Abstract
Background
The sensitive and accurate diagnosis of nosocomial meningitis and ventriculitis is still a critical problem. This study was designed to explore the diagnostic value of cerebrospinal fluid heparin-binding protein (HBP) in nosocomial meningitis and ventriculitis in comparison with procalcitonin and lactate.
Methods
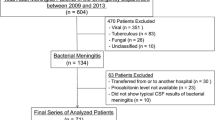
In this observational study, 323 suspected patients were enrolled, of which 42 participants were excluded because they could not be accurately grouped, 131 subjects who were eventually diagnosed with nosocomial meningitis or ventriculitis and 150 patients in whom infection was ultimately ruled out were included in the final analysis. The main results are expressed as medians (interquartile ranges). The Chi-squared test was used to compare the baseline characteristics. The Mann–Whitney U-test was used for group and subgroup analyses. The area under the receiver operating characteristic curve was calculated to describe the diagnostic accuracy of the biomarkers. Spearman's partial correlation was used to analyze associations between the biomarkers. Statistical significance was set when p value < 0.05.
Results
HBP achieved the largest area under the receiver operating characteristic curve, which was 0.99 (95% confidence interval 0.98—1.00) compared with 0.98 (95% confidence interval 0.96—0.99) for lactate and 0.69 (95% confidence interval 0.62—0.75) for procalcitonin. With a cutoff level at 23 ng/mL, HBP achieved a sensitivity of 97%, a specificity of 95%, a positive predictive value of 93% and a negative predictive value of 98%. The levels of HBP presented no significant discrepancy between patients who received previous empiric anti-infective therapy and those who did not (p > 0.05). Higher concentrations of HBP were present in patients with positive microbiological findings (p < 0.05). Levels of HBP positively correlated with polymorphonuclear cell count (Spearman's rho = 0.68, p < 0.01), white blood cell count (Spearman's rho = 0.57, p < 0.01) and lactate (Spearman's rho = 0.34, p < 0.01).
Conclusions
Cerebrospinal fluid heparin-binding protein is a reliable auxiliary diagnostic marker that is preferable over lactate and procalcitonin in identifying nosocomial meningitis and ventriculitis, and it also contributes to solving the diagnostic difficulties caused by empiric antibiotherapy.
Similar content being viewed by others
Introduction
Nosocomial meningitis and ventriculitis in adults mainly results from invasive neurosurgical procedures or head trauma [1]. It remains a life-threatening complication contributing to considerable morbidity [2, 3]. Patients with a drainage device may have an even higher incidence [4,5,6]. The syndrome can lead to severe sequelae and increased mortality [7, 8] and poses a particularly great threat to elderly people [9]. Given the adverse clinical outcomes [10, 11], empiric antibiotic therapy is usually initiated in the absence of bacteriologic findings. Cerebrospinal fluid (CSF) cytochemical parameters, including cell count, glucose, protein and lactate suffer from a lack of specificity [12, 13]. The lack of widely recognized cutoff values for these markers makes their interpretation difficult. Sensitivity for Gram staining is unacceptably low [7, 12, 13]. Culture, the gold standard, has an inherent delay of several days to obtain results. A sensitive and reliable biomarker is therefore required.
Heparin-binding protein (HBP) is rapidly mobilized and released from activated neutrophils in response to infections in the early stage of inflammation [14, 15], which makes it a promising biomarker with emerging roles in the diagnosis of infectious diseases. The protein has demonstrated its superiority over procalcitonin (PCT) and C-reactive protein in early recognition of infections [16, 17]. Similarly, HBP showed more powerful diagnostic capability in distinguishing bacterial meningitis from viral meningitis than CSF cytochemical markers [18,19,20]. However, published results regarding the accuracy of HBP in diagnosing postoperative meningitis and ventriculitis are lacking.
The present study was conducted to assess the value of CSF HBP in identifying meningitis and ventriculitis in patients following neurosurgery compared with CSF lactate and procalcitonin.
Methods
Study design and patient population
This single-center observational study was conducted at Beijing Tiantan Hospital, Capital Medical University, between August 2020 and June 2021 and was approved by the Ethics Committee of the hospital. The hospital is the China National Clinical Research Center for Neurological Diseases and most of the neurosurgical patients admitted are patients with central nervous system tumors. Eligible subjects were patients who were older than 18 years and experienced neurosurgery that involved dura opening. The exclusion criteria were community-acquired meningitis, meningitis or ventriculitis diagnosed in other centers before admission, infections secondary to spinal surgery or surgery that only involved blurring holes or shunts. Patients who received empiric antibiotic therapy before sampling were not excluded. The implementation of glucocorticoids and antimicrobial prophylaxis was integrated into routine treatment in patients following neurosurgery in our center. Patients who stayed in the intensive care unit (ICU) for more than 48 h were defined as critically ill.
