Abstract
Background
Authors of recent meta-analyses have reported that prolonged glucocorticoid treatment is associated with significant improvements in patients with severe pneumonia or acute respiratory distress syndrome (ARDS) of multifactorial etiology. A prospective randomized trial limited to patients with sepsis-associated ARDS is lacking. The objective of our study was to evaluate the efficacy of hydrocortisone treatment in sepsis-associated ARDS.
Methods
In this double-blind, single-center (Siriraj Hospital, Bangkok), randomized, placebo-controlled trial, we recruited adult patients with severe sepsis within 12 h of their meeting ARDS criteria. Patients were randomly assigned (1:1 ratio) to receive either hydrocortisone 50 mg every 6 h or placebo. The primary endpoint was 28-day all-cause mortality; secondary endpoints included survival without organ support on day 28.
Results
Over the course of 4 years, 197 patients were randomized to either hydrocortisone (n = 98) or placebo (n = 99) and were included in this intention-to-treat analysis. The treatment group had significant improvement in the ratio of partial pressure of oxygen in arterial blood to fraction of inspired oxygen and lung injury score (p = 0.01), and similar timing to removal of vital organ support (HR 0.74, 95 % CI 0.51–1.07; p = 0.107). After adjustment for significant covariates, day 28 survival was similar for the whole group (HR 0.80, 95 % CI 0.46–1.41; p = 0.44) and for the larger subgroup (n = 126) with Acute Physiology and Chronic Health Evaluation II score <25 (HR 0.57, 95 % CI 0.24–1.36; p = 0.20). With the exception of hyperglycemia (80.6 % vs. 67.7 %; p = 0.04), the rate of adverse events was similar. Hyperglycemia had no impact on outcome.
Conclusions
In sepsis-associated ARDS, hydrocortisone treatment was associated with a significant improvement in pulmonary physiology, but without a significant survival benefit.
Trial registration
ClinicalTrials.gov identifier NCT01284452. Registered on 18 January 2011.
Similar content being viewed by others
Background
Acute respiratory distress syndrome (ARDS) is a secondary disease that follows—usually within 6–48 h—a primary disease of multifactorial etiology (most frequently pneumonia and extrapulmonary sepsis [1]) associated with severe systemic inflammation. Inflammatory mediators released into the systemic circulation (systemic inflammation) from the site of infection reach the broad pulmonary capillary surface, producing severe and diffuse inflammatory exudate of the pulmonary lobules and resulting in hypoxemic respiratory failure [2]. In addition to the lung, systemic inflammation involves other vital organs, particularly the cardiovascular and renal systems. In ARDS, baseline plasma inflammatory cytokine levels are associated with a significantly increased risk of death after adjustment for tidal volume (6 ml/kg vs. 12 ml/kg) and severity of illness [3], and higher inflammatory cytokine levels are found in the largest subgroup of sepsis-associated ARDS [3]. Sepsis-associated ARDS, in comparison with sepsis without ARDS [4] or non-sepsis-related ARDS [1, 5], is associated with significantly higher morbidity and higher (up to 60 % [4, 6]) mortality.
In sepsis and ARDS, systemic inflammation is activated by the nuclear factor-κB (NF-κB) signaling system and downregulated by activated glucocorticoid receptor α (GRα) [7]. In these patients, inadequate (endogenous glucocorticoid-activated) GRα-mediated downregulation of proinflammatory transcription factor NF-κB in circulating and tissue cells leads to higher initial levels and persistent elevation over time of plasma and bronchoalveolar lavage markers of inflammation, hemostasis, and tissue repair [7]. Inadequate intracellular GRα-mediated anti-inflammatory activity for the severity of the patient’s illness was recently termed critical illness-related corticosteroid insufficiency (CIRCI) [8]. Experimental [9] and clinical research [7] shows that CIRCI can be improved with quantitatively and temporally adequate glucocorticoid administration, and a new meta-analysis provides support for its use in ARDS of multifactorial etiology [10].
