possible there may be differences in obesity, and therefore plasma IL-18 concentration, between the trial populations that may have influenced the effect of statin therapy. Finally, SAILS enrolled patients with sepsis-associated ARDS [10], whilst HARP-2 included patients irrespective of their risk factor for developing ARDS [9]. The attributable mortality from ARDS in patients with sepsis may be lower compared to patients with other aetiological risk factors [24]. This suggests the mechanisms implicated in determining mortality may differ according to the aetiological risk factor. Although the majority of patients in HARP-2 had sepsis, the difference in the recruited patient populations between the two studies may contribute to the difference in the observed effect between this study and the previously reported analysis of the SAILS study [11].
Our report has some limitations. First, it is not possible to infer causation from our data, and therefore we are unable to state with certainty that simvastatin reduces mortality of patients with ARDS who have high baseline plasma IL-18. Second, the robustness of our findings is limited by the absence of a significant interaction between simvastatin therapy and high baseline plasma IL-18, and this may relate to a lack of power to detect a statistically significant interaction. Whilst the magnitude of mortality difference of > 10% in patients with high IL-18 randomised to simvastatin would be clinically important, this lack of statistical significance of interaction makes these results more exploratory. Third, our measurement of total IL-18 may not fully reflect IL-18 activity because of the presence of IL-18 binding protein, which binds free active IL-18. In measuring total IL-18 it is plausible that we have measured both bound and free IL-18, and this measurement may not fully reflect IL-18 activity [31]. However, like sepsis, ARDS is characterised by systemic inflammation, and it is known that in sepsis although IL-18 binding protein is upregulated, free IL-18 remains elevated [32], suggesting that elevated total IL-18 is likely to still represent an increase in pro-inflammatory, free active IL-18. To better understand the relationship between total IL-18, IL-18 binding protein, inflammation, and clinical outcomes in patients with ARDS, further studies are required. Fourth, this is not a prospective study but a retrospective analysis of a clinical trial. Fifth, whilst the use of a pre-specified threshold to determine high plasma IL-18 may be considered a strength, we demonstrate that a baseline plasma IL-18 threshold of 1014 pg/ml had greater specificity for 28-day mortality in this population. Although the findings were similar, and the sensitivity for 28-day mortality was higher with the 800 pg/ml threshold, it remains uncertain what value of plasma IL-18 should be considered “high” in patients with ARDS and thus used in future studies. Sixth, the MDM data presented in this manuscript suggest that simvastatin attenuates macrophage-induced IL-18 and IL-1β release. These data represent a pre-treatment model which is different to both the SAILS and HARP-2 studies which evaluated statin therapy after ARDS onset, whilst prior statin use was an exclusion criteria [9, 10]. Furthermore, these in vitro findings were only evaluated in monocyte-derived macrophages. Although macrophages contribute to the pathophysiology of lung injury in ARDS [33], other cell types are also important in the development of ARDS [34]. It is likely that the effect of simvastatin in patients with high baseline plasma IL-18 is not exclusively mediated via macrophage activity and our findings should be considered hypothesis-generating. There remains a need for further studies in other cell types, and in addition to IL-18 secretion, measurement of IL-18 expression with RT-PCR would be valuable. In addition, the use of clinically relevant human models that may more accurately reflect ARDS biology [35], will further improve understanding of the role of IL-18 in ARDS.
Conclusion
In summary, high baseline plasma IL-18 is independently associated with increased mortality in patients with ARDS, and patients with high plasma IL-18 at baseline had reduced 28-day mortality when randomised to simvastatin. These results require prospective validation in clinical trials to determine the potential for a personalised approach to ARDS that uses baseline plasma IL-18 to identify those who might benefit from simvastatin therapy.
Availability of data and materials
The dataset used to generate this manuscript may be made available from the corresponding author on reasonable request.
References
Bellani G, Laffey JG, Pham T, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315:788–800.
Mac Sweeney R, McAuley DF. Acute respiratory distress syndrome. Lancet. 2016;388:2416–30.
The ARDS Definition Task Force. Acute respiratory distress syndrome: the berlin definition. JAMA. 2012;307:2526–33.
Martinon F, Burns K, Tschopp J. The inflammasome: a molecular platform triggering activation of inflammatory caspases and processing of proIL-β. Mol Cell. 2002;10:417–26.
Latz E, Xiao TS, Stutz A. Activation and regulation of the inflammasomes. Nat Rev Immunol. 2013;13:397–411.
Fukumoto J, Fukumoto I, Parthasarathy PT, Cox R, Huynh B, Ramanathan GK, et al. NLRP3 deletion protects from hyperoxia-induced acute lung injury. Am J Physiol Cell Physiol. 2013;305:C182–9.
Dolinay T, Kim YS, Howrylak J, Hunninghake GM, An CH, Fredenburgh L, et al. Inflammasome-regulated cytokines are critical mediators of acute lung injury. Am J Respir Crit Care Med. 2012;185:1225–34.