Diagnostic criteria
We adopted an adjusted CDC/NHSN definition and specified the cutoffs of white blood cell (WBC) count, protein and glucose in CSF for transparency and reproducibility [21]. Nosocomial meningitis or ventriculitis was confirmed when a patient met criteria 1 or criteria 2 of the definition: 1. Positive cultures of CSF; 2. At least one of these clinical symptoms cannot otherwise be explained by other causes (body temperature > 38 ℃ or headache or meningeal signs or focal neurological impairments) and at least one of the following: 1) white blood cell count > 100 cells/mm3, protein > 50 mg/dL and glucose < 2.5 mmol/L in CSF; 2) positive findings on Gram staining of CSF; 3) positive cultures of blood. External ventricular drainage (EVD)-related infection was defined according to Clinical Practice Guidelines for Healthcare-Associated Ventriculitis and Meningitis from Infectious Diseases Society of America (IDSA)[22].
Data collection
Cerebrospinal fluid was sampled for glucose, protein, cell count, culture, HBP, PCT and lactate analysis in patients suspected to have central nervous system infections following neurosurgery. Patients were enrolled as the infected group when a diagnosis of meningitis or ventriculitis was established according to the criteria listed above. Patients with white blood cells ≤ 100 cells/mm3 and glucose ≥ 2.5 mmol/L were enrolled as the control group. Patients who could not be clearly classified were not included in the final statistical analysis. Data involving demographic characteristics, preexisting medical conditions, surgery descriptions and clinical manifestations were collected.
CSF samples for the determination of HBP and PCT were centrifuged and analyzed using Fluorescent Immunalyzer Model AFS-1000 (Guangzhou Labmis Biotech Co. Ltd, Guangzhou, China) according to the manufacturer's instructions. The analytical sensitivity was 0.05 ng/mL for PCT and 0.01 ng/mL for HBP. CSF samples for cytochemical examination (including CSF lactate) were tested in our center's clinical chemistry laboratories.
Statistical analysis
Given the nonnormality, the main results were expressed as medians (interquartile ranges [IQR]). The Chi-squared test was used to compare the baseline characteristics. The Mann–Whitney U-test was used for group comparisons and subgroup analyses. The area under the receiver operating characteristic curve (AUC) was calculated to describe the diagnostic accuracy of CSF biomarkers. Since previous studies showed positive correlations among WBC, HBP and lactate[19, 20], Spearman's partial correlation was used to analyze the correlations between the biomarkers by controlling the effect of one biomarker and analyzing the correlation between the other two. Statistical significance was set when p value < 0.05. All statistics were analyzed using GraphPad Prism version 8.0 (GraphPad Software, USA) and SPSS version 25.0 (IBM Corporation, USA).
Results
Baseline characteristics
Cerebrospinal fluid was sampled from 323 suspected patients, and 42 were eventually excluded because of the inability to determine the presence or absence of an infection. Analysis was thereby performed on 281 patients, including 131 patients who were diagnosed with meningitis or ventriculitis as the infected group and 150 patients in whom infection was eventually ruled out as the control group. A total of 325 samples were analyzed, including 131 samples from the infected group and 194 samples from the control group.
The baseline characteristics of the two groups are exhaustively described in Table 1. There were no statistical differences in data involving demographic characteristics and previously existing medical conditions. Among all the characteristics related to surgical descriptions, placement of external ventricular drainage device and emergency surgeries were more frequently observed in infected patients (p < 0.01), and the operative time of infected patients was significantly longer than that of the controls (p < 0.05).
The median time to onset of meningitis and ventriculitis was 5 days (IQR 3—7 days) post-neurosurgery. There were 126 patients who established a diagnosis based on abnormal cerebrospinal parameters combined with corresponding clinical manifestations. The other 5 patients had a normal white blood cell count or glucose level and were confirmed to be infected in light of positive cultures in CSF. The causal pathogens included 3 cases of coagulase-negative staphylococci, 1 case of Klebsiella pneumoniae and 1 case of Stenotrophomonas maltophilia.
Isolated organisms
A total of 35 patients were determined to be infected by positive cultures of CSF or blood, containing 28 patients with positive CSF cultures, 1 patient with positive blood culture and 6 patients with both positive cultures. As summarized in Table 2, 34 patients contributed to 41 CSF culture-positive episodes, and 7 patients contributed to 7 blood culture-positive episodes. Overall, Gram-negative bacteria were responsible for most infections, which were isolated from 21 (51%) patients, slightly above 20 (49%) of Gram-positive bacteria. Mixed infections occurred in 7 (20%) of the culture-positive patients. Repeated positive cultures were documented in 16 patients, and each of the other 19 patients showed a positive culture only from one single sample, including 7 episodes of coagulase-negative staphylococci, 4 episodes of Enterococcus spp., 3 episodes of Klebsiella pneumoniae, 3 episodes of Acinetobacter baumannii, 1 episode of Staphylococcus aureus and 1 episode of Raoultella ornithinolytica. The most frequently isolated organism was coagulase-negative staphylococci, followed by Klebsiella pneumoniae and Acinetobacter baumannii. Rare pathogens recorded included Raoultella ornithinolytica, Serratia marcescens, Citrobacter, Providencia stuartii and Alcaligenes faecalis.
