Abstract
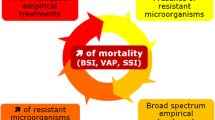
The rapid emergence and dissemination of antimicrobial-resistant microorganisms in ICUs worldwide constitute a problem of crisis dimensions. The root causes of this problem are multifactorial, but the core issues are clear. The emergence of antibiotic resistance is highly correlated with selective pressure resulting from inappropriate use of these drugs. Appropriate antibiotic stewardship in ICUs includes not only rapid identification and optimal treatment of bacterial infections in these critically ill patients, based on pharmacokinetic-pharmacodynamic characteristics, but also improving our ability to avoid administering unnecessary broad-spectrum antibiotics, shortening the duration of their administration, and reducing the numbers of patients receiving undue antibiotic therapy. Either we will be able to implement such a policy or we and our patients will face an uncontrollable surge of very difficult-to-treat pathogens.
Similar content being viewed by others
Introduction
Optimal antibiotic use is crucial in the critical care setting, especially in an era of rising antibiotic resistance and lack of new antimicrobial development [1]-[3]. Study results indicate that 30% to 60% of antibiotics prescribed in ICUs are unnecessary, inappropriate, or suboptimal [4]-[7]. Overprescribing and misprescribing antibiotics are undoubtedly contributing to the growing challenges posed by antibiotic-resistant bacteria, and epidemiological studies have clearly demonstrated direct relationships between antibiotic consumption and the emergence and dissemination of resistant strains in hospitals and ICUs [7]-[20]. As defined by the Society of Healthcare Epidemiology of America and Infectious Diseases Society of America (IDSA) Joint Committee on the Prevention of Antimicrobial Resistance in hospitals, ‘stewardship of antimicrobials is an apt descriptor of related activities that help optimize antimicrobial therapy, ensuring the best clinical outcome for the patient while lowering the risk of subsequent development of antimicrobial resistance’ [14]. Thus, in-ICU antibiotic stewardship encompasses rapid identification of patients with bacterial infections, better empirical treatment selection, using pharmacokinetic-pharmacodynamic (PK-PD) characteristics to optimize antibiotic dosing and administration modalities, de-escalation once culture results become available, shortening therapy duration, and reducing the numbers of patients treated unnecessarily.
Unfortunately, improving in-ICU antibiotic use is particularly difficult for three main reasons: infection severity often precludes withdrawing or postponing antibiotics, the complex decision-making process frequently involves doctors with limited expertise, and it is difficult to ensure disease-long continuity of care by the same medical team 24 hours a day, 7 days a week. Here, we review how in-ICU antibiotic therapy could possibly be optimized and rationalized.
Rapid identification of intensive care unit patients with bacterial infections
Most published observational data suggest that the time to appropriate antibiotic administration is a major outcome determinant for ICU patients with severe bacterial infections. Indeed, each hour of delay in administering effective antibiotics for septic shock is associated with measurably increased mortality [6],[21]-[25]. Thus, as strongly recommended by all guidelines [26]-[29], obtaining biological specimens should not postpone timely antibiotic administration to patients with severe sepsis or septic shock.
However, owing to methodological concerns, the harmful effects of inadequate therapy are not accepted by all [30]-[36]. Because in-ICU signs and symptoms of infection due to non-infectious causes are common, rushing to prescribe antibiotics may mean that many uninfected patients receive unnecessary treatment. In a quasi-experimental, before-and-after, observational cohort study of patients admitted to the University of Virginia surgical ICU, Hranjec and colleagues [32] postulated that delaying antibiotics for hemodynamically stable patients with suspected infections (35% pneumonia) until they were objectively documented would not worsen mortality. Notably, that conservative approach was associated with lower all-cause mortality, more initially appropriate therapy, and shorter mean treatment duration than the aggressive strategy. Thus, for clinically stable patients, that strategy might achieve better antibiotic use without impacting prognosis. Obtaining specimens for appropriate cultures before antibiotic administration is essential to confirm infection, identify responsible pathogens, and enable therapy de-escalation in response to susceptibility profiles.
The inaccuracy of conventional approaches to diagnose hospital-acquired infections (HAIs) and the impossibility of those strategies to avoid antibiotic overprescription led some investigators to hypothesize that using biological markers - for example, C-reactive protein, soluble-triggering receptor expressed on myeloid cells-1, or procalcitonin (PCT) - might better identify true bacterial infections and facilitate therapeutic decisions. However, although PCT is a good marker of community-acquired infections (CAIs), it does not seem to be for HAIs [37]-[41]. Indeed, blood PCT concentrations can rise in various non-septic conditions: major trauma, surgery, acute respiratory distress syndrome, multiorgan failure, post-transplantation rejection, cardiogenic shock, severe burns, heat stroke, and so on. Thus, high PCT concentrations the day sepsis is suspected are non-contributory because increases that are attributable to a prior non-infectious condition or active infection cannot be distinguished [39],[42],[43]. Moreover, PCT can remain low in some microbiologically proven bacterial infections, either because the infection remains contained in a tissue compartment that can synthesize PCT locally without systemic release, thereby explaining the low serum level despite true infection, or because of a 24- to 48-hour lag time in infection onset to peak PCT release. Thus, intensivists are rightly reluctant to rely exclusively on biological markers when severe infection is suspected [37],[38],[43]-[47].
Selection of initial antibiotic therapy
Owing to the emergence of multiresistant Gram-negative bacilli (GNB) (for example, Pseudomonas aeruginosa, extended-spectrum β-lactamase-producing Enterobacteriaceae, and carbapenemase-producing Klebsiella pneumoniae) and the increasing role of Gram-positive bacteria (like methicillin-resistant Staphylococcus aureus, or MRSA), empirical broad-spectrum antibiotics are justified for most ICU patients with clinically suspected HAIs [25]-[27],[48]. Regimen choice should be based on local antimicrobial susceptibility patterns and anticipated side effects while considering the antibiotics received within the preceding 2 weeks and striving whenever possible not to use the same classes [49]-[51]. Having current and frequently updated knowledge of local bacteriological epidemiology increases the likelihood of prescribing appropriate initial antibiotics. Whether surveillance cultures could further improve empirical treatment selection for ICU patients with suspected hospital-acquired pneumonia (HAP) is still debated but certainly should be weighed when difficult-to-treat microorganisms abound, making initial choices particularly risky [52],[53]. Observational study results confirmed that initial regimens combining a broad-spectrum β-lactam and an aminoglycoside increased the proportion of appropriately treated patients compared with monotherapy or a combination of β-lactam and fluoroquinolone [54],[55]. Only patients with mildly or moderately severe, early-onset infections and no specific risk factors (for example, prolonged hospitalization, immunosuppression, or recent prolonged antibiotics or a combination of these) can receive a relatively narrow-spectrum drug, like a non-pseudomonal third-generation cephalosporin.
For ICU patients admitted with health care-associated or community-onset infections or CAIs, more restraints for antimicrobial therapy selection are certainly possible. For example, it is increasingly recognized that applying current criteria for health care-associated pneumonia - hospitalization for at least 2 days during the preceding 90 days, residence in a nursing home or extended-care facility, home intravenous (antibiotics or chemotherapy) therapy, and chronic dialysis or home wound care (or both) during the preceding 30 days - as indications for broad-spectrum antibiotics may lead to overtreatment of many patients with pneumonia [56]-[62]. To address this conceptual limitation, investigators developed multiple risk-assessment models that refine those criteria [61],[63],[64]. Available data suggest that the incidence of pathogens resistant to the usual in-patient IDSA-American Thoracic Society guideline-recommended antibiotic regimen (that is, a non-pseudomonal cephalosporin and a macrolide) is usually not significantly increased unless two or more risk factors are present, with prior antibiotic use or hospitalization and poor functional status being more important predictors of resistant bacteria than nursing-home residence alone [61]. Using such an algorithm could lead to fewer pneumonia patients unnecessarily receiving broad-spectrum antibiotics.
Within the past decade, the way clinical microbiology laboratories identify microorganisms was revolutionized, leaving behind slow traditional methods based on phenotype characteristics (for example, growth on defined media, colony morphology, Gram staining, and biochemical reactions) incurring significant diagnosis delay, in exchange for new diagnostic techniques (real-time multiplex polymerase chain reaction and matrix-assisted laser desorption/ionization time-of-flight mass spectrometry) [65],[66]. The latter, making possible rapid pathogen identification and their antimicrobial resistance patterns (at least for certain organisms), could undoubtedly promote earlier therapy appropriateness and de-escalation [67]. Multiple instrument platforms, marketed by well-established manufacturers, are beginning to displace or complement (or both) automated conventional phenotyping tools, providing accurate microbial identification from blood cultures within 1 to 2 hours. Nevertheless, it is unlikely that any of those new diagnostic methods will completely replace phenotyping for antibiotic susceptibility testing in the near future.
