Abstract
Proteins and amino acids are widely considered to be subcomponents in nutritional support. However, proteins and amino acids are fundamental to recovery and survival, not only for their ability to preserve active tissue (protein) mass but also for a variety of other functions. Understanding the optimal amount of protein intake during nutritional support is therefore fundamental to appropriate clinical care. Although the body adapts in some ways to starvation, metabolic stress in patients causes increased protein turnover and loss of lean body mass. In this review, we present the growing scientific evidence showing the importance of protein and amino acid provision in nutritional support and their impact on preservation of muscle mass and patient outcomes. Studies identifying optimal dosing for proteins and amino acids are not currently available. We discuss the challenges physicians face in administering the optimal amount of protein and amino acids. We present protein-related nutrition concepts, including adaptation to starvation and stress, anabolic resistance, and potential adverse effects of amino acid provision. We describe the methods for assessment of protein status, and outcomes related to protein nutritional support for critically ill patients. The identification of a protein target for individual critically ill patients is crucial for outcomes, particularly for specific subpopulations, such as obese and older patients. Additional research is urgently needed to address these issues.
Similar content being viewed by others
Introduction
Proteins and amino acids (AAs) play a major role in the maintenance of body homeostasis and their metabolism in critically ill patients has been intensively researched over the past 40 years. In contrast, few studies of optimal protein or AA intake have been conducted in patients requiring nutritional support [1]. This review highlights the importance of protein in nutritional support for critically ill patients and provides the rationale for conducting additional, much-needed studies to improve protein and AA nutritional support.
In this review, protein intake refers to enteral nutrition, AA intake refers to parenteral nutrition (PN), and nitrogen (N) generally refers to metabolism and overall N balance. The administration of AA at pharmacological levels (for example, glutamine, arginine) is not discussed in detail because a number of reviews and meta-analyses have been published recently on this topic [2]-[4].
A historical perspective
Protein nutrition, provided by intravenous AA infusion, has been used for more than 70 years [5] and it was believed that insufficient intravenous energy provision prevented the efficient use of these AAs [6]. Infusion of hypertonic glucose through a central venous catheter was first described in 1955 [7] and indwelling catheters, hypertonic glucose, protein hydrolysates, and other nutrients were used successfully on a limited clinical basis over the next 10 years. Dudrick and colleagues demonstrated that all nutrients necessary for growth could be provided by intravenous feeding [8]. Over the following decade, research focused on accurately defining nutritional requirements, particularly for micronutrients, and on the technical aspects of adequate intravenous delivery of energy or AAs. As it became technically possible to deliver more nonprotein energy intravenously, the problem of overfeeding arose. One adverse effect of overfeeding is the deposition of fat in the liver, particularly in patients receiving total PN for reversal of the catabolic response to critical illness [9],[10].
The progressive and rapid loss of body mass and muscle well known to occur in patients with critical illness was termed hypermetabolism. The view at the time was that critically ill patients have very high energy expenditure and therefore require high-energy nutrition. Septic autocannibalism was a term used to describe the loss of muscle mass that does not benefit from increasing AA provision above minimum requirements [11]. Therefore, through the 1970s, researchers focused on ensuring that energy intake exceeded expenditure, rather than on targets for adequate protein intake [9]. Later, when enteral nutrition became a viable option in critically ill patients, nutritional interventions continued to focus on meeting energy requirements. When recommendations for protein or AA intake were given, they were generally expressed as a function of energy intake. For example, in the 1990s the American College of Chest Physicians recommended that, for patients in ICUs, `15-20% of the total calories administered per day can be given as protein or amino acids' [10]. However, the guidelines provided neither the rationale nor the scientific basis for this recommendation.
As we move further into the 21st century, our understanding of the importance of protein nutrition in critically ill patients is increasing. However, further research is needed to better define the optimal intake of protein, in the same way that total energy requirements are defined at present.
Important protein-related concepts: a metabolic perspective
Adaptation to starvation
In a healthy person, an inadequate supply of protein and energy (that is, semi-starvation or full starvation) results in protein energy malnutrition. Semi-starvation induces metabolic adaptations in protein metabolism that limit the rate at which lean mass is lost [12],[13]. When energy supplies fall short in a healthy person, physical activity is reduced to maintain an energy balance. However, a decrease in activity to some extent counteracts the adaptations that limit the loss of lean mass. During starvation, heart and lung muscle may initially be preferentially spared and a disproportionate amount of peripheral skeletal muscle is lost. Ultimately, however, the essential muscle mass of vital organs will also be reduced and, in combination with underused peripheral skeletal muscle, results in muscle weakness and functional disability [12],[13]. These adaptive responses may be considered successful because they allow humans to survive limited periods of starvation. However, if protein and energy provisions continue to remain inadequate, essential bodily functions, such as the immune system, will be adversely affected. Impaired immune function may lead to an increased risk of infections, which in starvation is often seen as a direct cause of death. Starvation has serious implications for a healthy individual, which are even more pronounced in critically ill patients, especially those with a low body mass index [14].
Adaptation of protein and amino acid metabolism under conditions of stress
Humans have developed survival systems during metabolic stress, such as AA use for gluconeogenesis and acute phase protein reactions, increased protein turnover, and adapted regulation by catabolic hormones. In stress situations, the priority of the metabolic response is to provide energy to both the brain and injured tissues to promote healing [15],[16]. Humans have very limited glucose stores and cannot synthesize glucose from fat. Therefore, in the absence of glucose intake, glucose is synthesized from gluconeogenic AA, lactate, and pyruvate. In the starving healthy individual, glucose infusion inhibits gluconeogenesis. In stress situations, however, gluconeogenesis is not readily reversed by glucose infusion, implying that N may be lost through ureagenesis. The pool of free essential AAs is very small, with most generated from net proteolysis, occurring particularly within muscles [17]. In critically ill patients, in parallel with the severity of the injury, increases in proinflammatory cytokines, glucocorticoids, and oxidative stress reinforce the effect of catabolic hormones, and contribute to insulin resistance and muscle wasting [18],[19]. Insulin resistance is common in critically ill patients [20], and contributes to net muscle protein catabolism and liver gluconeogenesis (see Anabolic resistance).
In critically ill patients, a fraction of the essential AAs arising from protein breakdown is oxidized in muscle at an increased rate, in particular branched-chain AAs, while another fraction is released into the blood at an accelerated rate and rapidly cleared by organs such as the liver. In general, there is a unidirectional flux of all AAs from muscle to liver, controlled by hormones. Cortisol promotes net muscle proteolysis and AA release, while glucagon promotes AA uptake by the liver and AA use in gluconeogenesis [21]. In the liver there is a large increase in AA uptake for gluconeogenesis and for protein synthesis, including the synthesis of acute phase proteins [22],[23]. Some AAs are also taken up selectively by other tissues for specific purposes. For example, glutamine is taken up by the kidneys (to sustain ammoniagenesis and counteract acidosis), by fibroblasts and enterocytes (for healing), and by immune cells (for replication and action) [24].
As long as these processes remain adaptive, plasma AA levels remain stable and in balance. However, when the stress response becomes too intense and persists for too long, the balanced AA profile in plasma is disrupted, resulting in abnormal AA concentrations (both higher and lower levels than normal) [25]-[27]. In particular, plasma glutamine concentrations have been associated with unfavorable outcomes in critically ill patients [28],[29].
Under stress conditions, the various alterations in protein metabolism are reflected by an increase in whole-body protein turnover [30],[31] and an increase in AA oxidation and N loss. Since all proteins within the body have specific functions (see Table 1), they cannot be considered a form of AA storage, highlighting the importance of exogenous sources of protein or AA by nutritional support.