Diagnostic accuracy of CSF HBP
All three parameters in CSF presented universal increases in the infected group (p < 0.01) (Fig. 1a–c). CSF HBP increased notably in patients with postoperative meningitis or ventriculitis (median 140 ng/mL [IQR 87—189 ng/mL]) compared to patients in whom central nervous system infection was finally ruled out (median 1.2 ng/mL (IQR 0.7—3.5 ng/mL). (Fig. 1a).
Levels of heparin-binding protein, procalcitonin and lactate in cerebrospinal fluid. The median levels were labeled in the figures. The values were described as medians (interquartile ranges [IQR]) and listed below: a Heparin-binding protein (HBP) were 140 ng/mL (IQR 87—189 ng/mL) in the infected patients versus 1.2 ng/mL (IQR 0.7—3.5 ng/mL) in the control patients. b Procalcitonin (PCT) were 0.09 ng/mL (IQR 0.00—0.23 ng/mL) in the infected patients versus 0.05 ng/mL (IQR 0.00—0.07 ng/mL) in the control patients. c Lactate (Lac) were 6.6 mmol/L (IQR 4.8—10.4 mmol/L) in the infected patients versus 2.2 mmol/L (IQR 1.8—2.7 mmol/L) in the control patients. d HBP were 136 ng/mL (IQR 94—193 ng/mL) in the group with empirical antibiotics versus 144 ng/mL (IQR 86—188 ng/mL) in the group without empirical antibiotics. e PCT were 0.16 ng/mL (IQR 0.07—0.35 ng/mL) in the group with empirical antibiotics versus 0.08 ng/mL (IQR 0.00—0.17 ng/mL) in the group without empirical antibiotics. f Lactate were 7.0 mmol/L (IQR 4.7—12.4 mmol/L) in the group with empirical antibiotics versus 6.5 mmol/L (IQR 4.9—9.8 mmol/L) in the group without empirical antibiotics
The receiver operating characteristic curve (ROC curve) for the discrimination of nosocomial meningitis and ventriculitis indicated that CSF HBP achieved the largest AUC of 0.99 (95% confidence interval [CI], 0.98—1.00), which was higher than the other two biomarkers: 0.98 (95% CI 0.96—0.99) for CSF lactate and 0.69 (95% CI 0.62—0.75) for PCT (Fig. 2).
ROC curves of cerebrospinal fluid biomarkers for diagnosing nosocomial meningitis and ventriculitis. The area under the receiver operating characteristic curve (AUC) was 0.99 (95% CI 0.98—1.00) for heparin-binding protein (HBP), 0.98 (95% CI 0.96—0.99) for lactate (Lac) and 0.69 (95% CI 0.62—0.75) for procalcitonin (PCT)
A cutoff level of CSF HBP at 23 ng/mL identified postoperative meningitis and ventriculitis with a sensitivity of 97%, a specificity of 95%, a positive predictive value of 93% and a negative predictive value of 98%. With a cutoff level at 103 ng/mL, CSF HBP presented a specificity of 100%, but the sensitivity decreased to 69% (Table 3).
The value of CSF HBP in identifying bacterial meningitis and ventriculitis
The infected group (n = 131) was further divided into the culture-positive group (n = 35) and the culture-negative group (n = 96) based on bacterial findings in blood or CSF (Fig. 3a–c). The comparison was also performed on the culture-positive patients (n = 35) and all culture-negative cases (n = 246) (Fig. 3d–f). HBP levels in all culture-positive patients exceeded 23 ng/mL, including the patients who had a negative white blood cell count or glucose level and were confirmed infection by positive culture results, 28 (80%) cases among them had HBP levels above 103 ng/mL. Concentrations of all three parameters in CSF were significantly higher in patients with positive cultures. CSF HBP were 174 ng/mL (IQR 110—204 ng/mL) in the culture-positive group versus 137 ng/mL (IQR 77—184 ng/mL) in the culture-negative group (p < 0.05) and 3.3 ng/mL (IQR 0.9—85.2 ng/mL) in all culture-negative cases (p < 0.05).