Makabe H, Kojika M, Takahashi G, Matsumoto N, Shibata S, Suzuki Y, et al. Interleukin-18 levels reflect the long-term prognosis of acute lung injury and acute respiratory distress syndrome. J Anesth. 2012;26:658–63.
McAuley DF, Laffey JG, O’Kane CM, Perkins GD, Mullan B, Trinder TJ, et al. Simvastatin in the acute respiratory distress syndrome. N Engl J Med. 2014;371:1695–703.
The National Heart, Lung, and Blood Institute ARDS Clinical Trials Network Rosuvastatin for Sepsis-Associated Acute Respiratory Distress Syndrome. N Engl J Med. 2014;370:2191–200.
Rogers AJ, Guan J, Trtchounian A, Hunninghake GM, Kaimal R, Desai M, et al. Association of elevated plasma interleukin-18 level with increased mortality in a clinical trial of statin treatment for acute respiratory distress syndrome. Crit Care Med. 2019;47:1089–96.
Xu J-F, Washko GR, Nakahira K, Hatabu H, Patel AS, Fernandez IE, et al. Statins and pulmonary fibrosis. Am J Respir Crit Care Med. 2012;185:547–56.
Urbano F, Bugliani M, Filippello A, Scamporrino A, Di Mauro S, Di Pino A, et al. Atorvastatin but not pravastatin impairs mitochondrial function in human pancreatic islets and rat β-cells. Direct effect of oxidative stress. Sci Rep. 2017;7:11863.
Wang S, Xie X, Lei T, Zhang K, Lai B, Zhang Z, et al. Statins attenuate activation of the NLRP3 inflammasome by oxidized LDL or TNFα in vascular endothelial cells through a PXR-dependent mechanism. Mol Pharmacol. 2017;92:256–64.
Calfee CS, Delucchi KL, Sinha P, Matthay MA, Hackett J, Shankar-Hari M, et al. Acute respiratory distress syndrome subphenotypes and differential response to simvastatin: secondary analysis of a randomised controlled trial. Lancet Respir Med. 2018;6:691–8.
Sinha P, Delucchi KL, Thompson BT, McAuley DF, Matthay MA, Calfee CS, et al. Latent class analysis of ARDS subphenotypes: a secondary analysis of the statins for acutely injured lungs from sepsis (SAILS) study. Intensive Care Med. 2018;44:1859–69.
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, et al. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;149:818–24.
O’Kane CM, Elkington PT, Jones MD, Caviedes L, Tovar M, Gilman RH, et al. STAT3, p38 MAPK, and NF-κB drive unopposed monocyte-dependent fibroblast MMP-1 secretion in tuberculosis. Am J Respir Cell Mol Biol. 2010;43:465–74.
Shyamsundar M, McKeown STW, O’Kane CM, Craig TR, Brown V, Thickett DR, et al. Simvastatin decreases lipopolysaccharide-induced pulmonary inflammation in healthy volunteers. Am J Respir Crit Care Med. 2009;179:1107–14.
Morrison TJ, Jackson MV, Cunningham EK, Kissenpfennig A, McAuley DF, O’Kane CM, et al. Mesenchymal stromal cells modulate macrophages in clinically relevant lung injury models by extracellular vesicle mitochondrial transfer. Am J Respir Crit Care Med. 2017;196:1275–86.
Bauernfeind FG, Horvath G, Stutz A, Alnemri ES, MacDonald K, Speert D, et al. Cutting edge: NF-κB activating pattern recognition and cytokine receptors license NLRP3 inflammasome activation by regulating NLRP3 expression. J Immunol. 2009;183:787–91.
Bezbradica JS, Coll RC, Schroder K. Sterile signals generate weaker and delayed macrophage NLRP3 inflammasome responses relative to microbial signals. Cell Mol Immunol. 2017;14:118–26.
Ferrucci L, Corsi A, Lauretani F, Bandinelli S, Bartali B, Taub DD, et al. The origins of age-related proinflammatory state. Blood. 2005;105:2294–9.
Torres LK, Hoffman KL, Oromendia C, Diaz I, Harrington JS, Schenck EJ, et al. Attributable mortality of acute respiratory distress syndrome: a systematic review, meta-analysis and survival analysis using targeted minimum loss-based estimation. Thorax. 2021;76:1176–85.
Craig T, O’Kane C, McAuley DF. Potential mechanisms by which statins modulate the development of acute lung injury. In: Vincent JL, editor. Yearb Intensive Care Emerg Med. Berling: Springer; 2007. p. 276–88.
Craig TR, Duffy MJ, Shyamsundar M, McDowell C, O’Kane CM, Elborn JS, et al. A randomized clinical trial of hydroxymethylglutaryl–coenzyme a reductase inhibition for acute lung injury (the HARP study). Am J Respir Crit Care Med. 2011;183:620–6.
