Abstract
Background
The optimal control of blood volume without fluid overload is a main challenge in the daily care of intensive care unit (ICU) patients. Accordingly this study focused on the identification of biomarkers to help characterize fluid overload status.
Methods
Sixty-seven patients were studied from ICU admission to day 7 (D7). Blood and urine samples were taken daily and sodium and water balance strictly calculated resulting in a total cumulative assessment of ∆Na+ and ∆H2O. Furthermore, plasmatic biomarkers (cortisol, epinephrine, norepinephrine, renin, angiotensin II, aldosterone, pro-endothelin, copeptine, atrial natriuretic peptide, erythropoietin, mid-regional pro-adrenomedullin (MR-proADM)) and Sequential Organ Failure Assessment (SOFA) scores were measured at D2, D5 and D7. Blood volumes were measured with 51Cr fixed on red blood cells at D2 and D7.
Results
The ∆Na+ or ∆H2O were increased in all patients but never related to blood volumes at D2 nor D7. Total blood volumes were at normal values with constantly low red blood cell volumes and normal or decreased plasmatic volume. Weight, plasmatic proteins, and hemoglobin were weakly related to ∆Na+ or ∆H2O. Amongst all tested biomarkers, only MR-proADM was related to sodium and fluid overload. This biomarker was also a predictor of SOFA scores.
Conclusions
Plasmatic concentration in MR-proADM seems to be a good surrogate for evaluation of ∆Na+ or ∆H2O and predicts sodium and extracellular fluid overload.
Trial registration
ClinicalTrials.gov: NCT01858675 in May 13, 2013.
Similar content being viewed by others
Background
The maintenance of optimal blood volume without the development of a positive fluid balance is a major challenge in the daily care of patients suffering from acute traumatic, subarachnoid hemorrhage or infectious inflammatory disorders [1–10]. Indeed, capillary leak significantly contributes to the development of tissue edema and causes persistent hypovolemia despite fluid resuscitation [11–13]. The consequence is two-fold, with (1) a large volume fluid resuscitation and (2) an increase in tissue edema with impairment of microcirculation architecture and oxygen diffusion. This fluid overload caused by fluid resuscitation and excess sodium can be the source of organ dysfunction, including acute lung injury, abdominal compartment syndrome and acute renal injury [2–5, 14, 15], thereby contributing to higher mortality [7–9]. A 4-kg weight gain, corresponding to an accumulation of 4 L of water and 36 g of sodium chloride, is the limit beyond which morbidity and mortality increase [3, 16–18].
The accurate monitoring of fluid balance is therefore crucial in guiding fluid resuscitation. However, there is no gold standard method for complete measurement and the use of input/output charts in intensive care unit (ICU) patients is notorious for being incomplete and inaccurate. Consequently, accurate and reproducible methods to improve the monitoring of fluid balance are essential.
Several plasmatic biomarkers may contribute to arbitrating conflict between the control of optimal blood volume and the development of fluid overload: these include stress hormones, such as cortisol and catecholamines; hormones involved in volume regulation by sodium chloride or water retention, such as the renin-angiotensin II-aldosterone system [19]; vasopressin, expressed by (CT)-pro-arginine vasopressin, known as copeptin [20]; endothelin expressed by pro-endothelin and atrial natriuretic peptide (ANP), measured by pro-ANP; factors involved in the production of red blood cells, such as erythropoietin (EPO) [21]; and factors that repair the endothelium after injury, such as mid-regional pro-adrenomedullin (MR-proADM) [22, 23].
The first aim of the Etude des marqueurs iNnovants de la VOLémie (ENVOL study) was to identify a reliable surrogate biomarker capable of predicting blood volumes and/or cumulative sodium and water balance (∆Na+ and ∆H2O). We also tried to evaluate any relationship between extracellular volume and blood volume measurements. For these purposes, we precisely characterized changes in extracellular and blood volumes and changes in several plasmatic biomarkers involved in volume regulation during the first 7 days of ICU stay.
Methods
This prospective, 7-day observational study was conducted between March 2012 and September 2014 in the 38-bed Department of Anesthesiology and Intensive Care at Bicêtre University Hospital, in Le Kremlin-Bicêtre, France. The Institutional Review Board of the hospital (Comité de protection des personnes Ile de France VII) approved the study on December 2011 (reference 11-045). Written informed consent was systematically obtained from all participants included in the study or from a relative, in accordance with French legal ethics.