Levels of heparin-binding protein, procalcitonin and lactate in cerebrospinal fluid of culture-positive patients. HBP were 174 ng/mL (IQR 110—204 ng/mL) in the culture-positive group versus 137 ng/mL (IQR 77—184 ng/mL) in the culture-negative group (a) and 3.3 ng/mL (IQR 0.9—85.2 ng/mL) in all culture-negative cases (d). CSF PCT were 0.17 ng/mL (IQR 0.00—0.40 ng/mL) in the culture-positive group versus 0.08 ng/mL (IQR 0.00—0.18 ng/mL) in the culture-negative group (b) and 0.05 ng/mL (IQR 0.00—0.08 ng/mL) in all culture-negative patients (e). Lactate were 10.3 mmol/L (IQR 5.6—13.7 mmol/L) in the culture-positive group versus 6.2 mmol/L (IQR 4.7—9.1 mmol/L) in the culture-negative group (c) and 2.7 mmol/L (IQR 2.0—4.8 mmol/L) in all culture-negative patients (f)
CSF PCT presented a low sensitivity in the diagnosis of nosocomial meningitis and ventriculitis. Forty-three (33%) patients had PCT levels of less than 0.05 ng/mL, and 62 (47%) patients had PCT levels of less than 0.09 ng/mL (the cutoff level) among the 131 infected patients. Even among the 35 culture-positive patients, 9 (26%) had CSF PCT levels lower than 0.05 ng/mL.
Diagnostic accuracy of CSF HBP in patients who received empiric antibiotics
Empiric antimicrobial therapy prior to sampling was documented in 45 patients (34%), including 20 patients who were treated for more than 48 h. There was no statistical significance in the concentrations of CSF HBP and lactate between the patients who received empiric antibacterial therapy (n = 45) and those who did not (n = 86) (p > 0.05, Fig. 1d, f), while the levels of CSF PCT in the group with empiric antibiotics were significantly higher than those in the group without (Fig. 1e). The characteristics of patients with and without empiric antibiotics were compared to look for possible causative factors for this discrepancy. There were 19 (42%) critically ill patients and 19 (42%) culture-positive patients in the group with empiric antibiotic use versus 19 (22%) critically ill cases and 16 (19%) culture-positive cases among patients without antibiotic pretreatment. The median time to onset of infection was 7 days (IQR 4—10 days) post-neurosurgery in patients who were pretreated versus 4 days (IQR 2—6 days) post-neurosurgery in those who were not pretreated. The levels of the biomarkers were further compared between critically ill patients with and without empiric antibiotics, noncritically ill patients with and without empiric antibiotic use respectively. Concentrations of PCT showed no statistical significance between the two pairs of subgroups, p = 0.15 and p = 0.17 respectively.
Here, we observed that 43 (96%) cases had HBP concentrations above 23 ng/mL among the 45 patients who were treated with empiric anti-infective therapy, whereas the PCT levels were below 0.05 ng/mL in 9 (20%) patients and less than 0.09 ng/mL in 18 patients (40%).
Diagnostic accuracy of CSF HBP in EVD-related infections
As shown in Table 1, 96 patients with EVD devices were enrolled, 57 (44% of all the infected patients and 59% of patients with EVD devices) were diagnosed with meningitis or ventriculitis, and in 39 (26% of the total control patients and 41% of patients with EVD devices), central nervous system infection was finally ruled out. The median levels of the markers were: 154 ng/mL (IQR 110—192 ng/mL) for HBP in patients with EVD-related infections versus 1.6 ng/mL (IQR 0.7—3.9 ng/mL) in those without (p < 0.01), 0.09 ng/mL (IQR 0.00—0.27 ng/mL) for PCT in patients with EVD-related infections versus 0.05 ng/mL (IQR 0.00—0.07 ng/mL) in those without (p < 0.01) and 8.2 mmol/L (IQR 4.7—12.5 mmol/L) for lactate in patients with EVD-related infections versus 2.2 mmol/L (IQR 1.8—2.8 mmol/L) in those without (p < 0.01). The AUCs for the diagnosis of EVD-related infections were 0.99 (95% CI 0.98—1.00) for HBP, 0.97 (95% CI 0.95—1.00) for lactate and 0.72 (95% CI 0.62—0.82) for PCT. HBP achieved a sensitivity of 100% and a specificity of 96% with a cutoff value at 21 ng/mL. (Table 3).
Correlation between CSF biomarkers
After adjustment by using Spearman's partial correlation, there was still a strong association between HBP and WBC (Spearman's rho = 0.57, p < 0.01), as well as HBP and polymorphonuclear cell (PMN) (Spearman's rho = 0.68, p < 0.01). But the correlation between WBC and lactate (Spearman's rho = 0.38, p < 0.01), as well as HBP and lactate (Spearman's rho = 0.34, p < 0.01), was relatively weak. (Table 4).
Discussion
In the present study, we investigated the diagnostic accuracy of cerebrospinal fluid heparin-binding protein in patients with nosocomial meningitis or ventriculitis compared to procalcitonin and lactate and performed further subgroup analysis based on whether these patients had positive culture findings and whether empiric antibiotics were used. Our study highlights the discriminatory value of CSF HBP and contributes to solving the diagnostic difficulties caused by empiric antibacterial treatment for the diagnosis of nosocomial meningitis and ventriculitis.
