Abstract
Background
Intravenous vitamin C administration in septic shock may have a sparing effect on vasopressor requirements, and vitamin C’s enzyme cofactor functions provide a mechanistic rationale. Our study aimed to determine the effect of intravenous vitamin C administration on vasopressor requirements and other outcomes in patients with septic shock.
Methods
This was a double-blind, randomised placebo-controlled trial in 40 patients with septic shock who were randomised (1:1) to receive intravenous vitamin C (at a dose of 25 mg/kg of body weight every 6 h) or placebo (intravenous 5% dextrose) for up to 96 h, or until death or discharge. The primary outcome was intravenous vasopressor requirements (dose and duration), and secondary outcomes included Sequential Organ Failure Assessment (SOFA) scores, intensive care unit (ICU) and hospital length of stay, and mortality. In addition, blood samples were collected to determine vitamin C kinetics and inflammatory marker concentrations.
Results
Median plasma vitamin C concentrations were deficient at baseline (9.2 [4.4, 12] µmol/L) and increased to 408 (227, 560) µmol/L following 72 h of intervention. The mean duration of intravenous vasopressor infusion in the vitamin C group was 48 (95% CI 35–62) hours and in the placebo group was 54 (95% CI 41–62) hours (p = 0.52). The dose of vasopressor delivered over time was comparable between the two groups, as were SOFA scores (p > 0.05). The median ICU length of stay in the intervention group was 3.8 (2.2, 9.8) days versus 7.1 (3.1, 20) days in the placebo group (p = 0.12). The median hospital length of stay for the vitamin C group was 18 (11, 35) days versus 22 (10, 52) days for the placebo group (p = 0.65). Mortality was comparable between the two groups (p > 0.05). Of the inflammatory markers, neutrophil counts were elevated in the vitamin C group relative to placebo by 72 h (p = 0.01). C-reactive protein and myeloperoxidase concentrations were elevated at baseline, however, the two groups were comparable over time (p > 0.05).
Conclusions
Our pilot study indicated that intravenous vitamin C did not provide significant decreases in the mean dose or duration of vasopressor infusion. Further research that takes into account the potential impact of intervention timing, dose and duration, and location of trial, may provide more definitive evidence.
Trial registration
ACTRN12617001184369 (11/8/2017).
Similar content being viewed by others
Background
Sepsis is a life-threatening condition comprising organ dysfunction due to a dysregulated host response to infection [1]. Sepsis is a growing global health issue, with an estimated 49 million cases worldwide resulting in 11 million deaths [2]. As such, sepsis is responsible for 20% of annual global deaths. Septic shock is a more severe clinical presentation characterised by profound circulatory, cellular, and metabolic abnormalities and is associated with mortality rates greater than 40% [1]. Sepsis is managed through empiric intravenous antibiotic therapy, source control of infection, fluid resuscitation, and vasopressor administration. Additionally, organ support is provided via mechanical ventilation and renal replacement therapy [3]. Intravenous norepinephrine is usually the first-choice vasopressor to increase the mean arterial blood pressure ≥ 65 mmHg for patients with sepsis who remain hypotensive after adequate fluid resuscitation. At times, intravenous vasopressin is also commenced to aid mean arterial pressure target or decrease norepinephrine dosage.
Since the publication of several early trials indicating possible beneficial effects of intravenous vitamin C in critically ill patients with sepsis and septic shock, as monotherapy [4, 5] and in combination with thiamine and hydrocortisone [6], there has been an upsurge in clinical trials investigating its potential benefits in these patients [7]. Various trials administering intravenous vitamin C to patients with sepsis and septic shock have indicated decreased vasopressor requirements [5, 8,9,10], improved sequential organ failure assessment (SOFA) scores [4, 9], decreased ICU length of stay [8, 11], and decreased mortality [5, 9, 11]. However, some trials showed no effects of vitamin C intervention on SOFA scores [11], ICU length of stay [5], or mortality [8, 10], so the evidence is currently mixed with regard to these outcomes. Since the emergence of severe coronavirus disease in 2019 (COVID-19), research into the potential treatments of sepsis, a major complication of severe COVID-19, has become even more important. Early trials have indicated some potentially beneficial effects of intravenous vitamin C in severe COVID-19 [12,13,14]. In addition, the World Health Organisation has highlighted vitamin C as a potential adjunctive therapy with biologic plausibility for patients with critical COVID-19 [15].
