Abstract
Background
Neurofibromatosis type 1 (NF1) is a cancer predisposing syndrome. Studies suggest that women < 50 years old (y.o.) with NF1 have an increased breast cancer (BC) incidence and BC associated mortality. However, this has not been widely recognized secondary to small study populations.
Methods
A systematic literature review was conducted through database searches for BC and NF1: 3456 articles identified, 166 reviewed, 58 used for descriptive analysis and 4 utilized for meta-analysis. Fisher’s exact tests, Kaplan-Meier curves and random-effects meta-analysis models were used for analysis.
Results
Two hundred eighty-six cases of NF1 and female BC were identified with a median age of 46 years at diagnosis; 53% were < 50. Peak age of BC diagnosis was between 34 to 44 years. Women < 50 y.o. presented with more advanced disease vs. those ≥50 (56% vs. 22% stage III-IV, respectively; p = 0.005). Median survival for the entire cohort was 5 years vs. the reported median BC survival of over 20 years in the general population using the SEER database. Median age at BC death was 48.5 years; 64% of deceased patients were < 50. Meta-analysis of a total of 4178 women with NF1 revealed a BC standardized incidence ratio (SIR) of 3.07 (95%CI 2.16–4.38) for women with NF1 vs. the general population. Women < 50 y.o. demonstrated a higher SIR of 5.08 (95%CI 3.77–6.81) compared to 1.92 (95%CI 1.40–2.63) if ≥50 y.o.
Conclusions
This systematic literature review and meta-analysis suggests that women with NF1 < 50 y.o. have a five-fold increased risk of BC, present with more advanced disease, and may have an increased BC related mortality. Increased awareness and implementation of recent National Comprehensive Cancer Network early BC screening guidelines for this high-risk patient population is essential. Additional evaluation on the influence of NF1 gene mutations identified in patients undergoing hereditary cancer genetic testing on breast cancer risk in individuals without clinical evidence of NF1 is needed.
Similar content being viewed by others
Background
Neurofibromatosis type I (NF1) is one of the most common autosomal dominant genetic disorders in humans and has a reported incidence of 1 in 2000 to 3000 live births with most population based studies demonstrating a prevalence of the clinical diagnosis in 1 in 3000 to 1 in 5000 individuals [1,2,3,4,5]. Clinical diagnosis of NF1 is made following the National Institutes of Health guidelines in which the patient should have two or more of the seven cardinal diagnostic criteria: six or more café-au-lait spots (> 5 mm pre-puberty, > 15 mm post-puberty); two or more neurofibromas of any type, or one or more plexiform neurofibroma; freckling in the axillae or groin; optic glioma; two or more Lisch nodules; dysplasia of the sphenoid, or dysplasia or thinning of long bone cortex; or first degree relative with NF1 [6, 7]. NF1 is caused by a mutation in the neurofibromin 1 (NF1) gene located on chromosome 17q11.2, with a heterozygous mutation having nearly 100% penetrance [6]. The NF1 gene is 282.7 kilobase pairs in length, contains 60 exons, and encodes neurofibromin [7, 8]. Given its large size, the NF1 gene has one of the highest rates of spontaneous mutations in the entire human genome [6].
Neurofibromin functions as a tumor suppressor gene through regulation of Ras guanosine triphosphatase activity, inhibiting GTPase activation, and regulating cell proliferation and differentiation [6, 7]. Loss of neurofibromin results in uncontrolled cell proliferation and predisposition to the development of several cancers [8, 9]. The most commonly reported malignancies in patients with NF1 are gliomas and malignant peripheral nerve sheath tumors, however gastrointestinal stromal tumors, pheochromocytomas and childhood rhabdomyosarcoma have also been associated with NF1 [10,11,12,13,14]. Interestingly, somatic mutations of the NF1 gene are reported in 27.7% of all breast carcinomas and have been implicated as potential genomic drivers in the development of breast cancer [15, 16].
A link between NF1 and breast cancer has been suggested in several cohort and epidemiological studies [9, 17,18,19,20,21,22] and numerous cases of patients with NF1 presenting with breast cancer have been reported. The strength of the association between NF1 and the increased breast cancer risk remains uncertain due to the small study populations and differences in participants and methodological methods used in the previous studies. The objective of this study is to highlight the association between women with NF1 and an increased risk of breast cancer and to reinforce the importance for physician and patient education on the need for early breast cancer screening for this patient population. In the current study, we conducted a systematic review of the literature and meta-analysis of epidemiological studies to quantitatively assess the association between NF1 and the risk of breast cancer.
Methods
Literature sources and search strategy
The guidelines published by the Meta-analysis of Observational Studies in Epidemiology (MOOSE) group were followed to complete the meta-analysis (Additional file 1) [23]. A literature search was conducted using PubMed and PMC for all relevant studies published in English-language journals up to December 2015. We used the following MeSH and free-text terms in the search strategy: “Neurofibromatoses”, “Neurofibromatosis 1”, “genes, Neurofibromatosis 1”, and “Neurofibromatosis type 1” in combination with “breast neoplasms”, “breast cancer”, “malignancy”, “neoplasm”, “tumor”, or “cancer.” The search was restricted to studies in human beings and publications in English language. The reference lists of identified articles and relevant reviews were also checked for potentially eligible studies.
Study selection
The studies were reviewed and case reports of patients with NF1 and breast cancer and observational studies that investigated the relationship between NF1 and breast cancer risk were reviewed. All studies, including case reports, were included in our descriptive analysis. Studies that met the following criteria were included in the meta-analysis: (i) case-control or cohort-based study design; (ii) investigation of the association between NF1 and breast cancer incidence; (iii) presented standardized incidence ratio (SIR), relative risk (RR), odds ratios (OR), or hazard ratio (HR) estimates with 95% confidence intervals (CI) or sufficient data with which to calculate these. The exclusion criteria were (i) abstracts without full texts, (ii) unpublished studies, (iii) lack of available data, (iv) male sex and (v) the following types of articles: news, previews, reviews, comments, and discussions.