We studied four groups of ICU patients, including those with severe brain trauma (SBT), aneurysmal subarachnoid hemorrhage (SAH), severe non-cerebral trauma (NCT) or postoperative peritonitis with septic shock (PPS). Patients were included if they required continuous mechanical ventilation on day 2. SBT was defined as brain trauma with a Glasgow coma score of <9. Patients with SAH were included in the presence of a score ≥4 on the World Federation of Neurosurgical Societies (WFNS) scale [24]. Patients with NCT were included when the Injury Severity Score was ≥25. Patients with PPS were included after abdominal surgery complicated by manifestations of hemodynamic shock, including hypotension and low cardiac output or lactate concentration >4 mmol/L. Patients <18 years, pregnant or presenting with New York Heart Association (NYHA) graded ≥ II were excluded.
Data collection
During the ICU stay, general and demographic data were collected, including age, sex, weight, height, simplified index of illness severity after the first 48 h (Simplified Index of Gravity (IGS) II) and admission date. Sequential Organ Failure Assessment (SOFA) scores were measured upon admission (day 0 (D0)), and on days 2, 5 and 7 (D2, D5 and D7) [25]. Mean arterial pressure, doses of norepinephrine and core temperature were recorded daily. Blood laboratory tests included measurements of hemoglobin, proteins, electrolytes, creatinine and urinary concentrations of Na+, K+, Cl-, urea, creatinine and osmolarity. The urinary electrolytes, creatinine, urea and osmolarity were measured in the morning and the total 24-h output was used to calculate the previous day’s loss of Na+, K+, urea and the creatinine clearance. Weight was carefully measured using weighing beds and recorded on D2 and D7. The baseline weight was that recorded by the patient or a relative.
The daily intravenous fluid administration was based on the monitoring of heart rate, arterial pressure, blood lactate concentration, serial echocardiograms, cardiac filling pressures and output and signs of fluid responsiveness in ventilated patients [26, 27].
Evaluation of extracellular volume
Sodium and fluid balances were calculated daily in order to estimate changes in extracellular space. The previous day’s inputs and outputs of sodium and water were calculated each morning. All other losses were measured, including from ileostomies and external ventricular drainage when present. Sodium losses were measured from all liquids and deducted from sodium intake. The difference between water administration from enteral nutrition and daily crystalloids or colloid infusion and water loss was calculated. Insensitive losses were adjusted for body temperature. The sodium and water gains or losses were calculated daily and added to the previous day’s measurements as cumulative fluid balance (∆Na+ and ∆H2O). A >36 g ∆Na+ or >4 L ∆H2O was defined as fluid overload [16–18]. The creatinine clearance was calculated daily. All calculations were made by one caregiver and verified by another (PEL, HF and BV).
Blood volume measurements
The red blood cell volume (RBCV) was measured on D2 and D7 (±1 day), using 10 mL of the patient’s red blood cells (RBC) labeled with radioactive chromium (51Cr-RBC). We re-injected a known quantity of radioactive RBC intravenously and collected two arterial samples 10 and 30 minutes later. From the radioactivity of these samples we derived RBCV in mL/kg using the patient’s body weight recorded before admission [28]. The arterial hematocrit and RBCV defined the total blood volume (TBV), in mL/kg and the plasma volume (PV), in mL/kg. The normal values are 32 ± 6 mL/kg for RBCV, 72 ± 14 mL/kg for TBV, and 40 ± 8 mL/kg for PV. Hypovolemia was noted when TBV was <20 % of normal values [28]. On D7, we also measured PV by intravenously injecting a small amount of albumin labeled with radioactive iodine (125I-albumin), and collected arterial samples at 10 and 30 minutes and at 2 h [29]. The normal PV measured with 125I is 45 ± 10 mL/kg, slightly larger than that measured with 51Cr-RBC [28].
Biomarker analysis
Plasma biomarkers were analyzed on D2, D5 and D7. MR-proADM, Pro-ANP, renin, angiotensin II, aldosterone, cortisol, norepinephrine and epinephrine, copeptin, pro-endothelin and EPO were measured for potential interference with extracellular or blood volumes. All biologic biomarkers were analyzed together after inclusion in November 2014.