Calfee CS, Eisner MD, Ware LB, Thompson BT, Parsons PE, Wheeler AP, et al. Trauma-associated lung injury differs clinically and biologically from acute lung injury due to other clinical disorders. Crit Care Med. 2007;35:2243–50.
Calfee CS, Delucchi K, Parsons PE, Thompson BT, Ware LB, Matthay MA. Subphenotypes in acute respiratory distress syndrome: latent class analysis of data from two randomised controlled trials. Lancet Respir Med. 2014;2:611–20.
Calfee CS, Janz DR, Bernard GR, May AK, Kangelaris KN, Matthay MA, et al. Distinct molecular phenotypes of direct vs indirect ARDS in single-center and multicenter studies. Chest. 2015;147:1539–48.
Sharma BR, Kanneganti T-D. NLRP3 inflammasome in cancer and metabolic diseases. Nat Immunol. 2021;22:550–9.
Dinarello C, Novick D, Kim S, Kaplanski G. Interleukin-18 and IL-18 binding protein. Front Immunol. 2013. https://doi.org/10.3389/fimmu.2013.00289.
Novick D, Schwartsburd B, Pinkus R, Suissa D, Belzer I, Sthoeger Z, et al. A novel IL-18BP ELISA shows elevated serum IL-18BP in sepsis and extensive decrease of free IL-18. Cytokine. 2001;14:334–42.
Frank JA, Wray CM, McAuley DF, Schwendener R, Matthay MA. Alveolar macrophages contribute to alveolar barrier dysfunction in ventilator-induced lung injury. Am J Physiol Lung Cell Mol Physiol. 2006;291:L1191–8.
Perkins GD, Nathani N, McAuley DF, Gao F, Thickett DR. In vitro and in vivo effects of salbutamol on neutrophil function in acute lung injury. Thorax. 2007;62:36–42.
Proudfoot AG, McAuley DF, Griffiths MJD, Hind M. Human models of acute lung injury. Model Mech. 2011;4:145–53.
Acknowledgements
The views expressed in this article are those of the authors and not necessarily those of the Medical Research Council (MRC), National Health Service, NIHR, or Department of Health.
Funding
This study was supported by the UK EME Programme, an MRC and NIHR partnership (08/99/08 and 16/33/01). The EME Programme is funded by the MRC and NIHR, with contributions from the Chief Scientist Office in Scotland, the National Institute for Social Care and Health Research in Wales, and the Health and Social Care (HSC) Research and Development Division, Public Health Agency for Northern Ireland. Additionally, MS-H is supported by the NIHR Clinician Scientist Award (CS-2016-16-011).
Author information
Authors and Affiliations
Contributions
AJB, PF, CMO and DFM conceived and designed this secondary analysis of the HARP-2 study. AJB, IB, CMO and DFM developed the statistical analysis plan. PF and JC performed laboratory experiments, and AJB prepared the dataset. IB performed statistical analysis. AJB, PF, MS-H, AJR and DFM drafted the first version of the manuscript, and all authors critically revised the manuscript and approved the final version. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was granted by Queen’s University Belfast School Research Ethics Committee (ref. 14/06). During the consent process for HARP-2, written informed consent was obtained for storage and future analysis of samples.
Consent for publication
Not applicable.
Competing interests
Outside of the submitted work, and in the past 36 months, Prof O’Kane has received funding from Wellcome Trust, MRC, Northern Ireland Health and Social Care Research and Development Office, and Innovate UK, for ARDS research. Prof O’Kane has received fees for grant panel membership, including the review of ARDS-related projects, from the California Institute for Regenerative Medicine (CIRM). Outside of the submitted work, the spouse of CO’K has received consultancy/educational fees from Bayer, GSK, Boehringer Ingelheim, Eli Lilly, SOBI and Novartis, and fees for being a DMEC member for VIr Biotechnology and Faron. Prof O’Kane has received consultancy fees from Insmed for unrelated work. Prof McAuley has received funding to his institution for studies outside of this submitted work from the NIHR, Wellcome Trust, Innovate UK, Northern Ireland Health and Social Care Research and Development Office and Randox. Prof McAuley has a patent application issued to his institution. Outside of the submitted work Prof McAuley has received fees for consultancy from Bayer, GSK, Boehringer Ingelheim, Eli Lilly and Novartis and SOBI and for being a member of the data monitoring and ethics committee for Vir Biotechnology and Faron studies and as an educational seminar speaker for GSK. The spouse of Prof McAuley has received consultancy fees from Insmed unrelated to this work, and fees for grant panel membership from CIRM. All other authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary tables.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Boyle, A.J., Ferris, P., Bradbury, I. et al. Baseline plasma IL-18 may predict simvastatin treatment response in patients with ARDS: a secondary analysis of the HARP-2 randomised clinical trial. Crit Care 26, 164 (2022). https://doi.org/10.1186/s13054-022-04025-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-022-04025-w