Vitamin C has pleiotropic mechanisms of action that could plausibly contribute to its beneficial effects in sepsis and severe COVID-19, such as antioxidant, anti-inflammatory, antithrombotic, and immuno-modulatory functions, including roles in leukocyte and platelet functions, and endothelial and epithelial cell integrity [16, 17]. Patients with sepsis and septic shock have low vitamin C status and a high prevalence of deficiency [18, 19], and these critically ill patients require gram doses of intravenous vitamin C to replete their plasma status [20, 21]. In 2015 we proposed that vitamin C’s role as a cofactor for the endogenous synthesis of vasopressors (norepinephrine and vasopressin) may provide a rationale for its administration in septic shock as these vasopressors are routinely administered to critically ill patients to try and increase their blood pressure [22]. Shortly afterwards, Zabet et al. [5] published a paper supporting this premise, reporting a decrease in both dose and duration of noradrenaline administration in patients with septic shock who received intravenous vitamin C at a dose of 100 mg/kg body weight per day. We initiated a pilot double-blind, randomised-controlled trial to ascertain if these findings were reproducible.
Methods
Patient enrolment
This was a double-blind, randomised placebo-controlled trial of intravenous vitamin C infusion in patients with septic shock at Christchurch Hospital ICU, Christchurch, New Zealand. Ethical approval for the study was obtained from the New Zealand Northern A Health and Disability Ethics Committee (16NTA238). The study was registered with the Australia and New Zealand Clinical Trial Registry (ACTRN12617001184369). Proxy consent was obtained from the treating physician in consultation with the next of kin when patient consent was not immediately possible. Written informed consent from the patients was sought as soon as they had sufficiently recovered.
Patients with septic shock were screened on admission to the ICU. They were enrolled into the study if they met the following criteria: receiving intravenous antimicrobial therapy specifically for infection, receiving ≥ 5 µg/minute (≥ 0.06 µg/kg/min) noradrenaline or adrenaline, evidence of organ dysfunction, i.e. Sequential Organ Failure Assessment (SOFA) score ≥ 2 for at least one of respiratory function (ratio of partial pressure of arterial oxygen and fraction of inspired oxygen [PaO2/FiO2] < 300), liver function (bilirubin > 33 μmol/L), coagulation (platelets < 100 × 103/μL) and renal function (creatinine > 171 μmol/L). Exclusion criteria included: aged < 18 years, consent could not be obtained, patient not expected to survive 24 h, known glucose-6-phosphate dehydrogenase (G6PD) deficiency, known or suspected pregnancy or breastfeeding.
The primary outcome was the patients’ vasopressor requirements expressed as mean hourly dose and duration of noradrenaline equivalents administered. Sample size calculations were derived from the means and SDs of the noradrenaline dose and duration data from the Zabet et al. RCT [5], which was the only published data available at the time. This indicated that a total of 36 participants (18 per group) would have 95% power to detect a difference in the mean norepinephrine dose over three days of 6.5 (SD 6) µg/min or a difference of 22 (SD 22) hours norepinephrine duration with 5% type 1 error. Therefore, a total of 40 participants were enrolled to account for an anticipated 10% loss due to withdrawal of consent to continue.
Administration of intervention
A computer-generated random block size randomisation sequence was prepared in advance by the study statistician (JW). This was used to randomise the participants (1:1 ratio) to the vitamin C intervention group or placebo control group. Blinding of the treatment allocation was through sequentially numbered opaque sealed envelopes opened by the research nurses who also prepared the intervention. Finally, the intervention was dispensed to clinical staff blinded to which study arm the participants were allocated.
Patients in the active intervention group received intravenous vitamin C (ASCOR L500, McGuff Pharmaceuticals, Santa Ana, USA) in 5% dextrose at a dose of 25 mg/kg body weight every 6 h. This was made up into a 50 ml syringe and administered over 30 min via syringe pump into a peripheral or central venous line. The total dose of 100 mg/kg/day was administered for up to 96 h (duration of the study), or until death or ICU discharge if earlier. Patients in the placebo control group received intravenous 5% dextrose in water made up in identical 50 mL syringes swap to delivered and administered the same as for the intervention group.
Collection of clinical data
Data was collected and managed using REDCap (Research Electronic Data Capture), a secure, web-based data collection and storage tool hosted at the University of Otago, New Zealand. Data was de-identified using a patient study code. The following demographic and clinical data were collected at baseline: age, gender, weight, ethnicity, primary diagnosis contributing to sepsis, comorbidities, ICU severity scores (SAPS, APACHE III, and SOFA), vasopressor dose, vital signs and oxygenation parameters. In addition, the following clinical data were collected daily: vasopressor dose delivered over time (units/min), SOFA scores (predicts ICU mortality), vital signs, oxygenation parameters, and at follow-up: length of ICU and hospital stay, and ICU and hospital mortality.
Adverse events, other than those considered part of the study inclusion process and/or study outcome assessments (e.g. organ failure, death; unless believed to be due to the intervention), were recorded as per the Common Terminology Criteria for Adverse Events (CTCAE, version 4.0).