Pending the complete development of those above-mentioned techniques, Bouza and colleagues [68] described simple microbiology laboratory-accessible, rapid, antimicrobial susceptibility E-tests directly on samples (lower respiratory tract or other biological specimens) to improve early appropriate in-ICU antimicrobial choices. In a prospective randomized study of 250 patients with microbiologically confirmed ventilator-associated pneumonia (VAP), the authors showed that reporting rapid E-test-obtained antibiotic susceptibility of responsible microorganisms to the treating physicians (mean ± standard deviation: 1.4 ± 0.75 days post-sampling versus 4.2 days with standard methods) was associated with fewer days of fever and antibiotics until VAP-episode resolution, less antibiotic consumption, less Clostridium difficile-associated diarrhea, lower antimicrobial costs, and fewer days on mechanical ventilation (MV) [68].
Pharmacokinetic-pharmacodynamic-optimized antimicrobial therapy
Reported findings demonstrated the need to individually adjust the antibiotic target doses and administration modalities to treat severe bacterial infection to each patient’s PK and putative or documented pathogens’ susceptibilities, as assessed by their minimal inhibitory concentrations (MICs) [69]-[73]. Most investigators distinguish antimicrobials by their killing mechanism: concentration-dependent (for example, aminoglycosides and fluoroquinolones) or time-dependent (for example, β-lactams and carbapenem). The most important PK-PD parameters are peak concentration/MIC >8-10 and 24-hour area under the concentration curve (AUC)/MIC >100-125 for aminoglycosides and fluoroquinolones. For β-lactams and carbapenem, the blood concentration should be maintained for >90-100% of the between-dose interval above MIC, at least in the case of severe infection [74],[75]. However, it should be acknowledged that the exact target for PK-PD-optimized therapy remains elusive. Some antibiotics, such as fluoroquinolones and glycopeptides, are more complex and exhibit both concentration- and time-dependent kill characteristics where the best predictor of efficacy is the AUC/MIC. Others, such as carbapenems, have a marked post-antibiotic effect (that is, lead to a prolonged suppression of bacterial growth even with antibiotic concentrations below the MIC) [76],[77].
ICU patients’ altered PK secondary to increased volume of distribution and decreased elimination can result in insufficient serum aminoglycosides or β-lactam concentrations (or both) when standard doses are administered, emphasizing the need to carefully monitor peak and trough antibiotic levels when treating resistant pathogens, respectively [5],[78],[79]. Antibiotic doses for ICU patients derived from other patient groups are likely to be suboptimal because of significant antibiotic PK changes, particularly volume of distribution and clearance. Organ support techniques, including renal replacement therapy and extracorporeal membrane oxygenation, increase PK variability (Figure 1) [80]-[82]. In a recent prospective study conducted at 64 hospitals worldwide, 20% and 40% of 248 ICU patients receiving β-lactams for infection did not achieve free antibiotic concentrations above their pathogens’ MICs during 50% and 100% (50% and 100% fT > MIC, respectively) of the dosing interval (Figure 2) [5]. Frequently, higher than usually recommended antibiotic doses or continuous or extended infusions (or a combination of these) are needed [5],[70],[71],[73],[79],[83]-[85]. Interestingly, use of prolonged infusion appeared to be associated with a significant reduction in mortality and improvement in clinical success when compared with intermittent boluses in a recent meta-analysis of 29 studies (18 randomized controlled trials and 11 observational studies) with a total of 2,206 patients [85].
Pathophysiological changes commonly observed in critically ill patients and their effects on drug concentrations. Reproduced with permission from Elsevier Limited [75]. ECMO, extracorporeal membrane oxygenation; RRT, renal replacement therapy.
Achievement of pharmacokinetic/pharmacodynamic targets in intensive care unit patients according to antibiotics used. Data are expressed as percentage of patients achieving target. Doses for each antibiotic are given as a median. This figure was drawn from data in Table 3 of [5] with permission from Oxford Journals. 50% fT > MIC, free drug concentration maintained above minimum inhibitory concentration of the known or suspected pathogen for at least 50% of dosing interval; 50% fT > 4 × MIC, free drug concentration maintained above a concentration fourfold higher than the minimum inhibitory concentration of the known or suspected pathogen for at least 50% of dosing interval; 100% fT > MIC, free drug concentration maintained above minimum inhibitory concentration of the known or suspected pathogen throughout the entire dosing interval; 100% fT > 4 × MIC, free drug concentration maintained above a concentration fourfold higher than the minimum inhibitory concentration of the known or suspected pathogen throughout the entire dosing interval.
Development of a priori dosing algorithms based on MIC, creatinine clearance and weight, and the clinician-specified AUC target might improve management of these patients, obtaining more precise antibiotic use than current guidelines [73],[79],[83],[84],[86]. Ultimately, adjusting antibiotic doses based on pathogen MICs and daily free antibiotic blood concentrations may reach optimized PK-PD targets in most ICU patients. A therapeutic drug-monitoring strategy, compared with traditional dosing methods, might not only reduce clinical failure rates in ICU patients but also prevent adverse events due to too high (toxic) antibiotic levels [87],[88].
A double-blind randomized trial comparing 7 days of doripenem three times a day (4-hour infusion of 1 gram) with 10 days of imipenem-cilastin (1-hour infusion of 1 gram) for GNB VAP was prematurely stopped after random assignment of 274 patients because of inferior efficacy and higher day-28 all-cause mortality in the subgroup of doripenem-treated, P. aeruginosa-infected patients [89]. Despite longer doripenem infusions to optimize targeted antibiotic concentrations above the pathogens’ MICs during the 8-hour interval, this protocol performed more poorly, clearly documenting the risk associated with a so-called PK-PD-optimized antibiotic strategy when blood concentrations cannot be monitored and adjusted to stay above the responsible pathogens’ MICs. Perhaps the treatment duration or concentrations (or both) were sub-therapeutic for patients with elevated creatinine clearance, clearly documenting the risk associated with a so-called PK-PD-optimized antibiotic strategy when blood concentrations cannot be monitored and adjusted to stay above the MIC of the responsible pathogens [90].
For patients on MV, aerosolized antibiotics delivered via an efficient system, synchronized with inspiration, achieved airway drug concentrations 100- to 300-fold higher than the MICs of most bacteria, including multidrug-resistant pathogens [91]-[95]. Those levels, without systemic toxicity, might eradicate proximal airway pathogens in patients on MV and lower the pressure for selection of new resistant organisms, as shown in a recent, double-blind, placebo-controlled study of 42 ICU patients who required prolonged MV and who were colonized or infected (or both) with potentially difficult-to-treat pathogens (for example, MRSA and non-fermenting GNB) [96]. However, larger clinical trials must confirm those findings before that strategy can be recommended, in light of its potentially deleterious impact on the local epidemiology when used for all ICU patients over prolonged periods [97]-[99].
Antimicrobial therapy de-escalation
The need to ensure that ICU patients with true bacterial infections receive prompt and appropriate antibiotics can lead to many more patients receiving antimicrobials than necessary, because of non-specific clinical signs of infection. This is particularly true for HAP/VAP, which represents the first in-ICU indication for starting antibiotics. Thus, regardless of the diagnostic strategy used for suspected HAP/VAP, serial clinical and microbiological evaluations are highly relevant to re-assess therapy after 48 to 72 hours and to stop it if infection is unlikely [48],[100]. To accomplish that goal, each ICU should design its own diagnostic decision-tree strategy to manage patients with clinically suspected HAP/VAP to identify those with a low probability of infection, whose therapy can be discontinued when infection appears improbable [27],[48]. At least, antibiotics should be withdrawn when the following three criteria are fulfilled on day 3: (a) the clinical diagnosis of pneumonia is unlikely - no definite infiltrates seen on repeat chest radiography and only one of the following three findings is present: temperature greater than 38.3°C, leukocytosis (greater than 12,000/mm3) or leukopenia (less than 4,000/mm3), or purulent tracheobronchial secretions - or an alternative non-infectious diagnosis is confirmed; (b) non-significant tracheobronchial aspirate culture results; and (c) no severe sepsis or shock [101]. Direct examination of distal pulmonary samples collected by bronchoalveolar lavage with or without a bronchoscope and quantitative culture results have consistently yielded fewer microorganisms growing above the diagnostic threshold than qualitative tracheal aspirate cultures [48],[102]. Pertinently, when therapeutic decisions were based on those results, compared with the clinical approach, fewer patients received antibiotics that were of a potentially narrower spectrum, thereby limiting the emergence and dissemination of drug-resistant strains and minimizing antibiotic-related toxicity [103].
For many ICU patients with infections (including late-onset infections), therapy can be de-escalated, once respiratory tract, blood, or other specimen culture results become available, if no resistant organism (for example, P. aeruginosa, Acinetobacter spp., or MRSA) is recovered or because the isolated pathogen is sensitive to a narrower-spectrum antibiotic than that prescribed empirically [26],[27],[48]. For example, if MRSA is not found, vancomycin and linezolid should be stopped unless the patient is allergic to β-lactams or has developed an infection with Gram-positive bacteria susceptible only to them. Very-broad-spectrum agents (like carbapenems, piperacillin-tazobactam, and cefepime) should also be restricted to patients whose infectious pathogens are susceptible only to them. Because fluoroquinolones have been associated with the emergence of resistant strains, their in-ICU use probably should be discouraged [104],[105]. Antifungals should never be prescribed for Candida isolated from respiratory secretions alone [106]. However, clinicians should know that, when third-generation cephalosporins are chosen to treat infections caused by Enterobacteriacaea with inducible β-lacatamase (Enterobacter, Citrobacter, Morganella morganii, indole-positive Proteus, or Serratia spp.), the emergence of resistant variants may lead to treatment failure. Unfortunately, study results showed that de-escalation, though not associated with any adverse outcomes, was not consistently applied in many ICUs [107]-[111].
