Abstract
Introduction
In septic shock patients, the prevalence of low (<70%) central venous oxygen saturation (ScvO2) on admission to the intensive care unit (ICU) and its relationship to outcome are unknown. The objectives of the present study were to estimate the prevalence of low ScvO2 in the first hours of ICU admission and to assess its potential association with mortality in patients with severe sepsis or septic shock.
Methods
This was a prospective, multicentre, observational study conducted over a one-year period in ten French ICUs. Clinicians were asked to include patients with severe sepsis or septic shock preferably within 6 hours of ICU admission and as soon as possible without changing routine practice. ScvO2 was measured at inclusion and 6 hours later (H6), by blood sampling.
Results
We included 363 patients. Initial ScvO2 below 70% was present in 111 patients and the pooled estimate for its prevalence was 27% (95% Confidence interval (95%CI): 18% to 37%). At time of inclusion, among 166 patients with normal lactate concentration (≤2 mmol/L), 55 (33%) had a low initial ScvO2 (<70%), and among 136 patients who had already reached the classic clinical endpoints for mean arterial pressure (≥65 mmHg), central venous pressure (≥8 mmHg), and urine output (≥0.5 mL/Kg of body weight), 43 (32%) had a low initial ScvO2 (<70%). Among them, 49% had lactate below 2 mmol/L. The day-28 mortality was higher in case of low initial ScvO2 (37.8% versus 27.4%; P = 0.049). When adjusted for confounders including the Simplified Acute Physiology Score and initial lactate concentration, a low initial ScvO2 (Odds ratio (OR) = 3.60, 95%CI: 1.76 to 7.36; P = 0.0004) and a low ScvO2 at H6 (OR = 2.18, 95%CI: 1.12 to 4.26; P = 0.022) were associated with day-28 mortality by logistic regression.
Conclusions
Low ScvO2 was common in the first hours of admission to the ICU for severe sepsis or septic shock even when clinical resuscitation endpoints were achieved and even when arterial lactate was normal. A ScvO2 below 70% in the first hours of ICU admission and six hours later was associated with day-28 mortality.
Similar content being viewed by others
Introduction
Central venous oxygen saturation (ScvO2) has long been studied as a prognostic marker and resuscitation end-point in patients with shock [1]. It is an imperfect surrogate of mixed venous oxygen saturation (SvO2) because it reflects the oxygen supply-to-consumption ratio of the upper part of the body only. However, ScvO2 is simple to measure either continuously or intermittently, and spontaneous or therapy-induced changes in ScvO2 and SvO2 are closely correlated [2].
Based on these principles, Rivers et al. [3] showed that an early therapeutic strategy that includes aiming for the rapid normalization of ScvO2 (≥70%) in patients suffering from severe sepsis or septic shock at presentation to the emergency department could improve survival. Since then, international guidelines have recommended targeting ScvO2 at ≥70% during the first 6 hours of care in patients presenting with severe sepsis or septic shock [4]. However, this recommendation remains controversial. Indeed, resuscitation protocols including an ScvO2 target have been mostly tested in the emergency department [5]-[7], not after ICU admission. Importantly, after ICU admission, targeting normal ScvO2 is deemed to have little place, as ScvO2 is frequently considered to be already normalized on ICU admission [8]. However, the prevalence of low ScvO2 (<70%) in ICU septic patients is poorly known. It has been assessed only in two prospective studies of limited size [9],[10], while other studies have only reported the mean initial value of ScvO2 [8],[11]. In addition, the relationship between low ScvO2 and outcome is still unknown.
Since the Rivers study [3], the idea that the relationship between low ScvO2 and fatal outcome in septic patients has been widely demonstrated has remained. Up to now, however, such a relationship has not been demonstrated in multicentre prospective studies performed either in the emergency department [12] or in the ICU [10]. Accordingly, the aim of the present multicentre observational prospective study was to estimate the prevalence of low ScvO2 in patients presenting with severe sepsis or septic shock after ICU admission, and to assess its potential association with outcome.
Materials and methods
The study took place in 10 French medical-surgical adult ICUs (4 university hospitals, 1 regional and teaching hospital, and 5 general hospitals) with a combined total of 154 ICU beds. Participating ICUs were asked to screen consecutive patients presenting with sepsis and circulatory failure for potential inclusion in the study, over a period left at their discretion, from July 2011 to June 2012.
Clinicians were asked to include patients with severe sepsis or septic shock, preferably within 6 hours of ICU admission, and as soon as possible without changing routine practice. Patients were included if they had circulatory failure of septic origin (that is, severe sepsis or septic shock [13]) within 12 hours after ICU admission, and had an intra-arterial and superior vena cava (internal jugular or subclavian) catheter in situ. Circulatory failure was defined by either the use of vasopressor (septic shock) or, in case of severe sepsis, by a mean arterial pressure <65 mmHg or a systolic arterial pressure <90 mmHg at least twice over a 15-minute period, associated with at least one condition reflecting tissue hypoperfusion or low flow state (see Table 1, Criteria for circulatory failure at inclusion). Patients were not included in the case of brain death, admission following cardiac arrest, or if imminent death was expected.