Statistical analysis
Because our original aim was to assess the correlation of the biomarkers with intravascular volumes, the study sample size was calculated considering that brain natriuretic peptide (BNP) and EPO are good surrogate markers of intravascular volumes. We then used published values of BNP and EPO concentrations in similar patients [21, 30] to calculate the number of patients needed (three groups of patients with hypervolemia, normovolemia and hypovolemia, respectively, considering the initial protocol with a 50 % between-group difference and power of 80 %). Data were analyzed using R [31]. The normality of data distribution was verified using quantile-quantile plots and Shapiro’s test. Because most data were measured with error, Deming regression with equal variances was used to calculate the slope of the regression curves.
Because biomarkers were approximately log-normally distributed, comparisons between D2, D5 and D7 values were performed on the log transformed data using the Tukey test after analysis of variance (ANOVA). As our objective was also the measurement of extracellular volume, we also studied fluid overload. For this purpose we considered 4 L and 36 g as ∆H2O and ∆Na+ (equivalent to 4 L of saline), respectively, for the cutoff of response variables [16–18].
We also calculated the performance of biomarkers to predict a SOFA score >9. The calculation of ∆H2O and ∆Na+ and SOFA score were performed on the same day as the biomarkers were assessed. Because of the large number of variables that were candidates for inclusion in multivariate analysis, we first used random forest regression [32] to select the most pertinent demographic and biological covariates explaining fluid and sodium overload and SOFA score. This was followed by linear mixed effect regression in which subject and day of measurement were considered as random effects due to correlation between days of measurement.
Receiver operating characteristic (ROC) curves were constructed to calculate the performance of the biomarkers in predicting fluid and sodium overload (∆H2O and ∆Na+) and SOFA score. The optimal sensitivity/specificity cutoff for predictive variables was calculated, using the non-weighted Youden index. The statistical significance was set at P <0.05. Data are reported as means ± standard deviation (SD), medians (25–75 percentiles) or counts and percentages or 95 % confidence interval (95 % CI).
Results
In the first 7 days after admission to the ICU, 67 patients including those with SBT (n = 21), SAH (n = 20), NCT (n = 20) and PPS (n = 6) were studied. General demographic data, the number of patients studied in each group and SOFA scores on D0, D2, D5 and D7 are shown in Table 1.
Sodium and hydric balance
The cumulative sodium and water gains are reported as ∆Na+ and ∆H2O on D2 and D7 in each study group (Fig. 1). A fluid overload (i.e. more than 36 g of Na+ or 4 L of H2O) on D2 was observed in 43 patients (64 %) for ∆Na+ and 36 for ∆H2O (54 %), and on D7 in 18 (27 %) for ∆Na+ and 33 (49 %) for ∆H2O. This sodium and water positive balances on D2 and D7 were observed in all groups, with a higher increase in sodium and water in the NCT and PPS than in the SBT and SAH groups. For example, on D2, a cumulative increase in Na+ of 70 ± 32 and 77 ± 28 g was measured in the NCT and PPS group, in contrast to 43 ± 24 and 28 ± 24 g in the SBT and SAH groups (P < 0.0001, Fig. 1a). The ∆Na+ was related to ∆H2O, confirming that retained water is related to retained sodium (∆Na+(g) = 7.2∆H2O(L)-4.0; r 2 = 0.67; P < 0.0001). As a known indicator of extracellular space, plasma concentration of proteins and variation in weight were related to ∆Na+ and ∆H2O, though these relationships were weak (r 2 = 0.44 and r 2 = 0.35 for plasma proteins and ∆Na+ or ∆H2O, r 2 = 0.27 and r 2 = 0.33 for ∆ weight and ∆Na+ or ∆H2O, P < 0.001 for all). Like plasma proteins, hemoglobin was weakly related to ∆Na+ (r 2 = 0.15) or ∆H20 (r 2 = 0.23), P < 0.001.
a Cumulative sodium balance (∆Na+, g) on day 2 (D 2 ) and D 7 in the 67 patients studied. b Cumulative fluid balance (∆H2O, L) on D 2 and D 7 . Thresholds of 36 g for sodium and 4 L for water, corresponding to 4 L of saline and described as a tolerable fluid overload, are marked as shaded zone around equilibrate balances. SBT severe brain trauma, SAH aneurysmal subarachnoid hemorrhage, NCT severe non-cerebral trauma, PPS postoperative peritonitis with shock
Blood volumes
TBV, RBCV and PV were measured with 51Cr in 62 patients on D2 and in 63 patients on D7 (with 125I-albumin in 58 patients on D7). TBV, RBCV and PV are shown in Fig. 2. A decrease in TBV was observed in most patients. Only 28 patients on D2 (45 %) and 31 on D7 (49 %) were in the normal range. Hypovolemia (TBV <20 %) was present in 34 patients (55 %) on D2 and 32 patients (51 %) on D7. Low RBCV was observed in all but three transfused patients (Fig. 2b). Decrease in RBCV was sometimes notably low with a RBCV <50 % in 34 patients (55 %) on D2 and 21 patients (33 %) on D7. We found no significant relationship between TBV or RBCV and ∆Na+ or ∆H2O (see Additional file 1).