Muscle proteins
Muscle proteins are in a constant state of turnover and the balance between the rates of protein breakdown and synthesis determines whether there is a net gain (anabolism) or a net loss (catabolism, wasting). A number of circumstances (for example, burn injury, trauma complicated with sepsis, head trauma) result in loss of muscle mass driven by an accelerated rate of protein breakdown [32]. The increased release of AAs from protein breakdown provides a stimulus for accelerated muscle protein synthesis [33]. Protein synthesis cannot match the increased rate of muscle protein breakdown, although protein synthesis rates do vary significantly from patient to patient [22],[34].
In a stress situation, the catabolic loss of muscle can be avoided only if the uptake of AAs from the blood is increased either by intravenous infusion or the digestion of enterally administered proteins, peptides, or AAs. These sources of AA may then stimulate protein synthesis to offset the accelerated rate of protein breakdown and AA oxidation [22],[35],[36].
Anabolic resistance
Anabolic resistance refers to the state in which a patient is resistant to the normal stimulatory effect of AAs on muscle protein synthesis. This is common in older patients and may contribute to the estimated 1.4 to 2.5% muscle loss per year in that group [37]. Anabolic resistance is also frequently observed in critically ill patients [38], in patients on bed rest, or in people exposed to weightless environments (such as in space) [39]. Three main factors explain anabolic resistance: splanchnic sequestration of AAs following feeding [40],[41], which decreases the AAs available to muscles; insulin resistance, which limits AA uptake into muscles [42] and hinders the maintenance of muscle protein [39]; and blunted responses to AAs with anabolic properties, such as the essential AA leucine [19],[43]. The older patients require a higher intake of essential AAs compared with the young to generate the same acute response [42]. However, there is a lack of data on AA requirements in older patients in the ICU; these requirements warrant urgent research, since the number of older patients in the ICU is likely to increase in parallel with that of the general population. Muscle protein anabolism can be optimized in otherwise healthy individuals by a combination of adequate protein or AA intake, combined with exercise and insulin [44].
Anabolic resistance is also driven by insensitivity to the normal anabolic action of leucine. In stressed patients, the level of muscle-free leucine is higher than in patients without stress [25],[45],[46]. Experimental models show that leucine stimulates protein synthesis via signaling through the mammalian target of rapamycin system [47]. Leucine and insulin share common pathways for activating protein synthesis, suggesting that signal transduction is impaired somewhere within the mammalian target of rapamycin pathway. However, there may be differences in the acute and prolonged effects of leucine supplementation [48]. Research into the role of leucine in different clinical settings has potential implications for the treatment of muscle loss in metabolically stressed patients.
Interaction of protein with nonprotein energy
The efficiency of protein intake in stimulating protein synthesis is dependent to some extent on the level and nature of the nonprotein energy intake. Many nutritional guidelines for macronutrient intake during nutritional support are derived from requirements for healthy individuals. It has been known for almost 100 years that the amount of protein intake required to maintain N balance in healthy individuals is a function of the amount of concomitant energy intake [49]. Meeting energy requirements is a major goal of appropriate nutrition support. However, delivering excessive energy to severely stressed patients usually fails to enhance the retention of body protein [50] and often causes adverse effects, such as severe fatty infiltration of the liver [51]. In a catabolic state, loss of lean body mass (LBM) often cannot be entirely prevented by nutrition support.
The realistic aim of nutrition support is to blunt the loss of LBM, and the goal should be to supply the amount and nature of protein or AA intake that can maximally stimulate protein synthesis [52]. Even in the insulin-resistant state, AAs can stimulate, to some extent, muscle protein synthesis [53]. The provision of adequate, but not excessive, nonprotein energy may provide some benefit to stressed patients. The potential for detrimental effects is considerable, however, and care should be taken to avoid supplying nonprotein energy in excess of energy expenditure.
Amino acid transport
The first step in AA processing is cellular uptake, and many different AA transporters occur in different cell types [54]. There are also transporters that cycle certain AAs between the cytosol and mitochondria. For example, the ureagenesis pathway transports ornithine from the cytosol to mitcohondria and citrulline from mitochondria to the cytosol [55]. One transporter may take up several AAs, and a single AA may have more than one transporter. Consequently, some AAs compete with each other for cellular uptake and the provision of an imbalanced AA solution may lead to an inappropriate cellular response. The pharmacokinetic properties of any new AA formula should therefore be tested, as well as the quantity and quality of the AA formulation.
Potential adverse effects of amino acid provision
Most AAs are precursors of neuromediators or of false neuromediators (that is, AAs or metabolites able to bind to neuroreceptors, eliciting or blocking the messages of the true mediators). Administration of large nonphysiologic amounts of AA may lead to seizures and brain damage [56]. Defining an upper limit of safe intake for each AA is therefore of utmost importance [57]. This has been achieved for leucine, which has an upper limit of safe intake of 0.53 g/kg body weight/day in healthy subjects [58]. Of note, this level of leucine intake is well above the normal requirement. There is currently no recommendation concerning the safety of leucine administration in patients, due to the lack of dose-ranging studies. Tolerability varies from one AA to another [59]. Some AAs appear extremely safe even when given in the 15 to 30 g/day range (for example, glutamine, citrulline) [24], at least in the short term [60], whereas tolerance to other AAs (for example, methionine) seems limited [61]. At present, the safety of arginine in ICU patients is a topic of some debate [62],[63].
Methods for assessment of protein status
Nitrogen balance
The N balance is commonly used as the basis for estimating protein requirements in healthy individuals [64],[65] and in patients [66]-[68]. The N balance becomes negative when intake falls short of the minimum protein requirement, leading to loss of LBM. In an otherwise healthy person, however, a chronic low-protein diet may lead to adaptation to a stable overall N balance [69].
Estimation of both N intake and N loss presents challenges that must be considered carefully [70]. While N intake can be accurately measured in patients supported with total enteral nutrition or PN, the assessment of oral dietary protein intake is extremely difficult in clinical practice. Measuring N loss is also problematic, because it is not easy to collect complete 24-hour urine samples, especially in patients with large fecal or urinary output (for example, those with burns or a bone marrow transplant) [71]. In the critically ill patient, total body N loss from urinary urea content underestimates N loss as these patients have an increase in ammonia loss not accounted for in N calculations from urinary urea [72],[73]. Therefore, in ICU patients, total urinary N loss should be measured directly rather than estimated from urinary urea. However, even direct measurements of urinary loss do not reflect the total loss, as they do not include N loss from diarrhea, fistulas, or draining wounds [71].
A positive N balance is not synonymous with improved protein balance, as the N balance after administration of a load of a single AA may simply reflect cellular accumulation of the free AA [74]. In addition, for critically ill patients, intravenous administration of protein-containing blood products confounds N-balance assessments. Nevertheless, measurement of urinary N loss and calculation of N balance remains the most commonly used biomarker to assess protein accretion or loss in ICU patients. Additional information on plasma and urinary levels of conventional markers of protein status is provided in Table 2.