The two most commonly cited reasons to prescribe combined antibiotics for the entire treatment duration are to achieve synergy and to prevent the emergence of resistant strains. However, antibiotic synergy has been shown to be valuable only in vitro and in patients with neutropenia, bacteremia, or a greater than 25% probability of death [25],[112]-[122]. Randomized controlled trial results on combined therapy showed its benefit to be inconsistent or null, even when they were pooled in meta-analyses or when analysis was restricted to P. aeruginosa-infected patients [113],[121],[123],[124]. Importantly, such regimens did not prevent the emergence of antimicrobial resistance during therapy and were associated with significantly more nephrotoxicity [121]. Those observations were confirmed in a randomized, open-label trial on 600 patients meeting criteria for severe sepsis or septic shock: combined meropenem and moxifloxacin versus meropenem alone did not achieve less organ failure or better survival or any secondary endpoints [113]. Based on those data, most patients’ therapy could be safely switched to monotherapy after 3 to 5 days, provided that the initial therapy was appropriate, the clinical course evolved favorably, and microbiological data did not indicate difficult-to-treat microorganisms, with high in vitro MICs, as can be observed for some non-fermenting GNB.
Shortening treatment duration
Although shortening the duration of antibiotic administration for ICU patients may represent the most powerful strategy to reduce antibiotic impact on resistance emergence, most guidelines still recommend relatively prolonged or imprecise durations [26],[28],[125],[126]. Efforts to shorten the duration for bacterial infections are justified by study results on the natural history of therapeutic responses. Most patients who had CAIs or HAIs, including VAP, and who received appropriate antimicrobial therapy had good clinical responses within the first 6 days [127]-[129]. Prolonged therapy facilitates colonization with antibiotic-resistant bacteria, which may precede recurrent infectious episodes.
Results of a multicenter, randomized controlled trial on 401 patients with microbiologically proven VAP showed that their clinical outcomes were similar to those of patients receiving appropriate empirical therapy for 8 or 15 days [130]. Relapse rates for short-duration therapy tended to be higher when P. aeruginosa or Acinetobacter spp. was the causative agent, but clinical outcomes were indistinguishable. Those observations were confirmed by trials that evaluated an antibiotic discontinuation policy for patients with other infections [111],[131]-[138].
Many clinicians remain reluctant to prescribe fewer days of antibiotics for patients with severe HAIs and prefer tailoring antibiotic duration to the ensuing clinical course or using serial biomarker (for example, PCT) determinations (or both). The rationale for using the latter to customize treatment duration relies on evidence that the inflammatory response is often proportional to infection severity. When the response is absent or mild, antibiotics might logically be discontinued earlier. Thus, adapting treatment duration to PCT kinetics seems reasonable and was demonstrated to be useful in several randomized trials, including seven in the ICU, targeting patients with acute respiratory infections [37],[41],[139]-[143]. The largest of those studies was the PRORATA trial that included 621 ICU patients; 67% of these patients were on MV, 50% had CAIs, and 50% had HAIs, and half of them had septic shock [37]; patients in the PCT group had significantly more (mean ± standard deviation) days without antibiotics than controls (14.3 ± 9.1 versus 11.6 ± 8.2; absolute difference 2.7 days; 95% confidence interval 1.4 to 4.1; P < 0.0001), and this lower antibiotic consumption was not associated with poorer outcomes. Furthermore, regardless of infection site and the infectious agent, results were consistent (Figure 3).
Duration of antibiotic treatment of the first episode in the PRORATA trial, according to infection site. White bars indicate patients included in the control group. Hatched bars indicate patients included in the procalcitonin-guided group. This figure was drawn from data in Table 2 of [37] with permission from Elsevier Limited. CAP, community-acquired pneumonia; PRORATA, Use of Procalcitonin to Reduce Patients’ Exposure to Antibiotics in Intensive Care Units; UTI, urinary tract infection; VAP, ventilator-associated pneumonia.
In summary, shortening the treatment duration for ICU patients with infections is possible and not detrimental for most of them. Indeed, the diversity of patients enrolled in those trials and the consistency of the findings suggest that the conclusions may be applicable to most critically ill patients who develop infections, including severe sepsis or septic shock, with the possible exception of those who are immunosuppressed, those who are infected with multiresistant microorganisms or whose course deteriorates despite treatment, or those whose initial regimen was inappropriate for the responsible pathogens. That strategy should help contain health-care costs and limit in-ICU emergence of bacterial resistance.
Implementing a structured antibiotic stewardship program
Optimizing in-ICU antimicrobial therapy is difficult. No single measure alone can succeed, emphasizing the need to devise a structured antibiotic stewardship program. Unfortunately, the exact set of key interventions essential to this multifaceted and multidisciplinary ‘care bundle’ remains unknown, as do the factors contributing to its success [1],[3],[109],[144]-[146]. The interventions should be packaged so that compliance is readily assessable and achievable, which usually means that each bundle includes no more than five to eight interventions. Table 1 provides an example of antibiotic stewardship for patients with VAP. Successful implementation requires an interdisciplinary team, educational interventions, system innovations, process indicator evaluation, and feedback to health-care workers. Several studies using quasi-experimental designs confirmed the usefulness of such a strategy to optimize in-ICU antibiotic stewardship, but not all designs proved to be effective [111],[147],[148]. As the results of a recent study [149] showed, simply having a reference checklist, without a robust implementation-and-adherence strategy, is unlikely to improve patient outcomes [149],[150].
Computerized decision-support programs linked to electronic patient records can facilitate the dissemination of information to physicians for immediate use in therapeutic decision making and improving quality of care [151]-[154]. Partially or non-automated protocols, often instigated by hospital-based quality-improvement teams, also had demonstrated efficacy [154]-[157]. A prospective intervention of having an infectious disease specialist interact regularly with the medical ICU team was conducted to assess guideline compliance and antibiotic and health-care costs; it achieved significantly reduced use of extended-spectrum penicillins, carbapenems, vancomycin, and metronidazole [157]. Specifically, the intervention group had a significantly lower rate of treatments not corresponding to guidelines, with fewer MV days, shorter stays, and lower in-hospital mortality. Moreover, $89,944 was saved for early antibiotic discontinuation alone [157].
Conclusions
The high antibiotic resistance observed in ICU patients who develop infections limits treatment options and justifies using regimens combining several broad-spectrum antibiotics, even when the presumed infection probability is low, because initial inappropriate therapy has been linked to poor prognoses. More than its economic impact, this ‘spiraling empirical’ practice increasingly leads to undue antibiotic administration to many ICU patients without true infections, paradoxically causing the emergence of more antibiotic-resistant microorganisms causing infections that, in turn, are associated with heightened mortality and morbidity. Therefore, antibiotic therapy for ICU patients with infections should be viewed as a two-stage process: the first involves administering broad-spectrum antibiotics to avoid inappropriate treatment of true bacterial infections, and the second focuses on trying to achieve the first without antibiotic overuse or abuse. In general, the first goal can be accomplished by rapidly identifying patients with infection and starting empirical therapy likely to treat the institution’s most common etiological agents. This strategy requires that initial antibiotic choices be guided by local antibiotic resistance patterns and laboratory test results (including Gram staining), rapidly yielding identities of likely responsible pathogens. The second aim involves stopping therapy when the probability of infection is low, focusing and narrowing treatment once the microorganism is known, switching to monotherapy after day 3 whenever possible, and shortening treatment to 7 to 8 days for most patients, based on the clinical response and bacteriology findings. Therefore, every effort should be made to obtain reliable specimens from the specific suspected infection site in each patient for direct microscope examination and cultures in order to de-escalate antibiotics.
Key messages
-
The rapid in-ICU emergence and dissemination of multidrug-resistant microorganisms worldwide constitute a problem of crisis dimensions that is linked directly to inappropriate antimicrobial use.
-
Appropriate antibiotic stewardship is a two-stage process.
-
Stage I includes rapidly identifying patients with infection, starting an empirical regimen likely to treat the institution’s most common etiological agents, and optimizing bacterial killing by adjusting antibiotic doses and administration modalities based on PK-PD characteristics.
-
Stage II involves stopping therapy in patients unlikely to have infections, focusing and narrowing treatment once the responsible pathogen is known, switching to monotherapy after day 3 whenever possible, and shortening antibiotic administration to 7 to 8 days for most patients, based on the therapeutic response and microbiology data.
-
Any antibiotic stewardship program should be implemented in a structured manner and requires an interdisciplinary team, educational interventions, system innovations, process indicator evaluation, and feedback to health-care workers.
Note
This article is part of a series on Antibiotic resistance in the ICU, edited by Steven Opal. Other articles in this series can be found at http://ccforum.com/series/antibioticresistance.