Total blood volume (TBV, mL/Kg) (a), red blood cell volume (RBCV, mL/Kg) (b) and plasmatic volume (PV, mL/Kg) (c) on day 2 (D 2 ) and D 7 . Thresholds of 20 % around normal values are marked as shaded zones. SBT severe brain trauma, SAH aneurysmal subarachnoid hemorrhage, NCT severe non-cerebral trauma, PPS postoperative peritonitis with shock
The distribution of PV was in the normal range (Fig. 2c). Only 13 patients on D2 (21 %) and 10 patients on D7 (16 %) were below the 20 % range. Importantly, we found no relationship between PV and ∆Na+ or ∆H2O (see Additional file 1). Identically, no correlation was observed between PV and plasma proteins. Hemoglobin concentration was weakly related to RBCV (r 2 = 0.33, P < 0.001) and was not related to PV (r 2 = 0.026, P = 0.07). On D7, PV was measured by 125I-albumin in 58 patients. There was a statistically significant relationship between PV calculated from 51Cr-RBC and PV directly measured with 125I-albumin (P < 0.0001). The slope of the Deming regression was 0.852 (0.610–1.08) with an r 2 value of 0.75.
Biomarkers
Detailed kinetics of all biomarkers are shown in Table 2. Most biomarkers increased on D2 and decreased significantly on D5 and D7 (copeptin, angiotensin II and renin). MR-proADM and EPO decreased significantly on D7. Cortisol, aldosterone, pro-ANP and pro-endothelin remained unchanged. Plasma norepinephrine concentration was not reliable because it was infused as a treatment.
Of all biomarkers tested, only MR-proADM and angiotensin II were significantly related to ∆Na + (P = 0.01 and P = 0.03) and MR-proADM to ∆H2O (P < 10-5). SOFA was related to ∆Na+ (P < 10-5), MR-proADM (P < 10-5), and EPO (P = 0.03) (see Additional file 2). No difference was found associated to the type of pathological characteristics.
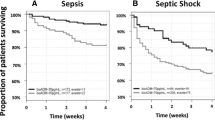
We constructed ROC curves with MR-proADM because it was the only predictor covariate common to the three variables tested (∆H2O, ∆Na+ and SOFA). MR-proADM has good discriminative properties with an area under the curve (AUC) of 0.838 (0.780–0.888) for ∆H2O and an AUC of 0.823 (0.764–0.880) for ∆Na+ (Fig. 3). We determined a threshold of MR-proADM predicting a positive balance greater than 36 g Na+ or 4 L H2O. These thresholds were 0.865 nmol/L (specificity 0.625 (0.538–0.714), sensitivity 0.865 (0.787–0.933)) for ∆Na+ and 1.125 nmol/L (specificity 0.900 (0.833–0.9560, sensitivity 0.604 (0.513–0.694)) for ∆H2O. Furthermore, MR-proADM predicted a SOFA score >9 with an AUC of 0.750 (0.658–0.830) and a threshold at 1.035 nmol/L (specificity 0.635 (0.560–0.711), sensitivity 0.762 (0.643–0.881)).
ROC curves to describe the relationship between the plasmatic concentration of mid-regional pro-adrenomedullin (MR-proADM) and fluid overload of 4 L for ∆H2O and 36 g for ∆Na+. Area under the curve (AUC) is 0.838 (0.780–0.888) for ∆H2O and 0.823 (0.764–0.880) for ∆Na+ determining the relationship between dangerous fluid overload and plasmatic MR-proADM. The Youden index indicates a threshold for plasmatic MR-proADM (0.865 nmol/L (specificity 0.625/sensitivity 0.865) for ∆Na+ >36 g and 1.125 nmol/L (specificity 0.900/sensitivity 0.604) for ∆H2O >4 L) to predict fluid overload
We also tested the relationships between biomarkers and measured blood volumes. It is noteworthy that among all biomarkers, only EPO was related to RBCV (P < 10-5) but the ROC curve constructed for a 50 % decrease in RBCV revealed a low AUC (0.70 (0.60–0.78)).