Assessment of qualitative and quantitative amino acid requirements
AA requirements may be assessed by simple pharmacokinetic studies. The balance between the requirement for and intake of an AA can be assessed by measuring the plasma concentration of that specific AA in the basal state and at various times during AA administration. Several studies, summarized in 2003 [85], indicate that during continuous parenteral administration of AAs there is a sharp increase in AA levels followed by a plateau that lasts several hours. The level of the plateau appears to be related to the rate of infusion of each AA [85]. It is therefore possible to construct a one-compartment model with first-order elimination kinetics [86] to study the relationship between the increase in plasma AA concentration and the rate of infusion for any AA. This model was tested in surgical ICU patients. In ICU patients receiving a more individualized AA solution, based on the dynamic test described above, abnormal changes in AA levels were almost eliminated, while they persisted in the control group. The 5-day N balance was significantly improved with this individualized kinetic approach in the surgical ICU study [87]. These studies suggest that, in the future, AA solutions for PN should be formulated for specific disease states. However, the concepts demonstrated by this kinetic approach will need to be validated by additional prospective clinical studies.
Whole-body and muscle protein synthesis
Estimation of N balance is a black-box approach that provides no information about underlying mechanisms, such as variations of protein synthesis and breakdown at the whole-body or tissue level. An alternative approach is to quantify protein needs and determine appropriate protein provision by measuring protein synthesis in the whole body and/or muscle.
AA tracers are commonly used in clinical research. They are created by incorporating stable isotopes of carbon, hydrogen, or N into an AA to produce a uniquely identifiable molecule. Labeled AAs can be administered in small amounts by infusion or ingestion to trace the metabolism of the more abundant form of the AA in the body. Mass spectrometry analysis of the AA tracer in blood or protein enables the calculation of whole-body protein synthesis and whole-body protein breakdown. All proteins in the body, including muscle, will incorporate the labeled AA at rates that reflect the fractional synthetic rate of the protein [88].
The muscle fractional synthetic rate reflects only the synthetic rate of muscle protein. The net gain or loss of protein is determined by the balance between its rate of synthesis and its rate of breakdown. However, the muscle fractional protein breakdown rate is not commonly assessed because it requires a more complicated experimental protocol, additional blood sampling, and complex calculations, especially during feeding [89]. One approach to calculating muscle protein synthesis and breakdown is to measure the balance of specific AAs across the leg or arm [90]. This requires arterial and venous catheterization and measurement of tissue blood flow. When combined with muscle tissue biopsy data, the rates of muscle protein synthesis, breakdown, and net balance can be calculated. In addition, the rate of AA uptake and release into blood can be measured [90]. Differences in limb blood flow may alter the measured arteriovenous balance, however, limiting the applicability of this technique.
In a research setting, whole-body protein synthesis and breakdown can also be measured in response to protein feeding or PN. One commonly used approach is the addition of phenylalanine/leucine to a meal, together with an infusion of labeled tyrosine and phenylalanine, followed by blood sampling [88]. An advantage of this approach is that muscle biopsies are not required, and frequent blood sampling enables calculations of both synthesis and breakdown during protein or AA absorption. While tracer methods have been used to study the acute response of whole-body or protein synthesis in metabolically stressed patients, a systematic investigation of protein synthesis and breakdown has not yet been performed. An appropriately designed isotopic study providing direct evidence for the protein needs of critically ill patients would be of great value.
Muscle mass and lean body mass
Measurement of LBM (that is, fat-free mass, including extracellular fluid) over time should provide important insights into an individual patient's requirement for protein intake. However, attempts to measure LBM easily and accurately at the bedside in the ICU have to date been unsuccessful. It is important to determine which body-compartment measurement best reflects the daily amount of protein needed to maintain equilibrium. Total body mass is not useful because the varying amounts of fat mass are not relevant to protein metabolism. Also, standard body weight or ideal body weight measurements are not appropriate as they lead to imprecise estimates in obese patients [91]. The most appropriate compartments for determining protein requirements are LBM and body cell mass (that is, the sum of all living cells excluding extracellular fluid and bone mass). Both of these compartments can be measured in clinical practice using bioelectrical impedance analysis [92],[93]. However, the overall precision of bioelectrical impedance analysis may be reduced by variations in hydration status. Dual-energy X-ray absorptiometry [94] can be used to assess LBM, although dual-energy X-ray absorptiometry scanners are not available in every hospital and are not routinely used for critically ill patients.
Computed tomography (CT) may also be used to assess LBM [95]. Specialized CT software has been used at the third lumbar spine to determine the area of skeletal muscle, as well as subcutaneous, intramuscular, and visceral adipose tissue. A lower LBM, as determined by CT imaging at the third lumbar spine, is an adverse prognostic factor in patients with pancreatic cancer and sarcopenic obesity [96]. Recently, Moisey and colleagues have demonstrated the prognostic value of LBM for predicting mortality in critically ill, older, sarcopenic, injured patients [97]. Weijs and colleagues confirmed these findings in a population with a much broader age range and mixed diagnoses [98].
Since CT scanning technology exists in most hospitals and many hospital patients undergo an abdominal CT scan, analysis of skeletal muscle in a single CT slice could be carried out routinely. However, routine use of CT scanning for patients in the ICU remains a difficult logistical problem. Bedside ultrasound imaging could also be used to measure muscle thickness, avoiding the potential issues associated with radiation doses from CT scans. However, additional research is needed to develop a reliable and sensitive technique for assessing LBM [99] and these methods require validation in this setting [68]. The report of muscle wasting in ICU patients by Puthucheary and colleagues highlights the importance of monitoring [34]. Recent studies have provided preliminary data showing a statistical relationship between muscle wasting and protein intake [100],[101]. However, muscle mass varies too slowly to be used as a day-to-day tool for fine-tuning protein intake.
Protein nutrition support and outcome in critically ill patients
Muscle wasting and functional impairment
As outlined above, body protein from functional tissues is catabolized during critical illness and may culminate in a clinically significant loss of muscle mass [34]. The extent of muscle mass loss may impact the ultimate prognosis of an individual. Significantly reduced muscle mass often leads to impaired functioning, which hinders activities such as weaning from the ventilator and muscle function recovery. These adverse outcomes can result in increased nosocomial infection, such as pneumonia, bacteremia, and wound infection, leading to a renewed state of increased catabolism. This vicious cycle is associated with poor patient outcomes. Functional disability may be long term and may never fully return to normal levels [102],[103]. The increased efflux of AAs from catabolic muscle also places a metabolic burden on the liver. Therefore, in highly catabolic states of muscle protein breakdown, it is clinically important that the liver clearance of AAs for protein synthesis and other metabolic functions remains intact [104],[105].
Pharmacological therapy has the potential to work in concert with dietary protein to ameliorate the rate of muscle loss in critically ill patients. Among others, insulin [106], propranolol [107], and testosterone [108] have all been used successfully in seriously burned patients in conjunction with adequate nutritional support to lessen the extent of muscle protein loss. Pharmacological doses of growth hormone actually stimulate muscle protein synthesis in the critically ill [109]. However, critically ill patients treated with human growth hormone had a higher mortality than untreated patients [110]. In other words, blocking muscle protein breakdown is not recommended if adequate nutritional support is not provided. When feasible, the combination of adequate protein intake with early exercise should be further investigated as a means by which to improve both short-term and long-term outcomes.