Collection and analysis of blood samples
Blood samples were collected daily for routine haematological and biochemical parameters (e.g. white cell counts and differentials, lactate, creatinine, C-reactive protein), and were analysed by Canterbury Health Laboratories, an International Accreditation New Zealand (IANZ) laboratory. A blood sample (4 ml LiHeparin) was also collected daily before the first vitamin C infusion. This was then processed rapidly at 4 °C for subsequent storage of acidified supernatants and plasma aliquots at − 80 °C for batch analysis of vitamin C by HPLC with electrochemical detection, as described previously [23], and for analysis of plasma myeloperoxidase using a commercial sandwich ELISA kit (AbCam, Cambridge, UK).
Statistical analyses
The baseline characteristics were summarised descriptively and tabulated by treatment group. Plasma vitamin C concentrations were summarised by treatment group and day. The patients’ hourly vasopressor requirements post randomisation (the primary outcome of interest) were calculated as noradrenaline dose equivalent units/min (equivalent to 0.1 µg/kg/min noradrenaline) by summing noradrenaline (µg/kg/min), adrenaline (µg/kg/min), and 2.5*vasopressin (units/min) according to the formula by Goradia et al. [24]. Each patients’ total vasopressor requirements were then summarised as mean dose delivered per hour over the 96-h study period or until death if this occurred prior, and total duration of delivery. Differences in mean vasopressor dose by treatment group were assessed by unpaired t-test. Time until event data (including duration of vasopressor delivery, discharge from ICU, and discharge from hospital) was assessed using Kaplan–Meier plots and log-rank tests censoring for death. Differences in duration of vasopressor delivery over the study period (0–96 h) were assessed by comparing the restricted mean survival time (equivalent to the area under the Kaplan Meier curve) between the study groups [25]. SOFA scores were measured at 0, 24, 48 and 96 h post randomisation; patients who were discharged were given a score of 0 (the minimum) and those who died a score of 24 (the maximum). Linear models were used to estimate the change in SOFA scores over time, and the difference in change over time between groups. All statistical analyses were performed using R (4.1.1, R Core Team 2021, Vienna, Austria) [26].
Results
Participant characteristics at baseline
Of the 65 patients assessed for eligibility, 40 were randomised to either placebo or intravenous vitamin C (Fig. 1). The participants were predominantly male (67%), aged 68 (61, 75) years and weighed 80 (72, 98) kg (Table 1). They comprised 85% European, 10% Māori/Pasifika peoples and 5% Asian/other ethnicities. The predominant source of sepsis was abdominal (35%), followed by pulmonary (23%), skin/soft tissue and blood (18% each; Table 1). The ICU severity scores (SAPS, APACHE III and SOFA) and other physiological and biochemical parameters for the whole cohort and the treatment subgroups are also shown in Table 1. The median (Q1, Q3) time from admission to randomisation was 17 (12, 25) hours and from randomisation to first treatment was 45 (33, 73) minutes.
Vitamin C kinetics
The plasma vitamin C status of the study participants was deficient at baseline, with a median (Q1, Q3) of 9.2 (4.4, 11.4) µmol/L. Intravenous vitamin C was administered at a dose of 25 mg/kg six-hourly. The median weight of the participants was 80 kg, resulting in median administration of 2 g vitamin C six-hourly (or 8 g/day). Blood samples were collected immediately before the first intervention infusion of each day, i.e., on average, six hours post the last infusion. Within 24 h, there was a significant increase in plasma vitamin C concentrations in the intervention group from 10 (4, 13) µmol/L to 264 (159, 391) µmol/L and up to 408 (227, 560) µmol/L by 72 h (Fig. 2). In contrast, the placebo group decreased from 8.2 (4.7, 11) µmol/L to 4.4 (3.1, 8.8) µmol/L over the 72 h.
Plasma vitamin C concentrations for patients with septic shock who received intravenous vitamin C relative to placebo. Intravenous vitamin C was administered at a dose of 25 mg/kg six-hourly, and blood samples were collected daily to analyse vitamin C concentrations by HPLC. Box plots show median values with 25th and 75th percentiles as boundaries and whiskers indicate range; circles indicate mean values and 95% CI
One patient with severe renal dysfunction (oliguria—urine output of 253 [197, 339] ml/day, serum creatinine of 656 (592, 806) µmol/L and estimated glomerular filtration rate of 5 [4, 7] ml/min/1.73 m2), had elevated plasma vitamin C concentrations (952 [643–1095] µmol/L). This was likely due to an attenuated ability of the kidneys to clear the infused doses. No adverse events were reported in association with these elevated vitamin C concentrations.