Discussion
This study revealed that MR-proADM, a biomarker of endothelial permeability [22, 23], may be used as a surrogate for the increase in sodium and water balance in the extracellular space, within the first week after admission of critically ill patients to the ICU. In addition, we found no relationship between the increase in sodium or water balance and direct measurement of blood volumes on D2 and D7. We found that MR-proADM thresholds of 0.865 nmol/L for ∆Na+ and 1.125 nmol/L for ∆H20 were predictive of fluid and of salt overloads, respectively. Moreover, MR-proADM was related to the concurrent SOFA score.
Excessive sodium and fluid balance is a risk factor for morbidity and mortality in critically ill patients [7–9, 33]. A reliable and easy to measure surrogate biomarker could be very useful in improving the monitoring of fluid balance and identification of patients with a positive interstitial fluid and sodium balance. This biomarker should enable us to better personalize therapy and to guide fluid resuscitation and administration of vasopressors or diuretics.
While MR-proADM seems to be a particularly reliable indicator of sodium and fluid balance, it does not exclusively indicate capillary permeability. Indeed, MR-proADM is a stable fragment of pro-adrenomedullin which reflects levels of the rapidly degraded active peptide adrenomedullin [22]. In addition to its role in vascular endothelial barrier permeability in blood vessels [23], adrenomedullin also stabilizes the lymphatic endothelial barrier [34] and is implicated as an important pleiotropic effector of the host defense mechanism [35].
In the ICU, fluid balance is evaluated by the use of input/output charts and by the daily measure of weight. However, it is time consuming and difficult to perform accurately. In addition, the present study identified a weak relationship between weight and fluid balance. Measurement of patient’s weight in inflammatory disorders may be biased by practical issues but also by loss of muscle mass, interfering with the estimate of fluid overload. Moreover, we found that the usual markers of extracellular volume, such as plasma proteins and hemoglobin also had a weak relationship with sodium or water balance. Thus, the monitoring of sodium and fluid balance is currently a difficult task using tools that have their own limits. MR-proADM concentration, on the other hand, offers a measure of sodium balance and extracellular space, which could be used as a good surrogate to improve fluid balance monitoring. Possibly, it will be useful in the future to test a score centered on MR-proADM but also taking into account simple values such as basal weight or plasma proteins, to easily obtain an even better measurement.
No marker accurately estimated the TBV, PV or RBCV. Moreover, ∆Na+ or ∆H2O are not predictors of blood volume. We found no relationship between fluid balance and plasma volume. This was particularly unexpected, because plasma volume expansion is the main justification for fluid infusion. Yet, plasma was the only volume that was in the normal range on D2 and D7. The absence of correlation between PV and fluid balance supports the hypothesis of possible trapping of Na+ and water in the interstitial volume [36, 37]. Tighter control of PV would be useful in daily practice, though we did not find relationships with biomarkers, proteins or hemoglobin. This issue warrants further examination with a combination of other biomarkers or predictors.
The good correlation between the measurements of PV deducted from RBCV with 51Cr and directly measured with 125I-albumin at D7 strengthened our results. The distribution volume of albumin may be larger than that obtained with RBC, especially when the capillary permeability is pathologically increased. On D7 the difference was weak, suggesting that the capillary permeability was nearly repaired. While it would have been worthwhile to examine this comparison on D2, this was precluded by the interactions between 125I and some of the measurements of biomarkers.
The observation of a decreased RBCV is common and explains low TBV. The measurement of RBCV with 51Cr is a recognized method but requires time [28]. As hematocrit, hemoglobin is dependant of the ratio between RBCV and PV, we found, as others, that hemoglobin concentration is a poor surrogate for RBCV in ICU [38]. EPO is related to RBCV but the ROC curve is not sufficiently discriminative. We found no good biomarker of RBCV to help address this problem.