Measurements and data collection
The measurement of ScvO2 was performed as soon as possible (at the time defined as zero hours (H0)) by sampling blood from the superior vena cava through the central venous catheter, and at 6 hours after inclusion (H6). ScvO2 was either calculated from blood gas analysis by a standard blood gas analyser in four centres, or measured by a co-oximeter in six centres. Concomitantly, arterial blood was drawn at each time point for blood gas analysis and lactate measurement. Other demographic, clinical and laboratory data prospectively recorded are provided in Additional file 1. Independent data monitoring was conducted in each site to ascertain the accuracy of recorded information.
The Ethics Committee of the teaching hospital of Limoges, France, approved the protocol for all hospitals involved (agreement number 65-2011-11) and waived the need for prior informed consent because the study procedures fulfilled the criteria of a non-interventional study as defined by the French Law [17]. Patients’ next-of-kin and then patients themselves if they regained capacity were informed of their participation and their right to refuse the use of the obtained data was clearly established.
Haemodynamic monitoring and treatment of shock followed international [18] and national guidelines [19] that corresponded to standard of care of the participating centres. However, none of the participating ICUs had implemented systematic treatment algorithms based on ScvO2 monitoring.
Study objective
The study primary objective was to estimate the prevalence of low ScvO2 (<70%, but other thresholds were also tested) and to assess the possible association between low ScvO2 and day-28 mortality.
Data reporting and statistical analysis
Categorical data are expressed as percentages, and continuous variables are expressed as means ± SD or medians and IQR, as appropriate. The prevalence and 95% CI of ScvO2 < 70% was estimated taking into account participating centres as a random effect [20]. The ScvO2 < 70% and other thresholds of initial ScvO2 values determined by locally weighted scatterplot smoothing (LOWESS) [21] were examined for their potential association with day-28 mortality.
Each given threshold of the initial ScvO2 value was entered in a mixed-effect logistic regression model, with participating centres entered as a random effect, and adjusted for all covariables available at H0 and linked to day-28 mortality with a P-value <0.15, by univariate analysis. The covariables were eliminated using the backward method until the final logistic model with the best fit (as assessed by the Akaike information criterion [15]) was reached. Based on the results of a retrospective study performed in one participating ICU [22], we calculated that 1-year study duration would allow the inclusion of at least 350 patients with 100 fatalities, which would allow multivariate evaluation of ten covariables, including ScvO2.
We re-ran the logistic analyses in predefined subgroups of patients (for example, mechanical ventilation or not at H0, patients below or above median values of continuous variables such as initial lactate level or amount of volume expansion before inclusion, et cetera).
Percentages were compared using the Fisher exact test, chi-square test, or chi-square test for trend (Cochran-Armitage test), and continuous variables were compared using the unpaired Student t-test or by analysis of variance when appropriate. Unadjusted comparisons of survival curves were performed using the log-rank test. Adjusted odds ratios (OR) are given with the 95% CI. A two-tailed P-value <0.05 was considered statistically significant. Mixed-effect logistic regression was performed using the lme4 package of R 2.15.2 [23].
Results
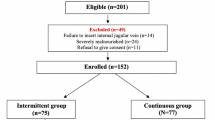
We screened 670 patients with severe sepsis or septic shock. Among them, 363 patients were enrolled (Figure 1). The Simplified acute physiology score (SAPSII) [24] and ICU death rates were similar in enrolled and non enrolled patients (see Additional file 2).
Demographic and clinical characteristics are shown in Table 1. The median time between ICU admission and inclusion (H0), and between the time at which criteria for inclusion were satisfied and inclusion, was 211 minutes (IQR 83 to 339) and 189 minutes (IQR 84 to 292), respectively. The median time between severe sepsis identification and inclusion (H0) was 7.6 hours (IQR 2 to 13.2). Details of resuscitation administered before inclusion and time of inclusion in patients classified according to their origin (transferred from another hospital, from the ward, or from the emergency department) are shown in Table 2.
The mean initial ScvO2 value was 74.1 ± 11.0% and was not different between survivors and non survivors at day 28 (74.6 ± 10.0% versus 73.0 ± 12.9%, respectively; P = 0.21).