Data extraction and quality assessment
The following data from each included study were extracted: first author, publication year, country, study design, sample size, number of cases/controls, diagnostic criteria, age at time of breast cancer diagnosis, follow-up duration, breast cancer stage at time of diagnosis, breast cancer subtype, development of bilateral breast cancer, development of other primary cancers, development of metastatic breast cancer, survival outcome, and effect sizes (SIR, RR, OR, HR) with 95% CI and adjusted factors. Data were independently extracted and analyzed by two investigators and a final decision was reached by consensus. The methodological quality of the studies included in the meta-analysis was assessed using the Newcastle-Ottawa Scale (NOS) [24]. NOS scores of 0–3, 4–6, and 7–9 were regarded as low, moderate, and high quality, respectively [25].
Comparison to population data
Rough comparisons of the NF1 patients with breast cancer identified in this study were made to the general population using data reported in the Surveillance Epidemiology and End Results (SEER) database for the years 1975–2012 [26]. Age distribution of incident cases and age distribution of deaths for female breast cancer reported in the SEER data base were compared to the age distribution of incident cases and age distribution of deaths of the female NF1 patients with breast cancer identified in this study using SEER data Table 1.11 and Table 1.13 [27, 28]. The relative survival of the female NF1 patients with breast cancer identified in this study was compared to the general population using SEER data Tables 4.14, 4.15, and 4.16 controlling for age and year of diagnosis for each patient [29,30,31].
Statistical analysis
Descriptive statistics were provided to summarize patient characteristics and outcomes for the two NF1 age groups. For those variables in categories, Fisher’s exact test was used for testing across groups. Kaplan-Meier curves were used to estimate survival probabilities for the collected NF1 cases, and compared to the matched survival probabilities of general population from SEER database. To statistically combine estimates from studies that contained sufficient information, we used random effects meta-analysis models [32]. The log(SIR) and corresponding standard error from each study were combined to estimate the overall average SIR. The SIRs for the entire population, those under age 50 and those over age 50 were separately estimated. Each model was fit using the DerSimonian-Laird approach [33] as implemented in the MAd R package [34].
Results
Literature search and study selection
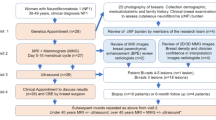
The search strategy resulted in 3796 records: 89 from PubMed, 2572 from PMC and 1135 through examination of reference lists. After excluding duplicated reports, 166 full-text articles were identified on the basis of language, title, and abstract. After further evaluation, 101 records were excluded due to male sex, the lack of NF1 diagnosis, benign breast disease, review article, duplicate data, neurofibromatosis type 2, and non-primary breast cancer. A total of 58 eligible articles published between 1933 and 2015 were identified and were included in the descriptive analysis [9, 10, 17,18,19,20,21,22, 35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84]. Out of the 58 eligible articles, four meet the required inclusion criteria and were included in the meta-analysis [9, 18, 20, 21]. The study selection process is shown in Fig. 1.
Descriptive analysis
Among the 58 studies included in the descriptive analysis, 41 were case reports, one was a case series, 13 were retrospective cohort studies, two were prospective cohort studies, and one was a cross-sectional cohort study. Two hundred and eighty-six cases of NF1 and female breast cancer were identified. The female NF1 patients with breast cancer originated from 23 different countries, with the majority of them originating from the United States of America (38%), United Kingdom (31%), and Japan (12%). Characteristics of these cases are described in Table 1.
Of the 286 cases identified, 181 reported the age of the patient. Mean age at breast cancer diagnosis was 49.3 years with a median age of 46 years and an interquartile range of 38.3 to 58.0 years. The majority of the patients were < 50 years of age with 53% < 50 years old, 28% between 35 and 44 years old and 15% < 35 years old. Age distribution of the incidence of breast cancer identified in these NF1 cases was evaluated based on their age at the time of diagnosis and revealed a peak age of diagnosis between the ages of 34 to 44 years. This incidence of breast cancer cases was compared to the SEER database for reported breast cancer age distribution of incident cases, which demonstrated a peak age of diagnosis between the ages of 55 to 64 years in the general population (Fig. 2a).
Descriptive analysis of breast cancer cases reported. a Age distribution of the incidence of breast cancer identified in 181 NF1 patients compared to the SEER database reported breast cancer age distribution of incident cases. b Distribution of breast cancer stage at time of diagnosis of breast cancer identified in 54 NF1 patients. c Age distribution of the incidence of breast cancer death identified in 76 NF1 patients compared to the SEER database reported breast cancer age distribution of deaths
The type of breast cancer was reported in 110 cases; invasive ductal carcinoma (IDC) was the most commonly reported breast cancer subtype (75.5%). The other 176 breast cancer cases were identified as breast carcinoma. Breast cancer stage at time of diagnosis was reported in 54 cases (27 cases of patients < 50 years of age and 27 cases of patients ≥50 years of age). When analyzing all the female NF1 patients with breast cancer, the majority presented with stage I or II disease. However, when separated by age, women < 50 years of age presented with more advanced disease compared to those ≥50 years of age (56% vs. 22% stage III-IV, respectively, p = 0.005; Fig. 2b).
Follow-up information was provided in 76 of the reported cases. Mean follow-up time was 44.7 months with a range of 1.9 to 204 months. Nearly half of the reported patients were dead at the time of last follow-up. Mean age at breast cancer death was 45.7 years with a median age of 48.5 years and an interquartile range of 41.3–59.7 years. The majority of the patients were < 50 years of age at time of breast cancer death with 64% < 50 years old, 38% between 35 and 44 years old and 10% < 35 years old. Age distribution of the incidence of breast cancer death identified in these NF1 breast cancer cases was evaluated based on their age at the time of death and revealed a peak age of death between the ages of 34 to 44 years. This incidence of breast cancer deaths was compared to the SEER database for reported breast cancer age distribution of deaths, demonstrating a peak age of death between the ages of 55 to 64 years in the general population (Fig. 2c). The relative survival of the female NF1 patients with breast cancer identified in this study was compared to the general population using the SEER database controlling for age and year at diagnosis for each patient (Fig. 3). The median survival for this entire NF1 breast cancer cohort was 5 years compared to the reported median breast cancer survival of over 20 years in the general population using the SEER database. When separated by age, the median survival of the female NF1 patients with breast cancer identified in this study was 5.58 years in those < 50 years of age and over 15 years in those ≥50 years of age.