Level of protein nutrition support in critically ill patients
Current recommendations advise a protein intake level in critically ill patients of more than 1.2 g/kg/day [111]-[113]. Guidelines are based on results from studies employing N balance and body composition techniques in which protein intake exceeding 1.5 g/kg/day did not provide any advantage [15],[111]-[114]. However, based on N balance data, authors of a systematic and critical review suggested that a level of 2.0 to 2.5 g/kg/day may be safe in many critically ill patients [68]. An observational study of patients with head trauma demonstrated that a higher N intake provided a better short-term N balance, which at best supports the conclusion of safety [115]. Further, a recent study evaluating whole-body protein turnover in adolescent patients given PN reported a protein balance advantage with a protein intake as high as 3.0 g/kg/day [116]. Whether this level of intake is appropriate for adults, however, is unknown. To date there have been no outcome studies providing this level of protein intake to critically ill patients. Even though recommended protein intakes for critically ill patients vary widely, there is a consistent recommendation that protein intake should exceed the levels of 0.8 g/kg/day required by normal, healthy individuals. At present, however, most critically ill adults receive less than one-half of the recommended protein intake (about 0.6 g/kg/day) [14].
Current evidence for protein nutrition support and outcome
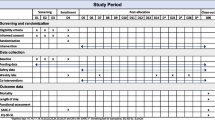
There appears to be a lower than recommended protein provision within the first week of patient admission [14],[68]. The clinical outcomes of several studies reporting protein intake in critically ill patients are summarized in Table 3. Three large prospective trials [117]-[119] investigating the use of evidence-based feeding guidelines in critically ill patients showed no significant difference in mortality, while nonrandomized studies indicate a potential relationship between protein levels in nutrition support and mortality [14],[120]-[122]. These studies suggest that protein supply is of major importance to outcome in critically ill patients.
Randomized trials focusing only on energy provision have not shown an impact on mortality [123]-[125],[127],[129]. Measured energy expenditure may be needed during targeted feeding in the early phase of critical illness to avoid overfeeding, and providing energy at 80 to 90% of energy expenditure may be sufficient [130]. All of the large randomized trials of early PN in critically ill patients have used energy targets based on crude estimations of energy requirements. Hypothetically, a high energy intake may inhibit autophagia, which may be a disadvantage for the critically ill patient, as this enables the accumulation of cellular damage [131]. Whether this inhibition is restricted to patients given PN or whether there is any clinical impact from this observation remains an open question.
No randomized trials to date have adequately studied protein provision in critically ill patients. New studies using whole-body protein kinetics are needed to enable reassessment of the current recommendations [111]-[113]. Protein intake should be tailored to suit the patient, but presently there is no recognized marker available to guide individualized requirements.
In general, if enteral nutrition is possible, early provision is advantageous to the patient [132] as demonstrated in patients following trauma [133]. In patients with sepsis, the evidence is less robust. However, this evidence assumes enteral nutrition can be delivered to meet both protein and energy goals. Randomized trials have shown that the use of early PN did not improve mortality [123],[129]. However, these studies used low protein intake levels compared with current guidelines.
Older studies using the endpoint of N balance or body composition provide less relevant information during the initial phase of critical illness due to the hemodynamic instability of the patient [15],[114]. Further research into the relationship between whole-body (and organ) protein turnover and the level of organ failure and energy expenditure is needed to characterize the status of protein metabolism in the early phase of critical illness before any recommendations can be given [31],[116],[134].
Route of administration
For healthy individuals, the digestion of food demands energy. However, in terms of N balance there is no difference between enteral and parenteral routes of administration. For the critically ill patient the situation is less clear, as it is difficult to characterize digestion and absorption because patients are rarely in a steady state long enough for N-balance studies to be completed. It should be recognized that AAs provided by PN are free, hydrated molecules, and thus the actual amount of protein substrate provided by parenteral AA mixtures is usually overestimated, the amount provided being approximately 20% less than that provided in food protein [68]. For enteral protein, the level of absorption is a complicating factor because it may be low and/or variable [71].
There is no option to store AAs in the body, so the only way to handle excess protein intake is by AA oxidation. Whether or not the oxidation of AA differs in relation to the route of administration is dependent upon nutritional status, the amount of energy, protein, and AA given, and the level of metabolic stress imposed on the subject. Additional studies are needed in critically ill patients to assess gastrointestinal uptake of AAs and to measure whole-body (and organ) protein turnover and AA oxidation for different levels of intake [31],[116],[134].
Conclusions
Nutrition support in the critically ill has to date focused on adequate provision of energy to the patient. Protein and AA provision has been dealt with as a subcomponent of energy supply. However, proteins and AAs are fundamental to recovery and survival, not only to preserve active tissue (protein) mass but also to maintain a variety of other essential functions. The scientific recognition of the importance of protein is growing [68], and although optimal protein dosing studies are not available, expert opinion supports administering in excess of 1.2 g/kg/day [121],[122],[130]. The use of one fixed protein-to-energy ratio to achieve both energy intake and protein intake targets often results in protein underfeeding or energy overfeeding. A mixed approach with a range of enteral or parenteral formulas may therefore help to balance protein and energy targeted feeding [121],[130],[135],[136]. The identification of a target for protein provision for individual patients is a crucial step in recognizing the key role of protein in nutrition support, especially for obese and older patients (with low muscle mass) who are seen in increasing numbers in the ICU. Further research is urgently needed to assess the specific quantitative and qualitative requirements of these patient subgroups.
Abbreviations
- AA:
-
amino acid
- CT:
-
computed tomography
- LBM:
-
lean body mass
- N:
-
nitrogen
- PN:
-
parenteral nutrition
References
Plank LD: Protein for the critically ill patient - what and when?. Eur J Clin Nutr. 2013, 67: 565-568.
Marik PE, Zaloga GP: Immunonutrition in critically ill patients: a systematic review and analysis of the literature. Intensive Care Med. 2008, 34: 1980-1990.
Cynober L, de Bandt JP, Moinard C: Leucine and citrulline: two major regulators of protein turnover. World Rev Nutr Diet. 2013, 105: 97-105.
Cynober L, De Bandt JP: Glutamine in the intensive care unit. Curr Opin Clin Nutr Metab Care. 2014, 17: 98-104.
Elman R, Weiner DO, Bradley E: Intravenous injections of amino-acids (hydrolyzed casein) in postoperative patients. Ann Surg. 1942, 115: 1160-1165.
Shils ME: Guidelines for total parenteral nutrition. JAMA. 1972, 220: 1721-1729.
Merrill JP: The Treatment of Renal Failure. 1955, Grune & Stratton, New York
Dudrick SJ, Wilmore DW, Vars HM, Rhoads JE: Can intravenous feeding as the sole means of nutrition support growth in the child and restore weight loss in an adult? An affirmative answer. Ann Surg. 1969, 169: 974-984.
Wolfe RR, O'Donnell TF, Stone MD, Richmand DA, Burke JF: Investigation of factors determining the optimal glucose infusion rate in total parenteral nutrition. Metabolism. 1980, 29: 892-900.
Cerra FB, Benitez MR, Blackburn GL, Irwin RS, Jeejeebhoy K, Katz DP, Pingleton SK, Pomposelli J, Rombeau JL, Shronts E, Wolfe RR, Zaloga GP: Applied nutrition in ICU patients. A consensus statement of the American College of Chest Physicians. Chest. 1997, 111: 769-778.
Cerra FB, Siegel JH, Coleman B, Border JR, McMenamy RR: Septic autocannibalism. A failure of exogenous nutritional support. Ann Surg. 1980, 192: 570-580.
Hoffer LJ: Clinical nutrition: 1. Protein-energy malnutrition in the inpatient. CMAJ. 2001, 165: 1345-1349.
Cahill GF: Starvation in man. Clin Endocrinol Metab. 1976, 5: 397-415.
Alberda C, Gramlich L, Jones N, Jeejeebhoy K, Day AG, Dhaliwal R, Heyland DK: The relationship between nutritional intake and clinical outcomes in critically ill patients: results of an international multicenter observational study. Intensive Care Med. 2009, 35: 1728-1737.