Prevalence of low initial ScvO2
Initial ScvO2 < 70% was present in 111 patients and the pooled estimate for its prevalence, taking into account participating centres as a random effect, was 27% (95% CI 18%, 37%). At H0, 136 patients (37%) had reached the classic clinical endpoints for mean arterial pressure (≥65 mmHg), central venous pressure (≥8 mmHg), and urine output (≥0.5 mL/Kg of body weight). Among them, 32% (43/136) had an initial ScvO2 < 70%, with normal lactate concentration (≤2 mmol/L) in 21 (49%) patients. At H0, 166 patients (46%) had normal lactate concentration (≤2 mmol/L). Among them, 55 (33%) had an initial ScvO2 < 70%. The delay between severe sepsis identification and inclusion and the amount of fluids administered for resuscitation before inclusion had no influence on the mean initial ScvO2 values or on the proportions of patients with initial ScvO2 < 70% (see Additional file 3).
Crude day-28 death rate and initial ScvO2level
As determined by visual inspection of the LOWESS plot (see Additional file 4), we assessed the association between day-28 mortality and initial ScvO2 < 70%, <75%, and >85%. The day-28 death rate was significantly higher in patients with initial ScvO2 < 70% than in patients with initial ScvO2 ≥ 70% (42/111 (37.8%) versus 69/252 (27.4%), respectively; P = 0.049), whereas it was similar in patients with initial ScvO2 below or above the other thresholds examined (all P-values >0.35) (see Additional file 5: Table E8).
Association between ScvO2and mortality when adjusted for potential confounders
The initial ScvO2 entered in the logistic model as a continuous variable was negatively linked to day-28 mortality: OR = 0.96 (95% CI 0.93, 0.99) for each 1% increase in initial ScvO2; P = 0.004 (see Additional file 5: Table E9). An initial ScvO2 < 70% was significantly and independently associated with day-28 mortality (OR = 3.60, 95%CI 1.76, 7.36; P = 0.0004) (Table 3), a trend consistently observed across the different subgroups examined (Figure 2).
Forest plot for subgroup analysis. aAll cutoff values provided in the figure for demographic, clinical or laboratory variables are median values calculated on the whole study population. bSequential organ failure assessment (SOFA) score is the highest value during the first 24 hours after enrollment. cWith the use of a cutoff of 2 mmol/L for lactate, the odds ratio for day-28 death (OR) was 1.29 (0.54, 3.05) in the case of lactate >2 mmol/L, and 4.59 (1.79, 11.84) in the case of lactate ≤2 mmol/L. dVasopressor dose = continuous intravenous (iv) norepinephrine dose plus continuous iv epinephrine dose. eLeft ventricular ejection fraction assessed by transthoracic echocardiography before 24 hours after enrollment. fHaemoglobin concentration was taken into account only if measured between 6 hours before and 6 hours after enrollment. SAPSII, Simplified acute physiology score; ScvO2, central venous oxygen saturation.
An initial ScvO2 < 75% was also significantly associated with day-28 mortality (OR = 2.15, 95% CI 1.16 to 3.98; P = 0.015) (see Additional file 5: Table E10).
Evolution of ScvO2and relationship to lactate concentration
The evolution of ScvO2 between H0 and H6 was similar between survivors and non survivors on day 28 (see Additional file 6: Figure E3). However, by logistic regression analysis, a ScvO2 < 70% at H6 still appeared as a risk factor for day-28 death (OR = 2.18, 95% CI 1.12, 4.26; P = 0.022) (see Additional file 5: Table E11).
The proportion of patients with initial ScvO2 < 70% was similar in the case of lactate above or below the median initial lactate value of 2.2 mmol/L (29% versus 33%; P = 0.3). Figure 3 shows the survival curves and the crude death rates at day 28 in four patients’ subgroups according to their lactate concentration and ScvO2 at H0 (for subgroups according to lactate and ScvO2 at H6 see Additional file 6: Figure E4). In subgroup analysis, the logistic regression showed that ScvO2 < 70% was independently associated with day-28 death in patients with initial lactate level <2.2 mmol/L (OR = 3.31) (Figure 2).
Survival curve and death rate (%) at day 28 according to initial lactate level and central venous oxygen saturation (S cv O 2 ). The left part of the figure shows survival curves in four patients’ subgroups according to their initial zero hours (H0) lactate concentration and ScvO2. The right part of the figure shows the day-28 death rate in each subgroup. Numbers inside the bars are number of non survivors/total number of patients in each subgroup. aUnadjusted pair comparison of survival curves between the different subgroups were not statistically significant on log-rank test. bThere was no significant difference in crude death rate at day-28 among the four groups (chi-squared test). However, there was a significant global trend towards higher death rate from the condition with normal lactate and ScvO2 to the condition with high lactate and low ScvO2 (P <0.001, Cochran-Armitage test).