Relative breast cancer survival. Kaplan-Meier curves were used to estimate survival probabilities for the collected NF1 cases, and compared to the matched survival probabilities of general population from SEER database. Tick marks represent data censored at the last time the patient was known to be alive. Top panel represents 76 female NF1 patients of all ages. Middle panel represents 29 female NF1 patients aged 50 years or older. Bottom panel represents 43 female NF1 patients aged less than 50 years of age
Meta-analysis characteristics of included studies
Among the four included studies, two were from the United States of America (USA) and two were from the United Kingdom (UK). These studies involved a total of 4178 female participants with NF1 who were being followed and documented 87 reported cases of breast cancer. The characteristics of these studies are summarized in Table 2. All included studies identified patients with NF1 via analyses of medical records, genetic registries, or national databases. The diagnoses of breast cancer were made via linked analyses of cancer registries, medical records, or national databases. All the included studies adjusted for age as a potential confounding factor. In quality assessment, the Newcastle-Ottawa Scale score of each included study ranged from 6 to 8 stars.
Meta-analysis results
The unadjusted SIRs for each study and the combined SIR of breast cancer in women with NF1 are presented in Fig. 4. Based on a random-effects model, the combined SIR of breast cancer for all women with NF1 was 3.07 (95% CI: 2.16–4.38). We observed moderate heterogeneity between studies for all women (I2 = 44%). However, women with NF1 < 50 years of age demonstrated a higher SIR of 5.08 (95% CI: 3.77–6.81) compared to 1.92 (95% CI: 1.40–2.63) in those ≥50 years of age. For both age groups, very low heterogeneity was observed with I2 values less than 5%. Similar results were found using a fixed-effects model (data not shown).
Standardized incidence ratio of breast cancer in women with NF1. Random effects meta-analysis models were used to generate Forest plots showing the relationship between NF1 and the risk of female breast cancer for all female patients with NF1 (a) and by age groups (b). Squares represent the risk estimate for each individual study. Horizontal lines represent 95% confidence interval. Diamonds represent the summary risk estimate with 95% confidence interval. SIR, standardized incidence ratio. CI, confidence interval
Discussion
The association between NF1 and increased risk of malignant tumors has been widely described with the most commonly reported associations being gliomas and malignant peripheral nerve sheath tumors [10,11,12,13,14]. Case reports and several cohort and epidemiological studies have described an association of breast cancer with NF1. The first case of a female patient with NF1 and a breast malignancy identified in this study was reported in 1933 by Arthur Jackson, where a 52 year old female with a neurogenic sarcoma of the left breast was presented [35]. Since then, 41 additional case reports/case series have been reported describing an additional 74 females with NF1 that developed breast cancer [17, 36, 38,39,40,41, 44,45,46,47,48,49,50, 53,54,55,56,57,58,59,60,61,62,63,64,65,66,67, 71,72,73,74,75, 77,78,79,80,81,82,83,84]. A total of 16 cohort studies evaluating breast cancer in NF1 patients were identified with a total of 211 cases of female breast cancer reported [9, 10, 18,19,20,21,22, 37, 42, 43, 51, 52, 68,69,70, 76].
Descriptive analysis of these 286 reported cases of NF1 and female breast cancer demonstrated a median age of 46 years at time of breast cancer diagnosis, compared to 62 years in the general population reported in the SEER database. The peak age of breast cancer diagnosis in these NF1 women was between 34 to 44 years. NF1 women younger than 50 years of age were found to have more advanced disease at the time of their breast cancer diagnosis (56% presenting with stage III-IV disease) compared to those 50 years of age or older (22% presenting with stage III-IV disease). The median survival for all of the identified cases of NF1 women with breast cancer was 5 years compared to the reported median breast cancer survival of over 20 years in the general population using the SEER data base. The median age at time of breast cancer death was found to be 48.5 years in this group of NF1 breast cancer cases compared to 68 years in the general population reported in the SEER database. These findings suggest that there is a high incidence of breast cancer in NF1 women younger than 50 years of age and that these women tend to present with more advanced disease and possibly experienced an increased breast cancer related mortality. However, it is important to note that true comparison with SEER database is difficult with this cohort of patients as these patients originated from 23 different countries and the survival reported in the USA SEER database may be better than in some other countries included in this cohort.
To our knowledge, this study is the first meta-analysis to evaluate the association between women with NF1 and the risk of developing breast cancer. Findings of this meta-analysis of 4 cohort studies, following a total of 4178 female patients with NF1, indicate that women with NF1 have a three-fold increased risk of developing breast cancer compared to the general population (SIR = 3.07; 95%CI 2.16–4.38). Additionally, a higher-than-expected number of breast cancer cases were identified in women with NF1 who were younger than 50 years of age, giving a five-fold increased risk of breast cancer in this age group compared to women younger than 50 years old in the general population (SIR = 5.08; 95%CI 3.77–6.81). Women with NF1 who were 50 years of age and older demonstrated a smaller increased risk of breast cancer compared to women 50 years and older in the general population. This lower increased risk of breast cancer in older NF1 patients may be due to the fact that women with NF1 develop breast cancer at a younger age than the general population. Given this early elevated risk a fair number of the susceptible NF1 population may develop breast cancer prior to 50 years of age, thereby decreasing the number of susceptible women in the older population.
In addition to the four studies included in this meta-analysis, several other cohort and epidemiological studies have suggested an association of breast cancer in young women with NF1. In 1972 Brasfield et al. described a cohort of 110 NF1 patients from the USA looking at the biologic behavior and the natural history of this disease. Herein, he found that 5 of 54 (9.3%) females, one of them 39 years old, developed breast cancer and noted that all patients with breast cancer died within 5 years of the breast cancer diagnosis [22]. Following this study, Sorensen et al. described a 42 year follow-up on a nation-wide cohort of 212 NF1 patients from Denmark and found that 7 of 88 (8.0%) females developed breast cancer [42]. In 1988 Huson et al. published a population-based study in south-east Wales to determine the prevalence of NF1 and its complications and identified that 1 of 75 (1.3%) females developed breast cancer; that patient was only 43 years old [43]. Zoller et al. conducted a long term follow-up study of 70 adult NF1 patients previously identified in a population-based study that were living in Goteborg, Sweden where 2 of 33 (6.1%) females were found to have developed breast cancer; of which, one was 38 years of age at the time of her diagnosis [19]. Nakamura et al. evaluated 26 female Japanese patients with NF1 and breast cancer and found an 18.5% incidence of breast cancer in NF1 women younger than 35 years old compared to a previously reported 6.7% incidence in the general Japanese female population among 1438 cases [49]. Kim et al. conducted a retrospective review of 125 NF1 patients to investigate the incidence and spectrum of malignant tumors in Korean NF1 patients and found that 3 of 62 (4.8%) female patients, one less than 50 years of age, developed breast cancer [70].