Ishibashi N, Plank LD, Sando K, Hill GL: Optimal protein requirements during the first 2 weeks after the onset of critical illness. Crit Care Med. 1998, 26: 1529-1535.
Souba WW: Glutamine: a key substrate for the splanchnic bed. Annu Rev Nutr. 1991, 11: 285-308.
Felig P: Amino acid metabolism in man. Annu Rev Biochem. 1975, 44: 933-955.
De Bandt JP, Lim SK, Plassart F, Lucas CC, Rey C, Poupon R, Giboudeau J, Cynober L: Independent and combined actions of interleukin-1 beta, tumor necrosis factor alpha, and glucagon on amino acid metabolism in the isolated perfused rat liver. Metabolism. 1994, 43: 822-829.
Lang CH, Frost RA: Glucocorticoids and TNFα interact cooperatively to mediate sepsis-induced leucine resistance in skeletal muscle. Mol Med. 2006, 12: 291-299.
van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P, Bouillon R: Intensive insulin therapy in critically ill patients. N Engl J Med. 2001, 345: 1359-1367.
Brosnan JT: Interorgan amino acid transport and its regulation. J Nutr. 2003, 133: 2068S-2072S.
Essen P, McNurlan MA, Gamrin L, Hunter K, Calder G, Garlick PJ, Wernerman J: Tissue protein synthesis rates in critically ill patients. Crit Care Med. 1998, 26: 92-100.
Barle H, Gamrin L, Essen P, McNurlan MA, Garlick PJ, Wernerman J: Growth hormone does not affect albumin synthesis in the critically ill. Intensive Care Med. 2001, 27: 836-843.
Roth E: Nonnutritive effects of glutamine. J Nutr. 2008, 138: 2025S-2031S.
Gamrin L, Essen P, Forsberg AM, Hultman E, Wernerman J: A descriptive study of skeletal muscle metabolism in critically ill patients: free amino acids, energy-rich phosphates, protein, nucleic acids, fat, water, and electrolytes. Crit Care Med. 1996, 24: 575-583.
Vesali RF, Klaude M, Rooyackers OE, TJäder I, Barle H, Wernerman J: Longitudinal pattern of glutamine/glutamate balance across the leg in long-stay intensive care unit patients. Clin Nutr. 2002, 21: 505-514.
Gielen M, Vanhorebeek I, Wouters PJ, Mesotten D, Wernerman J, Van den Berghe G, Rooyackers O: Amino acid concentrations in critically ill children following cardiac surgery. Pediatr Crit Care Med. 2014, 15: 314-328.
Oudemans-van Straaten HM, Bosman RJ, Treskes M, van der Spoel HJ, Zandstra DF: Plasma glutamine depletion and patient outcome in acute ICU admissions. Intensive Care Med. 2001, 27: 84-90.
Rodas PC, Rooyackers O, Hebert C, Norberg A, Wernerman J: Glutamine and glutathione at ICU admission in relation to outcome. Clin Sci (Lond). 2012, 122: 591-597.
Jahoor F, Desai M, Herndon DN, Wolfe RR: Dynamics of the protein metabolic response to burn injury. Metabolism. 1988, 37: 330-337.
Berg A, Rooyackers O, Bellander BM, Wernerman J: Whole body protein kinetics during hypocaloric and normocaloric feeding in critically ill patients. Crit Care. 2013, 17: R158-
Wolfe RR: Regulation of skeletal muscle protein metabolism in catabolic states. Curr Opin Clin Nutr Met Care. 2005, 8: 61-65.
Wolfe RR, Miller SL: Amino acid availability controls muscle protein metabolism. Diabetes Nutr Metab. 1999, 12: 322-328.
Puthucheary ZA, Rawal J, McPhail M, Connolly B, Ratnayake G, Chan P, Hopkinson NS, Padhke R, Dew T, Sidhu PS, Velloso C, Seymour J, Agley CC, Selby A, Limb M, Edwards LM, Smith K, Rowlerson A, Rennie MJ, Moxham J, Harridge SD, Hart N, Montgomery HE: Acute skeletal muscle wasting in critical illness. JAMA. 2013, 310: 1591-1600.
Hammarqvist F, Petersson B, Ali MR, Wernerman J: Glutamine in postoperative parenteral nutrition has a positive effect on nitrogen balance. Lakartidningen. 1989, 86: 229-231.
Essen P, McNurlan MA, Wernerman J, Vinnars E, Garlick PJ: Uncomplicated surgery, but not general anesthesia, decreases muscle protein synthesis. Am J Physiol. 1992, 262: E253-E260.
Frontera WR, Hughes VA, Fielding RA, Fiatarone MA, Evans WJ, Roubenoff R: Aging of skeletal muscle: a 12-yr longitudinal study. J Appl Physiol. 2000, 88: 1321-1326.
Rennie MJ: Anabolic resistance in critically ill patients. Crit Care Med. 2009, 37: S398-S399.
Biolo G, Ciocchi B, Lebenstedt M, Barazzoni R, Zanetti M, Platen P, Heer M, Guarnieri G: Short-term bed rest impairs amino acid-induced protein anabolism in humans. J Physiol. 2004, 558: 381-388.
Jourdan M, Deutz NE, Cynober L, Aussel C: Features, causes and consequences of splanchnic sequestration of amino acid in old rats. PLoS One. 2011, 6: e27002-
Boirie Y, Gachon P, Beaufrere B: Splanchnic and whole-body leucine kinetics in young and elderly men. Am J Clin Nutr. 1997, 65: 489-495.
Paddon-Jones D, Sheffield-Moore M, Zhang XJ, Volpi E, Wolf SE, Aarsland A, Ferrando AA, Wolfe RR: Amino acid ingestion improves muscle protein synthesis in the young and elderly. Am J Physiol Endocrinol Metab. 2004, 286: E321-E328.
Dardevet D, Remond D, Peyron MA, Papet I, Savary-Auzeloux I, Mosoni L: Muscle wasting and resistance of muscle anabolism: the `anabolic threshold concept' for adapted nutritional strategies during sarcopenia. Scientific World Journal. 2012, 2012: 269531-
Prod'homme M, Rieu I, Balage M, Dardevet D, Grizard J: Insulin and amino acids both strongly participate to the regulation of protein metabolism. Curr Opin Clin Nutr Metab Care. 2004, 7: 71-77.
Chua HR, Baldwin I, Fealy N, Naka T, Bellomo R: Amino acid balance with extended daily diafiltration in acute kidney injury. Blood Purif. 2012, 33: 292-299.
Hammarqvist F, Wernerman J, Ali R, von der Decken A, Vinnars E: Addition of glutamine to total parenteral nutrition after elective abdominal surgery spares free glutamine in muscle, counteracts the fall in muscle protein synthesis, and improves nitrogen balance. Ann Surg. 1989, 209: 455-461.
Vary TC: Acute oral leucine administration stimulates protein synthesis during chronic sepsis through enhanced association of eukaryotic initiation factor 4G with eukaryotic initiation factor 4E in rats. J Nutr. 2007, 137: 2074-2079.
Van Loon LJ: Leucine as a pharmaconutrient in health and disease. Curr Opin Clin Nutr Metab Care. 2012, 15: 71-77.
Sherman HC: The protein requirement of maintenance in man. Proc Natl Acad Sci U S A. 1920, 6: 38-40.