Among the 335 patients with lactate and ScvO2 measured at H0 and H6, 148 (44%) had a satisfactory lactate clearance (defined as at least a 10% decrease between H0 and H6 [25]) and 187 (56%) had not. The proportion of patients with ScvO2 < 70% at H6 was similar in the case of satisfactory or not satisfactory lactate clearance (22% versus 23%, respectively). Additional file 6: Figure E5 shows the survival curves and the crude death rates at day-28 in four patients’ subgroups according to their lactate clearance and ScvO2 at H0 and H6. On logistic regression, ScvO2 < 70% at H6 was independently associated with day-28 mortality in the subgroup of patients with non satisfactory lactate clearance (OR = 2.32 (1.03, 5.23)) but not in patients with satisfactory lactate clearance (OR = 0.98 (0.21, 4.54)). Additional results for the roles played by initial respiratory conditions, haemoglobin concentration and body temperature in the prevalence of low ScvO2 and mortality are given in Additional file 7.
Discussion
The main finding of our study is that more than one quarter of septic patients had ScvO2 < 70% in the first hours after ICU admission. Furthermore, low ScvO2 in the first hours of ICU admission (and/or 6 hours later) was independently associated with 28-day mortality. These data suggest that one quarter of septic patients admitted to the ICU could be candidates for ICU protocol-based therapy targeting ScvO2.
Prevalence of low ScvO2
In the present multicentre study, using ScvO2 measurements planned as early as possible in routine care, we report a 27% prevalence of low ScvO2 (<70%). This value is below the 40% to 50% prevalence reported in the few, small sized, available prospective studies performed to date in the ICU [9],[10]. These studies analysed selected patients: one study analysed only half of the patients with lactate above 3 mmol/L enrolled in a comparative therapeutic trial [9], and the other study excluded patients with malignancy [10]. However, the 27% prevalence of low ScvO2 we observed in our study with few exclusion criteria represents a non negligible proportion of septic patients and does not support the view that low ScvO2 is uncommon after admission to the ICU [5]-[8].
Importantly, even when classic clinical endpoints of initial resuscitation were achieved (mean blood pressure (BP) >65 mmHg, central venous pressure (CVP) > 8 mmHg and urine output >0.5/ml/Kg) low ScvO2 could not be ruled out as it was observed in one third of our apparently resuscitated patients. Furthermore, arterial lactate also misclassified patients in their low/high contemporaneous ScvO2: the prevalence of ScvO2 < 70% was similar in the case of lactate above or below the median value of 2.2 mmol/L (29% versus 33%; P = 0.3). This underlines that ScvO2 measurement is not interchangeable with these routine clinical and biological data.
Association between low ScvO2 and outcome
As expected, the SAPSII score and the arterial lactate consistently appeared as powerful predictors of day-28 death. Independently of these two well-known predictors [24],[26], low initial ScvO2 was also consistently linked to day-28 mortality. To the best of our knowledge, this has never been previously shown in either emergency department or ICU studies. Of note, our study was not designed to assess whether the link between low ScvO2 and mortality is a causal relationship.
Clinical perspectives
One quarter of our septic patients had low ScvO2 in the first hours of ICU admission and this was associated with poor outcome. This was also the case for persisting low ScvO2 (at 6 hours after the first measurement). These patients could be candidates for ICU protocol-based therapy targeting the ScvO2 in addition to routine initial care. The choice between lactate-guided, ScvO2-guided therapy, or between both, is still under debate [27]. In emergency department septic patients, there is no significant difference in patients’ outcomes when managed either with lactate-guided or ScvO2-guided therapy [28]. Interestingly, our results suggest that, rather than choosing one of these measurements, ScvO2 should be tested in combination with lactate monitoring because low ScvO2 may be present or persist even in the case of low lactate, or in the case of satisfactory lactate clearance (see Figure 3 and Additional file 6). This later finding was also observed in studies performed in emergency department patients in the very early phase of resuscitation: Arnold et al. [29] have shown that 15% of patients with good lactate clearance and 21% of patients with poor lactate clearance had ScvO2 < 70%; in the study by Jones et al. [28], an interventional, randomized trial comparing lactate clearance or ScvO2 > 70% as therapeutic targets, the proportion of patients who did not have normalized ScvO2 was 19% in both groups. This proportion is lower than the one we observed but may not reflect what happens in real conditions, as resuscitation was performed per protocol for the purpose of the randomized trial. For their part, Jansen et al. [9] compared usual care and protocol-based therapy with lactate clearance as a target in an ICU population of septic patients, and showed that at 6 hours, 33% of patients in the intervention group still had ScvO2 < 70% while more than 40% had lactate clearance >20%. Although these findings are consistent with ours, once again they may not reflect the real-life conditions as the patients were treated according to a rigorous and complex protocol. Therefore, to our knowledge, our study is the first to show that ScvO2 and lactate may show non parallel evolutions in septic patients cared for in the ICU in real-life conditions.