The protein demonstrated superior diagnostic capability in distinguishing patients with postoperative meningitis or ventriculitis as shown by the largest AUC in comparison with CSF PCT and lactate. Similar results were observed in the diagnosis of EVD-related infections. Published studies revealed that CSF lactate had a higher diagnostic accuracy with a cutoff level at 4 mmol/L compared to conventional CSF markers, including glucose, protein and white blood cell count [23, 24]. However, its diagnostic value may be limited when CSF samples are mixed with blood [25], which is common in patients following neurosurgery, and normal levels of lactate may not rule out all infected patients [26]. Our study justified that CSF HBP better recognized postoperative meningitis and ventriculitis than lactate, but with modest differences and overlapping confidence intervals. HBP presented a higher sensitivity and negative predictive value but a lower specificity and positive predictive value than lactate, while lactate showed the opposite results. This indicates that the measurement of CSF HBP may be more helpful in identifying infection, with a low risk of missed diagnosis, and elevated lactate values are more indicative of an existing infection, with a low risk of misdiagnosis. Detecting the two markers simultaneously may be more helpful in this setting.
Contrary to previous studies [19, 20], our research showed significant positive correlation between HBP and CSF WBC and an even more notable correlation between HBP and CSF PMN. While the correlation between HBP and lactate was weak. Previous studies did not consider the mutual influence between the markers, which likely explains these differences. Compared with WBC and lactate, WBC and HBP presented a stronger positive correlation after adjusting. This revealed a potential risk of overestimating the diagnostic performance of HBP, since HBP is generated from activated neutrophils and we adopted leukocytosis as one of the diagnostic criteria.
The findings that CSF HBP increased in all culture-positive cases indicate that HBP could have a large clinical use in early identification of patients with a bacterial infection, especially in those with otherwise negative cytochemistry. Clinicians should be cautious when neurosurgical patients have a normal CSF leukocyte count and CSF glucose level but an elevated HBP level in CSF, they should be assumed to have bacterial meningitis until a negative CSF culture is obtained. Our results are in agreement with previous clinical investigations on community-acquired meningitis [19, 20]. Stored in mature neutrophils [14], HBP can be mobilized and released from neutrophils immediately under the stimulation of bacterial pathogens [15, 27]. Adam Linder and coworkers found that the levels of HBP most likely reflected the cell count of functional neutrophils, other than the absolute number of white blood cells [19]. This may partly explain the striking elevation of CSF HBP in patients with positive bacteriological results and a negative white blood cell count.
It should also be mentioned that there is a considerable overlap in HBP concentrations between the culture-positive and culture-negative cases in the infected group, which indicates that HBP may not be able to fully discriminate bacterial meningitis from culture-negative meningitis, and there may be subjects with chemical meningitis in the culture-negative group. The problem is hard to address since the CDC/NHSN definition allows for diagnosis of culture-negative meningitis.
As the sensitivity of culture and Gram staining is low, patients without microbiological confirmation are clinically more common. Most of the infected patients were diagnosed based on clinical symptoms and CSF cytochemistry abnormalities at enrollment in our study, which is more in line with clinical practice, but this may not help to identify causal pathogens. In fact, infections were verified largely depending on subsequent bacteriological results and responsiveness to empiric antibacterial therapy. We excluded from the study patients who met only one or two of the following criteria: decreased CSF glucose, pleocytosis and increased protein. However, these patients may also have symptoms such as low fever or headache, and clinicians tend to initiate antibacterial treatment. It was difficult to define whether such patients were infected or not and were thereby excluded. Therefore, a risk of misclassification may exist.
The IDSA guideline defines that positive cultures with normal CSF cytochemical parameters and no suspicious clinical manifestations as contamination (or colonization), that positive cultures with leukocytosis and clinical symptoms as infection [22]. There was a possibility that the bacteria grew were not the causal pathogens, especially in patients who had only one positive culture. But the effectiveness of targeted antibacterial treatment against these pathogens may help to identify whether the isolated bacteria were responsible. In our study, all culture-positive patients presented clinical manifestations of suspected infections, and most of them also had CSF abnormalities except for 5 patients who had positive cultures and a normal CSF leukocyte count or glucose level. Three of the 5 culture-positive patients had a normal CSF cell count and all isolated bacteria were coagulase-negative staphylococci. Thus, a possibility of erroneously judging contamination (or colonization) as infection may exist in these 3 patients.