Abbreviations
- AUC:
-
Area under the concentration curve
- CAI:
-
Community-acquired infection
- GNB:
-
Gram-negative bacilli
- HAI:
-
Hospital-acquired infection
- HAP:
-
Hospital-acquired pneumonia
- IDSA:
-
Infectious Diseases Society of America
- MIC:
-
Minimal inhibitory concentration
- MRSA:
-
Methicillin-resistant Staphylococcus aureus
- MV:
-
Mechanical ventilation
- PCT:
-
Procalcitonin
- PK-PD:
-
Pharmacokinetic-pharmacodynamic
- VAP:
-
Ventilator-associated pneumonia
References
Arnold HM, Micek ST, Skrupky LP, Kollef MH: Antibiotic stewardship in the intensive care unit. Semin Respir Crit Care Med. 2011, 32: 215-227.
Laxminarayan R, Duse A, Wattal C, Zaidi AK, Wertheim HF, Sumpradit N, Vlieghe E, Hara GL, Gould IM, Goossens H, Greko C, So AD, Bigdeli M, Tomson G, Woodhouse W, Ombaka E, Peralta AQ, Qamar FN, Mir F, Kariuki S, Bhutta ZA, Coates A, Bergstrom R, Wright GD, Brown ED, Cars O: Antibiotic resistance - the need for global solutions. Lancet Infect Dis. 2013, 13: 1057-1098.
Leuthner KD, Doern GV: Antimicrobial stewardship programs. J Clin Microbiol. 2013, 51: 3916-3920.
Bergmans DC, Bonten MJ, Gaillard CA, van Tiel FH, van der Geest S, de Leeuw PW, Stobberingh EE: Indications for antibiotic use in ICU patients: a one-year prospective surveillance. J Antimicrob Chemother. 1997, 39: 527-535.
Roberts JA, Paul SK, Akova M, Bassetti M, De Waele JJ, Dimopoulos G, Kaukonen KM, Koulenti D, Martin C, Montravers P, Rello J, Rhodes A, Starr T, Wallis SC, Lipman J: DALI: defining antibiotic levels in intensive care unit patients: are current beta-lactam antibiotic doses sufficient for critically ill patients?. Clin Infect Dis. 2014, 58: 1072-1083.
Kollef MH: Optimizing antibiotic therapy in the intensive care unit setting. Crit Care. 2001, 5: 189-195.
Kollef MH, Fraser VJ: Antibiotic resistance in the intensive care unit. Ann Intern Med. 2001, 134: 298-314.
McGowan JE: Antimicrobial resistance in hospital organisms and its relation to antibiotic use. Rev Infect Dis. 1983, 5: 1033-1048.
Goldmann DA, Weinstein RA, Wenzel RP, Tablan OC, Duma RJ, Gaynes RP, Schlosser J, Martone WJ: Strategies to prevent and control the emergence and spread of antimicrobial-resistant microorganisms in hospitals, A challenge to hospital leadership. JAMA. 1996, 275: 234-240.
Lipsitch M, Bergstrom CT, Levin BR: The epidemiology of antibiotic resistance in hospitals: paradoxes and prescriptions. Proc Natl Acad Sci U S A. 2000, 97: 1938-1943.
MacDougall C, Polk RE: Antimicrobial stewardship programs in health care systems. Clin Microbiol Rev. 2005, 18: 638-656.
Paterson DL: The role of antimicrobial management programs in optimizing antibiotic prescribing within hospitals. Clin Infect Dis. 2006, 42: S90-S95.
Rice LB: The maxwell finland lecture: for the duration-rational antibiotic administration in an era of antimicrobial resistance and clostridium difficile. Clin Infect Dis. 2008, 46: 491-496.
Shlaes DM, Gerding DN, John JF, Craig WA, Bornstein DL, Duncan RA, Eckman MR, Farrer WE, Greene WH, Lorian V, Levy S, McGowan JE, Paul SM, Ruskin J, Tenover FC, Watanakunakorn C: Society for Healthcare Epidemiology of America and Infectious Diseases Society of America joint committee on the prevention of antimicrobial resistance: guidelines for the prevention of antimicrobial resistance in hospitals. Clin Infect Dis. 1997, 25: 584-599.
Sievert DM, Ricks P, Edwards JR, Schneider A, Patel J, Srinivasan A, Kallen A, Limbago B, Fridkin S: Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the national healthcare safety network at the centers for disease control and prevention, 2009–2010. Infect Control Hosp Epidemiol. 2013, 34: 1-14.
Thomas JK, Forrest A, Bhavnani SM, Hyatt JM, Cheng A, Ballow CH, Schentag JJ: Pharmacodynamic evaluation of factors associated with the development of bacterial resistance in acutely ill patients during therapy. Antimicrob Agents Chemother. 1998, 42: 521-527.
Zillich AJ, Sutherland JM, Wilson SJ, Diekema DJ, Ernst EJ, Vaughn TE, Doebbeling BN: Antimicrobial use control measures to prevent and control antimicrobial resistance in US hospitals. Infect Control Hosp Epidemiol. 2006, 27: 1088-1095.
Armand-Lefevre L, Angebault C, Barbier F, Hamelet E, Defrance G, Ruppe E, Bronchard R, Lepeule R, Lucet JC, El Mniai A, Wolff M, Montravers P, Plesiat P, Andremont A: Emergence of imipenem-resistant gram-negative bacilli in intestinal flora of intensive care patients. Antimicrob Agents Chemother. 2013, 57: 1488-1495.
Malhotra-Kumar S, Lammens C, Coenen S, Van Herck K, Goossens H: Effect of azithromycin and clarithromycin therapy on pharyngeal carriage of macrolide-resistant streptococci in healthy volunteers: a randomised, double-blind, placebo-controlled study. Lancet. 2007, 369: 482-490.
Landman D, Quale JM, Mayorga D, Adedeji A, Vangala K, Ravishankar J, Flores C, Brooks S: Citywide clonal outbreak of multiresistant Acinetobacter baumannii and Pseudomonas aeruginosa in Brooklyn, NY: the preantibiotic era has returned. Arch Intern Med. 2002, 162: 1515-1520.
Kollef MH: Inadequate antimicrobial treatment: an important determinant of outcome for hospitalized patients. Clin Infect Dis. 2000, 31: S131-S138.
Kollef MH, Sherman G, Ward S, Fraser VJ: Inadequate antimicrobial treatment of infections: a risk factor for hospital mortality among critically ill patients. Chest. 1999, 115: 462-474.
Kumar A: Early antimicrobial therapy in severe sepsis and septic shock. Curr Infect Dis Rep. 2010, 12: 336-344.
Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, Suppes R, Feinstein D, Zanotti S, Taiberg L, Gurka D, Cheang M: Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006, 34: 1589-1596.
Kumar A, Zarychanski R, Light B, Parrillo J, Maki D, Simon D, Laporta D, Lapinsky S, Ellis P, Mirzanejad Y, Martinka G, Keenan S, Wood G, Arabi Y, Feinstein D, Dodek P, Kravetsky L, Doucette S: Early combination antibiotic therapy yields improved survival compared with monotherapy in septic shock: a propensity-matched analysis. Crit Care Med. 2010, 38: 1773-1785.
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb SA, Beale RJ, Vincent JL, Moreno R: Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013, 41: 580-637.
Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia.Am J Respir Crit Care Med 2005, 171:388–416.,
Masterton RG, Galloway A, French G, Street M, Armstrong J, Brown E, Cleverley J, Dilworth P, Fry C, Gascoigne AD, Knox A, Nathwani D, Spencer R, Wilcox M: Guidelines for the management of hospital-acquired pneumonia in the UK: report of the working party on hospital-acquired pneumonia of the British Society for Antimicrobial Chemotherapy. J Antimicrob Chemother. 2008, 62: 5-34.
Muscedere J, Dodek P, Keenan S, Fowler R, Cook D, Heyland D: Comprehensive evidence-based clinical practice guidelines for ventilator-associated pneumonia: diagnosis and treatment. J Crit Care. 2008, 23: 138-147.
Amaral AC, Holder MW: Timing of antimicrobial therapy after identification of ventilator-associated condition is not associated with mortality in patients with ventilator-associated pneumonia: a cohort study. PLoS One. 2014, 9: e97575-
Bloos F, Thomas-Ruddel D, Ruddel H, Engel C, Schwarzkopf D, Marshall JC, Harbarth S, Simon P, Riessen R, Keh D, Dey K, Weiss M, Toussaint S, Schadler D, Weyland A, Ragaller M, Schwarzkopf K, Eiche J, Kuhnle G, Hoyer H, Hartog C, Kaisers U, Reinhart K: Impact of compliance with infection management guidelines on outcome in patients with severe sepsis: a prospective observational multi-center study. Crit Care. 2014, 18: R42-
Hranjec T, Rosenberger LH, Swenson B, Metzger R, Flohr TR, Politano AD, Riccio LM, Popovsky KA, Sawyer RG: Aggressive versus conservative initiation of antimicrobial treatment in critically ill surgical patients with suspected intensive-care-unit-acquired infection: a quasi-experimental, before and after observational cohort study. Lancet Infect Dis. 2012, 12: 774-780.
Pines JM, Isserman JA, Hinfey PB: The measurement of time to first antibiotic dose for pneumonia in the emergency department: a white paper and position statement prepared for the American Academy of Emergency Medicine. J Emerg Med. 2009, 37: 335-340.