Despite the high prevalence and mortality of sepsis-associated ARDS, a prospective randomized controlled trial (RCT) investigating glucocorticoid treatment is lacking. We conducted this RCT to test the hypothesis that the anti-inflammatory action of 7 days of hydrocortisone treatment would result in accelerated disease resolution and lower mortality. The primary outcome was 28-day all-cause mortality; secondary endpoints included 28-day survival without organ support and 60-day mortality.
Methods
Study design
We conducted an investigator-initiated, single-center, double-blind, randomized, parallel-groups, placebo-controlled trial between December 2010 and December 2014 in the medical intensive care unit of Siriraj Hospital, Bangkok, Thailand. This trial is registered with ClinicalTrials.gov (NCT01284452). The study was conducted in accordance with the original protocol. The full study protocol is available by contacting the principal investigator.
Patients
We prospectively screened patients aged 18 years or older meeting the criteria for severe sepsis or septic shock [11]. Patients with severe sepsis or septic shock receiving mechanical ventilation (MV) for hypoxemic respiratory failure were eligible if, within 12 h of study entry, they met the diagnostic criteria for acute lung injury-ARDS according to the American-European Consensus definition [12], as later reclassified on the basis of the 2012 Berlin criteria for the diagnosis of ARDS [13]. Informed consent was obtained from the patients or their legally authorized representatives prior to enrollment. Exclusion criteria included moribund state (i.e., not expected to live more than 24 h), advanced malignancy with life expectancy <6 months, pregnancy, immunosuppressive therapy, underlying disease requiring long-term glucocorticoid treatment within the last 6 months or short-term glucocorticoid treatment within the past 4 weeks, and difficult-to-control diabetes.
Randomization and study intervention
The coinvestigators (CP, WM, VV) evaluated patients for eligibility, obtained informed consent, and enrolled the participants. After inclusion, patients were randomly assigned without restriction in a 1:1 ratio (hydrocortisone to placebo) according to a computer-generated randomization table derived from www.randomization.com by the principal investigator, who had no role in patient management. A research nurse not otherwise involved in the study prepared both the study drug and placebo. The attending physicians, nursing care teams, research investigators, and participants and their family members were blinded to treatment allocation. Hydrocortisone was given daily as an intravenous bolus (50 mg in 10 ml of normal saline) every 6 h for 7 days. The control group received a comparable volume of normal saline on the same time schedule. Fluid resuscitation and vasopressor treatment were administered according to the Surviving Sepsis Campaign guidelines [14, 15]. Clinicians were asked to comply with the ARDS Network guidelines on low tidal volume and positive end-expiratory pressure [16]. The attending physician managed adjustments of ventilator settings, antibiotic selection, nutritional support, glycemic control, and the initiation of renal replacement therapy.
Study endpoints and data collection
This RCT tested the hypothesis that the addition of hydrocortisone treatment to standard care would result in accelerated disease resolution and lower mortality. The primary endpoint of the study was all-cause mortality at study day 28. Secondary outcomes included (1) patients alive without organ support (ventilator, renal replacement therapy, and vasopressors) on day 28, (2) MV-free days up to day 28, (3) vasopressor (dopamine, norepinephrine, or adrenaline)-free days up to day 28 (free days to day 28 for patients who died before or on study day 28 was set to 0), and (4) mortality at study day 60. Return to MV after initial successful (off or at least 48 h) extubation was included in the total duration of MV until study day 28.
Baseline data collected included, age, sex, comorbidities, sepsis severity, source of infection, Acute Physiology and Chronic Health Evaluation (APACHE) II score [17], Sequential Organ Failure Assessment score [18], and Lung Injury Score (LIS) [19]. Progression of ARDS was monitored with longitudinal measurements of the LIS (days 0–7 and 14) [19]. For adverse events, we monitored for nosocomial infections, hyperglycemia (glucose >150 mg/dl), and gastrointestinal bleeding until study day 28.
Statistical analysis
The study protocol stated that the number needed to enroll in this study was calculated by assuming that the 28-day mortality of severe sepsis or septic shock-associated ARDS was 60 % [4, 6]. To detect a 20 % absolute mortality reduction, enrollment of at least 194 patients was required to provide study power of 80 % and a two-sided alpha error of 0.05. There was no planned interim analysis.
