Abstract
Background
Diarrhea is frequent in patients in intensive care units (ICU) and is associated with discomfort and complications and may increase the length of stay and nursing workload.
Methods
This was a prospective, double-blind, randomized, controlled single-center pilot study to assess the incidence and frequency of diarrhea and the respective effects of a modified enteral diet (intervention: Peptamen® AF, rich in proteins, medium chain triglycerides and fish oil) compared to a standard diet (control: Isosource® Energy) in 90 randomized adult patients (intervention, n = 46; control, n = 44) with an ICU stay ≥5 days and tube feeding ≥3 days. Tube feeding was initiated within 72 h of ICU admission and continued up to 10 days. The caloric goal was adjusted to needs by indirect calorimetry. Gastrointestinal function, nutritional intake, and nursing workload were recorded. Follow-up was until 28 days after randomization.
Results
Median age was 63.3 (interquartile range (IQR) 51.0–73.2) years and Simplified Acute Physiology Score (SAPS) II was 61.0 (IQR 47.8–74). Time to reach caloric goal (intervention: 2.2 (0.8–3.7) days (median, IQR); control: 2.0 (1.3–2.7) days; p = 0.16), length of time on study nutrition (intervention: 5.0 (3.6–6.4) days; control: 7.0 (5.3–8.7) days; p = 0.26), and calorie intake (intervention: 18.0 (12.5–20.9) kcal/kg/day; control 19.7 (17.3–23.1) kcal/kg/day; p = 0.08) did not differ between groups, with a higher protein intake for Peptamen® group (1.13 (0.78–1.31) g/kg/day vs 0.80 (0.70–0.94); p < 0.001). No difference in diarrhea incidence (intervention group: 29 (64%); control group: 31 (70%); p = 0.652), use of fecal collectors (23 (51%) vs. 24 (55%); p = 0.83), or diarrhea-free days (161 (64%) vs 196 (68%); p = 0.65) was found. Nursing workload and cost for diarrhea care were not different between the groups. In a post-hoc analysis, adjusted for treatment group, age, sex, and SAPS II score, diarrhea was associated with length of mechanical ventilation (9.5 (6.0–13.1) vs. 3.9 (3.2–4.6) days; p = 0.006) and length of ICU stay (11.0 (8.9–13.1) vs. 5.0 (3.8–6.2) days; p = 0.001).
Conclusions
In this pilot study, we found a high incidence of diarrhea, which was not attenuated by Peptamen® AF. Patients with diarrhea stayed longer in the ICU.
Trial registration
ClinicalTrials.gov identifier, NCT01581957. Registered on 18 April 2012.
Similar content being viewed by others
Background
Gastrointestinal dysfunction is common in critically ill patients with prolonged intensive care unit (ICU) stay [1], and diarrhea is one of the leading clinical symptoms [2,3,5]. The causes of diarrhea are multifactorial and include recent abdominal surgery, infection, decreased gastrointestinal perfusion, and antibiotics. In a prospective study in patients during the first 2 weeks of ICU stay, the combination of enteral nutrition covering >60% of the energy target and antibiotics or antifungal drugs increased the incidence of diarrhea [6].
The inability to absorb sufficient amounts of nutrition can increase muscle wasting and prolong recovery from critical illness [7]. Attempts to reduce diarrhea using fiber-enriched enteral formulas have been disappointing in ICU patients [8–11]. Diarrhea, independent of its reason, may predispose patients to a risk of malnutrition and development of decubitus ulcers. It causes substantial discomfort for patients and is likely to add to the workload of nurses and the cost of care.
There is a wide range of diarrhea incidence reported in recent randomized clinical studies (14% [6], 19–23% [12], 22–26% [13], 26–29% [14], and 33–92% [15]), partly related to patient population and varying diarrhea definition. Reports on diarrhea-related costs are scarce.
We performed a pilot study to test the effect of a new enteral formula on the frequency of diarrhea and gastrointestinal tolerance, and on all diarrhea-related costs in ICU long-stayers. The purpose of the study was also to gain information for the design of a future confirmatory trial. The tested formula has a high energy density in order to reduce the necessary feeding volume, enzymatically hydrolyzed whey protein to improve absorption [16], and its lipid fraction contains 50% medium chain triglycerides and fish oil due to their possible benefits in inflammatory states [17].