The usefulness of protocol-based resuscitation including the normalization of ScvO2 has been recently challenged by the ProCESS trial [30], a randomized trial conducted in emergency departments in the very early phase of resuscitation of septic patients. This study showed no advantage in terms of survival with the protocol-based therapy including the normalization of ScvO2 as compared to usual care [30]. Of note, the ProCESS trial population was quite different from that we studied in our work, in which we estimated the prevalence of ScvO2 and of persisting ScvO2 in ICU patients, after the initial phase of resuscitation. On the other hand, in 1995 Gattinoni et al. [31] also showed that therapy aimed at normalizing the SvO2 value did not lead to better outcome than standard care in a general population of critically ill patients. Their results cannot be transposed to our study population as they included fewer than 25% of septic patients, and included them more than 48 hours after ICU admission [31], a time frame quite different from that used for inclusion in our work. For these reasons we believe it is premature to abandon the concept of normalization of ScvO2 in severely septic patients admitted to the ICU for whom low ScvO2 cannot be neglected, given its association with increased day-28 mortality. Further studies are required to precisely identify which ICU patients would benefit from therapeutic strategies aimed at ScvO2 normalization.
The LOWESS plot (see Additional file 4) used to identify cutoff values of initial ScvO2 illustrates that below ScvO2 of 75%, the lower the ScvO2 the lower was the survival. Hence, ScvO2 < 75% was also associated with day-28 mortality in our multivariate analysis. This cutoff of 75% for worse outcome in our septic patients is higher than that found in cardiac failure patients [32],[33]. This is consistent with the physiopathology of septic shock in which microcirculatory shunts lead to intra-organ oxygen extraction impairment that necessitates maintaining a high level of oxygen delivery to ensure adequate organ oxygen uptake [34]. Beyond the confirmation that ScvO2 of 70% is an important threshold for patient outcome, our study also suggests that, in septic patients, ScvO2 of 75% could be an even more relevant target that best ensures that overall tissue oxygenation is adequate in the context of septic oxygen extraction impairment. However, the thresholds of ScvO2 that could be proposed after the visual inspection of the LOWESS plot were statistically estimated cutoff values in the entire study population that may not apply at the individual level. Therefore, ScvO2 value of 67% for instance does not necessarily place a given patient in a dangerous condition, and conversely an ScvO2 of 73% should not be seen as necessarily reassuring. In fact each individual patient probably has his/her own threshold from which it could be dangerous to deviate, depending on how his/her tissues are trained to extract oxygen in situations of high oxygen demand [35] or insufficient oxygen transport, and depending on the intensity of the microcirculatory shunts [36] linked to the severity of the sepsis process. In relation with this later issue, high values of ScvO2 may reflect the intensity of the microcirculatory derangements caused by sepsis. Some studies have suggested that either ScvO2 higher than 80% within the first 3 days in the ICU [37] or ScvO2 higher than 90% in the emergency department [38], were markers of poor prognosis. Indeed, although our study was underpowered to specifically examine the role of high values of ScvO2, we also observed that, beyond the threshold of 75%, the higher the ScvO2, the lower was the survival (see Additional file 4).
Limitations of the study
First, this study was not designed to seek for the reasons of low ScvO2. Since we have not systematically measured cardiac output, we cannot distinguish between the roles played by too-low oxygen delivery on the one hand and too-high oxygen demand on the other hand. Second, our study was clearly underpowered to draw conclusions about the significance of high ScvO2 values. Third, in view of our inclusion rate, selection bias cannot be definitely ruled out. However, patients were not selected on the basis of the variable of interest (ScvO2), which was not known during the screening/enrolment process. Additionally, enrolled and non enrolled patients’ characteristics were similar (see Additional file 2). Moreover, as shown in Additional file 2, the proportion of patients with low ScvO2 consistently ranged from around 24% to 36% in subgroups of patients classified according to their cardiac or respiratory status, or to the timing and intensity of therapeutic interventions performed before inclusion. Fourth, ScvO2 was not measured by the same method in all participating centres, as four used standard blood gas analysers and six used co-oximeters. This might have distorted the accurate determination of cutoff values of ScvO2, because the limits of agreement between both methods are wide [39]. However, this does not impair the general interpretation of our results as a majority (265/363) of the included patients had ScvO2 measured by co-oximetry and the link between low ScvO2 and day-28 mortality remained statistically significant in this patient subgroup.
Conclusion
Our study demonstrated that, in septic patients, low levels of ScvO2 in the first hours of ICU admission were frequent (<70% for more than one quarter), even when clinical resuscitation endpoints are achieved and even when arterial lactate was normal. Importantly, ScvO2 in the first hours of ICU admission and/or six hours later was linked to day-28 mortality.