The study was analyzed on an intention-to-treat basis. The continuous variables were compared at two or more levels of a categorical factor of interest using the Wilcoxon-Mann-Whitney test, which is a nonparametric counterpart of the two-samples t test. The categorical variables were compared with the use of the chi-square test or Fisher’s exact test, when suitable. The primary outcome was evaluated by chi-square test, and the secondary outcomes were analyzed by chi-square test and Wilcoxon-Mann-Whitney test. For the survival analysis, time to an event of interest was calculated from the date of randomization to the date of the event. Patients who did not experience the event were censored at their last-follow up date or at a specified cutoff date such as day 28 or day 60. Survival distributions were estimated using the Kaplan-Meier method and compared by log-rank test.
We also compared the distribution of the time to event, where an event was defined as death or removal of vital organ support independently, by the following prespecified variables: age (≤65 years or >65 years), APACHE II score (<25 or ≥25), LIS (<2.5 or ≥2.5), sepsis severity (absence of shock or vasopressor-dependent shock), ARDS severity (mild or moderate to severe), source of infection (pneumonia or extrapulmonary), and number of comorbidities (two or fewer or three or more). Association of the survival likelihood of a given event (death or removal from organ support, independently) with a set of variables was estimated using a Cox proportional hazards model in which treatment was kept in such multiple regression models regardless of its significance. To describe and compare the profiles of longitudinal variables of interest, a random coefficient modeling framework was used in which time was the primary predictor and time × treatment interaction indicated the treatment differences in the profiles under investigation. A p value <0.05 was considered statistically significant for all comparisons. SAS® version 9.4 software (SAS Institute, Cary, NC, USA) was used to conduct all of the analyses.
Results
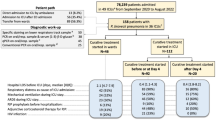
Figure 1 shows progress through the phases of the trial. The trial was stopped when target recruitment was achieved. Of the 206 randomized patients, 9 (6 hydrocortisone, 3 placebo) withdrew consent after randomization and were excluded from analysis. Two hundred thirteen patients were excluded because they were already receiving hydrocortisone for hemodynamic stabilization of refractory septic shock on high-dose vasopressors. The intention-to-treat analysis included 197 patients (98 hydrocortisone, 99 placebo). For the primary endpoint, none of the patients in the intention-to-treat analysis were lost to follow-up. Unless specified otherwise, comparison between groups is reported as hydrocortisone vs. placebo. The mean time (in hours) from meeting severe sepsis criteria to randomization was similar between groups (11.9 ± 7.9 h vs.14.0 ± 10.2 h; p = 0.21).
The baseline characteristics of each group at study entry were similar (Table 1). Most patients had vasopressor-dependent shock (n = 154; all but 7 with a lactate level >2 mmol/L) [20] and met criteria for moderate to severe ARDS (n = 135). Lactate level (3.9 ± 2.2 mmol/L vs. 4.0 ± 2.5 mmol/L; p = 0.95) and distribution of patients with fluid-responsive shock was similar (6.1 % vs. 4.0 %; p = 0.55). The most common comorbidities were hypertension and diabetes mellitus. The leading cause of sepsis was pneumonia; overall, bacteremia was present in 28 %. During treatment intervention, the treated group had significant improvement in gas exchange and LIS (Fig. 2), as well as a similar rate of extubation (43.3 % vs. 31.6 %; p = 0.11). On study day 7 (mean ± SE), the ratio of partial pressure of oxygen in arterial blood to fraction of inspired oxygen (PaO2/FiO2) was 319.1 ± 9.7 vs. 266.3 ± 11.7 (p = 0.001), and the LIS was 1.1 ± 0.1 vs. 1.4 ± 0.1 (p = 0.01). These positive effects persisted at day 14 (last measurement), 7 days after removal of the study drug. In addition, the random coefficients models using the longitudinal data for PaO2/FiO2 and LIS revealed that the treatment arm had significantly improved profiles over time (p = 0.002).