Walker et al. conducted a prospective population based cohort study of 448 NF1 patients (227 females) to evaluate the incidence and type of malignant tumors in this population in the UK. In this study, five (1.8%) females developed breast cancer and the risk of breast cancer was found to be significantly higher in NF1 patients younger than 50 years of age compared to this age group in the general population; SIR = 4.0 (95% CI: 1.1–10.3) [10]. This increased risk of breast cancer was not seen for NF1 patients 50 years of age or older; SIR = 0.59 (95% CI: 0.02–3.33) [10]. Of note, follow-up in this study was concluded at the time of diagnosis of the earliest first malignant cancer (not at the time of breast cancer diagnosis) and therefore was not included in the meta-analysis of this manuscript. A recently published study not included in the meta-analysis of this manuscript was conducted by Uusitalo et al. to evaluate the cancer incidence and mortality in a population-based cohort of 1404 (737 women) Finnish patients with NF1 [11]. In this study, thirty-one (4.2%) women developed breast cancer and the risk of breast cancer was found to be significantly higher in NF1 patients younger than 40 years of age compared to this age group in the general population; SIR = 11.1 (95% CI: 5.6–19.5) [11]. Additionally, Uusitalo et al. demonstrated that women with NF1 have a five-fold increased risk of breast cancer mortality compared to the general population with a SMR of 5.2 (95% CI: 2.4–9.9) and found that when breast cancer survival was analyzed alone, 5-year survival was poorer in patients with NF1 compared with those without NF1 (67.9% vs. 87.8%, respectively) [11].
Given the rarity of breast cancer events described, especially when divided by age groups, it is important to evaluate a large defined population. This meta-analysis was able to assess the risk of breast cancer in a large defined patient population. The strengths of the present meta-analysis include less influence exerted by small-study bias, a moderate-to-high quality of studies included in the meta-analysis, and very low heterogeneity observed for both age groups. However, this study has several limitations. First, the associations presented are unadjusted. Due to the lack of reporting across studies, other known confounding risk factors for breast cancer, such as medications, smoking, use of hormone replacement therapy, parity or other reproductive factors cannot be accounted for. Thus, one cannot exclude residual or unmeasured confounding as the alternative explanation of these results. Second, given that the number of available cohort studies was limited, this study has a potential to be limited by publication bias. It is possible that a number of neuro-fibromatosis centers have assessed breast cancer in their cohorts without finding evidence of an increased risk and that these findings have not been published. Third, referral bias may be present in two of the included studies [18, 20]. Referral bias of single institution studies of large tertiary centers may result from selective referral of malignant cases to these institutions. Thus, data from these single institution studies may not be representative of the whole population.
This systematic literature review and meta-analysis suggests that women with NF1 less than 50 years of age have a five-fold increased risk of breast cancer, present with more advanced disease, and may have an increased breast cancer related mortality. The findings of this study support the notion that it may be reasonable to consider NF1 in conjunction with other hereditary breast cancer syndromes. Early breast cancer screening guidelines need to be extended to include women with NF1. Given that this study demonstrated a peak age of breast cancer diagnosis between 35 and 44 years of age in these patients with NF1, this study provides further evidence for early breast cancer screening starting at 30 years of age in women with NF1. Guidelines recently produced by the National Comprehensive Cancer Network (NCCN) now suggested early screening for NF1 patients beginning at age 30 [85]. However, screening methods need to be carefully evaluated and weighed against the risk of radiation exposure to young women with NF1. Additionally, core biopsies of image-detected lesions may give a diagnosis of benign neurofibromas rather than breast cancer. The risk of over-diagnosis may be exacerbated by the lower specificity of MRI, although experienced breast radiologists should be able to distinguish neurofibroma from breast cancer in most instances [86].
With the recent improvement and reduced cost of DNA sequencing technology, the use of multigene panels for clinical genetic testing of patients with a high risk of hereditary breast cancer has increased [87]. The NF1 gene is included in some of the breast cancer screening genetic panels as deleterious mutations on the NF1 gene have been associated with a two to four fold increased risk of breast cancer [88]. The goal of these genetic panels are to help stratify of patients according to levels of risk, aid in family cancer genetic counseling, and provide guidance on the identification of women to whom early breast cancer screening, risk-reducing medication, and/or risk-reducing surgery should be offered [88]. However, with the use of multigene panels unexpected pathogenic variants or variants of uncertain significance can be identified for which clinical significance of increased cancer risk is unknown. Multigene panel breast cancer genetic testing may identify mutations in the NF1 gene in patients not previously known to have NF1. Given that approximately 50% patients with NF1 have de novo mutations [89], patients who are identified in this manner should be carefully assessed for subtle features with NF1.
The NF1 gene has been implicated as a breast cancer driver with somatic mutations reported in 27.7% of all breast carcinomas [15, 16]. Previous studies have suggested that a mutation in the NF1 gene may also result in, or predispose cells to, a mutation in other genes on that same chromosome [90]. The NF1 gene and BRCA1 gene are both on chromosome 17, about 20 centiMorgan (cM) apart, and it has been suggested that there may be an interaction between these two genes [58, 81]. However, the risk of breast cancer in patients found to have a variant in the NF1 gene without any clinical evidence of NF1 is not clear.