Hart DW, Wolf SE, Chinkes DL, Beauford RB, Mlcak RP, Heggers JP, Wolfe RR, Herndon DN: Effects of early excision and aggressive enteral feeding on hypermetabolism, catabolism, and sepsis after severe burn. J Trauma. 2003, 54: 755-761. discussion 761-764
Aarsland A, Chinkes DL, Sakurai Y, Nguyen TT, Herndon DN, Wolfe RR: Insulin therapy in burn patients does not contribute to hepatic triglyceride production. J Clin Invest. 1998, 101: 2233-2239.
Evans WJ, Morley JE, Argilés J, Bales C, Baracos V, Guttridge D, Jatoi A, Kalantar-Zadeh K, Lochs H, Mantovani G, Marks D, Mitch WE, Muscaritoli M, Najand A, Ponikowski P, Rossi Fanelli F, Schambelan M, Schols A, Schuster M, Thomas D, Wolfe R, Anker SD: Cachexia: a new definition. Clin Nutr. 2008, 27: 793-799.
Katsanos CS, Aarsland A, Cree MG, Wolfe RR: Muscle protein synthesis and balance responsiveness to essential amino acids ingestion in the presence of elevated plasma free fatty acid concentrations. J Clin Endocrinol Metab. 2009, 94: 2984-2990.
Cynober LA: Plasma amino acid levels with a note on membrane transport: characteristics, regulation, and metabolic significance. Nutrition. 2002, 18: 761-766.
Meijer AJ, Lamers WH, Chamuleau RA: Nitrogen metabolism and ornithine cycle function. Physiol Rev. 1990, 70: 701-748.
Yudkoff M, Daikhin Y, Nissim I, Horyn O, Luhovyy B, Lazarow A, Nissim I: Brain amino acid requirements and toxicity: the example of leucine. J Nutr. 2005, 135: 1531S-1538S.
Cynober L: Introduction to the 5th Amino Acid Assessment Workshop. J Nutr. 2006, 136: 1633S-1635S.
Cynober L, Bier DM, Kadowaki M, Morris SM, Renwick AG: A proposal for an upper limit of leucine safe intake in healthy adults. J Nutr. 2012, 142: 2249S-2250S.
Garlick PJ: The nature of human hazards associated with excessive intake of amino acids. J Nutr. 2004, 134: 1633S-1639S. discussion 1664S-1666S, 1667S-1672S
Holecek M: Side effects of long-term glutamine supplementation. JPEN J Parenter Enteral Nutr. 2013, 37: 607-616.
Garlick PJ: Toxicity of methionine in humans. J Nutr. 2006, 136: 1722S-1725S.
Manzanares W, Heyland DK: Pharmaconutrition with arginine decreases bacterial translocation in an animal model of severe trauma. Is a clinical studied justified?… The time is now!. Crit Care Med. 2012, 40: 350-352.
Cynober L, Moinard C, Charrueau C: If the soup tastes bad, it doesn't mean the potatoes are the culprit. Crit Care Med. 2012, 40: 2540-2541. author reply 2541-2542
Energy and protein requirements. Report of a joint FAO/WHO/UNU Expert Consultation.World Health Organ Tech Rep Ser 1985, 724:1-206.,
Scientific opinion on dietary reference values for protein. EFSA J. 2012, 10: 2557-
Scheinkestel CD, Adams F, Mahony L, Bailey M, Davies AR, Nyulasi I, Tuxen DV: Impact of increasing parenteral protein loads on amino acid levels and balance in critically ill anuric patients on continuous renal replacement therapy. Nutrition. 2003, 19: 733-740.
Singer P: High-dose amino acid infusion preserves diuresis and improves nitrogen balance in non-oliguric acute renal failure. Wien Klin Wochenschr. 2007, 119: 218-222.
Hoffer LJ, Bistrian BR: Appropriate protein provision in critical illness: a systematic and narrative review. Am J Clin Nutr. 2012, 96: 591-600.
Waterlow JC: The nature and significance of nutritional adaptation. Eur J Clin Nutr. 1999, 53: S2-S5.
Furst P, Stehle P: What are the essential elements needed for the determination of amino acid requirements in humans?. J Nutr. 2004, 134: 1558S-1565S.
Wierdsma NJ, Peters JH, Weijs PJ, Keur MB, Girbes AR, van Bodegraven AA, Beishuizen A: Malabsorption and nutritional balance in the ICU: fecal weight as a biomarker: a prospective observational pilot study. Crit Care. 2011, 15: R264-
Milner EA, Cioffi WG, Mason AD, McManus WF, Pruitt BA: Accuracy of urinary urea nitrogen for predicting total urinary nitrogen in thermally injured patients. JPEN J Parenter Enteral Nutr. 1993, 17: 414-416.
Cynober L, Coudray-Lucas C: Urinary urea nitrogen prediction of total urinary nitrogen. JPEN J Parenter Enteral Nutr. 1995, 19: 174-
Walser M: Misinterpretation of nitrogen balances when glutamine stores fall or are replenished. Am J Clin Nutr. 1991, 53: 1337-1338.
Potter MA, Luxton G: Transthyretin measurement as a screening tool for protein calorie malnutrition in emergency hospital admissions. Clin Chem Lab Med. 2002, 40: 1-6.
McClave SA, Mitoraj TE, Thielmeier KA, Greenburg RA: Differentiating subtypes (hypoalbuminemic vs marasmic) of protein-calorie malnutrition: incidence and clinical significance in a university hospital setting. JPEN J Parenter Enteral Nutr. 1992, 16: 337-342.
Buzby GP, Williford WO, Peterson OL, Crosby LO, Page CP, Reinhardt GF, Mullen JL: A randomized clinical trial of total parenteral nutrition in malnourished surgical patients: the rationale and impact of previous clinical trials and pilot study on protocol design. Am J Clin Nutr. 1988, 47: 357-365.
Bouillanne O, Morineau G, Dupont C, Coulombel I, Vincent JP, Nicolis I, Benazeth S, Cynober L, Aussel C: Geriatric nutritional risk index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr. 2005, 82: 777-783.
Sjolin J, Stjernstrom H, Arturson G, Andersson E, Friman G, Larsson J: Exchange of 3-methylhistidine in the splanchnic region in human infection. Am J Clin Nutr. 1989, 50: 1407-1414.
Coudray-Lucas C, Cynober L, Lioret N, Saizy R, Baux S, Giboudeau J: Origins of hyperphenylalaninemia in burn patients. Clin Nutr. 1985, 4: 179-183.
Curis E, Nicolis I, Moinard C, Osowska S, Zerrouk N, B Nazeth S, Cynober L: Almost all about citrulline in mammals. Amino Acids. 2005, 29: 177-205.
van de Poll MC, Siroen MP, van Leeuwen PA, Soeters PB, Melis GC, Boelens PG, Deutz NE, Dejong CH: Interorgan amino acid exchange in humans: consequences for arginine and citrulline metabolism. Am J Clin Nutr. 2007, 85: 167-172.
Crenn P, Coudray-Lucas C, Thuillier F, Cynober L, Messing B: Postabsorptive plasma citrulline concentration is a marker of absorptive enterocyte mass and intestinal failure in humans. Gastroenterology. 2000, 119: 1496-1505.
Crenn P, Hanachi M, Neveux N, Cynober L: Circulating citrulline levels: a biomarker for intestinal functionality assessment. Ann Biol Clin (Paris). 2011, 69: 513-521.