Methods
This study was approved by the local Ethics Committee (KEK Bern, 060/12) and is registered at clinicalTrials.gov (NCT01581957). Informed consent was obtained from each patient or from a close relative. The study was designed as a prospective, double-blind, randomized, controlled single-center pilot study, where Peptamen® AF was compared in a 1:1 allocation to a standard formula (Isosource® Energy) with the same amount of caloric density. The allocation sequence was generated by an independent statistician not involved in the final analysis of the trial. It was based on computer generated random numbers in randomly varying blocks of four and six using the statistical software package Stata (StataCorp LP, College Station, TX, USA). Randomization was stratified by the presence or absence of diarrhea at the time of randomization. The study was conducted from 8 January 2013 (first patient included) until 29 August 2014 (last follow-up).
Objectives
The primary objective was to evaluate diarrhea and other gastrointestinal symptoms in critically ill patients with prolonged ICU stay who are either fed with Peptamen® AF or Isosource® Energy. Secondary objectives were determination of inflammatory status, organ function, workload and cost, and safety of patients fed with either one of the two products. Accordingly, the primary outcomes were diarrhea-free days and number of diarrhea events per day during enteral nutrition administration in the ICU. Diarrhea was assessed according to the definition by Whelan et al. [18] from start of enteral nutrition until the end of enteral feeding or ICU discharge, whichever came first. Whelan assigned scores to three categories of stool amounts (<100 g, 100–200 g, >200 g) and four categories of stool consistencies (hard and formed, soft and formed, loose and unformed, liquid), ranging from 1 (<100 g, hard and formed) to 12 (>200 g, liquid). Diarrhea is defined as a score of 15 or more during 1 day. A list of the secondary outcomes is provided in Additional file 1.
Inclusion and exclusion criteria
Inclusion criteria were medical and surgical ICU patients ≥18 years with an expected ICU stay of ≥5 days and anticipated tube feeding for ≥3 days. Exclusion criteria were the presence of contraindications for enteral nutrition or placement of an enteral feeding tube, patients receiving enteral nutrition with ≥75% of caloric goal already administered, restrictions in full intestinal support, parenteral nutrition of any kind unless due to enteral nutrition intolerance, a history of allergy or intolerance to study product components (test or control product), nonfunctional gastrointestinal tract, limited care, and participation in another interventional trial during the last month.
Test products
The active product, Peptamen® AF, is a liquid tube-feeding calorie-dense formula (1.5 Kcal/ml) not containing fibers. It has a high whey protein concentration delivering 25% of the energy by proteins, 39% by lipids, and 36% by carbohydrates.
The control product, Isosource® Energy, is a liquid tube-feeding, calorie-dense formula (1.5 Kcal/ml) without fibers, delivering 16% of the energy by protein, 35% by lipids, and 50% by carbohydrates. The exact composition of both formulas is indicated in Additional file 1 (Table S6).
Feeding protocol
Patients in the trial received tube feeding initiated 0 to 72 h post-ICU admission. They received either Peptamen® AF or Isosource® Energy. The caloric target was 25 Kcal/kg/day body weight (taken from medical records or relatives, or estimated by medical staff) to be reached on the third day after enteral nutrition was started. The quantity was subsequently adjusted to caloric estimates by indirect calorimetry to be performed whenever possible during the first night after study start, 3 days afterwards, at end of nutrition with the study product, and 2 days afterwards if still intubated. The total formula intake was monitored via the Patient Data Management System (PDMS) as described below. Tube feeding could be interrupted for clinical reasons (cardiovascular instability, invasive interventions, reanimation, severe diarrhea, high gastric residual volumes or vomiting, and transportation). The study period on the product lasted a maximum of 10 days. Afterwards, patients were switched to standard enteral nutrition if still required. According to internal nursing guidelines, a fecal collector was administered when diarrhea was present or more than three stool passages occurred per shift, but always at the discretion of the treating physician who also evaluated the presence of contraindications (leuco- or severe thrombopenia, rectal obstruction). Standard physiological parameters were continuously recorded in a PDMS (Centricity Critical Care Clinisoft®; General Electrics, Helsinki, Finland). Study-related additional parameters (diarrhea, material costs based on Additional file 1 (Table S5), and nursing workload) were recorded in the same PDMS using specifically designed case report forms which were later exported to a database provided by the local clinical trial unit (CTU). Due to logistic reasons at the bedside, the nurses did not always record consistency and the number of stools exactly at the same time. In such cases, the closest entries for consistency and stool number were merged off-line. In patients with fecal collectors where the content of the collector was measured only once per day, the frequency and number of individual stool events could not be assessed. Patient-days with fecal collectors were therefore omitted for the characterization of the stool events and the calculation of the Whelan score (Additional file 1: Table S1).