Couch et al. recently evaluated the risk of breast cancer associated with inactivating variants of the NF1 gene, along with several other genes associated with increased risk of breast cancer, identified by clinical genetic testing of patients with breast cancer. After exclusion of BRCA1, BRCA2, and syndromic breast cancer genes (CDH1, PTEN, and TP53), observed pathogenic variants in ATM, BARD1, CHEK2, PALB2 and RAD51D were associated with high or moderately increased risks of breast cancer [91]. But, pathogenic variants in the NF1 gene were not associated with increased risks of breast cancer [91]. Several other studies assessing the risk of breast cancer with multi-gene panels have also failed to demonstrate an association with NF1 pathogenic variants and an increased risks of breast cancer [92,93,94]. However, Evans et al. warn about the potential pitfalls of using commercial multi-gene panels to confirm syndromic associations with cancers, in particularly NF1 and breast cancer [95]. Their review discussed two main reasons why pathogenic variants in the NF1 gene may have not been associated with an increased risks of breast cancer; 1) it is likely that patients with NF1 are selected out of testing due to their know diagnosis or other socioeconomic factors and 2) lack of appropriate controls [95]. Additionally, a study conducted by Frayling et al. evaluating NF1 constitutional mutation types and breast cancer risk in patients with NF1 and breast cancer showed that different NF1 variants demonstrated different risks of breast cancer and that nonsense and missense mutations may be associated with a higher breast cancer risk [96].
Conclusions
The increased risk of breast cancer found in this meta-analysis and other previous studies reinforces that increased attention to the breast cancer risk in young women with NF1 is needed. Appropriate physician and patient education with increased awareness of the association of early onset breast cancer in patients with NF1 and the need for early breast cancer screening is crucial for this patient population. Continued education of the general public and primary health care providers will allow for appropriate implementation of the most recent NCCN breast cancer screening guidelines in all young women with NF1 starting at 30 years of age. Furthermore, additional studies are required to assess the influence of NF1 pathogenic variants identified in patients undergoing clinical genetic testing on breast cancer risk in individuals without clinical evidence of NF1.
Abbreviations
- CI:
-
Confidence interval
- HR:
-
Hazard ratio
- MOOSE:
-
Meta-analysis of Observational Studies in Epidemiology
- NCCN:
-
National Comprehensive Cancer Network
- NF1:
-
Neurofibromatosis type I
- NOS:
-
Newcastle-Ottawa Scale
- OR:
-
Odds ratios
- RR:
-
Relative risk
- SEER:
-
Surveillance Epidemiology and End Results
- SIR:
-
Standardized incidence ratio
References
Rasmussen SA, Friedman JM. NF1 gene and Neurofibromatosis 1. Am J Epidemiol. 2000;151(1):33–40.
Kallionpää RA, Uusitalo E, Leppävirta J, Pöyhönen M, Peltonen S, Peltonen J. Prevalence of neurofibromatosis type 1 in the Finnish population. Genetics In Medicine. 2018;20(9):1082–6.
Friedman JM. Epidemiology of neurofibromatosis type 1. Am J Med Genet. 1999;89(1):1–6.
Uusitalo E, Leppävirta J, Koffert A, Suominen S, Vahtera J, Vahlberg T, Pöyhönen M, Peltonen J, Peltonen S. Incidence and mortality of Neurofibromatosis: a total population study in Finland. J Investig Dermatol. 2015;135(3):904–6.
Evans DG, Howard E, Giblin C, Clancy T, Spencer H, Huson SM, Lalloo F. Birth incidence and prevalence of tumor-prone syndromes: estimates from a UK family genetic register service. Am J Med Genet A. 2010;152A(2):327–32.
Boyd KP, Korf BR, Theoas A. Neurofibromatosis type 1. J Am Acad Dermatol. 2009;61(1):1–14.
Korf BR. Neurofibromatosis. In: Dulac O, Lassonde M, Sarnat HB, editors. Handbook of Clinical Neurology. Volume 111, edn: Elsevier; 2013. p. 333–40.
Xu W, Yang X, Hu X, Li S. Fifty-four novel mutations in the NF1 gene and integrated analyses of the mutations that modulate splicing. Int J Mol Med. 2014;34:53–60.
Sharif S, Moran A, Huson SM, Iddenden R, Shenton A, Howard E, Evans DGR. Women with neurofibromatosis 1 are at a moderately increased risk of developing breast cancer and should be considered for early screening. J Med Genet. 2007;44(8):481–4.
Walker L, Thompson D, Easton D, Ponder B, Ponder M, Frayling I, Baralle D. A prospective study of neurofibromatosis type 1 cancer incidence in the UK. Br J Cancer. 2006;95(2):233–8.
Uusitalo E, Rantanen M, Kallionpää RA, Pöyhönen M, Leppävirta J, Ylä-Outinen H, Riccardi VM, Pukkala E, Pitkäniemi J, Peltonen S, et al. Distinctive cancer associations in patients with Neurofibromatosis type 1. J Clin Oncol. 2016;34(17):1978–86.
Korf BR. Malignancy in Neurofibromatosis type 1. Oncologist. 2000;5:477–85.
Evans DGR. What is the malignancy risk in Neurofibromatosis type 1? J Clin Oncol. 2016;34(17):1967–9.
Seminog OO, Goldacre MJ. Risk of benign tumours of nervous system, and of malignant neoplasms, in people with neurofibromatosis: population-based record-linkage study. Br J Cancer. 2012;108:193.
The Cancer Genome Atlas Network. In: Comprehensive molecular portraits of human breast tumors. vol. 490. Nature: Macmillan Publishers Limited; 2012: 61–70.
Wallace MD, Pfefferle AD, Shen L, McNairn AJ, Cerami EG, Fallon BL, Rinaldi VD, Southard TL, Perou CM, Schimenti JC. Comparative oncogenomics implicates the neurofibromin 1 gene (NF1) as a breast cancer driver. Genetics. 2012;92(2):385–96.
Salemis NS, Nakos G, Sambaziotis D, Gourgiotis S. Breast cancer associated with type 1 neurofibromatosis. Breast Cancer. 2010;17:306–9.
Madanikia SA, Bergner A, Ye X, O’Neill Blakeley J. Increased risk of breast cancer in women with NF1. Am J Med Genet A. 2012;158A(12):3056–60.
Zoller MET, Rembeck B, Oden A, Samuelson M, Angervall L. Malignant and benign tumors in patients with neurofibromatosis type 1 in a defined Swedish population. Cancer. 1997;79(11):2125–31.