Cynober L: Lessons from pharmacokinetics in the design of new nutrition formulas for critically ill patients. Nestle Nutr Workshop Ser Clin Perform Programme. 2003, 8: 265-272. discussion 272-277
Abumrad N, Darmaun D, Cynober L: Approaches to studying amino acid metabolism: from quantitative assays to flux assessment using stable isotopes. Amino Acid Metabolism in Health and Nutritional Disease. Edited by: Cynober L. 1995, CRC Press, Boca Raton, FL, 15-30.
Berard MP, Pelletier A, Ollivier JM, Gentil B, Cynober L: Qualitative manipulation of amino acid supply during total parenteral nutrition in surgical patients. JPEN J Parenter Enteral Nutr. 2002, 26: 136-143.
Wolfe RR, Chinkes DL: Isotope Tracers in Metabolic Research: Principles and Practice of Kinetic Analysis. 2004, John Wiley & Sons, Hoboken, New Jersey, USA
Zhang XJ, Chinkes DL, Wolfe RR: Measurement of muscle protein fractional synthesis and breakdown rates from a pulse tracer injection. Am J Physiol Endocrinol Metab. 2002, 283: E753-E764.
Biolo G, Fleming RY, Maggi SP, Wolfe RR: Transmembrane transport and intracellular kinetics of amino acids in human skeletal muscle. Am J Physiology. 1995, 268: E75-E84.
McClave SA, Kushner R, Van Way CW, Cave M, DeLegge M, Dibaise J, Dickerson R, Drover J, Frazier TH, Fujioka K, Gallagher D, Hurt RT, Kaplan L, Kiraly L, Martindale R, McClain C, Ochoa J: Nutrition therapy of the severely obese, critically ill patient: summation of conclusions and recommendations. JPEN J Parenter Enteral Nutr. 2011, 35: 88S-96S.
Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Gómez JM, Heitmann BL, Kent-Smith L, Melchior JC, Pirlich M, Scharfetter H, Schols AM, Pichard C: Bioelectrical impedance analysis - part I: review of principles and methods. Clin Nutr. 2004, 23: 1226-1243.
Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Manuel Gómez J, Lilienthal Heitmann B, Kent-Smith L, Melchior JC, Pirlich M, Scharfetter H, MWJ Schols A, Pichard C: Bioelectrical impedance analysis - part II: utilization in clinical practice. Clin Nutr. 2004, 23: 1430-1453.
Heymsfield SB, Smith R, Aulet M, Bensen B, Lichtman S, Wang J, Pierson RN: Appendicular skeletal muscle mass: measurement by dual-photon absorptiometry. Am J Clin Nutr. 1990, 52: 214-218.
Mourtzakis M, Prado CM, Lieffers JR, Reiman T, McCargar LJ, Baracos VE: A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl Physiol Nutr Metab. 2008, 33: 997-1006.
Tan BH, Birdsell LA, Martin L, Baracos VE, Fearon KC: Sarcopenia in an overweight or obese patient is an adverse prognostic factor in pancreatic cancer. Clin Cancer Res. 2009, 15: 6973-6979.
Moisey LL, Mourtzakis M, Cotton BA, Premji T, Heyland DK, Wade CE, Bulger E, Kozar RA: Skeletal muscle predicts ventilator-free days, ICU-free days, and mortality in elderly ICU patients. Crit Care. 2013, 17: R206-
Weijs PJ, Looijaard WG, Dekker IM, Stapel SN, Girbes AR, Oudemans-van Straaten HM, Beishuizen A: Low skeletal muscle area is a risk factor for mortality in mechanically ventilated critically ill patients. Crit Care. 2014, 18: R12-
Campbell IT, Watt T, Withers D, England R, Sukumar S, Keegan MA, Faragher B, Martin DF: Muscle thickness, measured with ultrasound, may be an indicator of lean tissue wasting in multiple organ failure in the presence of edema. Am J Clin Nutr. 1995, 62: 533-539.
Braunschweig CA, Sheean PM, Peterson SJ, Perez SG, Freels S, Troy KL, Ajanaku FC, Patel A, Sclamberg JS, Wang Z: Exploitation of diagnostic computed tomography scans to assess the impact of nutritional support on body composition changes in respiratory failure patients. JPEN J Parenter Enteral Nutr. 2014, 38: 880-885.
Casaer MP, Wilmer A, Hermans G, Wouters PJ, Mesotten D, Van den Berghe G: Role of disease and macronutrient dose in the randomized controlled EPaNIC trial: a post hoc analysis. Am J Respir Crit Care Med. 2013, 187: 247-255.
Herridge MS, Tansey CM, Matté A, Tomlinson G, Diaz-Granados N, Cooper A, Guest CB, Mazer CD, Mehta S, Stewart TE, Kudlow P, Cook D, Slutsky AS, Cheung AM: Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011, 364: 1293-1304.
Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al-Saidi F, Cooper AB, Guest CB, Mazer CD, Mehta S, Stewart TE, Barr A, Cook D, Slutsky AS: One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003, 348: 683-693.
Rosenblatt S, Clowes GH, George BC, Hirsch E, Lindberg B: Exchange of amino acids by muscle and liver in sepsis. Arch Surg. 1983, 118: 167-175.
Pearl RH, Clowes GH, Hirsch EF, Loda M, Grindlinger GA, Wolfort S: Prognosis and survival as determined by visceral amino acid clearance in severe trauma. J Trauma. 1985, 25: 777-783.
Sakurai Y, Aarsland A, Herndon DN, Chinkes DL, Pierre E, Nguyen TT, Patterson BW, Wolfe RR: Stimulation of muscle protein synthesis by long-term insulin infusion in severely burned patients. Ann Surg. 1995, 222: 283-294. 294-297
Herndon DN, Hart DW, Wolf SE, Chinkes DL, Wolfe RR: Reversal of catabolism by beta-blockade after severe burns. N Engl J Med. 2001, 345: 1223-1229.
Ferrando AA, Sheffield-Moore M, Wolf SE, Herndon DN, Wolfe RR: Testosterone administration in severe burns ameliorates muscle catabolism. Crit Care Med. 2001, 29: 1936-1942.
Gamrin L, Essen P, Hultman E, McNurlan MA, Garlick PJ, Wernerman J: Protein-sparing effect in skeletal muscle of growth hormone treatment in critically ill patients. Ann Surg. 2000, 231: 577-586.
Takala J, Ruokonen E, Webster NR, Nielsen MS, Zandstra DF, Vundelinckx G, Hinds CJ: Increased mortality associated with growth hormone treatment in critically ill adults. N Engl J Med. 1999, 341: 785-792.
Kreymann KG, Berger MM, Deutz NE, Hiesmayr M, Jolliet P, Kazandjiev G, Nitenberg G, van den Berghe G, Wernerman J, Ebner C, Hartl W, Heymann C, Spies C: ESPEN guidelines on enteral nutrition: intensive care. Clin Nutr. 2006, 25: 210-223.
Singer P, Berger MM, Van den Berghe G, Biolo G, Calder P, Forbes A, Griffiths R, Kreyman G, Leverve X, Pichard C: ESPEN guidelines on parenteral nutrition: intensive care. Clin Nutr. 2009, 28: 387-400.
McClave SA, Martindale RG, Vanek VW, McCarthy M, Roberts P, Taylor B, Ochoa JB, Napolitano L, Cresci G: Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr. 2009, 33: 277-316.
Larsson J, Lennmarken C, Martensson J, Sandstedt S, Vinnars E: Nitrogen requirements in severely injured patients. Br J Surg. 1990, 77: 413-416.