Key messages
-
In septic shock patients, low ScvO2 (<70%) is common in the first hours of admission to the ICU
-
In septic shock patients, low ScvO2 (<70%) in the first hours of admission to the ICU is associated with increased day-28 mortality
-
In addition to usual care, ICU protocol-based therapy targeting ScvO2 may be tested in controlled trials in septic patients with low or persisting low ScvO2 in the first hours of ICU admission
Authors’ information
Clinical Research in Intensive Care and Sepsis (CRICS) Group (http://www.crics.fr).
Additional files
Abbreviations
- LOWESS:
-
locally weighted scatterplot smoothing
- OR:
-
adjusted odds ratios
- SAPSII:
-
Simplified acute physiology score
- ScvO2:
-
central venous oxygen saturation
- SvO2:
-
mixed venous oxygen saturation
References
Rady MY, Rivers EP, Nowak RM: Resuscitation of the critically ill in the ED: responses of blood pressure, heart rate, shock index, central venous oxygen saturation, and lactate. Am J Emerg Med. 1996, 14: 218-225. 10.1016/S0735-6757(96)90136-9.
Dueck MH, Klimek M, Appenrodt S, Weigand C, Boerner U: Trends but not individual values of central venous oxygen saturation agree with mixed venous oxygen saturation during varying hemodynamic conditions. Anesthesiology. 2005, 103: 249-257. 10.1097/00000542-200508000-00007.
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M: Early Goal-Directed Therapy Collaborative Group: early goal directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001, 345: 1368-1377. 10.1056/NEJMoa010307.
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb SA, Beale RJ, Vincent JL, Moreno R: Surviving Sepsis Campaign Guidelines Committee including the Pediatric Subgroup. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013, 41: 580-637. 10.1097/CCM.0b013e31827e83af.
Bellomo R, Reade MC, Warrillow SJ: The pursuit of a high central venous oxygen saturation in sepsis: growing concerns. Crit Care. 2008, 12: 130-10.1186/cc6841.
Perel A: Bench-to-bedside review: the initial hemodynamic resuscitation of the septic patient according to Surviving Sepsis Campaign guidelines–does one size fit all?. Crit Care. 2008, 12: 223-10.1186/cc6979.
Peake S, Webb S, Delaney A: Early goal-directed therapy of septic shock: we honestly remain skeptical. Crit Care Med. 2007, 35: 994-995. 10.1097/01.CCM.0000257481.37623.3B.
van Beest PA, Hofstra JJ, Schultz MJ, Boerma EC, Spronk PE, Kuiper MA: The incidence of low venous oxygen saturation on admission to the intensive care unit: a multi-center observational study in The Netherlands. Crit Care. 2008, 12: R33-10.1186/cc6811.
Jansen TC, van Bommel J, Schoonderbeek FJ, Sleeswijk Visser SJ, van der Klooster JM, Lima AP, Willemsen SP, Bakker J: Early lactate-guided therapy in intensive care unit patients: a multicenter, open-label, randomized controlled trial. Am J Respir Crit Care Med. 2010, 182: 752-761. 10.1164/rccm.200912-1918OC.
Chung KP, Chang HT, Huang YT, Liao CH, Ho CC, Jerng JS, Yu CJ: Central venous oxygen saturation under non-protocolized resuscitation is not related to survival in severe sepsis or septic shock. Shock. 2012, 38: 584-591. 10.1097/SHK.0b013e318274c674.
Bracht H, Hänggi M, Jeker B, Wegmüller N, Porta F, Tüller D, Takala J, Jakob SM: Incidence of low central venous oxygen saturation during unplanned admissions in a multidisciplinary intensive care unit: an observational study. Crit Care. 2007, 11: R2-10.1186/cc5144.
Pope JV, Jones AE, Gaieski DF, Arnold RC, Trzeciak S, Shapiro NI: Multicenter study of central venous oxygen saturation (ScvO(2)) as a predictor of mortality in patients with sepsis. Ann Emerg Med. 2010, 55: 40-46. 10.1016/j.annemergmed.2009.08.014.
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G: 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003, 31: 1250-1256. 10.1097/01.CCM.0000050454.01978.3B.
McCabe WR, Jackson GG: Gram-negative bacteremia I. Etiology and ecology. Arch Intern Med. 1962, 110: 847-891. 10.1001/archinte.1962.03620240029006.
Akaike H: A new look at statistical model identification. IEEE Trans Automat Contr. 1974, 19: 716-722. 10.1109/TAC.1974.1100705.
Vincent JL, de Mendonça A, Cantraine F, Moreno R, Takala J, Suter PM, Sprung CL, Colardyn F, Blecher S: Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Med. Crit Care Med. 1998, 26: 1793-1800. 10.1097/00003246-199811000-00016.
Loi 2004-806 (August 9, 2004) relative à la politique de santé publique. J French Repub. 2004, 185: 14277-
Antonelli M, Levy M, Andrews PJ, Chastre J, Hudson LD, Manthous C, Meduri GU, Moreno RP, Putensen C, Stewart T, Torres A: Hemodynamic monitoring in shock and implications for management. International Consensus Conference, Paris, France, 27-28 April 2006. Intensive Care Med. 2007, 33: 575-590. 10.1007/s00134-007-0531-4.