Wang X, Levin AM, Smolinski SE, Vigneau FD, Levin NK, Tainsky MA. Breast cancer and other neoplasms in women with Neurofibromatosis type 1: a retrospective Review of cases in the Detroit metropolitan area. Am J Med Genet Part A. 2012;158A:3061–4.
Seminog OO, Goldacre MJ. Age-specific risk of breast cancer in women with neurofibromatosis type 1. Br J Cancer. 2015;112(9):1546–8.
Brasfield RD, Das Gupta TK. Von Recklinghausen’s disease: a clinicopathological study. Ann Surg. 1972;175(1):86–104.
Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283(15):2008–12.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Li Q, Cui L, Tian Y, Cui H, Li L, Dou W, Li H, Wang L. Protective effect of dietary calcium intake on esophageal Cancer risk: a meta-analysis of observational studies. Nutrients. 2017;9(5):510.
SEER Cancer Statistics Review, 1975-2012, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2012/, based on November 2014 SEER data submission, posted to the SEER web site, April 2015.
Created by www.seer.cancer.gov/csr/1975_2012/download_csr_datafile.php/sect_01_table.11.csv on 02/22/2016 2:27 pm. Source: SEER 18 areas (San Francisco, Connecticut, Detroit, Hawaii, Iowa, New Mexico, Seattle, Utah, Atlanta, San Jose-Monterey, Los Angeles, Alaska Native Registry, Rural Georgia, California excluding SF/SJM/LA, Kentucky, Louisiana, New Jersey and Georgia excluding ATL/RG).
Created by www.seer.cancer.gov/csr/1975_2012/download_csr_datafile.php/sect_01_table.13.csv on 02/22/2016 3:42 pm. Source: US Mortality Files, National Center for Health Statistics, Centers for Disease Control and Prevention.
Created by www.seer.cancer.gov/csr/1975_2012/download_csr_datafile.php/sect_04_table.14.csv on 02/18/2016 8:56 pm.
Created by www.seer.cancer.gov/csr/1975_2012/download_csr_datafile.php/sect_04_table.15.csv on 12/18/2015 7:18 pm.
Created by www.seer.cancer.gov/csr/1975_2012/download_csr_datafile.php/sect_04_table.16.csv on 12/18/2015 7:20 pm.
Thompson SG, Higgins JP. How should meta-regression analyses be undertaken and interpreted? Stat Med. 2002;51(11):1559–73.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Del Re AC & Hoyt WT (2014). MAd: Meta-Analysis with Mean Differences. R package version 0.8–2. URL http://cran.r-project.org/web/packages/MAd.
Jackson AH. Three cases of multiple neurofibromatosis with malignant degeneration. J Nerv Ment Dis. 1933;78(6):581–96.
Hudson LH, Cox TR. Simultaneous neurofibrosarcoma of the breast and back in von Recklinghausen's disease. Am J Surg. 1956;92(3):476–9.
Singleton AO. The surgical aspects of multiple neurofibromatosis. Am Surg. 1970;36(7):451–4.
Lima JB, Smith P. Sipple’s syndrome (pheochromocytoma and thyroid carcinoma) with bilateral breast carcinoma. Am J Surg. 1971;121(6):732–5.
Jain SP. von Recklinghausen's disease presenting as the neurofibrosarcoma of the female breast. J Indian Med Assoc. 1974;63(11):366–8.
Taylor WI. Neurofibromatosis (Recklinghausen's disease) with gastrointestinal and uterine manifestations: report of a case. J Am Osteopath Assoc. 1974;74(1):39–42.
McMillan MD, Edwards JL. Bilateral mandibular metastasis. Oral Surg Oral Med Oral Pathol. 1975;39(6):959–66.
Sorensen SA, Mulvihill JJ, Nielsen A. Long-term follow-up of von Recklinghausen neurofibromatosis. Survival and malignant neoplasms. N Engl J Med. 1986;314(16):1010–5.
Huson SM, Harper PS, Compston DA. Von Recklinghausen neurofibromatosis. A clinical and population study in south-East Wales. Brain. 1988;111:1355–81.
El-Zawahary MD, Farid M, El-Latif AA, Horeia H, El-Gindy M, Twakal G. Breast lesions in generalized neurofibromatosis: breast cancer and cystosarcoma phylloides. Neurofibromatosis. 1989;2(2):121–4.
Sanchis DV, Vazquez Albaladejo C. Von Recklinghausen’s neurofibromatosis. Eur J Surg Oncol. 1992;18(2):202–3.
Aramideh M, de Ongerboer Visser BW, Holstege G, Majoie CB, Speelman JD. Blepharospasm in association with a lower pontine lesion. Neurology. 1996;46(2):476–8.
Malas S, Krawitz HE, Sur RK, Uijs RR, Nayler SJ, Levin CV. Von Recklinghausen’s disease associated with a primary malignant schwannoma of the breast. J Surg Oncol. 1995;59(4):273–5.
Bhargava AK, Bryan N, Nash AG. Localized neurofibromatosis associated with chronic post-mastectomy lymphoedema--a case report. Eur J Surg Oncol. 1996;22(1):114–5.
Nakamura M, Tangoku A, Kusanagi H, Oka M, Suzuki T. Breast cancer associated with Recklinghausen's disease: report of a case. Nihon Geka Hokan. 1998;67(1):3–9.
Murayama Y, Yamamoto Y, Shimojima N, Takahara T, Kikuchi K, Iida S, Kondo Y. T1 breast cancer associated with Von Recklinghausen's Neurofibromatosis. Breast Cancer. 1999;6(3):227–30.
McGaughran JM, Harris DI, Donnai D, Teare D, MacLeod R, Westerbeek R, Kingston H, Super M, Harris R, Evans DG. A clinical study of type 1 neurofibromatosis in north West England. J Med Genet. 1999;36(3):197–203.
Rasmussen SA, Yang Q, Friedman JM. Mortality in Neurofibromatosis 1: an analysis using U.S. death certificates. Am J Hum Genet. 2001;68(5):1110–8.
Natsiopoulos I, Chatzichristou A, Stratis I, Skordalaki A, Makrantonakis N. Metaplastic breast carcinoma in a patient with Von Recklinghausen’s disease. Clinical Breast Cancer. 2007;7(7):573–5.