Effect of intervention on vasopressor requirements and organ failure
Noradrenaline and other vasopressors are used to titrate blood pressure to a target mean arterial pressure of typically 65 mmHg. Vasopressor administration is decreased when the mean arterial pressure target is being met. The mean dose rate of vasopressor administered in the vitamin C group was 0.99 units/min (SD = 1.15) and in the placebo group was 0.71 units/min (SD = 0.60), a mean difference of 0.28 units/min (95% CI − 0.31 to 0.87, p = 0.35; Fig. 3a). The mean duration of vasopressor administration in the vitamin C group was 48 (95% CI 35–62) hours and in the placebo group was 54 (41, 62) hours, with a between group difference of − 6 h (95% CI − 25 to 13, p = 0.54) hours (Fig. 3b). The use of steroids could influence the dose and duration of vasopressor administration in septic shock, however, we did not observed any significant differences in the proportion of people receiving intravenous hydrocortisone between the two groups over time (p > 0.05). Mean SOFA scores decreased over time by an estimated 0.73 units per 24 h, but there was no evidence of a difference between treatment groups (p = 0.20; see Additional file 1: Figure S2). At 96 h post randomisation the mean (SD) SOFA score in the vitamin C group was 6.7 (8.3) and in the placebo group was 5.5 (7.0), an estimated difference of 1.2 (95% CI − 3.8 to 6.1, p = 0.64).
Dose and duration of intravenous vasopressors delivered to patients with septic shock by treatment group. a Dot plot of mean vasopressor dose (units/min) delivered over the four-day study period (96 h) or until death by treatment group. Filled circles represent mean dose for each individual patient, black diamond with vertical line represent group means with 95% CIs. b Kaplan Meier plot of time from randomisation until cessation of vasopressor therapy by treatment groups. There was no significant difference between the patients who received intravenous vitamin C and those who received the placebo in mean dose (p = 0.35) nor duration (p = 0.64) of vasopressor administration. See Additional file 1: Figure S1 for the individual data
Effect of intervention on length of stay and mortality
The median ICU length of stay in the intervention group was 3.8 (2.2, 9.8) days versus 7.1 (3.1, 20) days in the placebo group (p = 0.12, censoring for death), a difference of − 3.3 days (Fig. 4). Median hospital length of stay in the intervention group was 18 (11, 35) days versus 22 (10, 52) days in the placebo group (p = 0.65, censoring for death), a difference of -4 days. Of the total cohort, 33% (intervention = 6, placebo = 7) of the cohort had died by 30 days and 38% (intervention = 8, placebo = 7) by 90 days; 35% (intervention = 7, placebo = 7) died in hospital. There was no difference in mortality between the two groups (p > 0.05).
Kaplan–Meier plot for ICU length of stay of the study participants. Lines (bands) indicate the percentage of patients (95% CIs) still in ICU by time in days since study randomisation. Crosses indicate participants censored for death. There was no significant difference between the intervention and placebo groups (p = 0.12, log rank test)
Effect of intervention on leukocytes and markers of inflammation
Leukocyte counts, particularly neutrophil counts, were elevated at baseline (13 [10, 18] × 109/L). By 72 h the neutrophil counts were higher in the vitamin C group than the placebo group (20 [15, 24] × 109/L vs 9 [6, 15] × 109/L, p = 0.01; see Additional file 1: Figure S3). Plasma concentrations of the neutrophil enzyme myeloperoxidase were also elevated at baseline (181 [155, 247] ng/mL); the concentrations did not change significantly throughout the study, nor was there a significant difference between the two treatment groups (p > 0.05; see Additional file 1: Figure S4). Plasma concentrations of C-reactive protein, a marker of inflammation, were elevated at baseline but decreased significantly during the study, from 277 (201, 384) mg/L to 167 (94, 210) mg/L (p < 0.0001). There was no significant difference between the two treatment groups (p > 0.05; see Additional file 1: Figure S5).
Adverse events
Only one adverse event (gastrointestinal bleed) was reported; this was not related to the intervention as the participant was in the placebo group.
Discussion
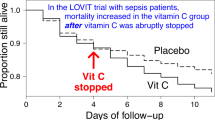
We carried out a pilot RCT to ascertain if intravenous vitamin C administration to patients with septic shock would decrease their vasopressor requirements relative to placebo. Overall, we did not observe a significant difference in dose or duration of total vasopressor (noradrenaline, adrenaline and vasopressin) administration between the two groups over the duration of our study. This is in contrast to the Zabet et al. RCT [5], which had reported a significant decrease in noradrenaline dose and a 22-h decrease in the duration of noradrenaline administration (mean of 50 vs 72 h; p = 0.007) in their cohort of septic patients treated with a comparable dose of intravenous vitamin C (100 mg/kg/day). Two other trials administered intravenous vitamin C at a dose of 6 g/day and also reported a significant decrease in duration of vasopressors (55 vs 156 h, p = 0.001, and 26 vs 44 h, p < 0.05) [8, 9]. Another trial administered 60 mg/kg/day vitamin C as a continuous infusion to critically ill patients with pneumonia and reported a decrease in vasopressor use from 82 to 55 h (p = 0.003) [10]. Further RCTs that have used vitamin C in combination with hydrocortisone and/or thiamine have also reported improvements in vasopressor requirements [27,28,29]. It is interesting to note that all seven trials were carried out in low-middle income countries (Iran, Egypt and India). A review of global vitamin C status and prevalence of deficiency indicated that low-middle income populations tend to have lower vitamin C status and a higher prevalence of deficiency than high-income populations [30]. Thus, vitamin C intervention may be more effective in countries whose populations are likely to be already chronically insufficient in vitamin C prior to the acute deficiency induced by severe sepsis.