Quattromani E, Powell ES, Khare RK, Cheema N, Sauser K, Periyanayagam U, Pirotte MJ, Feinglass J, Mark Courtney D: Hospital-reported data on the pneumonia quality measure ‘Time to first antibiotic dose’ are not associated with inpatient mortality: results of a nationwide cross-sectional analysis. Acad Emerg Med. 2011, 18: 496-503.
Welker JA, Huston M, McCue JD: Antibiotic timing and errors in diagnosing pneumonia. Arch Intern Med. 2008, 168: 351-356.
Yahav D, Leibovici L, Goldberg E, Bishara J, Paul M: Time to first antibiotic dose for patients hospitalised with community-acquired pneumonia. Int J Antimicrob Agents. 2013, 41: 410-413.
Bouadma L, Luyt CE, Tubach F, Cracco C, Alvarez A, Schwebel C, Schortgen F, Lasocki S, Veber B, Dehoux M, Bernard M, Pasquet B, Regnier B, Brun-Buisson C, Chastre J, Wolff M: Use of procalcitonin to reduce patients’ exposure to antibiotics in intensive care units (prorata trial): a multicentre randomised controlled trial. Lancet. 2010, 375: 463-474.
Layios N, Lambermont B, Canivet JL, Morimont P, Preiser JC, Garweg C, Ledoux D, Frippiat F, Piret S, Giot JB, Wiesen P, Meuris C, Massion P, Leonard P, Nys M, Lancellotti P, Chapelle JP, Damas P: Procalcitonin usefulness for the initiation of antibiotic treatment in intensive care unit patients. Crit Care Med. 2012, 40: 2304-2309.
Luyt CE, Combes A, Trouillet JL, Chastre J: Value of the serum procalcitonin level to guide antimicrobial therapy for patients with ventilator-associated pneumonia. Semin Respir Crit Care Med. 2011, 32: 181-187.
Schuetz P, Albrich W, Christ-Crain M, Chastre J, Mueller B: Procalcitonin for guidance of antibiotic therapy. Expert Rev Anti Infect Ther. 2010, 8: 575-587.
Schuetz P, Muller B, Christ-Crain M, Stolz D, Tamm M, Bouadma L, Luyt CE, Wolff M, Chastre J, Tubach F, Kristoffersen KB, Burkhardt O, Welte T, Schroeder S, Nobre V, Wei L, Bhatnagar N, Bucher HC, Briel M: Procalcitonin to initiate or discontinue antibiotics in acute respiratory tract infections. Cochrane Database Syst Rev. 2012, 9:
Uzzan B, Cohen R, Nicolas P, Cucherat M, Perret GY: Procalcitonin as a diagnostic test for sepsis in critically ill adults and after surgery or trauma: a systematic review and meta-analysis. Crit Care Med. 2006, 34: 1996-2003.
Wacker C, Prkno A, Brunkhorst FM, Schlattmann P: Procalcitonin as a diagnostic marker for sepsis: a systematic review and meta-analysis. Lancet Infect Dis. 2013, 13: 426-435.
Quenot JP, Luyt CE, Roche N, Chalumeau M, Charles PE, Claessens YE, Lasocki S, Bedos JP, Pean Y, Philippart F, Ruiz S, Gras-Leguen C, Dupuy AM, Pugin J, Stahl JP, Misset B, Gauzit R, Brun-Buisson C: Role of biomarkers in the management of antibiotic therapy: An expert panel review ii: clinical use of biomarkers for initiation or discontinuation of antibiotic therapy. Ann Intensive Care. 2013, 3: 21-
Jensen JU, Hein L, Lundgren B, Bestle MH, Mohr TT, Andersen MH, Thornberg KJ, Loken J, Steensen M, Fox Z, Tousi H, Soe-Jensen P, Lauritsen AO, Strange D, Petersen PL, Reiter N, Hestad S, Thormar K, Fjeldborg P, Larsen KM, Drenck NE, Ostergaard C, Kjaer J, Grarup J, Lundgren JD: Procalcitonin-guided interventions against infections to increase early appropriate antibiotics and improve survival in the intensive care unit: a randomized trial. Crit Care Med. 2011, 39: 2048-2058.
Pfister R, Kochanek M, Leygeber T, Brun-Buisson C, Cuquemelle E, Paiva Machado MB, Piacentini E, Hammond NE, Ingram PR, Michels G: Procalcitonin for diagnosis of bacterial pneumonia in critically ill patients during 2009 H1N1 influenza pandemic: a prospective cohort study, systematic review and individual patient data meta-analysis. Crit Care. 2014, 18: R44-
Annane D, Maxime V, Faller JP, Mezher C, Clec’h C, Martel P, Gonzales H, Feissel M, Cohen Y, Capellier G, Gharbi M, Nardi O: Procalcitonin levels to guide antibiotic therapy in adults with non-microbiologically proven apparent severe sepsis: a randomised controlled trial. BMJ Open. 2013, 3: pii: e002186-
Chastre J, Fagon JY: Ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002, 165: 867-903.
Trouillet JL, Vuagnat A, Combes A, Kassis N, Chastre J, Gibert C: Pseudomonas aeruginosa ventilator-associated pneumonia: comparison of episodes due to piperacillin-resistant versus piperacillin-susceptible organisms. Clin Infect Dis. 2002, 34: 1047-1054.
Carmeli Y, Troillet N, Eliopoulos GM, Samore MH: Emergence of antibiotic-resistant pseudomonas aeruginosa: comparison of risks associated with different antipseudomonal agents. Antimicrob Agents Chemother. 1999, 43: 1379-1382.
Luyt CE, Aubry A, Lu Q, Micaelo M, Brechot N, Brossier F, Brisson H, Rouby JJ, Trouillet JL, Combes A, Jarlier V, Chastre J: Imipenem, meropenem, or doripenem to treat patients with pseudomonas aeruginosa ventilator-associated pneumonia. Antimicrob Agents Chemother. 2014, 58: 1372-1380.
Brusselaers N, Labeau S, Vogelaers D, Blot S: Value of lower respiratory tract surveillance cultures to predict bacterial pathogens in ventilator-associated pneumonia: systematic review and diagnostic test accuracy meta-analysis. Intensive Care Med. 2013, 39: 365-375.
Michel F, Franceschini B, Berger P, Arnal JM, Gainnier M, Sainty JM, Papazian L: Early antibiotic treatment for BAL-confirmed ventilator-associated pneumonia: a role for routine endotracheal aspirate cultures. Chest. 2005, 127: 589-597.
Martinez JA, Cobos-Trigueros N, Soriano A, Almela M, Ortega M, Marco F, Pitart C, Sterzik H, Lopez J, Mensa J: Influence of empiric therapy with a beta-lactam alone or combined with an aminoglycoside on prognosis of bacteremia due to gram-negative microorganisms. Antimicrob Agents Chemother. 2010, 54: 3590-3596.
Micek ST, Welch EC, Khan J, Pervez M, Doherty JA, Reichley RM, Kollef MH: Empiric combination antibiotic therapy is associated with improved outcome against sepsis due to gram-negative bacteria: a retrospective analysis. Antimicrob Agents Chemother. 2010, 54: 1742-1748.
Chalmers JD, Taylor JK, Singanayagam A, Fleming GB, Akram AR, Mandal P, Choudhury G, Hill AT: Epidemiology, antibiotic therapy, and clinical outcomes in health care-associated pneumonia: a UK cohort study. Clin Infect Dis. 2011, 53: 107-113.
Garcia-Vidal C, Viasus D, Roset A, Adamuz J, Verdaguer R, Dorca J, Gudiol F, Carratala J: Low incidence of multidrug-resistant organisms in patients with healthcare-associated pneumonia requiring hospitalization. Clin Microbiol Infect. 2011, 17: 1659-1665.
Aliberti S, Di Pasquale M, Zanaboni AM, Cosentini R, Brambilla AM, Seghezzi S, Tarsia P, Mantero M, Blasi F: Stratifying risk factors for multidrug-resistant pathogens in hospitalized patients coming from the community with pneumonia. Clin Infect Dis. 2012, 54: 470-478.
Cardoso T, Ribeiro O, Aragao IC, Costa-Pereira A, Sarmento AE: Additional risk factors for infection by multidrug-resistant pathogens in healthcare-associated infection: a large cohort study. BMC Infect Dis. 2012, 12: 375-
Jeong BH, Koh WJ, Yoo H, Um SW, Suh GY, Chung MP, Kim H, Kwon OJ, Jeon K: Performances of prognostic scoring systems in patients with healthcare-associated pneumonia. Clin Infect Dis. 2013, 56: 625-632.
Shindo Y, Ito R, Kobayashi D, Ando M, Ichikawa M, Shiraki A, Goto Y, Fukui Y, Iwaki M, Okumura J, Yamaguchi I, Yagi T, Tanikawa Y, Sugino Y, Shindoh J, Ogasawara T, Nomura F, Saka H, Yamamoto M, Taniguchi H, Suzuki R, Saito H, Kawamura T, Hasegawa Y: Risk factors for drug-resistant pathogens in community-acquired and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2013, 188: 985-995.
Chalmers JD, Rother C, Salih W, Ewig S: Healthcare-associated pneumonia does not accurately identify potentially resistant pathogens: a systematic review and meta-analysis. Clin Infect Dis. 2014, 58: 330-339.