Yamamoto Y, Kanazawa H, Sugihara T. Breast reconstruction in the von Recklinghausen disease patient. Plast Reconstr Surg. 2002;110(1):357–8.
Ceccaroni M, Genuardi M, Legge F, Lucci-Cordisco E, Carrara S, D’Amico F, Greggi S, Scambia G. BRCA1-related malignancies in a family presenting with von Recklinghausen’s disease. Gynecol Oncol. 2002;86:375–8.
Medina-Franco H, Gamboa-Dominguez A, de La Medina AR. Malignant peripheral nerve sheath tumor of the breast. Breast J. 2003;9(4):332.
Satge D, Sasco AJ, Goldgar D, Vekemans M, Rethore M-O. A 23-year-old woman with Down syndrome, type 1 neurofibromatosis, and breast carcinoma. Am J Med Genet. 2004;125A:94–6.
Guran S, Safali M. A case of neurofibromatosis and breast cancer: loss of heterozygosity of NF1 in breast cancer. Cancer Genet Cytogenet. 2005;156(1):86–8.
Posada JG, Chakmakjian CG. Images in clinical medicine. Von Recklinghausen's disease and breast cancer. N Engl J Med. 2005;352(17):1799.
Stewart DR, Corless CL, Rubin BP, Heinrich MC, Messiaen LM, Kessler LJ, Zhang PJ, Brooks DG. Mitotic recombination as evidence of alternative pathogenesis of gastrointestinal stromal tumours in neurofibromatosis type 1. J Med Genet. 2007;44(1):e61.
Kawawa Y, Okamoto Y, Oharaski T, Takahashi K, Kohda E. Paget’s disease of the breast in a woman with neurofibromatosis. Clin Imaging. 2007;31(2):127–30.
Hasson DM, Khera SY, Meade TL, Dupont EL, Greenberg HM, Diaz NM, Romilly AP, Cox CE. Problems with the use of breast conservation therapy for breast cancer in a patient with neurofibromatosis type 1: a case report. Breast J. 2008;14(2):188–92.
Invernizzi R, Martinelli B, Pinotti G. Association of GIST, breast cancer and schwannoma in a 60-year-old woman affected by type-1 von Recklinghausen's neurofibromatosis. Tumori. 2008;94(1):126–8.
Alamsamimi M, Mirkheshti N, Mohajery MR, Abdollahi M. Bilateral invasive ductal carcinoma in a woman with neurofibromatosis type 1. Arch Iranian Med. 2009;12(4):412–4.
Hegyi L, Thway K, Newton R, Osin P, Nerurkar A, Hayes AJ, Fisher C. Malignant myoepithelioma arising in adenomyoepithelioma of the breast and coincident multiple gastrointestinal stromal tumours in a patient with neurofibromatosis type 1. J Clin Pathol. 2009;62(7):653–5.
Maheswari UM, Shau SS, Borkar DB, Paul B. An unusual presentation of neurofibromatosis with breast carcinoma. Bombay Hospital J. 2009;51(2):193–202.
Takeuchi H, Hiroshige S, Hashimoto K, Kusumoto T, Yoshikawa Y, Muto Y. Synchronous double tumor of breast cancer and gastrointestinal stromal tumor in a patient with neurofibromatosis type 1: report of a case. Anticancer Res. 2011;31(12):4481–4.
Evans DGR, O'Hara C, Wilding A, Ingham SL, Howard E, Dawson J, Moran A, Scott-Kitching V, Holt F, Huson SM. Mortality in neurofibromatosis 1: in North West England: an assessment of actuarial survival in a region of the UK since 1989. Eur J Hum Genet. 2011;19(11):1187–91.
Masocco M, Kodra Y, Vichi M, Conti S, Kanieff M, Pace M, Frova L, Taruscio D. Mortality associated with neurofibromatosis type 1: a study based on Italian death certificates (1995–2006). Orphanet J Rare Dis. 2011;6:11. https://doi.org/10.1186/1750-1172-1186-1111 [Online March 1125, 2011].
Kim ET, Namgung H, Shin HD, Lee SI, Kwon JE, Chang MC, Park DG. Oncologic manifestations of neurofibromatosis type 1 in Korea. J Korean Surg Soc. 2012;82(4):205–2010.
Zhou Y, Pan B, Mao F, Zhu Q, Huo Z, Wang H, Cai F, Liang Z, Wang C, Zhang Y, et al. A hidden breast lump covered by nipple appendices in a patient with von Recklinghausen disease: a case report and Review of the literature. Clin Breast Cancer. 2012;12(1):71–5.
Zagouri F, Sergentanis TN, Domeyer P, Zografos GC. Neurofibromatosis 1 and breast cancer: be alert. Am Surg. 2012;78(11):E446–7.
Onitilo AA, Engel JM. A new NF1 variant in a patient with atypical manifestations. Am J Med Genet A. 2013;161A(2):389–92.
Campos B, Balmana J, Gardenyes J, Valenzuela I, Abad O, Fabregas P, Volpini V, Diez O. Germline mutations in NF1 and BRCA1 in a family with neurofibromatosis type 1 and early-onset breast cancer. Breast Cancer Res Treat. 2013;139:597–602.
Jinkala SR, Rajesh NG, Ramkumar A. Basal like carcinoma of breast in patient with neurofibromatosis I: an association or co-existence? Indian J Pathol Microbiol. 2013;56(2):166–8.
Cheuk DK, Chiang AK, Ha SY, Chan GC. Malignancies in Chinese patients with neurofibromatosis type 1. Hong Kong Med J. 2013;19(1):42–9.
Vivas APM, Bomfin LE, Pinto CA, Nicolau UR, Alves FA. Oral metastasis of metaplastic breast carcinoma in a patient with neurofibromatosis 1. Case Rep Oncol Med. 2014;2014:1–7.
Nogimori M, Yokota K, Sawada M, Matsumoto T, Kono M, Akiyama M. Spindle cell carcinoma of the breast in a patient with neurofibromatosis type 1. Eur J Dermatol. 2014;24(3):397–8.
Kumar N, Pandey AN, Kumari S, Kishore S. Breast cancer associated with Von Recklinghausen's disease: case report and Review of literature. Indian J Surg Oncol. 2014;5(3):205–7.