The present study has some limitations. First, we found no marker that describes blood volume. We need a better understanding of all physiologic determinants, including capillary permeability, hormonal influences and low RBCV and interactions among theses determinants. On the other hand, we identified a biomarker of cumulative salt and water balance, which could be an interesting tool for fluid management in the ICU. Second, we made our study measurements on D2, D5 and D7, long after the admission of patients into the ICU, often after the peak of the disease manifestation. The distribution of extracellular volume may be different at D0 during initial resuscitation. The precise timing of measurements may also be a critical factor. While our study observed the changes that took place on D2 and D7 after an acute event, further studies are needed to fill the gaps.
Our study was observational. Patients who were included reflect the daily practice of our service. However, the group of patients as a covariate did not influence the prediction of fluid balance or blood volume, suggesting that volume abnormalities are independent of the pathology. Other studies will need to confirm our results.
Conclusion
A positive sodium balance is an important negative prognostic factor. We found that MR-proADM is a valuable surrogate to evaluate sodium and fluid overload in the first week after an acute and critical inflammatory illness. MR-proADM could improve the fluid balance monitoring and guide fluid resuscitation and administration of vasopressors or diuretics. After this first step, further studies are needed to test the ability of MR-proADM monitoring to control or prevent fluid overload and organ failure.
Abbreviations
- 125I-albumin:
-
radioactive iodine
- 51Cr-RBC:
-
radioactive chromium
- ANP:
-
atrial natriuretic peptide
- AUC:
-
area under the curve
- BMI:
-
body mass index
- CI:
-
confidence interval
- EPO:
-
erythropoietin
- ICU:
-
intensive care unit
- IGS II:
-
simplified index of gravity
- IQR:
-
interquartile range
- ISS:
-
injury severity score
- MR-proADM:
-
mid-regional pro-adrenomedullin
- NCT:
-
severe non-cerebral trauma
- NYHA:
-
New York Heart Association
- PPS:
-
postoperative peritonitis with shock
- PV:
-
plasma volume
- RBCV:
-
red blood cell volume
- ROC:
-
receiver operating characteristic
- SAH:
-
aneurysmal subarachnoid hemorrhage
- SBT:
-
severe brain trauma
- SOFA:
-
Sequential Organ Failure Assessment
- TBV:
-
total blood volume
- WFNS:
-
World Federation of Neurosurgical Societies
References
Chappell D, Jacob M, Hofmann-Kiefer K, Conzen P, Rehm M. A rational approach to perioperative fluid management. Anesthesiology. 2008;109:723–40.
Robertson CS, Valadka AB, Hannay HJ, Contant CF, Gopinath SP, Cormio M, Uzura M, Grossman RG. Prevention of secondary ischemic insults after severe head injury. Crit Care Med. 1999;27(10):2086–95.
Kissoon NR, Mandrekar JN, Fugate JE, Lanzino G, Wijdicks EF, Rabinstein AA. Positive fluid balance is associated with poor outcomes in subarachnoid hemorrhage. J Stroke Cerebrovasc Dis. 2015;24(10):2245–51.
Sakr Y, Vincent JL, Reinhart K, Groeneveld J, Michalopoulos A, Sprung CL, Artigas A, Ranieri VM, Sepsis Occurence in Acutely Ill Patients Investigators. High tidal volume and positive fluid balance are associated with worse outcome in acute lung injury. Chest. 2005;128:3098–108.
Bagshaw SM, Brophy PD, Cruz D, Ronco C. Fluid balance as a biomarker: impact of fluid overload on outcome in critically ill patients with acute kidney injury. Crit Care. 2008;12:169.
Payen D, de Pont AC, Sakr Y, Spies C, Reinhart K, Vincent JL, Sepsis Occurrence in Acutely Ill Patients (SOAP) Investigators. A positive fluid balance is associated with a worse outcome in patients with acute renal failure. Crit Care. 2008;12:R74.
Boyd JH, Forbes J, Nakada TA, Walley KR, Russell JA. Fluid resuscitation in septic shock: a positive fluid balance and elevated central venous pressure are associated with increased mortality. Crit Care Med. 2001;39:259–65.
Kelm DJ, Perrin JT, Cartin-Ceba R, Gajic O, Schenck L, Kennedy CC. Fluid overload in patients with severe sepsis and septic shock treated with early goal-directed therapy is associated with increased acute need for fluid-related medical interventions and hospital death. Shock. 2015;43:68–73.
Acheampong A, Vincent JL. A positive fluid balance is an independent prognostic factor in patients with sepsis. Crit Care. 2015;19:251.
van der Jagt M. Fluid management of the neurological patient: a concise review. Crit Care. 2016;20(1):126.