Park SC, Kim EY, Kang YA, Park MS, Kim YS, Kim SK, Chang J, Jung JY: Validation of a scoring tool to predict drug-resistant pathogens in hospitalised pneumonia patients. Int J Tuberc Lung Dis. 2013, 17: 704-709.
Shorr AF, Zilberberg MD, Reichley R, Kan J, Hoban A, Hoffman J, Micek ST, Kollef MH: Validation of a clinical score for assessing the risk of resistant pathogens in patients with pneumonia presenting to the emergency department. Clin Infect Dis. 2012, 54: 193-198.
Clark AE, Kaleta EJ, Arora A, Wolk DM: Matrix-assisted laser desorption ionization-time of flight mass spectrometry: a fundamental shift in the routine practice of clinical microbiology. Clin Microbiol Rev. 2013, 26: 547-603.
Hrabak J, Chudackova E, Walkova R: Matrix-assisted laser desorption ionization-time of flight (MALDI-TOF) mass spectrometry for detection of antibiotic resistance mechanisms: from research to routine diagnosis. Clin Microbiol Rev. 2013, 26: 103-114.
Clerc O, Prod’hom G, Vogne C, Bizzini A, Calandra T, Greub G: Impact of matrix-assisted laser desorption ionization time-of-flight mass spectrometry on the clinical management of patients with gram-negative bacteremia: a prospective observational study. Clin Infect Dis. 2013, 56: 1101-1107.
Bouza E, Torres MV, Radice C, Cercenado E, de Diego R, Sanchez-Carrillo C, Munoz P: Direct E-test (AB Biodisk) of respiratory samples improves antimicrobial use in ventilator-associated pneumonia. Clin Infect Dis. 2007, 44: 382-387.
Arnold HM, Hollands JM, Skrupky LP, Smith JR, Juang PH, Hampton NB, McCormick S, Reichley RM, Hoban A, Hoffmann J, Micek ST, Kollef MH: Prolonged infusion antibiotics for suspected gram-negative infections in the ICU: a before-after study. Ann Pharmacother. 2013, 47: 170-180.
Dulhunty JM, Roberts JA, Davis JS, Webb SA, Bellomo R, Gomersall C, Shirwadkar C, Eastwood GM, Myburgh J, Paterson DL, Lipman J: Continuous infusion of beta-lactam antibiotics in severe sepsis: a multicenter double-blind, randomized controlled trial. Clin Infect Dis. 2013, 56: 236-244.
Shiu J, Wang E, Tejani AM, Wasdell M: Continuous versus intermittent infusions of antibiotics for the treatment of severe acute infections. Cochrane Database Syst Rev. 2013, 3:
Walker MC, Lam WM, Manasco KB: Continuous and extended infusions of beta-lactam antibiotics in the pediatric population. Ann Pharmacother. 2012, 46: 1537-1546.
Falagas ME, Tansarli GS, Ikawa K, Vardakas KZ: Clinical outcomes with extended or continuous versus short-term intravenous infusion of carbapenems and piperacillin/tazobactam: a systematic review and meta-analysis. Clin Infect Dis. 2013, 56: 272-282.
Abdul-Aziz MH, Dulhunty JM, Bellomo R, Lipman J, Roberts JA: Continuous beta-lactam infusion in critically ill patients: the clinical evidence. Ann Intensive Care. 2012, 2: 37-
Roberts JA, Abdul-Aziz MH, Lipman J, Mouton JW, Vinks AA, Felton TW, Hope WW, Farkas A, Neely MN, Schentag JJ, Drusano G, Frey OR, Theuretzbacher U, Kuti JL: Individualised antibiotic dosing for patients who are critically ill: challenges and potential solutions. Lancet Infect Dis. 2014, 14: 498-509.
Baquero F, Culebras E, Patron C, Perez-Diaz JC, Medrano JC, Vicente MF: Postantibiotic effect of imipenem on gram-positive and gram-negative micro-organisms. J Antimicrob Chemother. 1986, 18: 47-59.
Spivey JM: The postantibiotic effect. Clin Pharm. 1992, 11: 865-875.
Taccone FS, Laterre PF, Dugernier T, Spapen H, Delattre I, Wittebole X, De Backer D, Layeux B, Wallemacq P, Vincent JL, Jacobs F: Insufficient beta-lactam concentrations in the early phase of severe sepsis and septic shock. Crit Care. 2010, 14: R126-
Duszynska W, Taccone FS, Hurkacz M, Kowalska-Krochmal B, Wiela-Hojenska A, Kubler A: Therapeutic drug monitoring of amikacin in septic patients. Crit Care. 2013, 17: R165-
Pea F, Viale P, Pavan F, Furlanut M: Pharmacokinetic considerations for antimicrobial therapy in patients receiving renal replacement therapy. Clin Pharmacokinet. 2007, 46: 997-1038.
Roberts DM, Roberts JA, Roberts MS, Liu X, Nair P, Cole L, Lipman J, Bellomo R: Variability of antibiotic concentrations in critically ill patients receiving continuous renal replacement therapy: a multicentre pharmacokinetic study. Crit Care Med. 2012, 40: 1523-1528.
Trotman RL, Williamson JC, Shoemaker DM, Salzer WL: Antibiotic dosing in critically ill adult patients receiving continuous renal replacement therapy. Clin Infect Dis. 2005, 41: 1159-1166.
Lodise TP, Drusano GL: Pharmacokinetics and pharmacodynamics: optimal antimicrobial therapy in the intensive care unit. Crit Care Clin. 2011, 27: 1-18.
Taccone FS, Laterre PF, Spapen H, Dugernier T, Delattre I, Layeux B, De Backer D, Wittebole X, Wallemacq P, Vincent JL, Jacobs F: Revisiting the loading dose of amikacin for patients with severe sepsis and septic shock. Crit Care. 2010, 14: R53-
Teo J, Liew Y, Lee W, Kwa AL: Prolonged infusion versus intermittent boluses of beta-lactam antibiotics for treatment of acute infections: a meta-analysis. Int J Antimicrob Agents. 2014, 43: 403-411.
Delattre IK, Musuamba FT, Jacqmin P, Taccone FS, Laterre PF, Verbeeck RK, Jacobs F, Wallemacq P: Population pharmacokinetics of four beta-lactams in critically ill septic patients comedicated with amikacin. Clin Biochem. 2012, 45: 780-786.
Grill MF, Maganti RK: Neurotoxic effects associated with antibiotic use: management considerations. Br J Clin Pharmacol. 2011, 72: 381-393.
Naeije G, Lorent S, Vincent JL, Legros B: Continuous epileptiform discharges in patients treated with cefepime or meropenem. Arch Neurol. 2011, 68: 1303-1307.
Kollef MH, Chastre J, Clavel M, Restrepo MI, Michiels B, Kaniga K, Cirillo I, Kimko H, Redman R: A randomized trial of 7-day doripenem versus 10-day imipenem-cilastatin for ventilator-associated pneumonia. Crit Care. 2012, 16: R218-
Udy AA, Baptista JP, Lim NL, Joynt GM, Jarrett P, Wockner L, Boots RJ, Lipman J: Augmented renal clearance in the ICU: results of a multicenter observational study of renal function in critically ill patients with normal plasma creatinine concentrations. Crit Care Med. 2014, 42: 520-527.
Luyt CE, Jacob A, Combes A, Nieszkowszka A, Fernandez C, Trouillet JL, Corkery K, Farinotti R, Chastre J: Nktr-061 (inhaled amikacin) achieves high epithelial lining fluid concentrations in gram-negative pneumonia in intubated and mechanically ventilated patients [abstract]. Am J Respir Crit Care Med. 2007, 175: A328-
Niederman MS, Chastre J, Corkery K, Fink JB, Luyt CE, Garcia MS: Bay41-6551 achieves bactericidal tracheal aspirate amikacin concentrations in mechanically ventilated patients with gram-negative pneumonia. Intensive Care Med. 2012, 38: 263-271.
Palmer LB, Smaldone GC, Chen JJ, Baram D, Duan T, Monteforte M, Varela M, Tempone AK, O’Riordan T, Daroowalla F, Richman P: Aerosolized antibiotics and ventilator-associated tracheobronchitis in the intensive care unit. Crit Care Med. 2008, 36: 2008-2013.
Luyt CE, Combes A, Nieszkowska A, Trouillet JL, Chastre J: Aerosolized antibiotics to treat ventilator-associated pneumonia. Curr Opin Infect Dis. 2009, 22: 154-158.
Luyt CE, Eldon MA, Stass H, Gribben D, Corkery K, Chastre J: Pharmacokinetics and tolerability of amikacin administered as bay41-6551 aerosol in mechanically ventilated patients with gram-negative pneumonia and acute renal failure. J Aerosol Med Pulm Drug Deliv. 2011, 24: 183-190.
Palmer LB, Smaldone GC: Reduction of bacterial resistance with inhaled antibiotics in the ICU. Am J Respir Crit Care Med. 2014, 189: 1225-1233.
Stevens RM, Teres D, Skillman JJ, Feingold DS: Pneumonia in an intensive care unit. A 30-month experience. Arch Intern Med. 1974, 134: 106-111.