Patients were followed-up daily until 2 days after the study end. An additional follow-up visit was conducted 28 days after randomization. There was independent on-site monitoring provided by the CTU to ensure Good Clinical Practice (GCP) compliance and data quality. Adverse and serious adverse events were recorded according to GCP Guidelines and are reported in Additional file 1 (Table S7–S9).
Statistics
Prior to the current pilot study, we did not formally assess and quantify diarrhea in our patients. Due to the pilot character of the study, a sample size calculation was therefore not performed. The active group and the control group both had a target sample size of n = 45. All randomized patients were included in the primary analysis in the arm to which they were randomized regardless of any protocol violations (intention-to-treat principle). If a fecal collector was administered, the number of stool events could not be counted. As a crude estimate of stool events in these patients, the amount of stool in the fecal collector was divided by the average amount of stool per event from all patient days without the fecal collector in the respective group.
Patient characteristics are presented as median and interquartile range (IQR) and number and percentage of patients for continuous and categorical data, respectively. The two primary outcomes were analyzed by negative binomial (number of diarrhea events) and mixed effects logistic regression (diarrhea-free days) with the treatment group as covariate. For a sensitivity analysis, the regression models were adjusted for baseline diarrhea or for antibiotics prescription, respectively. Secondary endpoints were analyzed by Wilcoxon rank-sum tests (non-normal continuous outcomes), Student t tests (normal continuous outcomes), Fisher’s exact test (binary outcomes), Poisson regressions with robust standard errors (count outcomes), and Cox proportional hazard models (time-to-event outcomes). The treatment effect is presented as incidence rate ratio (count outcomes), risk ratio (binary outcomes), mean difference (normal continuous outcomes), Hodges–Lehmann median differences (non-normal continuous outcomes), or hazard ratio (HR; time-to-event outcomes) with 95% confidence interval (CI). Line listings and descriptive statistics were used to analyze adverse event data. In a post-hoc analysis, patients that did or did not experience diarrhea during the course of enteral nutrition were compared. The analysis was adjusted for treatment group, age, sex, and Simplified Acute Physiology Score (SAPS) II admission diagnosis using negative binomial (number of diarrhea events), Poisson regression with robust standard errors (count outcomes), median regression (continuous outcomes) or Cox regression (time-to-event outcomes). Results are reported as incidence rate ratio, median difference, and HR with 95% CI, respectively.
Results
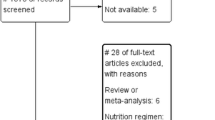
Ninety patients were included in the study (intervention group 46, controls 44; Fig. 1). Median age was 63.3 (IQR 51.0–73.2) years and SAPS II was 61.0 (IQR 47.8–74). Five (11%; Peptamen® AF group) and four (9%; Isosource® Energy group) patients, respectively, had diarrhea at study inclusion. Gastric residual volumes did not differ between groups at study inclusion (Table 1). Seventy-three (81%) patients received antibiotics during the course of the study, while 65 (72%) were on antibiotics at study inclusion.
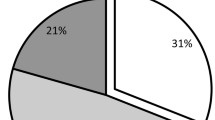
The time taken to reach the caloric goal and the length of time on study nutrition were not different between groups (Peptamen® AF: 2.2 (0.8–3.7) days and 5.0 (3.6–6.4) days; Isosource® Energy: 2.0 (1.3–2.7) days and 7.0 (5.3–8.7) days; p = 0.16 and p = 0.26, respectively; Table 2). Sixty patients experienced diarrhea during their ICU stay (Peptamen® AF group: 29 (64%); Isosource® Energy group: 31 (70%); p = 0.652). Twenty three (51%) of the Peptamen® group and 24 (55%) patients of the Isosource® group received a fecal collector during the study period because of diarrhea (p = 0.83; Table 3). The numbers of diarrhea-free days were 161 (64%) and 196 (68%) for Peptamen® AF and Isosource® Energy, respectively (p = 0.65). Stool events per patient ICU days were comparable between groups (Table 4 and Fig. 2 and Additional file 1: Table S1 and S2). In each group, 15 patients received prokinetic drugs (metoclopramide and/or erythromycin). The numbers did also not differ in the per protocol analysis and if only patients without fecal collectors were analyzed. Likewise, the results did not differ between groups when adjusted for baseline diarrhea or for antibiotics prescription (Fig. 2). The material costs were 3.09 (IQR 0.00–7.58) CHF/day/patient. Respective costs per day for patients with diarrhea were CHF 6.31 (0.00–17.11). The median nursing workload in all patients was 15.0 (0.0–27.0) min/day/patient, and for days with diarrhea 40.0 (17.5–74.4) min/patient and for days with fecal collector 20.0 (6.4–52.5) min/patient. Nursing workload and cost for diarrhea care were similar in both groups (Table 3 and Additional file 1: Table S3). Therapeutic intervention scoring system (TISS-76) per day were 46.0 (40.1–54.0) and 46.3 (42.2–50.3) (p = 0.83).