In our study, we observed a non-significant trend towards a shorter ICU length of stay of − 3.3 days in the vitamin C group (3.8 vs 7.1 days, p = 0.12) and a non-significant decrease in hospital length of stay of − 4 days (18 vs 22 days, p = 0.65). Recent meta-analyses have indicated that vitamin C administration to critically ill patients may decrease ICU length of stay [31, 32]. The median cost per ICU stay in Australia and New Zealand is > $4,000 per day, with an average length of stay of 10 days for septic patients (a total of > $40,000 per ICU stay) [33, 34]. Thus, a decrease in ICU length of stay of several days would positively impact the economic burden of septic shock on the healthcare system.
Administration of intravenous vitamin C at a dose of 25 mg/kg q 6 hourly to the septic patients (equating to 2 g q 6 hourly) resulted in a significant increase in median plasma vitamin C concentrations from deficient values (9.2 µmol/L) to 264 µmol/L within 24 h and up to 408 µmol/L by 72 h. Other studies have reported comparable plasma vitamin C concentrations for doses of 1.5 g q 6 hourly, 12.5–50 mg/kg q 6 hourly, and 1–5 g q 12 hourly [4, 21, 35]. Elevated vitamin C concentrations (952 [643–1095] µmol/L) were observed in one patient with severe renal dysfunction due to an attenuated ability to clear the intravenous doses. However, no adverse events related to the vitamin C infusion were reported. Nevertheless, elevated vitamin C concentrations can interfere with some point-of-care-glucose monitors resulting in spurious values and potential for overly aggressive insulin administration in some cases [36].
Markers of inflammation (e.g. C-reactive protein, myeloperoxidase) were elevated in the patients at baseline. However, there were no significant differences between the two groups over time. We did observe a significant increase in neutrophil counts in the vitamin C group relative to placebo by 72 h (20 vs 9 × 109/L, p = 0.01). Neutrophils are a primary innate immune defence against invading pathogens and are typically elevated during sepsis (reference range: 1.9–7.5 × 109/L). Although our observation may be an artefact of fewer patients in the vitamin C group relative to the placebo group at this time point (n = 9 vs n = 16), there are also mechanistic rationales for this finding. Despite the higher neutrophil counts in the vitamin C group, there were no significant differences in plasma concentrations of the neutrophil enzyme myeloperoxidase between the two groups. This may indicate decreased necrotic cell death of the neutrophils in the vitamin C arm. We, and others, have previously shown that vitamin C decreases NETosis, a form of neutrophil necrotic cell death [37,38,39]. Cell-free DNA, a marker of necrotic cell death, has been detected in patients with sepsis and is decreased in those treated with intravenous vitamin C [40, 41]. An early RCT in septic surgical patients has also indicated decreased neutrophil apoptotic cell death in patients treated with low dose intravenous vitamin C [42]. Thus, vitamin C may be decreasing necrotic and apoptotic cell death and thereby increasing the lifespan of neutrophils in septic patients.
There are several limitations of this study. First, the size of the study was likely too small to detect the clinical outcomes. The sample size for the primary outcome of vasopressor requirements (dose and duration) was determined from the Iranian Zabet et al. trial [5]. However, a subsequent meta-analysis of the effects of vitamin C on atrial fibrillation has indicated that trials carried out in Iran gave overly positive results compared with trials carried out in the US [43]. This may be due to the populations of low-middle income countries tending to have lower vitamin C status and a higher prevalence of deficiency than those from high-income countries [30]. Thus, higher participant numbers may be required to detect differences in cohorts from high-income countries who are not chronically insufficient in vitamin C. Another limitation may be the dose of vitamin C administered. At the time of ethics submission (2016), only two small vitamin C and sepsis RCTs had been published, the Fowler et al. trial (n = 24), which had administered 50 and 200 mg/kg/day vitamin C [4], and the Zabet et al. trial (n = 28) which had administered 100 mg/kg/day vitamin C [5]. Because fewer patients had been treated with the higher dose of vitamin C, the ethics committee asked that we halve our vitamin C dose to 100 mg/kg/day due to safety concerns, despite evidence in other diseases states indicating tenfold higher doses being safe [44]. Subsequent studies using vitamin C doses of 200 mg/kg/day and up to 25 g/day have shown potential effects on mortality in critically ill patients and an excellent safety profile [11, 12]. Of note, higher vitamin C doses may be required in septic patients due to potential downregulation of cellular vitamin C transporters in response to inflammatory mediators, thereby potentially attenuating cellular uptake of infused vitamin C [45]. A further limitation was the length of time between ICU admission and initiation of intravenous vitamin C administration (median of ~ 18 h). Sepsis is a very time-sensitive condition, with earlier intervention being associated with better patient outcomes [46]. A retrospective study of time sensitive mortality difference with vitamin C combination therapy indicated a significant decrease in mortality in participants who received the intervention within six hours of sepsis presentation relative to those who received it after more than six hours [47]. Furthermore, the duration of vitamin C administration is an important consideration for long-term clinical outcomes [48], with intervention for five or more days showing greater benefit [49]. Half of the intervention group in our trial did not receive the entire four days of intravenous vitamin C. Previous research has indicated that cessation of vitamin C infusions after 2–4 days can result in some patients reverting to hypovitaminosis C concentrations [11, 21]. Thus, overall, it appears that our dosing regimen may have been ‘too little, too late’ to see clinical benefits.