a Changes in ratio of partial pressure of oxygen in arterial blood fraction of inspired oxygen (PaO2/FiO2) over the course of 7 days and on day 14. In comparison with the placebo group, the hydrocortisone group had a significantly higher PaO2/FiO2 ratio by day 3 (p = 0.03) and throughout the observation period. b Changes in Lung Injury Score over the course of 7 days and on day 14. In comparison with the placebo group, the hydrocortisone group had a significantly lower Lung Injury Score by day 3 (p = 0.003) and throughout the observation period
Data for the primary and secondary outcomes are shown in Table 2. By day 28, the treated group had a nonsignificant reduction in duration (days) of MV (10.4 ± 9.4 days vs. 12.4 ± 11.0 days; p = 0.16) and vasopressor support (4.8 ± 3.0 days vs. 6.8 ± 5.7 days; p = 0.16), as well as a nonsignificant increase in patients alive on day 28 without organ support. To evaluate time to survival without organ support at 28 days, a Kaplan-Meier curve was plotted (Fig. 3a). After adjustment by Cox regression analysis for two covariates found to be significant in the multivariate survival model (Table 3), the hydrocortisone cohort showed an HR of 0.74 (95 % CI 0.51–1.07; p = 0.107).
a Kaplan-Meier estimate of time to removal of organ support by treatment arm after adjustment by Cox regression analysis for Acute Physiology and Chronic Health Evaluation II (APACHE II) score and Lung Injury Score. Continuous line corresponds to the placebo group, and dashed line corresponds to the hydrocortisone group. b Kaplan-Meier curve illustrates the probability of survival at 60 days based on APACHE II score <25 vs. ≥25. Continuous line corresponds to the subgroup with APACHE II score <25 (blue = hydrocortisone, red = placebo). Dashed line corresponds to the subgroup with APACHE score ≥25 (blue = hydrocortisone, red = placebo). After adjustment for the presence of vasopressor-dependent shock and Lung Injury Score, in the subgroup with APACHE score <25 (n = 126), the HR for probability of survival at 28 days was 0.57 (95 % CI 0.24–1.36; p = 0.20), and at 60 days it was 0.69 (95 % CI 0.36–1.31; p = 0.25). In the subgroup with APACHE II score ≥25 (n = 71), the HR for probability of survival at 28 days was 1.05 (95 % CI 0.49–2.23; p = 0.60), and at 60 days it was 0.97 (95 % CI 0.50–1.88; p = 0.92)
Unadjusted mortality at day 28 and day 60 was similar (Table 2). Subgroup analysis for the relative risk of death at days 28 and 60 is shown in Table 4. After adjustment by Cox regression analysis for covariates we found significant in the multivariate survival model (Table 3), the HRs for death at days 28 and 60 were 0.80 (95 % CI 0.46–1.41; p = 0.44) and 0.81 (95 % 0.51–1.28; p = 0.37), respectively. The APACHE II score was the most significant (p = 0.001) variable detected in the survival models (Table 3). A Kaplan-Meier curve adjusted for vasopressor-dependent shock and LIS at study entry was generated for the subgroups of patients with APACHE II score <25 vs. ≥25 by treatment (Fig. 3b). After adjustment for the presence of vasopressor-dependent shock and LIS, in the largest subgroup with APACHE II score <25 (n = 126), the HR for probability of survival at 28 days was 0.57 (95 % CI 0.24–1.36, p = 0.20), and at 60 days it was 0.69 (95 % CI 0.36–1.31; p = 0.25). In the subgroup with APACHE II score ≥25 (n = 71), the HR for probability of survival at 28 days was 1.05 (95 % CI 0.49–2.23; p = 0.60), and at 60 days it was 0.97 (95 % CI 0.50–1.88; p = 0.92).