Some small numerical differences in secondary endpoints between the two groups were identified, but without an overall trend specific to one product, and without clinical relevance (Tables 2, 3, 5, and 6). Both groups received a similar percentage of prescribed calories (median 85% (IQR 71%–95%) for Peptamen®, 90% (84%–96%) for Isosource®®; p = 0.07) and reached the caloric goal in equal time (2.2 (0.8–3.7) days for Peptamen®, 2.0 (1.3–2.7) days for Isosource®®; p = 0.16; Fig. 3). Median caloric intake did not differ between groups (Peptamen® AF: 18.0 (12.5–20.9) kcal/kg/day; Isosource® Energy: 19.7 (17.3–23.1) kcal/kg/day; p = 0.08), with a higher protein intake for the Peptamen® group (1.13 (0.78–1.31) g/kg/day vs 0.80 (0.70–0.94) g/kg/day; p < 0.001). Differences were found for the accumulated caloric deficit during enteral nutrition/day, which yielded −410 (−984 to −115) kcal for Peptamen® AF and −171 (−455 to −4) kcal for Isosource® Energy (p = 0.014; Table 2).
In the Isosource® group, three patients had positive stool samples for Clostridium difficile. There was no noticeable difference regarding adverse events or serious adverse events between the two treatment groups (Additional file 1: Table S7–S9). No ‘certain’ or ‘probable’ product-related events were identified. The length of mechanical ventilation and ICU and hospital stay were similar in both groups (Table 6).
At baseline, patients with diarrhea suffered from higher scores of disease severity (Acute Physiology and Chronic Health Evaluation (APACHE) II and SAPS II; Table 7). A post-hoc analysis adjusted for treatment group, age, sex, and SAPS II score showed that patients with diarrhea remained longer on mechanical ventilation (9.5 (6.0–13.1) days vs. 3.9 (3.2–4.6) days; p =0.006) and had longer stays in the ICU (11.0 (8.9–13.1) days vs. 5.0 (3.8–6.2) days; p =0.001) (Table 8).
Discussion
Diarrhea was present during one-third of all ICU days, and roughly two-thirds of our target patient population with a median ICU stay of 8 days experienced diarrhea. The gastrointestinal symptoms were not influenced by the nutritional product. Adjustment for baseline diarrhea (roughly 10% of the patients) and use of antibiotics (61%) did not alter the results. Associated abdominal discomfort was absent or mild-to-moderate in patients in whom it could be assessed, but the nursing workload related to diarrhea was high. The accumulated caloric deficit was <500 Kcal/day during the study period (428 Kcal/day for patients with diarrhea over both groups) but may have been underestimated if malabsorption occurred during periods of diarrhea. The higher caloric deficit in the Peptamen® AF group may be attributed to a higher rate of tube feeding interruptions per nutrition day. Most of the adverse events were judged as unrelated to the study product and the latter was withdrawn in only 3–5% of events.
Previous studies have reported diarrhea incidences ranging from around 15% to over 50% [19,20,21]. Some of the differences can be explained by a differing case mix and definition of diarrhea. The patients in the present study had several risk factors for diarrhea which were likely to contribute to the observed high diarrhea incidence: use of a hyperosmolar formula in both study groups [22]; a relatively high administration rate of the enteral nutrition [23]; the presence of hypoalbuminemia in all study patients [24, 25]; and frequent use of antibiotics in 77% of patients [26, 27].