Conclusions
In contrast to the Zabet et al. study [5], our pilot study did not show statistically significant decreases in dose or duration of vasopressor infusion. However, larger studies that take into account the intervention timing, dose and duration limitations described above, as well as the potential impact of country of trial, may provide more definitive evidence.
Availability of data and materials
The datasets generated during the current study are available from the corresponding author upon reasonable request for meta-analyses.
Abbreviations
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- ICU:
-
Intensive care unit
- SAPS:
-
Simplified Acute Physiology Score
- SOFA:
-
Sequential Organ Failure Assessment
References
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–10.
Rudd KE, Johnson SC, Agesa KM, Shackelford KA, Tsoi D, Kievlan DR, Colombara DV, Ikuta KS, Kissoon N, Finfer S, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the Global Burden of Disease Study. Lancet. 2020;395(10219):200–11.
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, Kumar A, Sevransky JE, Sprung CL, Nunnally ME, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Crit Care Med. 2017;45(3):486–552.
Fowler AA, Syed AA, Knowlson S, Sculthorpe R, Farthing D, DeWilde C, Farthing CA, Larus TL, Martin E, Brophy DF, Gupta S, Fisher BJ, Natarajan R. Phase I safety trial of intravenous ascorbic acid in patients with severe sepsis. J Transl Med. 2014;12:32.
Zabet MH, Mohammadi M, Ramezani M, Khalili H. Effect of high-dose ascorbic acid on vasopressor’s requirement in septic shock. J Res Pharm Pract. 2016;5(2):94–100.
Marik PE, Khangoora V, Rivera R, Hooper MH, Catravas J. Hydrocortisone, vitamin C, and thiamine for the treatment of severe sepsis and septic shock: a retrospective before-after study. Chest. 2017;151(6):1229–38.
Carr AC. Vitamin C administration in the critically ill: a summary of recent meta-analyses. Crit Care. 2019;23(1):265.
Nabil Habib T, Ahmed I. Early adjuvant intravenous vitamin C treatment in septic shock may resolve the vasopressor dependence. Int J Microbiol Adv Immunol. 2017;05(1):77–81.
Lv SJ, Zhang GH, Xia JM, Yu H, Zhao F. Early use of high-dose vitamin C is beneficial in treatment of sepsis. Ir J Med Sci. 2020.
Mahmoodpoor A, Shadvar K, Sanaie S, Hadipoor MR, Pourmoghaddam MA, Saghaleini SH. Effect of Vitamin C on mortality of critically ill patients with severe pneumonia in intensive care unit: a preliminary study. BMC Infect Dis. 2021;21(1):616.
Fowler AA 3rd, Truwit JD, Hite RD, Morris PE, DeWilde C, Priday A, Fisher B, Thacker LR 2nd, Natarajan R, Brophy DF, et al. Effect of vitamin C infusion on organ failure and biomarkers of inflammation and vascular injury in patients with sepsis and severe acute respiratory failure: The CITRIS-ALI randomized clinical trial. JAMA. 2019;322(13):1261–70.
Zhang J, Rao X, Li Y, Zhu Y, Liu F, Guo G, Luo G, Meng Z, De Backer D, Xiang H, Peng Z. Pilot trial of high-dose vitamin C in critically ill COVID-19 patients. Ann Intensive Care. 2021;11(1):5.
Kumari P, Dembra S, Dembra P, Bhawna F, Gul A, Ali B, Sohail H, Kumar B, Memon MK, Rizwan A. The role of vitamin C as adjuvant therapy in COVID-19. Cureus J Med Sci. 2020;12(11):e11779.