With the exception of hyperglycemia (80.6 % vs. 67.7 %; p = 0.04), the rate of adverse events was similar (Table 5). The incidence of hyperglycemia in patients with (80 % vs. 70 %; p = 0.45) and without (81 % vs. 66 %; p = 0.09) underlying diabetes was similar. Neither diabetes nor hyperglycemia (at study entry or after randomization) had an impact on survival (data not shown).
Discussion
This is the first prospective trial investigating a 7-day course of low-dose hydrocortisone treatment in patients with sepsis-associated early ARDS. Hydrocortisone treatment was associated with rapid and sustained improvement in pulmonary physiology and a nonsignificant increase (65.3 % vs. 55.6 %; p = 0.19) in patients alive on day 28 without organ support. The significant physiological improvements did not translate into an overall survival benefit for the whole group (HR 0.80, 95 % CI 0.46–1.41; p = 0.44), however, and for the largest subgroup of patients with APACHE II score <25 (HR 0.57, 95 % CI 0.24–1.36; p = 0.20). Importantly, in agreement with the literature on sepsis [21] and ARDS [10], we did not find an increased risk of complications, with the exception of hyperglycemia, and hyperglycemia did not affect outcome. Our findings are placed in the context of the limitations of the trial and the updated literature.
Our study has several limitations. First, and most important, our study was significantly underpowered by the recruitment of patients with less severe illness and lower mortality. While the original sample size calculation was based on a control mortality of 60 %, originating from the findings of the largest prior trial [6], our control 28-day mortality was almost half that and similar to the most recent report [5]. This is partly attributable to two main factors: (1) exclusion of a large number of patients who, during the screening process, were already receiving hydrocortisone treatment for refractory septic shock [14]; and (2) improved outcome as a result of implementing the international guidelines of the Surviving Sepsis Campaign [14]. In comparison with prior RCTs, our trial differs by not including longitudinal measurements of systemic inflammatory response syndrome parameters or markers of systemic inflammation [6, 22–27] and an assessment of adrenal function [6, 26].
Seven RCTs published in the English language investigated prolonged glucocorticoid treatment in ARDS [6, 22–27]. In each trial, glucocorticoid treatment was associated with a significant reduction in markers of systemic inflammation (inflammatory cytokines and/or C-reactive protein levels) and improvement in lung function. Three trials investigated hydrocortisone treatment in sepsis [22, 23] or septic shock-associated ARDS [6]. The largest study [6] is a post hoc analysis of 177 patients with ARDS from a trial of vasopressor-dependent septic shock investigating hydrocortisone (dosage similar to our trial) and fludrocortisone (50 μg daily) treatment [28]. In the largest trial [6], among those randomized to receive the active drug, the larger subgroup (n = 129) of nonresponders to a short corticotropin test, contrary to responders (n = 48), had more days alive and off a mechanical ventilator (5.6 ± 8.8 days vs. 2.6 ± 6.6 days; p = 0.006) and improved survival (47 % vs. 25 %; p = 0.021). Two other trials [22, 23] of patients with severe community-acquired pneumonia included 94 patients on MV with early ARDS (16 % with shock). In both trials [22, 23], a hydrocortisone bolus (200 mg) followed by an infusion (240–300 mg/24 h) was associated with a significant reduction in duration of MV; one research group reported improved survival [22].
Four trials investigated prolonged methylprednisolone treatment in early [26, 27] and late [24, 25] ARDS and were the subject of a recent individual patient data (IPD) meta-analysis (n = 322) [10]. By study day 28, the methylprednisolone group had fewer patients dying while on MV (12 % vs. 29 %; p < 0.001) and more patients successfully extubated (80 % vs. 50 %; p < 0.001); hospital mortality was decreased (20 % vs. 33 %; p = 0.006). Importantly, each trial [24–27] consistently reported a 9- to 10-day reduction in duration of MV during methylprednisolone administration (Table S3 supplementary material in [10]). All but one trial [25] incorporated slow tapering of the study drug after extubation; lack of slow tapering contributed to increased return to MV [25].