Dickerson RN, Pitts SL, Maish GO, Schroeppel TJ, Magnotti LJ, Croce MA, Minard G, Brown RO: A reappraisal of nitrogen requirements for patients with critical illness and trauma. J Trauma Acute Care Surg. 2012, 73: 549-557.
Verbruggen SC, Coss-Bu J, Wu M, Schierbeek H, Joosten KF, Dhar A, van Goudoever JB, Castillo L: Current recommended parenteral protein intakes do not support protein synthesis in critically ill septic, insulin-resistant adolescents with tight glucose control. Crit Care Med. 2011, 39: 2518-2525.
Doig GS, Simpson F, Finfer S, Delaney A, Davies AR, Mitchell I, Dobb G: Effect of evidence-based feeding guidelines on mortality of critically ill adults: a cluster randomized controlled trial. JAMA. 2008, 300: 2731-2741.
Barr J, Hecht M, Flavin KE, Khorana A, Gould MK: Outcomes in critically ill patients before and after the implementation of an evidence-based nutritional management protocol. Chest. 2004, 125: 1446-1457.
Martin CM, Doig GS, Heyland DK, Morrison T, Sibbald WJ: Multicentre, cluster-randomized clinical trial of algorithms for critical-care enteral and parenteral therapy (ACCEPT). CMAJ. 2004, 170: 197-204.
van Schijndel RJ S, Weijs PJ, Koopmans RH, Sauerwein HP, Beishuizen A, Girbes AR: Optimal nutrition during the period of mechanical ventilation decreases mortality in critically ill, long-term acute female patients: a prospective observational cohort study. Crit Care. 2009, 13: R132-
Weijs PJ, Stapel SN, de Groot SD, Driessen RH, de Jong E, Girbes AR, van Schijndel RJ S, Beishuizen A: Optimal protein and energy nutrition decreases mortality in mechanically ventilated, critically ill patients: a prospective observational cohort study. JPEN J Parenter Enteral Nutr. 2012, 36: 60-68.
Allingstrup MJ, Esmailzadeh N, Wilkens Knudsen A, Espersen K, Hartvig Jensen T, Wiis J, Perner A, Kondrup J: Provision of protein and energy in relation to measured requirements in intensive care patients. Clin Nutr. 2012, 31: 462-468.
Casaer MP, Mesotten D, Hermans G, Wouters PJ, Schetz M, Meyfroidt G, Van Cromphaut S, Ingels C, Meersseman P, Muller J, Vlasselaers D, Debaveye Y, Desmet L, Dubois J, Van Assche A, Vanderheyden S, Wilmer A, Van den Berghe G: Early versus late parenteral nutrition in critically ill adults. N Engl J Med. 2011, 365: 1-17.
Arabi YM, Tamim HM, Dhar GS, Al-Dawood A, Al-Sultan M, Sakkijha MH, Kahoul SH, Brits R: Permissive underfeeding and intensive insulin therapy in critically ill patients: a randomized controlled trial. Am J Clin Nutr. 2011, 93: 569-577.
Rice TW, Mogan S, Hays MA, Bernard GR, Jensen GL, Wheeler AP: Randomized trial of initial trophic versus full-energy enteral nutrition in mechanically ventilated patients with acute respiratory failure. Crit Care Med. 2011, 39: 967-974.
Singer P, Anbar R, Cohen J, Shapiro H, Shalita-Chesner M, Lev S, Grozovski E, Theilla M, Frishman S, Madar Z: The tight calorie control study (TICACOS): a prospective, randomized, controlled pilot study of nutritional support in critically ill patients. Intensive Care Med. 2011, 37: 601-609.
Heart N, Rice TW, Wheeler AP, Thompson BT, Steingrub J, Hite RD, Moss M, Morris A, Dong N, Rock P: Initial trophic vs full enteral feeding in patients with acute lung injury: the EDEN randomized trial. JAMA. 2012, 307: 795-803.
Heidegger CP, Berger MM, Graf S, Zingg W, Darmon P, Costanza MC, Thibault R, Pichard C: Optimisation of energy provision with supplemental parenteral nutrition in critically ill patients: a randomised controlled clinical trial. Lancet. 2013, 381: 385-393.
Doig GS, Simpson F, Sweetman EA, Finfer SR, Cooper DJ, Heighes PT, Davies AR, O'Leary M, Solano T, Peake S: Early parenteral nutrition in critically ill patients with short-term relative contraindications to early enteral nutrition: a randomized controlled trial. JAMA. 2013, 309: 2130-2138.
Weijs PJ, Wischmeyer PE: Optimizing energy and protein balance in the ICU. Curr Opin Clin Nutr Metab Care. 2013, 16: 194-201.
Vanhorebeek I, Gunst J, Derde S, Derese I, Boussemaere M, Güiza F, Martinet W, Timmermans JP, D'Hoore A, Wouters PJ, Van den Berghe G: Insufficient activation of autophagy allows cellular damage to accumulate in critically ill patients. J Clin Endocrinol Metab. 2011, 96: E633-E645.
Heyland DK, MacDonald S, Keefe L, Drover JW: Total parenteral nutrition in the critically ill patient: a meta-analysis. JAMA. 1998, 280: 2013-2019.
Doig GS, Heighes PT, Simpson F, Sweetman EA: Early enteral nutrition reduces mortality in trauma patients requiring intensive care: a meta-analysis of randomised controlled trials. Injury. 2011, 42: 50-56.
Rooyakers O, Koucheck-Zadeh R, Tjader I, Norberg A, Klaude M, Wernerman J: Whole body protein turnover in mechanically ventilated ICU patients. Intensive Care Med. 2012, 38: S130-
van Schijndel RJM S, Weijs PJM, Sauerwein HP, de Grootb SDW, Beishuizena A, Girbesa ARJ: An algorithm for balanced protein/energy provision in critically ill mechanically ventilated patients. e-SPEN J. 2007, 2: 69-74.
van Schijndel RJ, de Groot SD, Driessen RH, Ligthart-Melis G, Girbes AR, Beishuizen A, Weijs PJ: Computer-aided support improves early and adequate delivery of nutrients in the ICU. Neth J Med. 2009, 67: 388-393.
Acknowledgements
The authors would like to thank Angela Sickmann and Angela Rogers of Gardiner-Caldwell Communications, an Ashfield company (Macclesfield, UK), for support in incorporating authors' comments, reference formatting, and editing and styling the manuscript. Medical writing services from Gardiner-Caldwell Communications were funded by Baxter Healthcare Corporation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The meeting of the Protein Working Group was held in Barcelona, Spain, in 2012. The first outline for this manuscript was discussed at the Protein Working Group meeting, which was supported by Baxter. Authors were not paid for writing this manuscript. PJMW is in receipt of research grants from Baxter and Danone/Nutricia. LC's work was supported by a governmental grant (EA 4466) and a research grant from Nestlé Clinical Nutrition. LC has received honoraria from Baxter and Nestlé Clinical Nutrition. MD and GK are employed by Baxter. JW has received honoraria for advisory board membership from Baxter, Danone, Fresenius, Grifols, and Nestlé Clinical Nutrition. RRW has received research grants and personal fees from Baxter, National Cattleman’s Beef Association, and Abbott Nutrition.
Authors' contributions
The authors wrote and critically reviewed the manuscript and approved the final version.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Weijs, P.J., Cynober, L., DeLegge, M. et al. Proteins and amino acids are fundamental to optimal nutrition support in critically ill patients. Crit Care 18, 591 (2014). https://doi.org/10.1186/s13054-014-0591-0
Published:
DOI: https://doi.org/10.1186/s13054-014-0591-0