CSF PCT presented limited identifiable value and poor sensitivity for the diagnosis of nosocomial meningitis and ventriculitis compared with the other parameters we tested. Our findings are comparable with figures evaluated in previous observations [28, 29]. Wen Jiang and colleagues found that CSF PCT aided in the discrimination of Gram-negative bacterial meningitis [30]. However, our findings are not contradictory to theirs. In fact, the median levels of CSF PCT in patients with nosocomial meningitis or ventriculitis did increase with meaningful statistical difference, and its concentrations in patients with positive cultures were also significantly higher than those without, but not all infected patients contributed to the elevation of PCT values. PCT concentrations in a substantial portion of patients with meningitis or ventriculitis were recorded as negative in our study, and even a quarter of culture-positive patients had PCT levels below the lower limit of detection. Therefore, a significant increase in CSF PCT may indicate infections, but normal PCT levels cannot exclude all infected patients, suggesting that PCT may be more of a marker that implies an already existing infection rather than predicting infections in the specific setting of neurosurgery.
Suspicion of central nervous system infection following neurosurgery usually warrants empiric antibiotic prescription. However, this may blunt the changes of CSF markers, reduce the sensitivity of CSF microbiological testing and mask the typical clinical manifestations [31, 32]. Here, we observed that most of the infected patients who were already on antibiotics prior to sampling had elevated HBP concentrations at the time of diagnosis (exceeding 23 ng/mL), including those who were treated for more than 48 h, suggesting that HBP retains a high diagnostic ability in patients who received antibiotic pretreatment. How antibiotic pretreatment modifies these parameters in CSF requires further study.
Unexpectedly, our study suggested that patients who received empiric antimicrobial chemotherapy had significantly higher CSF PCT levels than those who did not. Comparison of the basic characteristics of the two groups showed that the portion of critically ill cases and culture-positive patients was greater and the median time to onset of infection was longer in the group given empiric antibiotics. Given these findings, we speculate that the reasons may be as follows. Mostly synthesized by the parafollicular C cells of the thyroid gland and derived largely from plasma penetration, CSF PCT may increase slowly and reach peak values at a relatively late stage of meningitis and ventriculitis. At the same time, patients who were given antibiotic intervention in advance were less likely to present typical clinical manifestations in the early period. Thus, the time from surgery to establish the diagnosis of meningitis and ventriculitis will be prolonged. The overlap of these two effects was probably the major reason that patients given empiric anti-infective therapy had a higher PCT value. Moreover, the discrepancy in the proportion of critically ill patients between the two subgroups may also be responsible. Given the catastrophic consequences that delayed antibiotics may incur, critically ill patients are more likely to initiate antibacterial treatment when suspected to have central nervous system infections, despite insufficient evidence. The PCT levels of critically ill patients may be higher than those of mild patients [33]. This made patients with empiric antibiotic pretreatment appear to have a higher PCT level. Studies on CSF PCT have mostly been of low-quality until recently, and our hypothesis needs to be confirmed by further research.
Further subgroup analysis revealed that regardless of whether critically ill or not, all three biomarkers were not significantly different between patients who received or did not receive empiric antibiotherapy. These results correspond to the findings of previous prospective studies [19, 28, 31]. However, CSF PCT is of questionable value for its poor sensitivity in diagnosing nosocomial meningitis and ventriculitis in patients with empiric antibiotic use. These findings highlight that the ability of CSF HBP to diagnose postoperative meningitis and ventriculitis will not decrease in the context of antimicrobial chemotherapy preceding diagnosis, and it may be a useful marker that contributes to resolving the diagnostic dilemmas in these patients.
The novelty of this research was that we assessed the efficacy of CSF HBP in diagnosing nosocomial meningitis and ventriculitis while previous studies were mainly designed for community-acquired meningitis [18,19,20]. Moreover, our research enrolled patients given anti-infective therapy prior to diagnosis, which is more consistent with the actual clinical situation, while previous studies mostly excluded these patients. Additionally, our study enrolled a larger sample size.
The limitations of the present study may be as follows. Patients admitted due to tumor surgery predominate in our subjects, which can increase patient homogeneity but may lead to selection bias as well, and we should be cautious when extrapolating our findings to patients with diseases other than tumors. In addition, definitions of postoperative meningitis adopted in different studies differ significantly, which makes the range of patient populations recruited vary. Our research used an internationally recognized definition to minimize the difference, which may have made strict choices for enrolled patients inadvertently.
Conclusions
Cerebrospinal fluid heparin-binding protein is a reliable auxiliary diagnostic marker outperforming lactate and procalcitonin in the identification of nosocomial meningitis and ventriculitis, and it contributes to solving the diagnostic difficulties caused by empirical antibacterial treatment.