Our trial is a single-center RCT, which may raise concerns regarding the generalization of the results based on participants’ characteristics and the intervention tested. In comparison with our study, severity of illness scores and LISs were higher in five RCTs [6, 24–27] and similar in two RCTs [22, 23]. Fundamental variables of the treatment protocol that may significantly affect overall response to glucocorticoid treatment in ARDS include study drug, dosage, and duration of administration, including tapering [7]. Our treatment intervention was comparable to the one investigated in the two RCTs with lower severity of illness [22, 23] and differed from the other five RCTs by study drug (hydrocortisone vs. hydrocortisone plus fludrocortisone [6] or methylprednisolone [24–27]), duration of treatment (7 days vs. 14–28 days [24–27]), and tapering (lack of tapering vs. slow tapering [24, 26, 27]).
In the past exogenous glucocorticoids were thought to be qualitatively indistinguishable because they act via the same receptor, but qualitative differences have been discovered, and one glucocorticoid cannot be simply replaced by another [29]. In reference to the RCTs described above [6, 24–27], hydrocortisone has (1) less anti-inflammatory potency when it is not combined with fludrocortisone (a drug with both mineralocorticoid and glucocorticoid activities) and (2) lesser direct inhibitory NF-κB activity than methylprednisolone (half-maximal inhibitory concentration for NF-κB inhibition 16 and 2.8, respectively) [30]. Methylprednisolone, because of its greater penetration in lung tissue and longer residence time [31], is the most frequently used intravenous glucocorticoid for the treatment of severe acute inflammatory lung diseases [32].
New understanding of the central role played by glucocorticoids in resolution of inflammation and restoration of tissue homeostasis [33] provides support for longer duration of treatment incorporating slow tapering (up to 4 weeks). A recent IPD meta-analysis demonstrates that lack of glucocorticoid tapering after extubation of patients with ARDS is frequently associated with clinical deterioration and return to MV [10]. Similarly, researchers in a comparison study of two concurrent RCTs—hydrocortisone 7-day infusion vs. prolonged methylprednisolone—reported that removing hydrocortisone without tapering led to a rebound of systemic inflammation with worsening organ dysfunction requiring reintubation [34]. In our study, we did not measure markers of inflammation and cannot comment on the presence of rebound inflammation. After completion of study treatment, however, the hydrocortisone group continued to demonstrate improved gas exchange and LIS, and the two groups had a similar rate of reintubation by day 28. While these findings may suggest that a clinically significant rebound effect is less likely, most patients (n = 55) had hydrocortisone treatment discontinued prior to extubation, masking a possible rebound.
Our trial does not confirm the benefits reported on the basis of prior RCTs for reduction in duration of MV and intensive care unit stay [22–27] or survival [22–24, 26, 27]. Our study is underpowered for the exploratory analysis to demonstrate a survival benefit in patients with APACHE II scores <25. It is likely that this cohort had a lesser degree of systemic inflammation than patients with APACHE II scores ≥25. Lacking measurement of markers of systemic inflammation over time, we cannot comment on whether our treatment protocol was less effective in achieving a significant anti-inflammatory effect in those with APACHE II scores ≥25.
Conclusions
In sepsis-associated ARDS, early administration of hydrocortisone 50 mg intravenously every 6 h for 7 days was safe and associated with improved lung function without a significant survival benefit. Our study is underpowered for the exploratory analysis to demonstrate a survival benefit in patients with APACHE II scores <25.
Key messages
-
Pneumonia and extrapulmonary sepsis are the leading causes of ARDS. Sepsis-associated ARDS, in comparison with sepsis without ARDS or non-sepsis-related ARDS, is associated with higher morbidity and mortality.
-
Despite the high prevalence and mortality of sepsis-associated ARDS, a prospective RCT investigating glucocorticoid treatment is lacking. This is the first randomized, double-blind, placebo-controlled trial evaluating the efficacy of hydrocortisone treatment in early sepsis-associated ARDS.
-
Hydrocortisone administration for 7 days was associated with improvement in oxygenation parameters and LIS without achieving a significant survival benefit. After hydrocortisone removal, improvements in oxygenation and LIS were maintained. With the exception of hyperglycemia, we found no increased rate of adverse events.