Pottecher T, Calvat S, Dupont H, Durand-Gasselin J, Gerbeaux P: Hemodynamic management of severe sepsis: recommendations of the French Intensive Care’ Societies (SFAR/SRLF) Consensus Conference, 13 October 2005, Paris. France Crit Care. 2006, 10: 311-10.1186/cc4658.
DerSimonian R, Laird N: Meta-analysis in clinical trials. Control Clin Trials. 1986, 7: 177-188. 10.1016/0197-2456(86)90046-2.
Cleveland WS, Devlin SJ: Locally-weighted regression: an approach to regression analysis by local fitting. J Am Stat Assoc. 1988, 83: 596-610. 10.1080/01621459.1988.10478639.
Boulain T, Runge I, Benzekri-Lefèvre D, Mathonnet A, Bretagnol A, Fleury C: Saturation veineuse cave supérieure (ScvO2) à la prise en charge du sepsis sévère en réanimation : fréquence des valeurs basses [Abstract]. Reanimation. 2011, 20: S226-10.1007/s13546-011-0230-6.
R Core Team: R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2013. ISBN 3-900051-07-0 [], [http://www.R-project.org/]
Le Gall JR, Lemeshow S, Saulnier F: A new simplified acute physiology score (SAPS II) based on a European/north American multicenter study. JAMA. 1993, 270: 2957-2963. 10.1001/jama.1993.03510240069035.
Nguyen HB, Rivers EP, Knoblich BP, Jacobsen G, Muzzin A, Ressler JA, Tomlanovich MC: Early lactate clearance is associated with improved outcome in severe sepsis and septic shock. Crit Care Med. 2004, 32: 1637-1642. 10.1097/01.CCM.0000132904.35713.A7.
Mikkelsen ME, Miltiades AN, Gaieski DF, Goyal M, Fuchs BD, Shah CV, Bellamy SL, Christie JD: Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock. Crit Care Med. 2009, 37: 1670-1677. 10.1097/CCM.0b013e31819fcf68.
Marik PE, Bellomo R: Lactate clearance as a target of therapy in sepsis: a flawed paradigm. OA Critical Care. 2013, 1: 3-10.13172/2052-9309-1-1-431.
Jones AE, Shapiro NI, Trzeciak S, Arnold RC, Claremont HA, Kline JA: Lactate clearance vs central venous oxygen saturation as goals of early sepsis therapy: a randomized clinical trial. JAMA. 2010, 303: 739-746. 10.1001/jama.2010.158.
Arnold RC, Shapiro NI, Jones AE, Schorr C, Pope J, Casner E, Parrillo JE, Dellinger RP, Trzeciak S: Multicenter study of early lactate clearance as a determinant of survival in patients with presumed sepsis. Shock. 2009, 32: 35-39. 10.1097/SHK.0b013e3181971d47.
Investigators PCESS, Yealy DM, Kellum JA, Huang DT, Barnato AE, Weissfeld LA, Pike F, Terndrup T, Wang HE, Hou PC, LoVecchio F, Filbin MR, Shapiro NI, Angus DC: A randomized trial of protocol-based care for early septic shock. N Engl J Med. 2014, 370: 1683-1693. 10.1056/NEJMoa1401602.
Gattinoni L, Brazzi L, Pelosi P, Latini R, Tognoni G, Pesenti A, Fumagalli R: A trial of goal-oriented hemodynamic therapy in critically ill patients. SvO2 Collaborative Group. N Engl J Med. 1995, 333: 1025-1032. 10.1056/NEJM199510193331601.
van Beest P, Wietasch G, Scheeren T, Spronk P, Kuiper M: Clinical review: use of venous oxygen saturations as a goal - a yet unfinished puzzle. Crit Care. 2011, 15: 232-10.1186/cc10351.
Gallet R, Lellouche N, Mitchell-Heggs L, Bouhemad B, Bensaid A, Dubois-Randé JL, Gueret P, Lim P: Prognosis value of central venous oxygen saturation in acute decompensated heart failure. Arch Cardiovasc Dis. 2012, 105: 5-12. 10.1016/j.acvd.2011.10.005.
Astiz ME, Rackow EC, Falk JL, Kaufman BS, Weil MH: Oxygen delivery and consumption in patients with hyperdynamic septic shock. Crit Care Med. 1987, 15: 26-28. 10.1097/00003246-198701000-00005.
Kalliokoski KK, Oikonen V, Takala TO, Sipila H, Knuuti J, Nuutila P: Enhanced oxygen extraction and reduced flow heterogeneity in exercising muscle in endurance-trained men. Am J Physiol Endocrinol Metab. 2001, 280: E1015-E1021.