Buelow E, Gonzalez TB, Versluis D, Oostdijk EA, Ogilvie LA, van Mourik MS, Oosterink E, van Passel MW, Smidt H, D’Andrea MM, de Been M, Jones BV, Willems RJ, Bonten MJ, van Schaik W: Effects of selective digestive decontamination (SDD) on the gut resistome. J Antimicrob Chemother. 2014, -[Epub ahead of print]
Oostdijk EA, Smits L, de Smet AM, Leverstein-van Hall MA, Kesecioglu J, Bonten MJ: Colistin resistance in gram-negative bacteria during prophylactic topical colistin use in intensive care units. Intensive Care Med. 2013, 39: 653-660.
Singh N, Rogers P, Atwood CW, Wagener MM, Yu VL: Short-course empiric antibiotic therapy for patients with pulmonary infiltrates in the intensive care unit. A proposed solution for indiscriminate antibiotic prescription. Am J Respir Crit Care Med. 2000, 162: 505-511.
Torres A, Ewig S: Diagnosing ventilator-associated pneumonia. N Engl J Med. 2004, 350: 433-435.
Baselski VS, Wunderink RG: Bronchoscopic diagnosis of pneumonia. Clin Microbiol Rev. 1994, 7: 533-558.
Fagon JY, Chastre J, Wolff M, Gervais C, Parer-Aubas S, Stephan F, Similowski T, Mercat A, Diehl JL, Sollet JP, Tenaillon A: Invasive and noninvasive strategies for management of suspected ventilator-associated pneumonia. A randomized trial. Ann Intern Med. 2000, 132: 621-630.
Charbonneau P, Parienti JJ, Thibon P, Ramakers M, Daubin C, du Cheyron D, Lebouvier G, Le Coutour X, Leclercq R: Fluoroquinolone use and methicillin-resistant staphylococcus aureus isolation rates in hospitalized patients: a quasi experimental study. Clin Infect Dis. 2006, 42: 778-784.
Nseir S, Di Pompeo C, Soubrier S, Delour P, Lenci H, Roussel-Delvallez M, Onimus T, Saulnier F, Mathieu D, Durocher A: First-generation fluoroquinolone use and subsequent emergence of multiple drug-resistant bacteria in the intensive care unit. Crit Care Med. 2005, 33: 283-289.
Cornely OA, Bassetti M, Calandra T, Garbino J, Kullberg BJ, Lortholary O, Meersseman W, Akova M, Arendrup MC, Arikan-Akdagli S, Bille J, Castagnola E, Cuenca-Estrella M, Donnelly JP, Groll AH, Herbrecht R, Hope WW, Jensen HE, Lass-Florl C, Petrikkos G, Richardson MD, Roilides E, Verweij PE, Viscoli C, Ullmann AJ: Escmid* guideline for the diagnosis and management of candida diseases 2012: non-neutropenic adult patients. Clin Microbiol Infect. 2012, 18: 19-37.
Rello J, Vidaur L, Sandiumenge A, Rodriguez A, Gualis B, Boque C, Diaz E: De-escalation therapy in ventilator-associated pneumonia. Crit Care Med. 2004, 32: 2183-2190.
Giantsou E, Liratzopoulos N, Efraimidou E, Panopoulou M, Alepopoulou E, Kartali-Ktenidou S, Manolas K: De-escalation therapy rates are significantly higher by bronchoalveolar lavage than by tracheal aspirate. Intensive Care Med. 2007, 33: 1533-1540.
Kaki R, Elligsen M, Walker S, Simor A, Palmay L, Daneman N: Impact of antimicrobial stewardship in critical care: a systematic review. J Antimicrob Chemother. 2011, 66: 1223-1230.
Kim JW, Chung J, Choi SH, Jang HJ, Hong SB, Lim CM, Koh Y: Early use of imipenem/cilastatin and vancomycin followed by de-escalation versus conventional antimicrobials without de-escalation for patients with hospital-acquired pneumonia in a medical ICU: a randomized clinical trial. Crit Care. 2012, 16: R28-
Silva BN, Andriolo RB, Atallah AN, Salomao R: De-escalation of antimicrobial treatment for adults with sepsis, severe sepsis or septic shock. Cochrane Database Syst Rev. 2013, 3:
Bliziotis IA, Samonis G, Vardakas KZ, Chrysanthopoulou S, Falagas ME: Effect of aminoglycoside and beta-lactam combination therapy versus beta-lactam monotherapy on the emergence of antimicrobial resistance: a meta-analysis of randomized, controlled trials. Clin Infect Dis. 2005, 41: 149-158.
Brunkhorst FM, Oppert M, Marx G, Bloos F, Ludewig K, Putensen C, Nierhaus A, Jaschinski U, Meier-Hellmann A, Weyland A, Grundling M, Moerer O, Riessen R, Seibel A, Ragaller M, Buchler MW, John S, Bach F, Spies C, Reill L, Fritz H, Kiehntopf M, Kuhnt E, Bogatsch H, Engel C, Loeffler M, Kollef MH, Reinhart K, Welte T: Effect of empirical treatment with moxifloxacin and meropenem vs meropenem on sepsis-related organ dysfunction in patients with severe sepsis: a randomized trial. JAMA. 2012, 307: 2390-2399.
Chamot E, Boffi El Amari E, Rohner P, Van Delden C: Effectiveness of combination antimicrobial therapy for pseudomonas aeruginosa bacteremia. Antimicrob Agents Chemother. 2003, 47: 2756-2764.
Cometta A, Calandra T, Gaya H, Zinner SH, de Bock R, Del Favero A, Bucaneve G, Crokaert F, Kern WV, Klastersky J, Langenaeken I, Micozzi A, Padmos A, Paesmans M, Viscoli C, Glauser MP: Monotherapy with meropenem versus combination therapy with ceftazidime plus amikacin as empiric therapy for fever in granulocytopenic patients with cancer. The International Antimicrobial Therapy Cooperative Group of the European Organization for Research and Treatment of Cancer and the Gruppo Italiano Malattie Ematologiche Maligne dell’Adulto Infection Program. Antimicrob Agents Chemother. 1996, 40: 1108-1115.
Dupont H, Carbon C, Carlet J: Monotherapy with a broad-spectrum beta-lactam is as effective as its combination with an aminoglycoside in treatment of severe generalized peritonitis: a multicenter randomized controlled trial, The Severe Generalized Peritonitis Study Group. Antimicrob Agents Chemother. 2000, 44: 2028-2033.
Falagas ME, Matthaiou DK, Bliziotis IA: The role of aminoglycosides in combination with a beta-lactam for the treatment of bacterial endocarditis: a meta-analysis of comparative trials. J Antimicrob Chemother. 2006, 57: 639-647.
Furno P, Bucaneve G, Del Favero A: Monotherapy or aminoglycoside-containing combinations for empirical antibiotic treatment of febrile neutropenic patients: a meta-analysis. Lancet Infect Dis. 2002, 2: 231-242.
Heyland DK, Dodek P, Muscedere J, Day A, Cook D: Randomized trial of combination versus monotherapy for the empiric treatment of suspected ventilator-associated pneumonia. Crit Care Med. 2008, 36: 737-744.
Kumar A, Safdar N, Kethireddy S, Chateau D: A survival benefit of combination antibiotic therapy for serious infections associated with sepsis and septic shock is contingent only on the risk of death: a meta-analytic/meta-regression study. Crit Care Med. 2010, 38: 1651-1664.
Paul M, Silbiger I, Grozinsky S, Soares-Weiser K, Leibovici L: Beta lactam antibiotic monotherapy versus beta lactam-aminoglycoside antibiotic combination therapy for sepsis. Cochrane Database Syst Rev. 2006, 1:
Tamma PD, Cosgrove SE, Maragakis LL: Combination therapy for treatment of infections with Gram-negative bacteria. Clin Microbiol Rev. 2012, 25: 450-470.
Marcus R, Paul M, Elphick H, Leibovici L: Clinical implications of beta-lactam-aminoglycoside synergism: systematic review of randomised trials. Int J Antimicrob Agents. 2011, 37: 491-503.
Pena C, Suarez C, Ocampo-Sosa A, Murillas J, Almirante B, Pomar V, Aguilar M, Granados A, Calbo E, Rodriguez-Bano J, Rodriguez F, Tubau F, Oliver A, Martinez-Martinez L: Effect of adequate single-drug vs combination antimicrobial therapy on mortality in pseudomonas aeruginosa bloodstream infections: a post hoc analysis of a prospective cohort. Clin Infect Dis. 2013, 57: 208-216.
Woodhead M, Blasi F, Ewig S, Huchon G, Leven M, Ortqvist A, Schaberg T, Torres A, van der Heijden G, Verheij TJ: Guidelines for the management of adult lower respiratory tract infections. Eur Respir J. 2005, 26: 1138-1180.
Solomkin JS, Mazuski JE, Bradley JS, Rodvold KA, Goldstein EJ, Baron EJ, O’Neill PJ, Chow AW, Dellinger EP, Eachempati SR, Gorbach S, Hilfiker M, May AK, Nathens AB, Sawyer RG, Bartlett JG: Diagnosis and management of complicated intra-abdominal infection in adults and children: guidelines by the surgical infection society and the Infectious Diseases Society of America. Clin Infect Dis. 2010, 50: 133-164.