Abbreviations
- APACHE II:
-
Acute Physiology and Chronic Health Evaluation II
- ARDS:
-
Acute respiratory distress syndrome
- CIRCI:
-
Critical illness-related corticosteroid insufficiency
- FiO2 :
-
Fraction of inspired oxygen
- GRα:
-
Glucocorticoid receptor α
- IPD:
-
Individual patient data
- LIS:
-
Lung Injury Score
- MV:
-
Mechanical ventilation
- NF-κB:
-
Nuclear factor-κB
- PaO2 :
-
Partial pressure of oxygen in arterial blood
- RCT:
-
Randomized controlled trial
- SOFA:
-
Sequential Organ Failure Assessment
References
Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, Neff M, et al. Incidence and outcomes of acute lung injury. N Engl J Med. 2005;353(16):1685–93.
Schwingshackl A, Meduri GU. Rationale for prolonged glucocorticoid use in pediatric ARDS: what the adults can teach us. Front Pediatr. 2016;4:58.
Parsons PE, Eisner MD, Thompson BT, Matthay MA, Ancukiewicz M, Bernard GR, et al. Lower tidal volume ventilation and plasma cytokine markers of inflammation in patients with acute lung injury. Crit Care Med. 2005;33(1):1–6. discussion 230–232.
Mikkelsen ME, Shah CV, Meyer NJ, Gaieski DF, Lyon S, Miltiades AN, et al. The epidemiology of acute respiratory distress syndrome in patients presenting to the emergency department with severe sepsis. Shock. 2013;40(5):375–81.
Sheu CC, Gong MN, Zhai R, Chen F, Bajwa EK, Clardy PF, et al. Clinical characteristics and outcomes of sepsis-related vs non-sepsis-related ARDS. Chest. 2010;138(3):559–67.
Annane D, Sébille V, Bellissant E, Ger-Inf-05 Study Group. Effect of low doses of corticosteroids in septic shock patients with or without early acute respiratory distress syndrome. Crit Care Med. 2006;34(1):22–30.
Meduri GU, Annane D, Chrousos GP, Marik PE, Sinclair SE. Activation and regulation of systemic inflammation in ARDS: rationale for prolonged glucocorticoid therapy. Chest. 2009;136:1631–43.
Marik PE, Pastores S, Annane D, Meduri G, Sprung C, Arlt W, et al. Clinical practice guidelines for the diagnosis and management of corticosteroid insufficiency in critical illness: recommendations of an international task force. Crit Care Med. 2008;36:1937–49.
Wang XQ, Zhou X, Zhou Y, Rong L, Gao L, Xu W. Low-dose dexamethasone alleviates lipopolysaccharide-induced acute lung injury in rats and upregulates pulmonary glucocorticoid receptors. Respirology. 2008;13(6):772–80.
Meduri GU, Bridges L, Shih MC, Marik PE, Siemieniuk RA, Kocak M. Prolonged glucocorticoid treatment is associated with improved ARDS outcomes: analysis of individual patients’ data from four randomized trials and trial-level meta-analysis of the updated literature. Intensive Care Med. 2016;42(5):829–40.
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest. 1992;101(6):1644–55.
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, et al. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;149(3 Pt 1):818–24.
Force ADT, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307(23):2526–33.
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Intensive Care Med. 2008;34(1):17–60.
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013;39(2):165–228.
The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301–8.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–29.
Vincent JL, de Mendonça A, Cantraine F, Moreno R, Takala J, Suter PM, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Crit Care Med. 1998;26(11):1793–800.
Murray JF, Matthay MA, Luce JM, Flick MR. An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis. 1988;138(3):720–3.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):801–10.
Annane D, Bellissant E, Bollaert PE, Briegel J, Keh D, Kupfer Y. Corticosteroids for treating sepsis. Cochrane Database Syst Rev. 2015;12(12):CD002243.
Confalonieri M, Urbino R, Potena A, Piattella M, Parigi P, Puccio G, et al. Hydrocortisone infusion for severe community-acquired pneumonia: a preliminary randomized study. Am J Respir Crit Care Med. 2005;171(3):242–8.