Ellis CG, Bateman RM, Sharpe MD, Sibbald WJ, Gill R: Effect of a maldistribution of microvascular blood flow on capillary O(2) extraction in sepsis. Am J Physiol Heart Circ Physiol. 2002, 282: H156-H164.
Textoris J, Fouché L, Wiramus S, Antonini F, Tho S, Martin C, Leone M: High central venous oxygen saturation in the latter stages of septic shock is associated with increased mortality. Crit Care. 2011, 15: R176-10.1186/cc10325.
Ho BC, Bellomo R, McGain F, Ones D, Naka T, Wan L, Braitberg G: The incidence and outcome of septic shock patients in the absence of early-goal directed therapy. Crit Care. 2006, 10: R80-10.1186/cc4918.
Subramanian G, Anitha VP, Ranjit S: Comparison of central venous saturation by standard ABG machine versus co-oximeter: Is 18 carat as good as the 24 carat gold standard` . Indian J Crit Care Med. 2013, 17: 82-86. 10.4103/0972-5229.114824.
Acknowledgments
We are indebted to all participating investigators who collected data and cared for study patients: Olivier Baudin, Sylvie Calvat, Christophe Cracco, Arnaud Desachy, Charles Lafon (Angoulême, CRICS group); Emmanuelle Boitrou, Hervé Mentec, Olivier Pajot, Gaëtan Plantefève, Marina Thirion (Argenteuil, CRICS group); Rémi Bruyère, Jean-Pierre Quenot (Dijon, CRICS group); Konstantinos Bachoumas, Maud Fiancette, Jean Claude Lacherade, Jean Baptiste Lascarrou, Christine Lebert, Laurent Martin-Lefèvre, Jean Reignier, Isabelle Vinatier, Aihem Yehia (La Roche sur Yon, CRICS group); Emmanuelle Begot, Remy Bellier, Marc Clavel, Bruno François, Antoine Galy, Nicolas Pichon, Philippe Vignon (Limoges, CRICS group); Patrick Bardou, Michel Bonnivard, Anne Marco, Jérôme Roustan, Sylvie Vimeux (Montauban, CRICS group); Anne Bretagnol, Armelle Mathonnet, Dalila Benzekri, Nicolas Bercault, Thierry Boulain, Toufik Kamel, Grégoire Muller, François Réminiac, Isabelle Runge, Marie Skarzynski (Orléans, CRICS group); Delphine Chatellier, Rémi Coudroy, Jean-Pierre Frat, Véronique Goudet, René Robert, Anne Veinstein (Poitiers, CRICS group); Vlad Botoc, Stéphanie Chevalier, François Collet, Jean-Paul Gouello (Saint-Malo); Julie Badin, Pierre-François Dequin, Denis Garot, Antoine Guillon, Annick Legras, Elodie Masseret, Emmanuelle Mercier, Patrice Talec, (Tours, CRICS group).
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
TB conceived and coordinated the study, obtained funding, participated in the acquisition, analysis and interpretation of data, performed the statistical analysis and drafted the manuscript. DG participated to the study design, participated to the acquisition, analysis and interpretation of data, and helped to draft the manuscript. PV participated in the study design and acquisition, analysis and interpretation of data, and helped to draft the manuscript. AM, JBL, AD, VB, AF, JPF, FB and JPQ all participated in the study design and the acquisition, analysis and interpretation of data. PFD participated in the study design and the acquisition, analysis and interpretation of data, and helped to draft the manuscript. All authors read and approved the final manuscript.
Electronic supplementary material
13054_2014_609_MOESM2_ESM.pdf
Additional file 2: Comparison of enrolled and non enrolled patients and proportions of patients with low central venous oxygen saturation (S cv O 2 ) in patients’ subgroups. (PDF 220 KB)
13054_2014_609_MOESM3_ESM.pdf
Additional file 3: Inclusion delays and resuscitation before inclusion: influence on central venous oxygen saturation (S cv O 2 ). (PDF 77 KB)
13054_2014_609_MOESM4_ESM.pdf
Additional file 4: Association between central venous oxygen saturation (S cv O 2 ) and day-28 survival as assessed by locally weighted scatterplot smoothing (LOWESS) plot. (PDF 93 KB)
13054_2014_609_MOESM5_ESM.pdf
Additional file 5: Thresholds of central venous oxygen saturation (S cv O 2 ) and mortality: bivariate and multivariate analyses. (PDF 96 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Boulain, T., Garot, D., Vignon, P. et al. Prevalence of low central venous oxygen saturation in the first hours of intensive care unit admission and associated mortality in septic shock patients: a prospective multicentre study. Crit Care 18, 609 (2014). https://doi.org/10.1186/s13054-014-0609-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-014-0609-7