Chappell D, Westphal M, Jacob M. The impact of the glycocalyx on microcirculatory oxygen distribution in critical illness. Curr Opin Anaesthesiol. 2009;22:155–62.
Jacob M, Chappell D, Hollmann MW. Current aspects of perioperative fluid handling in vascular surgery. Curr Opin Anaesthesiol. 2009;22:100–8.
Ostrowski SR, Haase N, Müller RB, Møller MH, Pott FC, Perner A, Johansson PI. Association between biomarkers of endothelial injury and hypocoagulability in patients with severe sepsis: a prospective study. Crit Care. 2015;19:191.
Sakr Y, Lobo SM, Moreno RP, Gerlach H, Ranieri VM, Michalopoulos A, Vincent JL, SOAP Investigators. Patterns and early evolution of organ failure in the ICU and their relation to outcome. Crit Care. 2012;16:R222.
Besen BA, Gobatto AL, Melro LM, Maciel AT, Park M. Fluid and electrolyte overload in critically ill patients: an overview. World J Crit Care Med. 2015;4:116–29.
Lobo DN, Bostock KA, Neal KR, Perkins AC, Rowlands BJ, Allison SP. Effect of salt and water balance on recovery of gastrointestinal function after elective colonic resection: a randomised controlled trial. Lancet. 2002;359(9320):1812–8.
Brandstrup B, Tønnesen H, Beier-Holgersen R, Hjortsø E, Ørding H, Danish Study Group on Perioperative Fluid Therapy, et al. Effects of intravenous fluid restriction on postoperative complications: comparison of two peri-operative fluid regimens: a randomized assessor-blinded multicenter trial. Ann Surg. 2003;238:641–8.
Bjerregaard LS, Møller-Sørensen H, Hansen KL, Ravn J, Nilsson JC. Using clinical parameters to guide fluid therapy in high-risk thoracic surgery. A retrospective, observational study. BMC Anesthesiol. 2015;15:91.
Farag E, Maheshwari K, Morgan J, Sakr E, Wael A, Doyle DJ. An update of the role of renin angiotensin in cardiovascular homeostasis. Anesth Analg. 2015;120:275–92.
Zweifel C, Katan M, Schuetz P, Siegemund M, Morgenthaler NG, Merlo A, Mueller B, Christ-Crain M. Copeptin is associated with mortality and outcome in patients with acute intracerebral hemorrhage. BMC Neurol. 2010;10:34.
Breymann C, Rohling R, Huch A, Huch R. Intraoperative endogenous erythropoietin levels and changes in intravascular blood volume in healthy humans. Ann Hematol. 2000;79:183–6.
Christ-Crain M, Morgenthaler NG, Struck J, Harbarth S, Bergmann A, Müller B. Mid-regional pro-adrenomedullin as a prognostic marker in sepsis: an observational study. Crit Care. 2005;9:R816–24.
Koyama T, Ochoa-Callejero L, Sakurai T, Kamiyoshi A, Ichikawa-Shindo Y, et al. Vascular endothelial adrenomedullin-RAMP2 system is essential for vascular integrity and organ homeostasis. Circulation. 2013;127:842–53.
Brisman JL, Song JK, Newell DW. Cerebral aneurysms. N Engl J Med. 2006;355:928–39.
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, Reinhart CK, Suter PM, Thijs LG. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22:707–10.
Feissel M, Michard F, Faller JP, Teboul JL. The respiratory variation in inferior vena cava diameter as a guide to fluid therapy. Intensive Care Med. 2004;30:1834–7.
Feissel M, Michard F, Mangin I, Ruyer O, Faller JP, Teboul JL. Respiratory changes in aortic blood velocity as an indicator of fluid responsiveness in ventilated patients with septic shock. Chest. 2001;119:867–73.
Gore CJ, Hopkins WG, Burge CM. Errors of measurement for blood volume parameters: a meta-analysis. J Appl Physiol (1985). 2005;99:1745–58.
Fairbanks VF, Klee GG, Wiseman GA, Hoyer JD, Tefferi A, Petitt RM, Silverstein MN. Measurement of blood volume and red cell mass: re-examination of 51Cr and 125I methods. Blood Cells Mol Dis. 1996;22:169–86.
Dorhout Mees SM, Hoff RG, Rinkel GJE, Algra A, van den Bergh WM. Brain natriuretic peptide concentrations after aneuvrismal subarachnoid hemorrhage: relationship with hypovolemia and hyponatremia. Neurocrit Care. 2011;4:176–81.