The composition of enteral feeding had no effect on diarrhea or feeding tolerance. The higher protein content of the new formula was aimed to facilitate higher protein intake, as recommended by recent guidelines [28]. The relevance of protein intake in ICU patients remains controversial [29]. Fewer surgical ICU patients with deficits in protein intake during enteral nutrition were discharged home [30]. In patients with pneumonia and/or sepsis, higher protein administration decreased mortality [31]. In contrast, a recent trial in patients with acute lung injury was stopped prematurely because administration of higher percentages of estimated protein (76% vs. 54%) and energy needs (85% vs. 55%) increased hospital mortality despite unchanged length of mechanical ventilation or infection rates [32]. An enteral diet rich in medium-chain triglycerides, carnitine, and taurine increased protein and energy intake and reduced feeding intolerance and diarrhea in a single-blind study in ICU patients with overall lower diarrhea incidence than in our study [33]. In our study, the differences in protein intake between the study groups were substantial, but were not associated with differences in diarrhea incidence or any of the secondary clinical outcomes.
There are limited data on resource use for patients with diarrhea, and the few published studies focus on Clostridium difficile-associated diarrhea. For example, a multicenter retrospective study reporting adjusted outcomes found longer ICU (8.3 days vs. 6.6 days; p < 0.01) and hospital stay (13.2 days vs. 8.5 days; p < 0.01) and almost 40% increased total cost for patients with compared to those without C. difficile-associated diarrhea [34]. Nursing workload for diarrhea care has not been addressed so far. In our study, with a low incidence of C. difficile, the average nursing workload for diarrhea care was more than 3 h/patient, with a moderate increase in material costs. However, also in our study, patients with diarrhea spent more days on mechanical ventilation and in the ICU compared to those without. This finding emphasizes the need for more research on potentially preventable factors associated with diarrhea.
A limitation of our study is the relatively small number of patients and the frequent use of fecal collectors, although this is clinically indicated and potentially able to decrease nursing workload. This prevented a more detailed analysis of stool frequency. Nevertheless, we can give a reliable estimate of stool events. Not using the fecal collector would have interfered with estimates of diarrhea cost and nursing workload as they occur in our unit.
Conclusions
We found that patients with diarrhea stayed longer in the ICU. This demonstrates that diarrhea is a significant problem in the ICU. While the data of this pilot study do not indicate that modification of the protein and fat content can attenuate the incidence of diarrhea, it does show that a product like Peptamen® AF can effectively deliver a high daily protein amount without overfeeding the ICU patients. More research should be conducted to reduce diarrhea in critically ill ICU long-stayers.
Abbreviations
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- CI:
-
Confidence interval
- CTU:
-
Clinical trial unit
- GCP:
-
Good Clinical Practice
- HR:
-
Hazard ratio
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- PDMS:
-
Patient Data Management System
- SAPS:
-
Simplified Acute Physiology Score
References
Reintam A, Parm P, Kitus R, Kern H, Starkopf J. Gastrointestinal symptoms in intensive care patients. Acta Anaesthesiol Scand. 2009;53(3):318–24.
Reintam Blaser A, Starkopf J, Malbrain ML. Abdominal signs and symptoms in intensive care patients. Anaesthesiol Intensive Ther. 2015;47(4):379–87.
Reintam Blaser A, Deane AM, Fruhwald S. Diarrhoea in the critically ill. Curr Opin Crit Care. 2015;21(2):142–53.
Aderinto-Adike AO, Quigley EM. Gastrointestinal motility problems in critical care: a clinical perspective. J Dig Dis. 2014;15(7):335–44.
Ukleja A. Altered GI, motility in critically ill patients. Nutr Clin Pract. 2010;25(1):16–25.
Thibault R, Graf S, Clerc A, Delieuvin N, Heidegger CP, Pichard C. Diarrhoea in the ICU: respective contribution of feeding and antibiotics. Crit Care. 2013;17(4):R153.
De Winter BY, De Man JG. Interplay between inflammation, immune system and neuronal pathways: effect on gastrointestinal motility. World J Gastroenterol. 2010;16(44):5523–35.
Kamarul Zaman M, Chin KF, Rai V, Majid HA. Fiber and prebiotic supplementation in enteral nutrition: a systematic review and meta-analysis. World J Gastroenterol. 2015;21(17):5372–81.
Spapen H, Diltoer M, Van Malderen C, Opdenacker G, Suys E, Huyghens L. Soluble fiber reduces the incidence of diarrhea in septic patients receiving total enteral nutrition: a prospective, double-blind, randomized, and controlled trial. Clin Nutr. 2001;20(4):301–5.