JamaliMoghadamSiahkali S, Zarezade B, Koolaji S, SeyedAlinaghi S, Zendehdel A, Tabarestani M, Sekhavati Moghadam E, Abbasian L, Dehghan Manshadi SA, Salehi M, et al. Safety and effectiveness of high-dose vitamin C in patients with COVID-19: a randomized open-label clinical trial. Eur J Med Res. 2021;26(1):20.
World Health Organization. A coordinated global research roadmap: 2019 novel coronavirus. Geneva: World Health Organization; 2020.
Kashiouris MG, L'Heureux M, Cable CA, Fisher BJ, Leichtle SW, Fowler AA. The emerging role of vitamin C as a treatment for sepsis. Nutrients. 2020;12(2).
Carr AC, Rowe S. The emerging role of vitamin C in the prevention and treatment of COVID-19. Nutrients. 2020;12(11).
Carr AC, Rosengrave PC, Bayer S, Chambers S, Mehrtens J, Shaw GM. Hypovitaminosis C and vitamin C deficiency in critically ill patients despite recommended enteral and parenteral intakes. Crit Care. 2017;21:300.
Hwang SY, Park JE, Jo IJ, Kim S, Chung SP, Kong T, Shin J, Lee HJ, You KM, Jo YH, et al. Combination therapy of vitamin C and thiamine for septic shock in a multicentre, double-blind, randomized, controlled study (ATESS): study protocol for a randomized controlled trial. Trials. 2019;20(1):420.
Long CL, Maull KI, Krishnan RS, Laws HL, Geiger JW, Borghesi L, Franks W, Lawson TC, Sauberlich HE. Ascorbic acid dynamics in the seriously ill and injured. J Surg Res. 2003;109(2):144–8.
de Grooth HJ, Manubulu-Choo WP, Zandvliet AS, Spoelstra-de Man AME, Girbes AR, Swart EL, Oudemans-van Straaten HM. Vitamin-C pharmacokinetics in critically ill patients: a randomized trial of four intravenous regimens. Chest. 2018;153(6):1368–77.
Carr AC, Shaw GM, Fowler AA, Natarajan R. Ascorbate-dependent vasopressor synthesis: a rationale for vitamin C administration in severe sepsis and septic shock? Crit Care. 2015;19:e418.
Carr AC, Pullar JM, Moran S, Vissers MC. Bioavailability of vitamin C from kiwifruit in non-smoking males: determination of “healthy” and “optimal” intakes. J Nutr Sci. 2012;1:e14.
Goradia S, Sardaneh AA, Narayan SW, Penm J, Patanwala AE. Vasopressor dose equivalence: a scoping review and suggested formula. J Crit Care. 2021;61:233–40.
Royston P, Parmar MK. Restricted mean survival time: an alternative to the hazard ratio for the design and analysis of randomized trials with a time-to-event outcome. BMC Med Res Methodol. 2013;13:152.
R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2021.
Balakrishnan M, Gandhi H, Shah K, Pandya H, Patel R, Keshwani S, Yadav N. Hydrocortisone, vitamin C and thiamine for the treatment of sepsis and septic shock following cardiac surgery. Indian J Anaesth. 2018;62:934–9.
Wani SJ, Mufti SA, Jan RA, Shah SU, Qadri SM, Khan UH, Bagdadi F, Mehfooz N, Koul PA. Combination of vitamin C, thiamine and hydrocortisone added to standard treatment in the management of sepsis: results from an open label randomised controlled clinical trial and a review of the literature. Infect Dis (Lond, Engl). 2020;52(4):271–8.
Karimpour H, Bahrami A, Amini S, Rezaei M, Amini-Saman J, Shahbazi F. Effects of a high dose of vitamin C along with thiamine in critically-ill patients with septic shock: a preliminary study. J Pharm Res Int. 2019;29(5):1–7.
Rowe S, Carr AC. Global vitamin C status and prevalence of deficiency: a cause for concern? Nutrients. 2020;12(2008).
Hemila H, Chalker E. Vitamin C can shorten the length of stay in the ICU: a meta-analysis. Nutrients. 2019;11(4).
Xing X, Xu M, Yang L, Zhang W, Niu X, Gao D. The efficacy of intravenous vitamin C in critically ill patients: a meta-analysis of randomized controlled trials. Clin Nutr. 2021;40(5):2630–9.
Hicks P, Huckson S, Fenney E, Leggett I, Pilcher D, Litton E. The financial cost of intensive care in Australia: a multicentre registry study. Med J Aust. 2019;211(7):324–5.
Thompson K, Taylor C, Jan S, Li Q, Hammond N, Myburgh J, Saxena M, Venkatesh B, Finfer S. Health-related outcomes of critically ill patients with and without sepsis. Intensive Care Med. 2018;44(8):1249–57.