Availability of data and materials
All data generated or analyzed during this study are included in this published article. The datasets generated or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- HBP:
-
Heparin-binding protein
- PCT:
-
Procalcitonin
- Lac:
-
Lactate
- CSF:
-
Cerebrospinal fluid
- IQR:
-
Interquartile range
- CI:
-
Confidence interval
- GCS score:
-
Glasgow Coma Scale score
- ROC curve:
-
Receiver operating characteristic curve
- AUC:
-
The area under receiver operating characteristic curve
- PMN:
-
Polymorphonuclear cell
- WBC:
-
White blood cell
- EVD-related infections:
-
External ventricular drainage-related infections
- IDSA:
-
Infectious Diseases Society of America
- ICU:
-
The intensive care unit
References
van de Beek D, Drake J, Tunkel A. Nosocomial bacterial meningitis. N Engl J Med. 2010;362(2):146–54.
Korinek A, Baugnon T, Golmard J, van Effenterre R, Coriat P, Puybasset L. Risk factors for adult nosocomial meningitis after craniotomy: role of antibiotic prophylaxis. Neurosurgery. 2008: 532–9.
McClelland S, Hall W. Postoperative central nervous system infection: incidence and associated factors in 2111 neurosurgical procedures. Clin Infect Dis. 2007;45(1):55–9.
Dorresteijn K, Jellema K, van de Beek D, Brouwer M. Factors and measures predicting external CSF drain-associated ventriculitis: a review and meta-analysis. Neurology. 2019;93(22):964–72.
Citerio G, Signorini L, Bronco A, Vargiolu A, Rota M, Latronico N. External ventricular and lumbar drain device infections in ICU patients: a prospective multicenter Italian study. Crit Care Med. 2015;43(8):1630–7.
Jamjoom A, Joannides A, Poon M, Chari A, Zaben M, Abdulla M, et al. Prospective, multicentre study of external ventricular drainage-related infections in the UK and Ireland. J Neurol Neurosurg Psychiatry. 2018;89(2):120–6.
Srihawan C, Castelblanco R, Salazar L, Wootton S, Aguilera E, Ostrosky-Zeichner L, et al. Clinical characteristics and predictors of adverse outcome in adult and pediatric patients with healthcare-associated ventriculitis and meningitis. Open Forum Infect Dis. 2016;3(2):ofw077.
Neuberger A, Shofty B, Bishop B, Naffaa M, Binawi T, Babich T, et al. Risk factors associated with death or neurological deterioration among patients with Gram-negative postneurosurgical meningitis. Clin Microbiol Infect. 2016;22(6):573.e1-4.
Srihawan C, Habib O, Salazar L, Hasbun R. Healthcare-associated meningitis or ventriculitis in older adults. J Am Geriatr Soc. 2017;65(12):2646–50.
Shi Y, Zheng G, Qian L, Qsman R, Li G, Zhang G. Longitudinal analysis of risk factors for clinical outcomes of meningitis/encephalitis in post-neurosurgical patients: a comparative cohort study during 2014–2019. Infect Drug Resist. 2020;13:2161–70.
Sharma R, Goda R, Borkar S, Katiyar V, Agarwal S, Kumar A, et al. Outcome following postneurosurgical Acinetobacter meningitis: an institutional experience of 72 cases. Neurosurg Focus. 2019;47(2):E8.
Schade R, Schinkel J, Roelandse F, Geskus R, Visser L, van Dijk J, et al. Lack of value of routine analysis of cerebrospinal fluid for prediction and diagnosis of external drainage-related bacterial meningitis. J Neurosurg. 2006;104(1):101–8.
Forgacs P, Geyer C, Freidberg S. Characterization of chemical meningitis after neurological surgery. Clin Infect Dis. 2001;32(2):179–85.
Tapper H, Karlsson A, Mörgelin M, Flodgaard H, Herwald H. Secretion of heparin-binding protein from human neutrophils is determined by its localization in azurophilic granules and secretory vesicles. Blood. 2002;99(5):1785–93.
Pereira H, Erdem I, Pohl J, Spitznagel J. Synthetic bactericidal peptide based on CAP37: a 37-kDa human neutrophil granule-associated cationic antimicrobial protein chemotactic for monocytes. Proc Natl Acad Sci U S A. 1993;90(10):4733–7.
Wu Y, Yo C, Hsu W, Qian F, Wu B, Dou Q, et al. Accuracy of heparin-binding protein in diagnosing sepsis: a systematic review and meta-analysis. Crit Care Med. 2021;49(1):e80–90.
Linder A, Arnold R, Boyd J, Zindovic M, Zindovic I, Lange A, et al. Heparin-binding protein measurement improves the prediction of severe infection with organ dysfunction in the emergency department. Crit Care Med. 2015;43(11):2378–86.
Ren D, Wu D, Liu F, Jiao S, Wu Y. Diagnostic value of heparin-binding protein in the cerebrospinal fluid for purulent meningitis in children. Braz J Med Biol Res. 2021; 54(11): e11295.
Linder A, Akesson P, Brink M, Studahl M, Björck L, Christensson B. Heparin-binding protein: a diagnostic marker of acute bacterial meningitis. Crit Care Med. 2011;39(4):812–7.