Sabry NA, Omar EED. Corticosteroids and ICU course of community acquired pneumonia in Egyptian settings. Pharmacol Pharm. 2011;2(2):73–81.
Meduri GU, Headley AS, Golden E, Carson SJ, Umberger RA, Kelso T, et al. Effect of prolonged methylprednisolone therapy in unresolving acute respiratory distress syndrome: a randomized controlled trial. JAMA. 1998;280(2):159–65.
Steinberg KP, Hudson LD, Goodman RB, Hough CL, Lanken PN, Hyzy R, et al. Efficacy and safety of corticosteroids for persistent acute respiratory distress syndrome. N Engl J Med. 2006;354(16):1671–84.
Meduri GU, Golden E, Freire AX, Taylor E, Zaman M, Carson SJ, et al. Methylprednisolone infusion in early severe ARDS: results of a randomized controlled trial. Chest. 2007;131(4):954–63.
Rezk N, Ibrahim A. Effects of methylprednisolone in early ARDS. Egypt J Chest Dis Tuberc. 2013;62(1):167–72.
Annane D, Sébille V, Charpentier C, Bollaert PE, François B, Korach JM, et al. Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA. 2002;288(7):862–71.
Czock D, Keller F, Rasche FM, Häussler U. Pharmacokinetics and pharmacodynamics of systemically administered glucocorticoids. Clin Pharmacokinet. 2005;44(1):61–98.
Li S, Kang GS, Miller DD, Meduri GU, Yates CR. Evaluation of AP-1 and NF-κB inhibitory potency for oral glucocorticoids. AAPS PharmSci. 2003;5(S1):Abstract R6173.
Greos LS, Vichyanond P, Bloedow DC, Irvin CG, Larsen GL, Szefler SJ, et al. Methylprednisolone achieves greater concentrations in the lung than prednisolone: a pharmacokinetic analysis. Am Rev Respir Dis. 1991;144(3 Pt 1):586–92.
Jantz MA, Sahn SA. Corticosteroids in acute respiratory failure. Am J Respir Crit Care Med. 1999;160(4):1079–100.
Busillo JM, Cidlowski JA. The five Rs of glucocorticoid action during inflammation: ready, reinforce, repress, resolve, and restore. Trends Endocrinol Metab. 2013;24(3):109–19.
Nawab Q, Golden E, Confalonieri M, Umberger R, Meduri G. Corticosteroid treatment in severe community-acquired pneumonia: duration of treatment affects control of systemic inflammation and clinical improvement. Intensive Care Med. 2011;37:1153–554.
Acknowledgements
We acknowledge Lisa Bridges, MSN, ACNP (Veterans Affairs Medical Center, Memphis, TN, USA), for assistance with the dataset.
Funding
This research was supported by Siriraj critical care research funding. The funding source had no role in the conduct of the study or the reporting of the results. This material is the result of work supported in part by the resources of and use of facilities at the Memphis Veterans Affairs Medical Center. The contents of this article do not represent the views of the U.S. Department of Veterans Affairs or the U.S. government.
Availability of data and materials
Not applicable.
Authors’ contributions
ST and CP developed the study protocol, performed data collection and analysis, and drafted the manuscript. WM and VV took part in protocol development, data collection, and manuscript preparation. SU, MK, and GUM carried out the statistical analysis and manuscript preparation. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
All the authors confirm that they agree to publication of this study in Critical Care.
Ethics approval and consent to participate
The protocol of this study was approved by the Siriraj Hospital Ethics Committee in accordance with the Declaration of Helsinki and good clinical practice guidelines. The study protocol number is 544/2553(EC3), and the certificate of approval number is Si 630/2010.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tongyoo, S., Permpikul, C., Mongkolpun, W. et al. Hydrocortisone treatment in early sepsis-associated acute respiratory distress syndrome: results of a randomized controlled trial. Crit Care 20, 329 (2016). https://doi.org/10.1186/s13054-016-1511-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-016-1511-2