Hudson EP, Collie JT, Fujii T, Luethi N, Udy AA, Doherty S, Eastwood G, Yanase F, Naorungroj T, Bitker L, Abdelhamid YA, Greaves RF, Deane AM, Bellomo R. Pharmacokinetic data support 6-hourly dosing of intravenous vitamin C to critically ill patients with septic shock. Crit Care Resusc. 2019;21(4):236–42.
Rosengrave PC, Wohlrab C, Spencer E, Williman J, Shaw G, Carr AC. Effect of intravenous vitamin C on arterial blood gas analyser and ACCU-CHEK point-of-care glucose monitoring in critically ill patients. Crit Care Resusc. 2022; in press.
Bozonet SM, Carr AC. The role of physiological vitamin C concentrations on key functions of neutrophils isolated from healthy individuals. Nutrients. 2019;11(6).
Sae-Khow K, Tachaboon S, Wright HL, Edwards SW, Srisawat N, Leelahavanichkul A, Chiewchengchol D. Defective neutrophil function in patients with sepsis is mostly restored by ex vivo ascorbate incubation. J Inflamm Res. 2020;13:263–74.
Mohammed BM, Fisher BJ, Kraskauskas D, Farkas D, Brophy DF, Fowler AA, Natarajan R. Vitamin C: a novel regulator of neutrophil extracellular trap formation. Nutrients. 2013;5(8):3131–51.
Natarajan R, Fisher BJ, Syed AA, Fowler AA. Impact of intravenous ascorbic acid infusion on novel biomarkers in patients with severe sepsis. J Pulm Respir Med. 2014;4(6).
Qiao X, Fisher B, Kashiouris MG, Truwit JD, Hite RD, Morris PE, Martin GS, Fowler AA. Effects of high dose intravenous vitamin C (IVC) on plasma cell-free DNA levels in patients with sepsis-associated ARDS. Am J Respir Crit Care Med. 2019;201:A2100.
Ferron-Celma I, Mansilla A, Hassan L, Garcia-Navarro A, Comino AM, Bueno P, Ferron JA. Effect of vitamin C administration on neutrophil apoptosis in septic patients after abdominal surgery. J Surg Res. 2009;153(2):224–30.
Hemilä H, Suonsyrjä T. Vitamin C for preventing atrial fibrillation in high risk patients: a systematic review and meta-analysis. BMC Cardiovasc Disord. 2017;17(1):49.
Carr AC, Cook J. Intravenous vitamin C for cancer therapy—identifying the current gaps in our knowledge. Front Physiol. 2018;9:1182.
Carr AC. Is “Mega-dose” IV vitamin C required for septic and critical coronavirus disease 2019 patients? Crit Care Med. 2021;49(4):e477–8.
Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, Suppes R, Feinstein D, Zanotti S, Taiberg L, Gurka D, Kumar A, Cheang M. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34(6):1589–96.
Long MT, Frommelt MA, Ries MP, Murray M, Osman F, Krause BM, Kory P. Early hydrocortisone, ascorbate and thiamine therapy for severe septic shock. Crit Care Shock. 2020;23(1):23–34.
Carr AC. Duration of intravenous vitamin C therapy is a critical consideration. Crit Care Resuscitation. 2019;21(3):220–1.
Jung SY, Lee MT, Baek MS, Kim WY. Vitamin C for ≥ 5 days is associated with decreased hospital mortality in sepsis subgroups: a nationwide cohort study. Crit Care. 2022;26(1):3.
Acknowledgements
We thank the study participants for their generous contribution to the study and the Christchurch Hospital ICU nurses for administering the interventions and collecting patient data and blood samples. Thanks also to Eveline van Leeuwen and Reuben Springer for helping to process the blood samples.
Funding
Health Research Council of New Zealand Sir Charles Hercus Health Research Fellowship (#16/037 to AC) and Canterbury Medical Research Foundation project grant (#16/01 to AC). The funding bodies had no role in the design of the study; in the collection, analysis or interpretation of data; or in writing the manuscript.
Author information
Authors and Affiliations
Contributions
AC and GS conceived and designed the study, PR coordinated the study, JM, SM, TD, KH, AM and GS screened and enrolled patients, ES carried out sample analyses, JW analysed the data, AC wrote the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures involving human participants were approved by the New Zealand Northern A Health and Disability Ethics Committee (#16NTA238). Proxy consent was obtained from the treating physician in consultation with the next of kin when patient consent was not immediately possible. Written informed consent from the patients was sought as soon as they had sufficiently recovered.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Supplemental material: Figure S1–S5.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rosengrave, P., Spencer, E., Williman, J. et al. Intravenous vitamin C administration to patients with septic shock: a pilot randomised controlled trial. Crit Care 26, 26 (2022). https://doi.org/10.1186/s13054-022-03900-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-022-03900-w