Silva AVD, Rodrigues FR, Pureza M, Lopes VG, Cunha KS. Breast cancer and neurofibromatosis type 1: a diagnostic challenge in patients with a high number of neurofibromas. BMC Cancer. 2015;15:183.
Chaudhry US, Yang L, Askeland RW, Fajardo LL. Metaplastic breast cancer in a patient with Neurofibromatosis. J Clin Imaging Sci. 2015;5(1):1–4.
Khalil J, Afif M, Elkacemi H, Benoulaid M, Kebdani T, Benjaafar N. Breast cancer associated with neurofibromatosis type 1: a case series and review of the literature. J Med Case Rep. 2015;9(61):1–4.
Jeon YW, Kim RM, Lim ST, Choi HJ, Suh YJ. Early-onset breast cancer in a family with Neurofibromatosis type 1 associated with a germline mutation in BRCA1. J Breast Cancer. 2015;18(1):97–100.
Seo YN, Park YM. Association between Neurofibromatosis type 1 and breast cancer: a report of two cases with a Review of the literature. Case Rep Med. 2015;2015.
Daly MB, Pilarski R, Berry M, Buys SS, Farmer M, Friedman S, Garber JE, Kauff ND, Khan S, Klein C, et al. NCCN Guidelines Insights: Genetic/Familial High-Risk Assessment: Breast and Ovarian, Version 2.2017. 2017;15(1):9–20.
Screening with magnetic resonance imaging and mammography of a UK population at high familial risk of breast cancer: a prospective multicentre cohort study (MARIBS). Lancet 2005, 365(9473):1769–1778.
Kurian AW, Hare EE, Mills MA, Kingham KE, McPherson L, Whittemore AS, McGuire V, Ladabaum U, Kobayashi Y, Lincoln SE et al: Clinical Evaluation of a Multiple-Gene Sequencing Panel for Hereditary Cancer Risk Assessment 2014, 32(19):2001–2009.
Easton DF, Pharoah PDP, Antoniou AC, Tischkowitz M, Tavtigian SV, Nathanson KL, Devilee P, Meindl A, Couch FJ, Southey M et al: Gene-Panel Sequencing and the Prediction of Breast-Cancer Risk 2015, 372(23):2243–2257.
Dubov T, Toledano-Alhadef H, Bokstein F, Constantini S, Ben-Shachar S: The effect of parental age on the presence of de novo mutations – Lessons from neurofibromatosis type I 2016, 4(4):480–486.
Yap YS, McPherson JR, Ong CK, Rozen SG, Teh BT, Lee AS, Callen DF. The NF1 gene revisited - from bench to bedside. Oncotarget. 2014;15(5):5873–92.
Couch FJ, Shimelis H, Hu C, et al. Associations between cancer predisposition testing panel genes and breast cancer. JAMA Oncol. 2017;3(9):1190–6.
Lu H-M, Li S, Black MH, Lee S, Hoiness R, Wu S, Mu W, Huether R, Chen J, Sridhar S, et al. Association of Breast and Ovarian Cancers with Predisposition Genes Identified by large-scale SequencingAssociation of breast and ovarian cancers with predisposition genes identified by large-scale SequencingAssociation of breast and ovarian cancers with predisposition genes identified by large-scale sequencing. JAMA Oncology. 2019;5(1):51–7.
Shimelis H, LaDuca H, Hu C, Hart SN, Na J, Thomas A, Akinhanmi M, Moore RM, Brauch H, Cox A, et al. Triple-negative breast Cancer risk genes identified by multigene hereditary cancer panel testing. J Natl Cancer Inst. 2018;110(8):855–62.
Thompson ER, Rowley SM, Li N, McInerny S, Devereux L, Wong-Brown MW, Trainer AH, Mitchell G, Scott RJ, James PA et al: Panel Testing for Familial Breast Cancer: Calibrating the Tension Between Research and Clinical Care 2016, 34(13):1455–1459.
Evans DG, Howell SJ, Frayling IM, Peltonen J. Gene panel testing for breast cancer should not be used to confirm syndromic gene associations. NPJ Genomic Med. 2018;3:32.
Frayling IM, Mautner V-F, van Minkelen R, Kallionpaa RA, Aktaş S, Baralle D, Ben-Shachar S, Callaway A, Cox H, Eccles DM, et al. Breast cancer risk in neurofibromatosis type 1 is a function of the type of NF1 gene mutation: a new genotype-phenotype correlation. J Med Genet. 2018; jmedgenet-2018-105599.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Institutes of Health Grant T32 5T32CA090223–12 (WEC) and P01 CA95426 (WEC). The funding body was not involved in the study design, collection, analysis, interpretation of data, or in writing of the manuscript.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Prior presentations
Abstracts of this work were presented at the Annual Presidential Symposium of the Columbus Surgical Society in Columbus, OH (2016, February) and at the Society of Surgical Oncology 70th Annual Cancer Symposium in Seattle, WA (2017, March). This manuscript, or any part of it, has not been published and will not be submitted elsewhere for publication while being considered by Hereditary Cancer in Clinical Practice.
Author information
Authors and Affiliations
Contributions
LPSK and WEC contributed to the study conception and research design. LY, DK and EBS verified proposed analytical methods. LPSK, LY and DK were involved in collection and assembly of data and data analysis. LPSK, LY, DK, EBS, DMA and WEC were involved in data interpretation. LPSK, LY, DK and WEC were involved in manuscript writing. LSK, EBS, DMA and WEC were involved in critical review of the manuscript. LPSK, LY, DK, EBS, DMA, and WEC provided final approval of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Meta-analysis of Observational Studies in Epidemiology (MOOSE) Checklist. Checklist with brief description of how research criteria of observational studies in epidemiology were handled for reporting of background, search strategy, methods, results, discussion, and conclusion in the meta-analysis. (PDF 306 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Suarez-Kelly, L.P., Yu, L., Kline, D. et al. Increased breast cancer risk in women with neurofibromatosis type 1: a meta-analysis and systematic review of the literature. Hered Cancer Clin Pract 17, 12 (2019). https://doi.org/10.1186/s13053-019-0110-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13053-019-0110-z