Combes A, Luyt CE, Fagon JY, Wolff M, Trouillet JL, Chastre J: Early predictors for infection recurrence and death in patients with ventilator-associated pneumonia. Crit Care Med. 2007, 35: 146-154.
Dennesen PJ, van der Ven AJ, Kessels AG, Ramsay G, Bonten MJ: Resolution of infectious parameters after antimicrobial therapy in patients with ventilator-associated pneumonia. Am J Respir Crit Care Med. 2001, 163: 1371-1375.
Luna CM, Blanzaco D, Niederman MS, Matarucco W, Baredes NC, Desmery P, Palizas F, Menga G, Rios F, Apezteguia C: Resolution of ventilator-associated pneumonia: prospective evaluation of the clinical pulmonary infection score as an early clinical predictor of outcome. Crit Care Med. 2003, 31: 676-682.
Chastre J, Wolff M, Fagon JY, Chevret S, Thomas F, Wermert D, Clementi E, Gonzalez J, Jusserand D, Asfar P, Perrin D, Fieux F, Aubas S: Comparison of 8 vs 15 days of antibiotic therapy for ventilator-associated pneumonia in adults: a randomized trial. JAMA. 2003, 290: 2588-2598.
Micek ST, Ward S, Fraser VJ, Kollef MH: A randomized controlled trial of an antibiotic discontinuation policy for clinically suspected ventilator-associated pneumonia. Chest. 2004, 125: 1791-1799.
Hedrick TL, McElearney ST, Smith RL, Evans HL, Pruett TL, Sawyer RG: Duration of antibiotic therapy for ventilator-associated pneumonia caused by non-fermentative gram-negative bacilli. Surg Infect (Larchmt). 2007, 8: 589-598.
Capellier G, Mockly H, Charpentier C, Annane D, Blasco G, Desmettre T, Roch A, Faisy C, Cousson J, Limat S, Mercier M, Papazian L: Early-onset ventilator-associated pneumonia in adults randomized clinical trial: comparison of 8 versus 15 days of antibiotic treatment. PLoS One. 2012, 7: e41290-
Dimopoulos G, Poulakou G, Pneumatikos IA, Armaganidis A, Kollef MH, Matthaiou DK: Short- vs long-duration antibiotic regimens for ventilator-associated pneumonia: a systematic review and meta-analysis. Chest. 2013, 144: 1759-1767.
Pugh R, Grant C, Cooke RP, Dempsey G: Short-course versus prolonged-course antibiotic therapy for hospital-acquired pneumonia in critically ill adults. Cochrane Database Syst Rev. 2011, 10:
Eliakim-Raz N, Yahav D, Paul M, Leibovici L: Duration of antibiotic treatment for acute pyelonephritis and septic urinary tract infection - 7 days or less versus longer treatment: systematic review and meta-analysis of randomized controlled trials. J Antimicrob Chemother. 2013, 68: 2183-2191.
Havey TC, Fowler RA, Daneman N: Duration of antibiotic therapy for bacteremia: a systematic review and meta-analysis. Crit Care. 2011, 15: R267-
Kyriakidou KG, Rafailidis P, Matthaiou DK, Athanasiou S, Falagas ME: Short- versus long-course antibiotic therapy for acute pyelonephritis in adolescents and adults: a meta-analysis of randomized controlled trials. Clin Ther. 2008, 30: 1859-1868.
Nobre V, Harbarth S, Graf JD, Rohner P, Pugin J: Use of procalcitonin to shorten antibiotic treatment duration in septic patients: a randomized trial. Am J Respir Crit Care Med. 2008, 177: 498-505.
Schuetz P, Briel M, Christ-Crain M, Stolz D, Bouadma L, Wolff M, Luyt CE, Chastre J, Tubach F, Kristoffersen KB, Wei L, Burkhardt O, Welte T, Schroeder S, Nobre V, Tamm M, Bhatnagar N, Bucher HC, Mueller B: Procalcitonin to guide initiation and duration of antibiotic treatment in acute respiratory infections: an individual patient data meta-analysis. Clin Infect Dis. 2012, 55: 651-662.
Kopterides P, Siempos II, Tsangaris I, Tsantes A, Armaganidis A: Procalcitonin-guided algorithms of antibiotic therapy in the intensive care unit: a systematic review and meta-analysis of randomized controlled trials. Crit Care Med. 2010, 38: 2229-2241.
Matthaiou DK, Ntani G, Kontogiorgi M, Poulakou G, Armaganidis A, Dimopoulos G: An ESICM systematic review and meta-analysis of procalcitonin-guided antibiotic therapy algorithms in adult critically ill patients. Intensive Care Med. 2012, 38: 940-949.
Prkno A, Wacker C, Brunkhorst FM, Schlattmann P: Procalcitonin-guided therapy in intensive care unit patients with severe sepsis and septic shock - a systematic review and meta-analysis. Crit Care. 2013, 17: R291-
Cotta MO, Roberts JA, Tabah A, Lipman J, Vogelaers D, Blot S: Antimicrobial stewardship of beta-lactams in intensive care units. Expert Rev Anti Infect Ther. 2014, 12: 581-595.
Dellit TH, Owens RC, McGowan JE, Gerding DN, Weinstein RA, Burke JP, Huskins WC, Paterson DL, Fishman NO, Carpenter CF, Brennan PJ, Billeter M, Hooton TM: Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis. 2007, 44: 159-177.
Lawrence KL, Kollef MH: Antimicrobial stewardship in the intensive care unit: advances and obstacles. Am J Respir Crit Care Med. 2009, 179: 434-438.
Davey P, Brown E, Fenelon L, Finch R, Gould I, Hartman G, Holmes A, Ramsay C, Taylor E, Wilcox M, Wiffen P: Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Syst Rev. 2005, 4:
Gomes Silva BN, Andriolo RB, Atallah AN, Salomao R: De-escalation of antimicrobial treatment for adults with sepsis, severe sepsis or septic shock. Cochrane Database Syst Rev. 2010, 12:
Weiss CH, Dibardino D, Rho J, Sung N, Collander B, Wunderink RG: A clinical trial comparing physician prompting with an unprompted automated electronic checklist to reduce empirical antibiotic utilization. Crit Care Med. 2013, 41: 2563-2569.
Weiss CH, Moazed F, McEvoy CA, Singer BD, Szleifer I, Amaral LA, Kwasny M, Watts CM, Persell SD, Baker DW, Sznajder JI, Wunderink RG: Prompting physicians to address a daily checklist and process of care and clinical outcomes: a single-site study. Am J Respir Crit Care Med. 2011, 184: 680-686.
Pestotnik SL, Classen DC, Evans RS, Burke JP: Implementing antibiotic practice guidelines through computer-assisted decision support: clinical and financial outcomes. Ann Intern Med. 1996, 124: 884-890.
Belletti D, Zacker C, Mullins CD: Perspectives on electronic medical records adoption: electronic medical records (EMR) in outcomes research. Patient Relat Outcome Meas. 2010, 1: 29-37.
Kullar R, Goff DA, Schulz LT, Fox BC, Rose WE: The ‘Epic’ challenge of optimizing antimicrobial stewardship: the role of electronic medical records and technology. Clin Infect Dis. 2013, 57: 1005-1013.
Leibovici L, Gitelman V, Yehezkelli Y, Poznanski O, Milo G, Paul M, Ein-Dor P: Improving empirical antibiotic treatment: prospective, nonintervention testing of a decision support system. J Intern Med. 1997, 242: 395-400.
Bailey TC, Ritchie DJ, McMullin ST, Kahn M, Reichley RM, Casabar E, Shannon W, Dunagan WC: A randomized, prospective evaluation of an interventional program to discontinue intravenous antibiotics at two tertiary care teaching institutions. Pharmacotherapy. 1997, 17: 277-281.
Ibrahim EH, Ward S, Sherman G, Schaiff R, Fraser VJ, Kollef MH: Experience with a clinical guideline for the treatment of ventilator-associated pneumonia. Crit Care Med. 2001, 29: 1109-1115.
Rimawi RH, Mazer MA, Siraj DS, Gooch M, Cook PP: Impact of regular collaboration between infectious diseases and critical care practitioners on antimicrobial utilization and patient outcome. Crit Care Med. 2013, 41: 2099-2107.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
C-EL has received lecture honoraria from or served on the advisory board of Thermo Fisher Brahms (Hennigsdorf, Germany), MSD (Whitehouse Station, NJ, USA), bioMérieux (Craponne, France), and Bayer (Leverkusen, Germany). JC has received lecture honoraria from or served on the advisory board of Astellas Pharma (Tokyo, Japan), Bayer/Nektar (San Francisco, CA, USA), Cubist (Lexington, MA, USA), Janssen-Cilag (Issy-les-Moulineaux, France), Pfizer (New York, NY, USA), and Sanofi Pasteur/KaloBios (Lyon, France). The other authors declare that they have no competing interests.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Luyt, CE., Bréchot, N., Trouillet, JL. et al. Antibiotic stewardship in the intensive care unit. Crit Care 18, 480 (2014). https://doi.org/10.1186/s13054-014-0480-6
Published:
DOI: https://doi.org/10.1186/s13054-014-0480-6