Kandil M, Khalil G, El-Attar E, Shehata G, Hassan S. Accuracy of heparin-binding protein: as a new marker in prediction of acute bacterial meningitis. Braz J Microbiol. 2018; 213–9.
CDC/NHSN Surveillance Definitions for Specific Types of Infections. January 2014. Available at: http://www.socinorte.com/wp-content/uploads/2014/06/17pscNosInfDef_current.pdf. Accessed 17 Aug 2021.
Tunkel A, Hasbun R, Bhimraj A, Byers K, Kaplan S, Scheld W, et al. 2017 Infectious Diseases Society of America's clinical practice guidelines for healthcare-associated ventriculitis and meningitis. Clin Infect Dis. 2017;64(6):e34–65.
Huy N, Thao N, Diep D, Kikuchi M, Zamora J, Hirayama K. Cerebrospinal fluid lactate concentration to distinguish bacterial from aseptic meningitis: a systemic review and meta-analysis. Crit Care. 2010;14(6):R240.
Leib S, Boscacci R, Gratzl O, Zimmerli W. Predictive value of cerebrospinal fluid (CSF) lactate level versus CSF/blood glucose ratio for the diagnosis of bacterial meningitis following neurosurgery. Clin Infect Dis. 1999;29(1):69–74.
Böer K, Pfister W, Kiehntopf M. Lactic acid is of low predictive value for the diagnosis of bacterial infection in ventricular cerebrospinal fluid samples containing residual blood. Clin Chem Lab Med. 2010;48(12):1777–80.
Conen A, Walti L, Merlo A, Fluckiger U, Battegay M, Trampuz A. Characteristics and treatment outcome of cerebrospinal fluid shunt-associated infections in adults: a retrospective analysis over an 11-year period. Clin Infect Dis. 2008;47(1):73–82.
Snäll J, Linnér A, Uhlmann J, Siemens N, Ibold H, Janos M, et al. Differential neutrophil responses to bacterial stimuli: Streptococcal strains are potent inducers of heparin-binding protein and resistin-release. Sci Rep. 2016;6:21288.
Li W, Sun X, Yuan F, Gao Q, Ma Y, Jiang Y, et al. Diagnostic accuracy of cerebrospinal fluid procalcitonin in bacterial meningitis patients with empiric antibiotic pretreatment. J Clin Microbiol. 2017;55(4):1193–204.
Li Y, Zhang G, Ma R, Du Y, Zhang L, Li Fea. The diagnostic value of cerebrospinal fluids procalcitonin and lactate for the differential diagnosis of post-neurosurgical bacterial meningitis and aseptic meningitis. Clin Biochem. 2015; 48: 50–4.
Li W, Yuan F, Sun X, Zhao Z, Zhang Y, Jiang W. Cerebrospinal fluid procalcitonin predicts Gram-negative bacterial meningitis in patients with empiric antibiotic pretreatment. Crit Care. 2019;23(1):21.
Adhikari S, Gauchan E, Bk G, Rao KS. Effect of antibiotic pretreatment on cerebrospinal fluid profiles of children with acute bacterial meningitis. Nepal J Med Sci. 2013;2(2):135–9.
Rogers T, Sok K, Erickson T, Aguilera E, Wootton S, Murray K, et al. Impact of antibiotic therapy in the microbiological yield of healthcare-associated ventriculitis and meningitis. Open Forum Infect Dis. 2019;6(3):ofz050.
Park B, Kim S, Park S, Kim J, Shin K, Ha S, et al. Procalcitonin as a potential predicting factor for prognosis in bacterial meningitis. J Clin Neurosci. 2017;36:129–33.
Acknowledgements
We thank Guojun Zhang, Department of Clinical Diagnosis, Laboratory of Beijing Tiantan Hospital, Capital Medical University, for assistance with data collection. We thank Chongqing Zearly Bio-Tech Co. LTD for assistance with technical support.
Funding
This work was supported by 'Beijing Municipal Administration of Hospitals—Yangfan Project' (Grant Number ZYLX202109).
Author information
Authors and Affiliations
Contributions
GZ S and YY K conceived and designed this study. YY K, Y Y and JW M collected data. YY K and Y Y designed and performed the statistical analyses. YY K and JW M wrote the first draft of the manuscript. GZ S reviewed and modified the final manuscript. All authors read, critically reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in the present study were in accordance with the Declaration of Helsinki and the study was reviewed and approved by Ethics Committee of Beijing Tiantan Hospital, Capital Medical University. Informed consent to participate in the study was obtained from participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kong, Y., Ye, Y., Ma, J. et al. Accuracy of heparin-binding protein for the diagnosis of nosocomial meningitis and ventriculitis. Crit Care 26, 56 (2022). https://doi.org/10.1186/s13054-022-03929-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-022-03929-x