The R Project for Statistical Computing. The R Foundation. Vienna: Vienna University of Economics and Business; 2016. http://www.r-project.org. Accessed 26 Jan 2016.
Breiman L. Manual On Setting Up, Using, And Understanding Random Forests V3.1. 2002. https://www.stat.berkeley.edu/~breiman/Using_random_forests_V3.1.pdf.
Malbrain ML, Marik PE, Witters I, Cordemans C, Kirkpatrick AW, Roberts DJ, Van Regenmortel N. Fluid overload, de-resuscitation, and outcomes in critically ill or injured patients: a systematic review with suggestions for clinical practice. Anaesthesiol Intensive Ther. 2014;46:361–80.
Dunworth WP, Fritz-Six KL, Caron KM. Adrenomedullin stabilizes the lymphatic endothelial barrier in vitro and in vivo. Peptides. 2009;29(12):2243–9.
Zudaire E, Portal-Núñez S, Cuttitta F. The central role of adrenomedullin in host defense. J Leukoc Biol. 2006;80(2):237–44.
Titze J. Sodium balance is not just a renal affair. Curr Opin Nephrol Hypertens. 2014;23:101–5.
Jantsch J, Binger KJ, Müller DN, Titze J. Macrophages in homeostatic immune function. Front Physiol. 2014;5:146.
Takanishi DM, Yu M, Lurie F, Biuk-Aghai E, Yamauchi H, Ho HC, Chapital AD. Peripheral blood hematocrit in critically ill surgical patients: an imprecise surrogate of true RBC volume. Anesth Analg. 2008;106:1808–12.
Acknowledgements
Not applicable.
Funding
Funding was provided by Thermo Fisher Scientific. The company had no role in data collection, data analysis, data interpretation or writing of the report.
Availability of data and materials
All authors hold data. All data are available.
Authors’ contributions
BV conceived the study, participated in study design, collected data, prepared data, deliberated on the statistical analysis and wrote the paper. PEL participated in study design, contributed to measurement of sodium and fluid balance and collected data. FM contributed to blood volume measurements and prepared data. EP contributed to biomarker measurements and prepared data. HF contributed to sodium and fluid balance measurements and collected data. AR, SF and AH participated in collecting echocardiographic data. JXM performed statistical analysis. HR participated in study design. JD participated in study design, revising the draft for important intellectual content and edited the final manuscript. All authors were involved in revising the draft. They read and approved the final manuscript.
Competing interests
All authors had full access to all the study data, and all agreed to submit for publication. BV has received a grant (industry-related sources) from Thermo Fisher and speaker’s fees from Thermo Fisher, Octapharma and LFB. HR works in Thermo Fisher Scientific. JD has received consulting and speaker’s fees from LFB. The other authors declare that they have no competing interests.
Ethics approval and consent to participate
The Institutional Review Board of the hospital, Comité de protection des personnes Ile de France VII, approved the study on December 2011 (reference 11-045).
Author information
Authors and Affiliations
Corresponding author
Additional files
Additional file 1:
Lack of relationship between cumulative sodium balance (∆Na +, g) (A); cumulative fluid balance (∆H 2 O, L) and total blood volume (TBV, mL/Kg), red blood cell volume (RBCV, mL/Kg) and plasmatic volume (PV, mL/Kg) at D2 and D7 (B). (DOCX 47 kb)
Additional file 2:
Random forests perform regression using decision trees. It is a non parametric machine learning method using a series of random decisions at each tree. We used random forests to perform an initial choice between the large number of variables to enter in the second phase of regression. A SOFA (top), ∆H2O (middle) and ∆Na+ (bottom) variable importance measured by random forests. This figure displays the dot chart used to choose the variables entered into the linear mixed-effect regression model. On the left is the normalized mean square error (MSE), on the right, the node impurity is the residual sum of squares. B Results of the mixed effect modeling for ∆Na+, ∆H2O and SOFA using the lme procedure from R. (DOCX 322 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Vigué, B., Leblanc, PE., Moati, F. et al. Mid-regional pro-adrenomedullin (MR-proADM), a marker of positive fluid balance in critically ill patients: results of the ENVOL study. Crit Care 20, 363 (2016). https://doi.org/10.1186/s13054-016-1540-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-016-1540-x