Caparros T, Lopez J, Grau T. Early enteral nutrition in critically ill patients with a high-protein diet enriched with arginine, fiber, and antioxidants compared with a standard high-protein diet. The effect on nosocomial infections and outcome. JPEN J Parenter Enteral Nutr. 2001;25(6):299–308. discussion 308–9.
Rushdi TA, Pichard C, Khater YH. Control of diarrhea by fiber-enriched diet in ICU patients on enteral nutrition: a prospective randomized controlled trial. Clin Nutr. 2004;23(6):1344–52.
Hsu CW, Sun SF, Lin SL, Kang SP, Chu KA, Lin CH, Huang HH. Duodenal versus gastric feeding in medical intensive care unit patients: a prospective, randomized, clinical study. Crit Care Med. 2009;37(6):1866–72.
Arabi YM, Tamim HM, Dhar GS, Al-Dawood A, Al-Sultan M, Sakkijha MH, Kahoul SH, Brits R. Permissive underfeeding and intensive insulin therapy in critically ill patients: a randomized controlled trial. Am J Clin Nutr. 2011;93(3):569–77.
Wan B, Fu H, Yin J. Early jejunal feeding by bedside placement of a nasointestinal tube significantly improves nutritional status and reduces complications in critically ill patients versus enteral nutrition by a nasogastric tube. Asia Pac J Clin Nutr. 2015;24(1):51–7.
Majid HA, Cole J, Emery PW, Whelan K. Additional oligofructose/inulin does not increase faecal bifidobacteria in critically ill patients receiving enteral nutrition: a randomised controlled trial. Clin Nutr. 2014;33(6):966–72.
Daniel H. Molecular and integrative physiology of intestinal peptide transport. Annu Rev Physiol. 2004;66:361–84.
Hecker M, Linder T, Ott J, Walmrath HD, Lohmeyer J, Vadasz I, Marsh LM, Herold S, Reichert M, Buchbinder A, et al. Immunomodulation by lipid emulsions in pulmonary inflammation: a randomized controlled trial. Crit Care. 2015;19:226.
Whelan K, Judd PA, Taylor MA. Assessment of fecal output in patients receiving enteral tube feeding: validation of a novel chart. Eur J Clin Nutr. 2004;58(7):1030–7.
McClave SA, Sexton LK, Spain DA, Adams JL, Owens NA, Sullins MB, Blandford BS, Snider HL. Enteral tube feeding in the intensive care unit: factors impeding adequate delivery. Crit Care Med. 1999;27(7):1252–6.
Montejo JC. Enteral nutrition-related gastrointestinal complications in critically ill patients: a multicenter study. The Nutritional and Metabolic Working Group of the Spanish Society of Intensive Care Medicine and Coronary Units. Crit Care Med. 1999;27(8):1447–53.
Reintam Blaser A, Poeze M, Malbrain ML, Bjorck M, Oudemans-van Straaten HM, Starkopf J. Gastro-Intestinal Failure Trial Group. Gastrointestinal symptoms during the first week of intensive care are associated with poor outcome: a prospective multicentre study. Intensive Care Med. 2013;39(5):899–909.
Smith CE, Marien L, Brogdon C, Faust-Wilson P, Lohr G, Gerald KB, Pingleton S. Diarrhea associated with tube feeding in mechanically ventilated critically ill patients. Nurs Res. 1990;39(3):148–52.
Adare A, Afanasiev S, Aidala C, Ajitanand NN, Akiba Y, Al-Bataineh H, Alexander J, Al-Jamel A, Aoki K, Aphecetche L, et al. Enhanced production of direct photons in Au + Au collisions at square root(S(NN)) = 200 GeV and implications for the initial temperature. Phys Rev Lett. 2010;104(13):132301.
Brinson RR, Kolts BE. Hypoalbuminemia as an indicator of diarrheal incidence in critically ill patients. Crit Care Med. 1987;15(5):506–9.
Hwang TL, Lue MC, Nee YJ, Jan YY, Chen MF. The incidence of diarrhea in patients with hypoalbuminemia due to acute or chronic malnutrition during enteral feeding. Am J Gastroenterol. 1994;89(3):376–8.
Reese JL, Means ME, Hanrahan K, Clearman B, Colwill M, Dawson C. Diarrhea associated with nasogastric feedings. Oncol Nurs Forum. 1996;23(1):59–66. discussion 66–8.
Guenter PA, Settle RG, Perlmutter S, Marino PL, DeSimone GA, Rolandelli RH. Tube feeding-related diarrhea in acutely ill patients. JPEN J Parenter Enteral Nutr. 1991;15(3):277–80.
Taylor BE, McClave SA, Martindale RG, Warren MM, Johnson DR, Braunschweig C, McCarthy MS, Davanos E, Rice TW, Cresci GA, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). Crit Care Med. 2016;44(2):390–438.
Singer P, Hiesmayr M, Biolo G, Felbinger TW, Berger MM, Goeters C, Kondrup J, Wunder C, Pichard C. Pragmatic approach to nutrition in the ICU: expert opinion regarding which calorie protein target. Clin Nutr. 2014;33(2):246–51.
Yeh DD, Fuentes E, Quraishi SA, Cropano C, Kaafarani H, Lee J, King DR, DeMoya M, Fagenholz P, Butler K, et al. Adequate nutrition may get you home: effect of caloric/protein deficits on the discharge destination of critically ill surgical patients. JPEN J Parenter Enteral Nutr. 2016;40(1):37–44.
Elke G, Wang M, Weiler N, Day AG, Heyland DK. Close to recommended caloric and protein intake by enteral nutrition is associated with better clinical outcome of critically ill septic patients: secondary analysis of a large international nutrition database. Crit Care. 2014;18(1):R29.
Braunschweig CA, Sheean PM, Peterson SJ, Gomez Perez S, Freels S, Lateef O, Gurka D, Fantuzzi G. Intensive nutrition in acute lung injury: a clinical trial (INTACT). JPEN J Parenter Enteral Nutr. 2015;39(1):13–20.
Qiu C, Chen C, Zhang W, Kou Q, Wu S, Zhou L, Liu J, Ma G, Chen J, Chen M, et al. A fat-modified enteral formula improves feeding tolerance in critically ill patients: a multicenter, single-blind, randomized controlled trial. JPEN J Parenter Enteral Nutr. 2015. epub ahead of print
Magee G, Strauss ME, Thomas SM, Brown H, Baumer D, Broderick KC. Impact of Clostridium difficile-associated diarrhea on acute care length of stay, hospital costs, and readmission: a multicenter retrospective study of inpatients, 2009-2011. Am J Infect Control. 2015;43(11):1148–53.
Acknowledgements
The authors thank all the nursing specialists for their support for the study in their everyday work. The research nurses of our department, in particular Margaret Jong and Michael Lensch, deserve our special gratitude.
Funding
The study products were provided by Nestlé Healthscience, Vevey, Switzerland. The provider had no influence on data analysis or content of the current manuscript.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors’ contributions
SMJ: conception and conduction of the study, data analysis and interpretation, drafting and revisions of the manuscript. LB: data analysis, contribution to the manuscript, DB: data analysis, contribution to the manuscript. MC: data analysis. JT; conception and conduction of the study, data interpretation, revision of the manuscript. All authors have read and approved the manuscript.
Competing interests
The Department of Intensive Care Medicine has had research & development and consulting contracts with Orion Corporation, Abbott Nutrition International, B. Braun Medical AG, CSEM SA, Edwards Lifesciences Services GmbH/SA, Kenta Biotech Ltd, Maquet Critical Care AB, Omnicare Clinical Research AG, and Nestlé. Educational grants were received from Fresenius Kabi, GSK, MSD, Lilly, Baxter, Astellas, AstraZeneca, B. Braun Medical AG, CSL Behring, Maquet, Novartis, Covidien, Nycomed, Pierre Fabre Pharma (Roba Pharma), Pfizer, and Orion Pharma. No personal financial benefit resulted from respective development/consulting contracts and/or educational grants.
Consent for publication
Not applicable.
Ethics approval and consent to participate
This study was approved by the local Ethics Committee (Kantonale Ethikkomission Bern, 060/12) and is registered at clinicalTrials.gov (NCT01581957), registered on 18 April 2012. Informed consent was obtained from each patient or from a close relative.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1:
Supplementary Tables (DOCX 48 kb).
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Jakob, S.M., Bütikofer, L., Berger, D. et al. A randomized controlled pilot study to evaluate the effect of an enteral formulation designed to improve gastrointestinal tolerance in the critically ill patient—the SPIRIT trial. Crit Care 21, 140 (2017). https://doi.org/10.1186/s13054-017-1730-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-017-1730-1